Abstract
Purpose
Very few studies have compared alumina-on-alumina ceramic and alumina-on-highly cross-linked polyethylene bearings in the same patient. The purpose of this prospective randomised study was to compare the clinical and radiographic results and the prevalence of osteolysis in cementless total hip arthroplasty using an alumina-on-alumina and alumina-on-highly cross-linked polyethylene bearings in young active patients.
Methods
We prospectively compared the results of 100 patients (200 hips) who had undergone a cementless total hip arthroplasty with an alumina-on-alumina ceramic bearing in one hip and an alumina-on-highly cross-linked polyethylene in the other. There were 66 men and 34 women with a mean age of 45.3 years (range, 21–49 years) at the time of surgery. The mean follow-up was 12.4 years (range, 11–13 years). The patients were assessed clinically and radiographically at three months, one year, and annually thereafter.
Results
Harris hip, Western Ontario and McMaster Universities Osteoarthritis Index, and University of California, Los Angeles activity scores did not show statistically significant differences between the two groups of bearings preoperatively or at the time of final follow-up. Radiographic findings of the component were not significantly different between the two groups. The mean polyethylene linear penetration was 0.031 ± 0.004 mm per year. No hips in either group displayed osteolysis. The Kaplan-Meier survivorship with revision as the end point at 12.4 years was 100 % (95 % confidence interval [CI], 94–100 %) for the femoral component in both groups and 99 % (95 %CI, 93–100 %) for the acetabular component.
Conclusion
The clinical and radiographic results of using an alumina-on-alumina ceramic and alumina-on-highly cross-linked polyethylene bearings were similar.
Keywords: Comparison ceramic on ceramic versus ceramic on highly cross-linked polyethylene, Prospective randomised controlled trial, Similar outcome
Introduction
Although mechanical fixation of contemporary total hip arthroplasty (THA) has improved markedly, the prevalence of osteolysis has increased with polyethylene wear rates in young patients [1, 2]. Strategies to reduce wear have focused on improvements in the bearing surface such as ceramic-on-ceramic or ceramic-on-highly cross-linked polyethylene bearings. Several studies have demonstrated that contemporary ceramic-on-ceramic or ceramic-on-highly cross-linked polyethylene bearings are associated with low prevalence of osteolysis in young and active patients [3–12].
Despite contemporary cementless THA with alumina-on-alumina bearings giving excellent clinical and radiographic outcomes, squeaking and fracture of the alumina head or acetabular liner have been reported in the literature [6, 13–16]. Therefore, the question arises as to whether alumina-on-highly cross-linked polyethylene bearings can replace alumina-on-alumina to reduce the prevalence of squeaking and ceramic fracture. To our knowledge, very few studies have compared alumina-on-alumina ceramic and alumina-on-highly cross-linked polyethylene bearings in the same patient.
The purpose of this prospective randomised study was to compare the clinical and radiographic results of cementless THA using alumina-on-alumina and alumina-on-highly cross-linked polyethylene bearings in young active patients. We also compared the prevalence of osteolysis, squeaking, and fracture of ceramic, or highly cross-linked polyethylene.
Materials and methods
From January 2000 to January 2002, 210 consecutive cementless THAs were performed in 105 patients who were aged less than 50 years, placing an alumina-on-alumina ceramic bearing (BIOLOX-forte, CeramTec, Plochingen, Germany) in one hip and an alumina-on-highly cross-linked polyethylene bearing (Marathon, DePuy, Warsaw, Indiana) in the other in each patient. In the Marathon process, extruded rod bar stock is irradiated with a dose of 50 kGy and then remelted at 150 °C. After remelting, the rods are annealed at 120 °C for 24 hours. Acetabular components are machined from the processed bar stock, enclosed in gas-permeable packaging, and then gas plasma sterilised. All patients underwent bilateral simultaneous sequential THAs at the same sitting. The study was approved by our institutional review board, and all patients provided informed consent. No patient died during the minimum 11-years follow-up. Five patients (ten hips) who moved abroad were lost to follow-up (before one year), leaving 100 patients (200 hips) in this study.
Sixty-six men and 34 women were enrolled in this study. The average age at the time of the index arthroplasty was 45.3 years (range, 21–49 years). The average weight of the patients was 69 kg (range, 52–109 kg). The average height was 173.1 cm (range, 159–188 cm) and the average body-mass index 23 kg/m2 (range, 20.1–38.7 kg/m2). The diagnosis was osteonecrosis of femoral head in 63 patients (63 %), developmental dysplasia in 20 (20 %), osteoarthritis in 13 (13 %), multiple epiphyseal dysplasia in two (2 %), and rheumatoid arthritis in 2 (2 %). All hips with osteonecrosis of the femoral head were Ficat stage III or IV [17]. The presumed cause of osteonecrosis was ethanol abuse in 35 patients (56 %), idiopathic in 19 (30 %), and steroid use in nine patients (14 %). The average follow-up period was 12.4 years (range, 11–13 years).
All surgeries were performed by a senior author (YHK) using a posterolateral surgical approach. A cementless Duraloc 100 or 1200 series acetabular component with an alumina forte liner of an inner diameter of 28 mm was used on one side and a cementless Duraloc 100 or 1200 series acetabular component with a highly cross-linked polyethylene liner of an inner diameter of 28 mm was used on the opposite side in each patient. Acetabular components were inserted using a press-fit technique. The average diameter of the cup was 51.2 mm (range, 48–54 mm) in both groups of bearings. The average polyethylene thickness was 7.6 mm (range, 6.0–8.9 mm). Randomisation of the use of an alumina forte or highly cross-linked polyethylene liner was determined from a sequential pool based on a table of random numbers. All patients received an Immediate Postoperative Stability cementless femoral component (IPS; DePuy, Leeds, United Kingdom) with a 28-mm alumina forte femoral head (BIOLOX-forte, CeramTec). The femoral component was inserted using a press-fit technique. The largest broach that would fit the metaphysis was used. The IPS femoral component is an anatomical metaphyseal-fitting titanium stem with a polished and tapered distal stem, designed to provide fixation in the metaphysis only, thus avoiding metal-to-bone contact below this point. The proximal 30 % of the femoral stem was porous-coated with sintered titanium beads displaying a mean pore size of 250 μm, to which a hydroxyapatite coating (thickness, 30 μm) was applied.
The patients were allowed to stand on the second postoperative day, and progressed to full weight-bearing with crutches, as tolerated. They were advised to use crutches for four weeks and then a cane, if required, while walking thereafter.
Clinical follow-up was at three months and one year, and yearly thereafter. Harris hip scores [18] and Western Ontario and McMaster Universities Osteoarthritis (WOMAC) [19] scores were determined before surgery and at the time of each follow-up. Patients subjectively evaluated thigh pain on a 10-point visual analog scale (with 0 indicating no pain and 10 indicating severe pain). The level of activity of the patients after the THA was assessed with the activity score of the University of California, Los Angeles (UCLA) [20].
Radiographic follow-up was at three months and one year, and yearly thereafter. An anteroposterior radiograph of the pelvis with the patient supine and with both hips in neutral rotation and 0° abduction, was undertaken for each patient. Consistent patient positioning was ensured by the use of a frame, which was constructed in such a way that it could be placed at the end of a standard X-ray table. Plastic polypropylene orthoses were secured to a plastic back-board through a vertical slot, and a wing nut allowed adjustment for limb length. Rotation and abduction remained constant. Cross-table lateral radiographs were also performed for each hip.
Femoral bone type was determined on preoperative radiographs applying the Dorr classification system [21]. The adequacy of the intramedullary fill by the stem was recorded according to a previously described method [22].
Definite loosening of the femoral component was defined as progressive axial subsidence of more than three millimetres or varus or valgus shift [23]. A femoral component was considered to be possibly loose when there was a complete radiolucent line surrounding the entire porous-coated surface on both the anteroposterior and lateral radiographs [24].
Definite loosening of the acetabular component was diagnosed when there was a change in the position of the component (greater than two millimetres vertically [25] and/or medially or laterally) or a continuous radiolucent line wider than two millimetres on both the anteroposterior and the lateral radiographs [25].
Penetration of the polyethylene liner was measured with AutoCAD 2013 (Autodesk, Inc., San Rafael, California) by three observers blinded to the clinical results [22]. The observers conducted three measurements on each radiograph, and the interobserver error was assessed. A ScanMaker 9600XL flatbed scanner (Microtek, Carson, California) digitised the anteroposterior radiograph of the pelvis as two-dimensional grey-scale arrays of twelve-bit (256-grey level) integers. The scanning resolution was 600 pixels per square inch (psi). Penetration of the head into the liner was determined annually from the anteroposterior pelvic radiographs. The amount of penetration on radiographs taken three months postoperatively was considered to be the “zero” position.
The presence and location of osteolysis in the acetabulum and femur were recorded in the anteroposterior and lateral radiographs according to the system of DeLee and Charnley [26] and Gruen et al. [27], respectively. The length and width of osteolytic lesions were measured, and the area expressed in square centimetres.
We developed an algorithm to address the beam-hardening artifacts and to measure the volume of ostolytic lesions. CT images were acquired using a Siemens AG scanner (Munich, Germany) with one millimetre collimation, a pitch of 1.5, and a 14–22-cm field of view. The raw data were reconstructed for one millimetre slices. The area within five centimetres of the prosthesis-bone interface in all directions was evaluated. The volume of osteolysis was calculated using a quantitative imaging system (VirtualScopics, Rochester, New York). CT images were acquired for all patients at an average follow-up time of 12.4 years (range, 11–13 years).
We performed priori power calculation using a clinically relevant difference in Harris hip score of 5 points and a standard deviation of 6.5 points. With α = 0.05 and β = 0.95, calculation revealed that a total of 89 patients would be needed in each group. To account for possible dropouts, we recruited about 10 % more participants, leading to 100 patients in each group. A post hoc power analysis using the actual number of patients in the study and the expected Harris hip score differences demonstrated 100 % power to detect those differences.
The change in the Harris hip, WOMAC and UCLA activity scores were evaluated with Student paired t test and the Pearson nonparametric chi-square test. The ranges of motion of the hip were compared between the two groups using a two-way repeated-measures analysis of variance. Nonparametric chi-square tests were used to compare complication rates and radiographic data between the two groups. The level of significance was set at p < 0.05. Kaplan-Meier survivorship analysis [28] was used to estimate the probability of retention of the total hip in the entire cohort. Ninety-five percent confidence intervals were calculated.
Results
In the ceramic-on-ceramic group of bearings, the mean preoperative Harris hip score was 38 points (range, 16–41 points), which improved to a mean of 94 points (range, 80–100 points) at the time of final follow-up. In the ceramic-on-highly cross-linked polyethylene group, the mean preoperative Harris hip score was 37 points (range, 11–45 points), which improved to 95 points (range, 85–100 points) at the time of final follow-up.
Dependence on walking aids and limp had decreased substantially at the time of final follow-up. At the last follow-up, 95 patients (95 %) in the ceramic-on-ceramic group and 94 patients (94 %) in the ceramic-on-highly cross-linked polyethylene group had no detectable limp. Mild limp was noticed in five patients (5 %) in the ceramic-on-ceramic group and six (6 %) in the ceramic-on-highly cross-linked polyethylene group. The ability to use stairs and public transportation, put on foot wear, and cut toenails was improved markedly after the operation. The mean preoperative UCLA activity score was 3 points (range, 1–5 points), which improved to a mean of 7.0 points (range, 5–8 points) in both groups at the final follow-up (Table 1).
Table 1.
Clinical results
| Parameter | Alumina-on-alumina bearing | Alumina-on-highly cross-linked polyethylene bearing | P-value (chi-square test) |
|---|---|---|---|
| Harris hip score (points)a | |||
| Preoperative | 38 (16–41) | 37 (11–45) | 0.673 |
| Postoperative | 94 (80–100) | 95 (85–100) | 0.785 |
| Thigh pain | 0 (0 %) | 0 (0 %) | |
| WOMAC score (point)a | |||
| Preoperative | 62 (49–81) | 63 (50–78) | 0.849 |
| Postoperative | 12 (9–12) | 11 (8–13) | 0.852 |
| UCLA activity scorea | |||
| Preoperative | 3 (1–5) | 3 (1–5) | 1.000 |
| Postoperative | 7.0 (5–8) | 7.0 (5–8) | 1.000 |
| Squeaking sound | 3 hips (3 %) | – | – |
| Clicking | 10 hips (2 %) | – | – |
| Follow-up (years) | 12.4 (11–13) | – | |
a The values are given as the mean with the range in parentheses
WOMAC Western Ontario and McMaster Universities Osteoarthritis Index, UCLA University of California, Los Angeles
No patient had thigh pain one year after the THA in both groups of bearings.
Eighteen (18 %) of the 100 patients changed their work involving heavy manual labour before the operation to sedentary work after it. The remaining 82 patients (82 %) remained in the previous occupation after the operation. All patients were advised not to participate in high-impact sports.
Three hips (3 %) with alumina-on-alumina ceramic bearings had squeaking sounds and ten hips (10 %) with alumina-on-alumina ceramic bearings had clicking sounds. No hips with squeaking or clicking sounds required revision. No hips with alumina-on-highly cross-linked polyethylene bearings had squeaking or clicking sounds.
No hip in either group had a fracture of ceramic head or acetabular ceramic liner.
There were no significant differences between the two groups in terms of Dorr bone type [18], acetabular and femoral component position, central rotation of the femoral head, femoral offset, abductor moment arm, limb length discrepancy, prevalence of radiolucent line, migration of the acetabular and femoral components, prevalence of osteolysis, and prevalence of aseptic loosening (Table 2).
Table 2.
Radiographic results for 200 hips
| Parameter | Alumina-on-alumina bearing | Alumina-on-highly cross-linked polyethylene bearing | P-value (paired t test) |
|---|---|---|---|
| Dorr bone type (no. [%]) | |||
| A | 85 (85 %) | 88 (88 %) | 0.519 |
| B | 15 (15 %) | 12 (12 %) | 0.525 |
| C | 0 (0 %) | 0 (0 %) | – |
| Acetabular component positiona (deg) | |||
| Inclination | 43.5 (35–45) | 42.8 (38–46) | 0.331 |
| Anteversion | 21.2 (19–26) | 22.0 (18–25) | 0.235 |
| Femoral component position (no. [%]) | |||
| Neutral position | 87 (87) | 85 (85) | 0.781 |
| Varus position | 12 (12) | 11 (11) | 0.932 |
| Valgus position | 1 (1) | 4 (4) | 0.131 |
| Centre of rotationa | |||
| Horizontal (mm) | 42 (36–47) | 41 (34 to 48) | 0.959 |
| Vertical (mm) | 15.1 (13–20) | 15 (12–21) | 0.782 |
| Femoral offseta (mm) | 39.8 (37–81) | 41 (38–83) | 0.717 |
| Abductor moment arma (mm) | 45 (39–85) | 46 (38–83) | 0.521 |
| Limb length discrepancyb (mm) | 0.3 ± 0.5 (−1.2–1.4) | 0.4 ± 0.3 (−0.8–1.2) | 0.821 |
| Radiolucent line (> 1 mm) (no. [%]) | 0 (0) | 0 (0) | – |
| Migration of the acetabular component (no. [%]) | 0 (0) | 0 (0) | – |
| Migration of the femoral component | 0 (0) | 0 (0) | – |
| Osteolysis (no. [%]) | |||
| Acetabular component | 0 (0) | 0 (0) | – |
| Femoral component | 0 (0) | 0 (0) | – |
| Stress shielding of femur | |||
| Calcar round off | 100 (100) | 100 (100) | |
| Head penetrationb (mm) | Not detectable | 0.337 ± 0.315 0.031 ± 0.004 m/year |
1.000 |
| Aseptic loosening (no. [%]) | 0 (0 %) | 0 (0 %) | – |
a The values are given as the mean with the range in parentheses
bThe values are given as the mean and the standard deviation, with the range in parentheses
The mean total amount (and standard error of the mean) of highly cross-linked polyethylene linear penetration was 0.337 ± 0.315 mm, and the mean annual penetration rate was 0.031 ± 0.004 mm per year. Normal accuracy of the measurement of this system was 0.001 mm. The chance-corrected kappa coefficient, which was calculated to determine interobserver agreement of hip scoring and wear measurement, was between 0.76 and 0.86. We noted increased penetration in the first postoperative year, suggesting that it was the bedding-in period. At a mean follow-up time of 12.4 years, four hips were outliers of the so-called osteolysis threshold of 0.10 mm per year, with the remaining 96 liners exhibiting a penetration rate below this level. In the four hips that were the outliers, there was no evidence of acetabular or femoral osteolysis. With the numbers available, univariate regression analysis revealed that age, sex, weight, activity level, cup inclination or cup anteversion had no influence on polyethylene liner penetration.
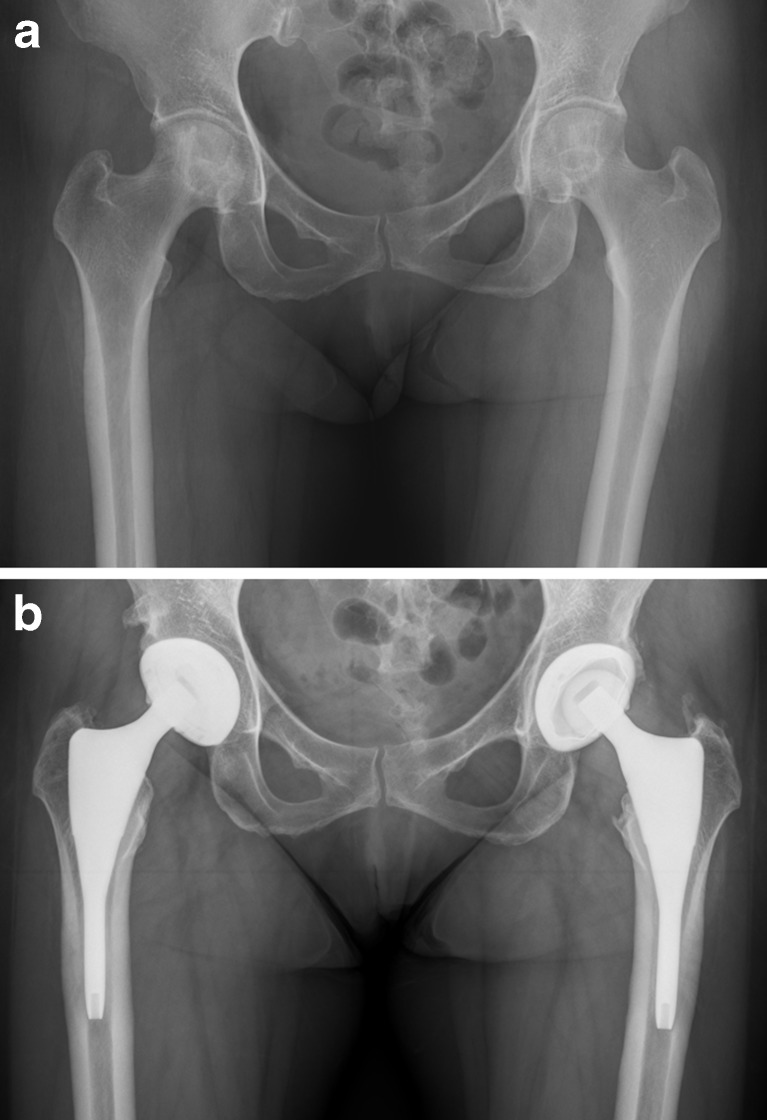
Radiographs and CT scans (Fig. 1) demonstrated that no acetabular or femoral osteolysis was detected in any hip at the time of the last follow-up.
Fig. 1.
Radiographs of a 43-year-old woman with osteonecrosis of both femoral heads. a A preoperative anteroposterior view of both hips shows a collapsed femoral head and Dorr type-A femoral bone. b An anteroposterior view of both hips taken 12 years after the hip arthroplasty shows that the acetabular and femoral components at both hips are solidly fixed in a satisfactory position, with no evidence of osteolysis. The right hip has an alumina-on-alumina ceramic bearing and the left hip has an alumina-on-highly cross-linked polyethylene
No femoral or acetabular component was revised because of aseptic loosening. One acetabular component (1 %) in each group was revised because of recurrent dislocation.
Kaplan-Meier survivorship analysis [28] revealed that the rate of survival of the femoral component at 12.4 years was 100 % (95 % confidence interval, 94–100 %), with loosening or revision considered the end-point for failure. Furthermore, the survival of the acetabular component was 99 % (95 %CI, 93–100 %) at 12.4 years, with loosening or revision considered the end point for failure.
Discussion
The midterm results of cementless metaphyseal fitting anatomic total hip THA with both an alumina-on-alumina and an alumina-on-highly cross-linked polyethylene bearings in our patients aged less than 50 years demonstrated an extremely low prevalence of thigh pain and no loosening or osteolysis. Our results are consistent with those from other studies on ceramic-on-ceramic bearing [10, 11, 29–34] and ceramic-on-highly cross-linked polyethylene bearing [3–5, 9].
The most common potential causes of thigh pain are instability of the femoral stem and a tight distal fill by a rigid femoral stem [3, 4, 6, 34]. The low prevalence of transitory thigh pain in our present series could be attributed to the axial and torsional stability of the stem, resulting from rigid proximal fixation of the stem and the absence of or minimal contact between the tapered polished distal part of stem and the inner cortex of the femur.
The mechanical fixation of a current generation of cementless total hip prostheses in young patients is quite encouraging [3, 4, 6, 24, 25, 34–36]. We showed in our study that this hip system had no mechanical failure (0 % at 12.4 years) despite a high patient activity level. We believe that several factors were responsible for our good results in young patients: the proximal canal-fitting design of the femoral stem, including pronounced lateral flare; anteroposterior buildup; the short and narrow polished distal end of the stem; a surgical technique that optimised fit; the strong trabecular bone in young patients; small and light patients; the absence of comorbidities; faster mobilisation than older patients; the use of an alumina-on-alumina ceramic or alumina-on-highly cross-linked polyethylene articulation; and a relatively consistent and optimal alignment of the acetabular component, avoiding impingement.
Recent studies of the third-generation alumina bearings have found little or no osteolysis [3, 7, 16, 32, 34]. Accordingly, we also found no osteolysis. We postulate that extremely low wear and the scant damage of the optimally positioned articular surface were insufficient to cause osteolysis.
The reported prevalence of squeaking with ceramic-on-ceramic bearing has ranged from 1 to 21 % [13–15]. In our series, three hips (3 %) demonstrated a squeaking sound and ten hips (10 %) demonstrated a clicking sound. Contributing factors to the low prevalence of squeaking or clicking sound in the present series may be related to the lower height and weight of the patient and the optimal acetabular component position.
Fracture of the alumina femoral head or acetabular liner has been reported in the literature [16, 33]. The absence of a ceramic head or liner fracture in our series was attributed to optimal cup orientation and optimal interlocking of the alumina head and taper of the stem.
Several authors have reported that the wear rate for alumina-on-highly cross-linked polyethylene was between 0.031 mm per year and 0.06 mm per year [3–5, 9] and they found no osteolysis. Kim et al. [3] compared intermediate results of simultaneous alumina-on-alumina bearing and alumina-on-highly cross-linked polyethylene bearing total hip arthroplasties. They observed that the mean annual penetration rate of highly cross-linked polyethylene (Marathon) was 0.06 ± 0.03 mm during the 5.6 years follow-up. No hip in either group had acetabular or femoral osteolysis. Furthermore, Kim et al. [4] reported cementless total hip arthroplasty with alumina-on-highly cross-linked polyethylene (Marathon) bearing in young patients with femoral head osteonecrosis. They found that the mean annual penetration rate was 0.05 ± 0.02 mm during the 8.5-years follow-up. Again, no hip had osteolysis. Recently, Kim et al. [5] reported polyethylene wear and osteolysis after cementless total hip arthroplasty with alumina-on-highly cross-linked polyethylene (Marathon) bearings in patients younger than 30 years of age. They demonstrated that the mean annual penetration rate of the polyethylene liner was 0.031 ± 0.04 mm during 10.8-years follow-up. No hip had osteolysis. Bitsch et al. [36] reported the mean annual femoral head penetration was 0.031 mm in the hips with a cobalt-chrome-on-Marathon highly cross-linked polyethylene liner. Osteolysis was not observed in any hip in their series. Engh et al. [35] reported that the mean wear rate for cobalt-chrome-on-Marathon liner was 0.01 ± 0.12 mm per year. These data suggest that there was no significant difference in the annual penetration rate of highly cross-linked polyethylene between alumina and metallic head during short-term follow-up. The benefit of the alumina head remains to be seen in the longer follow-up. For all but four patients in our study, the penetration rate of Marathon highly cross-linked polyethylene was below the so-called “osteolysis threshold” (0.1 mm per year). No detectable osteolysis was observed on radiographs or CT images in any of the hips in our study, consistent with other studies [3–5, 9].
The first generation of highly cross-linked polyethylene bearings had reduced fatigue, tensile, and toughness properties [37]. In our series, no hip displayed polyethylene liner fracture. We believe that this was due to the use of an adequate thickness of acetabular polyethylene liner (thicker than 6.0 mm) and satisfactory positioning of the acetabular component.
There has been some concern that smaller wear particles are produced with highly cross-linked polyethylene than with conventional polyethylene, leading to higher functional biological activity [38, 39]. However, in our 12.4-years follow-up data, no evidence of acetabular or femoral osteolysis was observed. A longer follow-up is necessary to draw conclusions about the biological activity of highly cross-linked polyethylene.
There are several strengths of this study. First, specific coordination of surgical technique and implant use was possible throughout the study by enrolling patients from a single centre. Second, the follow-up time was sufficient to determine the prevalence of osteolysis and loosening. Third, the performance of this stem and ceramic-on-ceramic and ceramic-on-highly cross-linked polyethylene bearings was investigated in a group of active patients. Finally, activity level data were collected from the patients and could be analysed as a risk factor for failure.
There are some limitations of this study. Firstly, all the operations were performed by a single surgeon, who could have introduced bias into the interpretation of the data. However, our findings were similar to other published results [3, 4, 8, 9, 30–33, 35, 36, 40, 41]. The similarity of our results to those of other reports mitigates single-surgeon bias. Second, it is frequently difficult for a patient who has undergone a bilateral total hip arthroplasty to determine which hip is functioning better. Therefore, the Harris and WOMAC function scores should be interpreted with caution because it is difficult for patients to attribute functional status to a particular hip.
Our results on alumina-on-alumina ceramic or alumina-on-highly cross-linked polyethylene bearings in patients aged 50 years or less suggest that cementless acetabular and femoral components provide outstanding midterm fixation and substantial pain relief well into the second decade after surgery, providing a high rate of survivorship without osteolysis. Because the results of using an alumina-on-alumina ceramic and alumina-on-highly cross-linked polyethylene bearings were similar, alumina-on-highly cross-linked polyethylene bearing could replace the alumina-on-alumina ceramic to avoid the potential squeaking or clicking sound and acetabular ceramic liner fracture.
Footnotes
The study was approved by the institutional review board, and all patients provided informed consent. All authors have participated in research for this paper. This manuscript has not been submitted elsewhere for publication.
References
- 1.Dowd JE, Sychterz CJ, Young AM, Engh CA. Characterization of long-term femoral-head-penetration rates. Association with and prediction of osteolysis. J Bone Joint Surg Am. 2000;82(8):1102–1107. doi: 10.2106/00004623-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Elfick AP, Hall RM, Pinder IM, Unsworth A. Wear in retrieved acetabular components: effect of femoral head radius and patient parameters. J Arthroplasty. 1998;13(3):291–295. doi: 10.1016/S0883-5403(98)90174-7. [DOI] [PubMed] [Google Scholar]
- 3.Kim Y-H, Kim J-S, Choi Y-W, Kwon O-R. Intermediate results of simultaneous alumina-on-alumina bearing and alumina-on-highly cross-linked polyethylene bearing total hip arthroplasties. J Arthroplasty. 2009;24(6):885–891. doi: 10.1016/j.arth.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y-H, Choi Y-W, Kim J-S. Cementless total hip arthroplasty with alumina-on-highly cross-linked polyethylene bearing in young patients with femoral head osteonecrosis. J Arthroplasty. 2011;26(2):218–223. doi: 10.1016/j.arth.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 5.Kim Y-H, Park J-W, Patel C, Kim D-Y. Polyethylene wear and osteolysis after cementless total hip arthroplasty with alumina-on-highly cross-linked polyethylene bearings in patients younger than thirty tears of age. J Bone Joint Surg Am. 2013;95(12):1088–1093. doi: 10.2106/JBJS.L.01211. [DOI] [PubMed] [Google Scholar]
- 6.Kim YH. The results of a proximally-coated cementless femoral component in total hip replacement: a five- to 12-year follow-up. J Bone Joint Surg Br. 2008;90(3):299–305. doi: 10.1302/0301-620X.90B3.20096. [DOI] [PubMed] [Google Scholar]
- 7.Capello WN, D’Antonio JA, Feinberg JR, Manley MT, Naughton M. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty. 2008;23(7 Suppl):39–43. doi: 10.1016/j.arth.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Garvin KL, Hartman CW, Mangla J, Murdoch N, Martell JM. Wear analysis in THA utilizing oxidized zirconium and crosslinked polyethylene. Clin Orthop Relat Res. 2009;467(1):141–145. doi: 10.1007/s11999-008-0544-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Urban JA, Garvin KL, Boese CK, Bryson L, Pedersen DR, Callaghan JJ, Miller RK. Ceramic-on-polyethylene bearing surfaces in total hip arthroplasty. Seventeen to twenty-one-year results. J Bone Joint Surg Am. 2001;83(11):1688–1694. doi: 10.2106/00004623-200111000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Kress AM, Schmidt R, Holzwarth U, Forst R, Mueller LA. Excellent results with cementless total hip arthroplasty and alumina-on-alumina pairing: minimum ten-years follow-up. Int Orthop. 2011;35:195–200. doi: 10.1007/s00264-010-1150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamnouche D, Zaoui A, Zadegan F, Sedel L, Nizand R. Thirty years of experience with alumina-on-alumina bearings in total hip arthroplasty. Int Orthop. 2011;35:207–213. doi: 10.1007/s00264-010-1187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, Timotijevic S. Alumina-on-alumina ceramic versus metal-on-highly cross-linked polyethylene bearing in total arthroplasty: a comparative study. Int Orthop. 2010;34(8):1129–1135. doi: 10.1007/s00264-009-0899-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91(6):1344–1349. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 14.Keurentjes JC, Kulpers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008;466(6):1438–1443. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walter WL, Waters TS, Gillies M, Donohoo S, Kurtz SM, Ranawat AS, Hozack WJ, Tuke MA. Squeaking hips. J Bone Joint Surg Am. 2008;90(suppl4):102–111. doi: 10.2106/JBJS.H.00867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty. A five-year minimum follow-up study. J Bone Joint Surg Am. 2005;87(3):530–535. doi: 10.2106/JBJS.D.01753. [DOI] [PubMed] [Google Scholar]
- 17.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67(1):3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Reumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 20.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 21.Dorr LD. Total hip replacement using APR system. Tech Orthop. 1986;1:22–34. doi: 10.1097/00013611-198610000-00007. [DOI] [Google Scholar]
- 22.Kim Y-H, Kim VE. Uncemented porous-coated anatomic total hip replacement. Results at six years in a consecutive series. J Bone Joint Surg Br. 1993;75(1):6–13. doi: 10.1302/0301-620X.75B1.8421036. [DOI] [PubMed] [Google Scholar]
- 23.Kim Y-H, Kim J-S, Oh S-H, Kim J-M. Comparison of porous-coated titanium femoral stems with and without hydroxyapatite coating. J Bone Joint Surg Am. 2003;85(9):1682–1688. doi: 10.2106/00004623-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y-H, Kim J-S, Cho S-H. A comparison of polyethylene wear in hips with cobalt-chrome or zirconia heads. A prospective, randomized study. J Bone Joint Surg Br. 2001;83(5):742–750. doi: 10.1302/0301-620X.83B5.10941. [DOI] [PubMed] [Google Scholar]
- 25.Sutherland CJ, Wilde AH, Borden LS, Marks KE. A ten-year follow-up of one hundred consecutive Müller curved-stem total hip-replacement arthroplasties. J Bone Joint Surg Am. 1982;64(7):970–982. [PubMed] [Google Scholar]
- 26.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 27.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 28.Kaplan EL, Meier P. Nonparametric estimation from incomplete observation. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 29.Hyder N, Nevelos AB, Barabas TG. Cementless ceramic hip arthroplasties in patients less than 30 years old. J Arthroplasty. 1996;11(6):679–686. doi: 10.1016/S0883-5403(96)80006-4. [DOI] [PubMed] [Google Scholar]
- 30.Bizot P, Banallec L, Sedel L, Nizard R. Alumina-on-alumina total hip prostheses in patients 40 years of age or younger. Clin Orthop Relat Res. 2000;379:68–76. doi: 10.1097/00003086-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Garcia-Rey E, Cruz-Pardos A, Garcia-Cimbrelo E. Alumina-on-alumina total hip arthroplasty in young patients: diagnosis is more important than age. Clin Orthop Relat Res. 2009;467(9):2281–2289. doi: 10.1007/s11999-009-0904-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoon H-J, Yoo J-J, Yoon K-S, Koo K-H, Kim H-J. Alumina-on-alumina THA performed in patients younger than 30 years: a 10-year minimum followup study. Clin Orthop Relat Res. 2012;470(12):3530–3536. doi: 10.1007/s11999-012-2493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bierbaum BE, Nairus J, Kuesis D, Morrison JC, Ward D. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002;405:158–163. doi: 10.1097/00003086-200212000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Kim Y-H, Park J-W, Kim J-S. Cementless metaphyseal fitting anatomic total hip arthroplasty with a ceramic-on-ceramic bearing in patients thirty years of age or younger. J Bone Joint Surg Am. 2012;94(17):1570–1575. doi: 10.2106/JBJS.K.00697. [DOI] [PubMed] [Google Scholar]
- 35.Engh CA, Jr, Stepniewski AS, Ginn SD, Beykirch SE, Sychterz-Terefenko CJ, Hopper RH, Jr, Engh CA. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked Marathon and non-cross-linked Enduron polyethylene liners. J Arthroplasty. 2006;21(6 suppl 2):17–25. doi: 10.1016/j.arth.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 36.Bitsch RG, Loidolt T, Heisel C, Ball S, Schmalzried TP. Reduction of osteolysis with use of Marathon cross-linked polyethylene. A concise follow-up, at a minimum of five years, of a previous report. J Bone Joint Surg Am. 2008;90(7):1487–1491. doi: 10.2106/JBJS.F.00991. [DOI] [PubMed] [Google Scholar]
- 37.Bradford L, Baker D, Ries MD, Pruitt LA. Fatigue crack propagation resistance of highly crosslinked polyethylene. Clin Orthop Relat Res. 2004;429:68–73. doi: 10.1097/01.blo.0000150124.34906.34. [DOI] [PubMed] [Google Scholar]
- 38.Endo M, Tipper JL, Barton DC, Stone MH, Ingham E, Fisher J. Comparison of wear, wear debris and functional biological activity of moderately crosslinked and non-crosslinked polyethylenes in hip prostheses. Proc Inst Mech Eng H. 2002;216(2):111–122. doi: 10.1243/0954411021536333. [DOI] [PubMed] [Google Scholar]
- 39.Fisher J, McEwen HM, Tipper JL, Galvin AL, Ingram J, Kamali A, Stone MH, Ingham E. Wear, debris, and biologic activity of cross-linked polyethylene in the knee: benefits and potential concerns. Clin Orthop Relat Res. 2004;428:114–119. doi: 10.1097/01.blo.0000148783.20469.4c. [DOI] [PubMed] [Google Scholar]
- 40.Thomas GE, Simpson DJ, Mehmood S, Taylor A, McLardy-Smith P, Gill HS, Murray DW, Glyn-Jones S. The seven-year wear of highly cross-linked polyethylene in total hip arthroplasty: a double-blind, randomized controlled trial using radiostereometric analysis. J Bone Joint Surg Am. 2011;93(8):716–722. doi: 10.2106/JBJS.J.00287. [DOI] [PubMed] [Google Scholar]
- 41.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty. A randomized controlled trial. J Bone Joint Surg Am. 2009;91(4):773–782. doi: 10.2106/JBJS.H.00244. [DOI] [PubMed] [Google Scholar]