Abstract
Purpose
The purpose of this study was to evaluate the clinical efficacy of using the proximal fibular graft for partial wrist arthrodesis or arthroplasty after the resection of giant cell tumours of the distal radius.
Methods
Between February 2006 and August 2010, 14 patients (seven males, seven females; average age, 35.7 years) with grade II and III giant cell tumours of the distal radius were treated by tumour resection and autologous proximal fibular grafts to reconstruct the wrist in our hospital. Seven patients each were treated by wrist arthroplasty and partial wrist arthrodesis, and were followed up for 2.2–6.8 years (average, 3.9 years).
Results
All patients achieved primary healing. No tumour recurrence was observed during follow-up in any of the patients. No statistically significant difference in forearm rotation was observed between patients undergoing the two different treatments. However, wrist flexion-extension activities were significantly better and the wrist grip strengths were significantly worse in the arthroplasty group than in the arthrodesis group. The Musculoskeletal Tumour Society score did not significantly differ between the groups.
Conclusions
Overall, joint arthroplasty remains a favourable treatment with regard to the functional outcome for giant cell tumours of the distal radius; however, some of these patients may have a weaker grip strength. In comparison, partial wrist fusion appears to provide a durable and stable wrist with good long-term functional outcome.
Keywords: Giant cell tumours of the distal radius, Fibular graft, Arthrodesis or arthroplasty?
Introduction
The reconstruction of the distal radius following resection of giant cell tumours (GCTs) primarily includes arthroplasty and partial wrist arthrodesis; however, it remains unclear which procedure provides a better functional outcome.
It is well known that GCTs of the bone are relatively rare and typically benign; however, GCTs, can be aggressive and metastasise to the lungs. GCTs have been reported to occur in the distal radius in approximately 10 % of cases (range, 8–13 %) [1]. Local control of GCTs in the distal end of the radius and subsequent reconstruction are challenging because of the limited amount of surrounding soft tissue, the proximity of this region to adjacent neurovascular structures, and the juxta-articular location.
The primary aim in treating distal radius GCT is to remove the tumour completely and preserve the wrist. Treatment consists of either curettage or en bloc resection of the lesion with subsequent reconstruction. Surgical options include radial carpal joint reconstruction, partial arthrodesis, or total arthrodesis for reconstruction of extensive defects of the distal radius. Classically, in the case of small lesions (Campanacci grade I), curettage and bone grafting or cementing is preferred for preserving the adjacent wrist joint; however, for grade II and III lesions, these procedures are often associated with high recurrence rates. For large lesions with extensive cortical destruction and soft tissue extension or lesions with pathological fractures, resection and reconstruction of the distal radius are preferred [2]. Among the many methods used for the reconstruction of segmental distal radial defects after tumour resection, the most frequently used method is the vascularised or non-vascularised autogenous fibular graft, with the reconstruction procedures primarily including arthroplasty or partial wrist arthrodesis [3–5]. However, it is unclear which reconstruction procedure provides a better functional outcome.
In our study, we aimed to compare the clinical and radiographic outcomes between partial wrist arthrodesis (fibula-scapho-lunate arthrodesis) and wrist arthroplasty in a single institution.
Patients and methods
Patients
Using our bone and soft tissue tumour database, we identified 14 patients who were treated between February 2006 and August 2010 for GCT of the distal radius. We performed a retrospective cohort study with a prospective evaluation and comparison for two different groups of patients: seven patients who underwent arthroplasty and seven patients who received partial wrist arthrodesis. The course of the disease ranged from one month to two years with the major clinical symptoms including joint pain, swelling, and activity limitation. All patients were examined with standard radiographs, CT scans, and magnetic resonance imaging of the wrist to localise the extent of the tumour and the soft tissue component. CT scan of the chest and bone scan were performed to determine whether lung metastasis and multiple bone lesions were present before surgery. Prospective database records and individual patient charts were reviewed to obtain surgical data, including the incidence of nonunion and complications. Radiographs and functional evaluation from the preoperative, postoperative, and follow-up periods were reviewed for evidence of tumour recurrence, union, and functional outcomes.
Surgery techniques
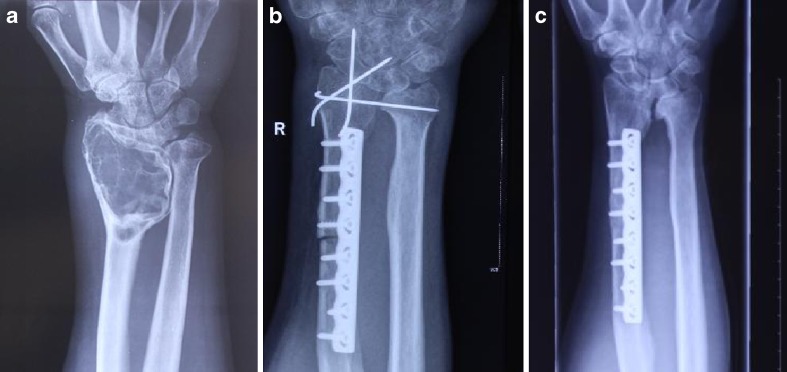
In the arthroplasty group, patients were suitably anaesthetised. Tumour excision and subsequent reconstruction for the distal radius were performed using the dorsal or volar surgical approach depending on the sites of radiographic thinning and breaches in the cortical bone. A biopsy tract was made in the initial incision. All tumours were removed by an intra-articular wide excision, and the radius was transected proximally. The ipsilateral fibula was approached through the standard direct lateral approach. The fibula was sectioned at the desired length depending on the defect created in the forearm after tumour resection. All grafts were fixed to the proximal radius with a dynamic compression plate or locked compression plate. Thereafter, additional stability in the radio-carpal joint was achieved by passing a K-wire through the fibula and into the proximal carpal row with the wrist in the functional position. Another K-wire was then passed from the fibula to the ulna to stabilise the fibulo-ulnar articulation, and the preserved fibrous capsule was reattached to the fibular head in cases undergoing arthroplasty (Fig. 1). After fixation was attained, in cases with a vascularised fibula, the peroneal artery was anastomosed with the radial artery, and the peroneal vein with the cephalic vein.
Fig. 1.
X-ray films of a 19-year-old male patient with a giant cell tumour in the right distal radius. a Before the operation. b Immediately after wrist arthroplasty. c Three years after the operation
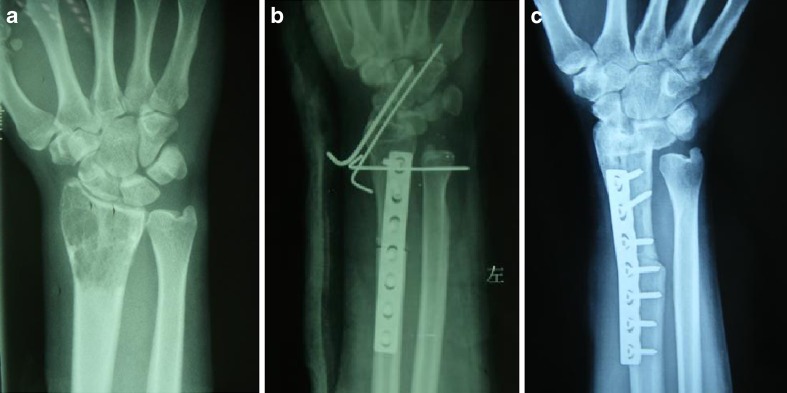
In the arthrodesis group, the process of removing the tumour and exposing the fibula was the same as that for the arthroplasty. Thereafter, it was necessary to remove the articular cartilage surface of the fibula-scapho-lunate, and arthrodesis for radiocarpal articulation was performed by fixation with two K-wires with the wrist in a functional position. In addition, a K-wire was passed from the fibula to the ulna to stabilise the fibulo-ulnar articulation (Fig. 2). After fixation, the fibular branch of the inferior lateral genicular artery and the accompanying vein were anastomosed to the superficial branch of the radial artery in the two cases involving a vascularised fibular graft.
Fig. 2.
X-ray films of a 38-year-old male patient with left distal radius giant cell tumour. a Before the operation. b Immediately after partial wrist arthrodesis. c Three years after the operation
Postoperative management
An above-elbow cast was used to protect the wrist for six weeks. The K-wires were removed approximately two months after surgery for all patients; however, the K-wires through the wrist in the arthrodesis patients were removed when bone healing could be observed in the wrist radiographs. After removal of the K-wires, gentle active and assisted wrist exercises were initiated; these exercises were gradually increased in intensity depending on the tolerance and progress. No heavy activity was allowed for one year. During the first year, plain radiographs of the forearm were repeated every three months to evaluate the union and detect any recurrence of the tumour, or graft-related complications. Follow up was then conducted at intervals of six months in the second and third years and then annually thereafter. The follow-up duration of the arthroplasty and arthrodesis groups was 2.2–6.8 years, and 3.0–4.6 years, respectively.
Efficacy evaluation
All patients were assessed clinically and radiographically. The functional outcomes were analysed using the Musculoskeletal Tumour Society (MSTS) functional classification [6]. The range of movements of the forearm and wrist was assessed. The grip strength was measured with a dynamometer, and the range of motion was measured with a goniometer, and these measurements compared to those of the contralateral wrists by Dr. CL Zhang. Radiographs were obtained of the operated forearm and wrist and were used to study radiographic union, tumour recurrence, and subluxation of the radiocarpal and distal radioulnar joints.
Statistical analysis
Data are expressed as the means ± SD, percentages, or the number of patients for each group. The quantitative data were analysed by the Student’s t-test, whereas the qualitative data were analysed by Fisher’s exact test using SAS statistics software (Version 9.13). A P value of <0.05 was considered statistically significant.
Results
A summary of the patients’ profiles and results is shown in Table 1. The patients (seven males, seven females) had an average age of 35.7 years (range, 19–55 years). There were three farmers, three workers, three housewives, two self-employed, one student, one officer, and one physical education teacher. The lesions were on the left side in four patients and on the right side in ten patients. There were nine cases with primary lesions and five cases of lesion recurrence. Seven patients were classified with grade II tumours; and seven patients were classified with grade III tumours, according to Campanacci’s radiological grading method [7]. Of the nine primary cases, initial preoperative CT-guided biopsy confirmation of GCT was performed in seven cases. The results of the preoperative imaging of the remaining cases were in line with the typical findings for GCT. We performed a frozen section diagnosis during the surgery to confirm the biopsy diagnosis. After confirming the diagnosis, we continued the procedure according to the preoperative plan. No evidence of metastatic disease was found in any of the patients at the time of diagnosis. Among the 14 patients, seven were treated by partial wrist arthrodesis with an autogenous fibular graft (two were treated with a vascularised fibula), and seven were treated by arthroplasty (one was treated with a vascularised fibula).
Table 1.
Patient profiles and functional results
| Patients | Gender | Age (y) | Surgical method | Grade | Fibular length (cm) |
Follow up (y) |
Recurrence | Flexion-extension (degrees) |
Pronation-supination (degrees) |
Grip (percent contralateral side) | MSTS score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 55 | arthroplasty | II | 9.0 | 5.5 | No | 65 | 145 | 82.4 % (28/34) | 27 |
| 2 | Male | 25 | arthroplasty | III | 7.0 | 5.4 | No | 80 | 150 | 65.8 % (25/35) | 26 |
| 3 | Female | 35 | arthroplasty | II | 8.0 | 6.8 | No | 70 | 145 | 50 % (17/34) | 27 |
| 4 | Male | 48 | arthroplasty | II | 6.0 | 3.1 | No | 100 | 135 | 67.5 % (27/40) | 25 |
| 5 | Female | 40 | arthroplasty | III | 9.0 | 2.2 | No | 47 | 110 | 41.4 % (12/29) | 23 |
| 6 | Female | 48 | arthroplasty | III | 9.0 | 2.6 | No | 67 | 155 | 54.1 % (20/37) | 26 |
| 7 | Female | 49 | arthroplasty | III | 8.0 | 2.8 | No | 72 | 140 | 52.9 % (18/34) | 27 |
| 8 | Female | 19 | arthrodesis | III | 7.5 | 4.1 | No | 50 | 140 | 69.4 % (25/36) | 25 |
| 9 | Male | 43 | arthrodesis | II | 8.0 | 3.4 | No | 64 | 125 | 82.6 % (38/46) | 25 |
| 10 | Female | 26 | arthrodesis | II | 6.5 | 4.6 | No | 44 | 127 | 71.4 % (20/28) | 25 |
| 11 | Female | 45 | arthrodesis | III | 7.0 | 4.4 | No | 62 | 103 | 77.1 % (27/35) | 26 |
| 12 | Male | 34 | arthrodesis | II | 6.5 | 4.0 | No | 51 | 145 | 77.6 % (38/49) | 26 |
| 13 | Male | 25 | arthrodesis | II | 7.0 | 4.0 | No | 60 | 118 | 77.4 % (29/39) | 25 |
| 14 | Male | 38 | arthrodesis | III | 7.0 | 3.0 | No | 60 | 135 | 80 % (36/45) | 27 |
MSTS Musculoskeletal Tumour Society
All patients achieved primary healing of the incision and were followed up for an average period of 3.9 years (range, 2.2–6.8 years). No bone absorption or articular surface collapse of the fibular head was noted. In the arthroplasty group, two cases of wrist subluxation and four cases of degenerative changes were observed; all of these patients had no pain but had functional impairment with moderate activity. There was one case of radial fibula fracture in the arthrodesis group following removal of the plate after approximately two years because of a slight trauma. This patient was treated with repeat LCP fixation, and bone union was observed after approximately six months. All patients had good finger activity, with the exception of an arthroplasty patient with limited movement in the small finger due to adhesion of the small finger flexor tendon. In our study, there were also some related complications, such as two cases of wrist volar subluxation and four cases of wrist degenerative changes. No local recurrence and no distance metastases were observed in either group. None of the patients were dissatisfied in terms of the shape and appearance of the wrist.
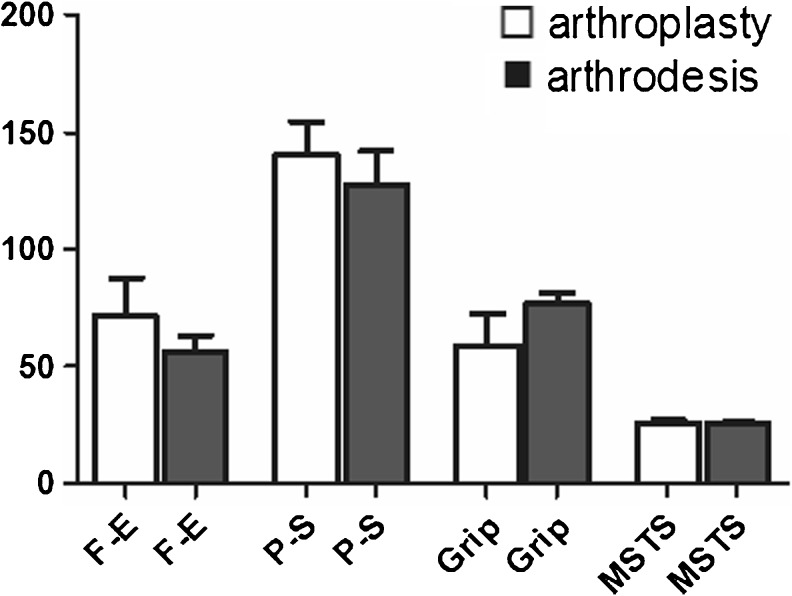
The average range of motion of the wrist in the arthroplasty group was 71.6 ± 16.1° of total flexion-extension, and 140 ± 14.7° of total pronation-supination. The average percentage of grip strength was 59.2 % ± 13.7 % compared with that of the contralateral side. The MSTS score was an average of 25.9 ± 1.46. In the arthrodesis group, the average range of motion of the wrist was 55.9 ± 7.5° of total flexion-extension, and 127.6 ± 14.2° of total pronation-supination. The percentage of the average grip strength was 76.5 % ± 4.6 %. The average MSTS score was 25.6 ± 0.78. No significant difference in forearm rotation was found between the two groups. With regard to the flexion-extension function, the arthroplasty group was superior to the arthrodesis group (p < 0.05). In contrast the arthrodesis group had significantly greater grip strength than the arthroplasty group (p < 0.05). However, statistical significance was not observed in relation to the MSTS score (Table 2, Fig. 3).
Table 2.
Postoperative functional comparison between the arthrodesis and arthroplasty groups
| Data | Arthroplasty | Arthrodesis | Statistical value |
|---|---|---|---|
| Patients | 7 | 7 | -- -- |
| Gender (m/f) | 4/3 | 3/4 | χ 2 = 0.2857, P = 1.000 |
| Age | 42.9 ± 10.2 | 32.9 ± 9.8 | t = 1.87, P = 0.087 |
| Grade (II/III) | 4/3 | 3/4 | χ 2 = 0.2857, P = 1.000 |
| Fibular length (cm) | 8 ± 1.15 | 7.07 ± 0.53 | t = 1.93, P = 0.078 |
| Time of follow up (y) | 4.06 ± 1.80 | 3.93 ± 0.56 | t = 0.18, P = 0.860 |
| Flexion-extension | 71.6 ° ± 16.1° | 55.9° ± 7.5° | t = 2.34, P = 0.037 |
| Pronation-supination | 140° ± 14.7° | 127.6° ± 14.2° | t = 1.61, P = 0.134 |
| Grip strength percentage | 59.2 % ± 13.7 % | 76.5 % ± 4.6 % | t = −3.18, P = 0.014 |
| MSTS score | 25.9 ± 1.46 | 25.6 ± 0.78 | t = 0.45, P = 0.657 |
MSTS Musculoskeletal Tumor Society
Fig. 3.
Statistical histogram of F-E, P-S, Grip, and MSTS for the two study groups. F-E = range of flexion-extension, P-S = range of pronation-supination
Discussion
The distal radius is the third most common site for giant cell lesions next to the distal femur and the proximal tibia [8]. A high rate of local recurrence is observed after local treatment by intralesional curettage and/or cauterisation with phenol [2, 8–11]. Moreover, this treatment cannot be used satisfactorily in larger lesions with eggshell thin cortices or late presentations in which the tumour has spread to adjacent soft tissues. Compared to intralesional procedures, en-bloc resection has been uniformly reported to yield better results in terms of local recurrence [4, 12]. The selection of the best treatment for GCTs is controversial, but several clinicians have reported basing their decisions on the radiographic grade and the staging system [8, 13]. Thorough curettage combined with cryosurgery and the packing of bone cement is generally considered the standard treatment for grade I lesions, and can preserve good joint function [8, 14]. For grade II or III lesions, or recurrent lesions after curettage, en bloc resection is required because the tumours can only be controlled by wide excision [15, 16]. However, large bone defects can result after wide resection of the tumour. Hence, reconstruction of the distal radius is a challenge with regard to regaining normal function in the hand with minimal complications. A number of studies have reported on the reconstruction of segmental distal radial defects after tumour resection by using a non-vascularised or vascularised autogenous fibular graft; the reconstruction procedures have mainly included arthroplasty [2, 4, 17–21], partial wrist arthrodesis [3, 22, 23] and complete wrist arthrodesis [24–26].
Because of the anatomical similarity of the fibular head and distal radius, arthroplastic reconstruction of the distal radius via the proximal end of the fibula is frequently used, and the aesthetic and functional results are often satisfactory. Ono et al. [15] suggested that performing wrist arthroplasty with a vascularised fibular head graft is the best surgical approach in the treatment of grade II GCT of the distal radius. Moreover, Saini et al. [17] reported a satisfactory clinical outcome after reconstructing bone defects with a non-vascularised proximal fibula graft in 12 cases of GCT of the distal radius after tumour resection. In our study, all of the fibulas survived successfully in the arthroplasty group. The average range of motion of the wrist and the MSTS scores were satisfactory. However, the average percentage of grip strength (59.2 % ± 13.7 %) was lower compared to those of other reports. In addition, several studies have reported that wrist arthroplasty with a fibular graft was associated with several surgical complications. The main complications included progressive degenerative changes, bone resorption, secondary bone collapse, subluxation, joint instability, and poor grip strength. The main causes underlying these complications was an incongruity between the fibular head and the proximal carpal row [3, 15, 27].
There are three different types of partial arthrodesis—radiolunate, radioscaphoid, and radioscapholunate. Of the three fusion types, radioscapholunate fusion has been shown to have the most biomechanically similar behaviour and the least change in the midcarpal joint force distribution, which is combined with an evenly distributed stress distribution on the radius, and the greatest stability of the carpus as compared with a healthy wrist [28]. Brigstocke et al. [29] recently reported that arthrodesis of the radiocarpal joint instead of the midcarpal joint will allow better wrist function during most activities of daily living by preserving the dart thrower’s motion—that is, the plane of global wrist motion used during most activities of daily living. Thus, in our study, partial wrist arthrodesis by fibula-scapho-lunate arthrodesis also makes it possible to obtain a stable and functional wrist because the range of movement in the mediocarpal joint is preserved. Although the range of movement is limited, it is able to meet the basic needs of life and work. Bickert et al. [30] introduced the fibulo-scapho-lunate arthrodesis for two patients suffering from malignant tumours of the distal radius, with excellent functional and radiological outcomes. Moreover, partial wrist arthrodesis is also widely used in reconstructing bone defects after resection of a GCT of the distal radius. This procedure preserves partial wrist function, and the surgical complications are relatively rare; moreover, the clinical efficacy is satisfactory [22, 23]. However, wrist partial arthrodesis also has some associated complications, such as delayed union, nonunion, fatigue or stress fractures [31]. In our study, the seven arthrodesis cases achieved better or similar functional results compared to those in the previously published series. The range of movement in the wrist was limited (55.9 ± 7.5° of total flexion-extension), but was sufficient to accomplish the majority of daily activities without discomfort. The complications of bone graft non-union and stress fractures also occurred.
Because of the relative rarity of GCT in the distal radius, very few studies [3, 15, 27] have compared the clinical results between arthroplasty and partial wrist arthrodesis using an autogenous fibular graft for the distal radial resection. According to these studies, the functional results were quite similar. Nine articles (Table 3) were closely relevant to our study, and provided data for MSTS, grip strength, and flexion-extension. Our findings showed that arthroplasty was superior to partial arthrodesis in terms of flexion-extension function, whereas the partial arthrodesis cases were superior to arthroplasty in terms of grip strength.
Table 3.
Functional results for distal radius reconstruction with arthroplasty or partial wrist arthrodesis using autogenous fibular graft in the recent literature
| Authors | Reconstruction | Number | Mean follow-p | MSTS | Flexion/extension | Pro-/supination | Grip |
|---|---|---|---|---|---|---|---|
| Saini et al. 2011 [17] | Arthroplasty | 12 | 6 years | NA | 73 | 89 | 71 % |
| Jaminet et al. 2012 [23] | Arthrodesis | 3 | 6–60 months | NA | 46 | 143 | 73 % |
| Peng-Fei and Yu-Hua 2011 [4] | Arthroplasty | 18 | NA | 26 | 110 | 47 | 75 % |
| Minami A et al. 2002 [3] | Arthrodesis | 2 | 3.2–6.6 years | 26 | 70 | 140 | 90 % |
| Bassiony et al. 2009 [18] | Arthroplasty | 10 | 3.9 years | 28 | NA | NA | NA |
| Saikia et al. 2010 [21] | Arthroplasty | 24 | 6.6 years | 26 | 88 | 98 | 67 % |
| Chadha et al. 2010 [19] | Arthroplasty | 9 | 4.7 years | NA | 70 | 90 | 50 % |
| Chung et al. 2012 [16] | Arthroplasty | 12 | 6.26 years | 26.4 | 73.1 | 102.9 | 57.25 % |
NA not applicable, MSTS Musculoskeletal Tumor Society
When the outcomes of our patients, as assessed through follow up, are compared with the reported literature, it can be noted that both proximal fibular graft by wrist arthroplasty and partial arthrodesis can both achieve satisfactory clinical results in the reconstruction of bone defects after resection of a GCT of the distal radius. Minami et al. [3] reported the treatment of four cases of distal radius GCT with free vascularised fibulas. Two cases underwent partial wrist arthrodesis, whereas the other two cases underwent wrist arthroplasty; the functional results of the arthrodesis were superior to those of arthroplasty. To date, little information is available on the two surgical methods in a control study. In our study, no significant difference was observed in the forearm rotation between the two groups. Moreover, the arthroplasty group was superior to the arthrodesis group in flexion-extension function, while the arthrodesis group was better than the arthroplasty group in grip strength. Finally, we compared the difference in MSTS scores between the two groups and found them to be similar.
In our study, the results suggest that tumour resection and use of an autologous proximal fibular graft to reconstruct the wrist is a good technique for the treatment of distal radius GCT. Overall, joint arthroplasty remains a favourable treatment with regard to functional outcome for GCTs of the distal radius; however, some of these patients may have weaker grip strength. In comparison, partial wrist fusion provides a durable and stable wrist with a good long-term functional outcome. Muramatsu et al. [25] recommended arthroplasty for patients who were not involved in heavy manual labour, and fibula-scapho-lunate (FSL) arthrodesis for young patients involved in high-energy activities in order to obtain a stable and powerful wrist. It is suggested that the decision to perform partial arthrodesis or arthroplasty should be based on the patient’s career, the need for activity, and stability of the wrist.
References
- 1.Liu YP, Li KH, Sun BH. Which treatment is the best for giant cell tumors of the distal radius? A meta-analysis. Clin Orthop Relat Res. 2012;470:2886–2894. doi: 10.1007/s11999-012-2464-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng CY, Shih HN, Hsu KY, et al. Treatment of giant cell tumor of the distal radius. Clin Orthop Relat Res. 2001;383:221–228. doi: 10.1097/00003086-200102000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Minami A, Kato H, Iwasaki N. Vascularized fibular graft after excision of giant-cell tumor of the distal radius: wrist arthroplasty versus partial wrist arthrodesis. Plast Reconstr Surg. 2002;110:112–117. doi: 10.1097/00006534-200207000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Peng-Fei S, Yu-Hua J. Reconstruction of distal radius by fibula following excision of grade III giant cell tumour: follow-up of 18 cases. Int Orthop. 2011;35:577–580. doi: 10.1007/s00264-010-0967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puloski SK, Griffin A, Ferguson PC, et al. Functional outcomes after treatment of aggressive tumors in the distal radius. Clin Orthop Relat Res. 2007;459:154–160. doi: 10.1097/BLO.0b013e318059b91f. [DOI] [PubMed] [Google Scholar]
- 6.Enneking WF, Dunham W, Gebhardt MC, et al. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 7.Campanacci M. Giant-cell tumor and chondrosarcomas: grading, treatment and results (studies of 209 and 131 cases) Recent Results Cancer Res. 1976;54:257–261. doi: 10.1007/978-3-642-80997-2_22. [DOI] [PubMed] [Google Scholar]
- 8.Campanacci M, Baldini N, Boriani S, et al. Giant-cell tumor of bone. J Bone Joint Surg Am. 1987;69:106–114. [PubMed] [Google Scholar]
- 9.Gitelis S, Mallin BA, Piasecki P, et al. Intralesional excision compared with en bloc resection for giant-cell tumors of bone. J Bone Joint Surg Am. 1993;75:1648–1655. doi: 10.2106/00004623-199311000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Malek F, Krueger P, Hatmi ZN, et al. Local control of long bone giant cell tumour using curettage, burring and bone grafting without adjuvant therapy. Int Orthop. 2006;30:495–498. doi: 10.1007/s00264-006-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oh JH, Yoon PW, Lee SH, et al. Surgical treatment of giant cell tumour of long bone with anhydrous alcohol adjuvant. Int Orthop. 2006;30:490–494. doi: 10.1007/s00264-006-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lackman RD, McDonald DJ, Beckenbaugh RD, et al. Fibular reconstruction for giant cell tumor of the distal radius. Clin Orthop Relat Res. 1987;218:232–238. [PubMed] [Google Scholar]
- 13.Enneking WF. A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res. 1986;204:9–24. [PubMed] [Google Scholar]
- 14.Eckardt JJ, Grogan TJ. Giant cell tumor of bone. Clin Orthop Relat Res. 1986;204:45–58. [PubMed] [Google Scholar]
- 15.Ono H, Yajima H, Mizumoto S, et al. Vascularized fibular graft for reconstruction of the wrist after excision of giant cell tumor. Plast Reconstr Surg. 1997;99:1086–1093. doi: 10.1097/00006534-199704000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Chung DW, Han CS, Lee JH, et al. Outcomes of wrist arthroplasty using a free vascularized fibular head graft for Enneking stage II giant cell tumors of the distal radius. Microsurgery. 2012;33:112–119. doi: 10.1002/micr.22028. [DOI] [PubMed] [Google Scholar]
- 17.Saini R, Bali K, Bachhal V, et al. En bloc excision and autogenous fibular reconstruction for aggressive giant cell tumor of distal radius: a report of 12 cases and review of literature. J Orthop Surg Res. 2011;6:14. doi: 10.1186/1749-799X-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bassiony AA. Giant cell tumour of the distal radius: wide resection and reconstruction by non-vascularised proximal fibular autograft. Ann Acad Med Singap. 2009;38:900–904. [PubMed] [Google Scholar]
- 19.Chadha M, Arora SS, Singh AP. Autogenous non-vascularized fibula for treatment of giant cell tumor of distal end radius. Arch Orthop Trauma Surg. 2010;130:1467–1473. doi: 10.1007/s00402-010-1059-6. [DOI] [PubMed] [Google Scholar]
- 20.Rtaimate M, Laffargue P, Farez E, et al. Reconstruction of the distal radius for primary bone tumors using a non-vascularized fibular graft (report of 4 cases) Chir Main. 2001;20:272–279. doi: 10.1016/S1297-3203(01)00046-4. [DOI] [PubMed] [Google Scholar]
- 21.Saikia KC, Borgohain M, Bhuyan SK, et al. Resection-reconstruction arthroplasty for giant cell tumor of distal radius. Indian J Orthop. 2010;44:327–332. doi: 10.4103/0019-5413.65134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray JA, Schlafly B. Giant-cell tumors in the distal end of the radius. Treatment by resection and fibular autograft interpositional arthrodesis. J Bone Joint Surg Am. 1986;68:687–694. [PubMed] [Google Scholar]
- 23.Jaminet P, Rahmanian-Schwarz A, Pfau M, et al. Fibulo-scapho-lunate arthrodesis after resection of the distal radius for giant-cell tumor of the bone. Microsurgery. 2012;32:458–462. doi: 10.1002/micr.21971. [DOI] [PubMed] [Google Scholar]
- 24.Sheth DS, Healey JH, Sobel M, et al. Giant cell tumor of the distal radius. J Hand Surg [Am] 1995;20:432–440. doi: 10.1016/S0363-5023(05)80102-9. [DOI] [PubMed] [Google Scholar]
- 25.Muramatsu K, Ihara K, Azuma E, et al. Free vascularized fibula grafting for reconstruction of the wrist following wide tumor excision. Microsurgery. 2005;25:101–106. doi: 10.1002/micr.20088. [DOI] [PubMed] [Google Scholar]
- 26.El-Kazzi W, Robert C, Mouraux D, et al. Arthrodesis of the wrist with bone autograft and Hoffmann external fixation. J Hand Surg Eur. 2012;37:149–154. doi: 10.1177/1753193411416565. [DOI] [PubMed] [Google Scholar]
- 27.Usui M, Murakami T, Naito T, et al. Some problems in wrist reconstruction after tumor resection with vascularized fibular-head graft. J Reconstr Microsurg. 1996;12:81–88. doi: 10.1055/s-2007-1006458. [DOI] [PubMed] [Google Scholar]
- 28.Gislason MK, Stansfield B, Bransby-Zachary M, et al. Load transfer through the radiocarpal joint and the effects of partial wrist arthrodesis on carpal bone behaviour: a finite element study. J Hand Surg Eur. 2012;37:871–878. doi: 10.1177/1753193412441761. [DOI] [PubMed] [Google Scholar]
- 29.Brigstocke GH, Hearnden A, Holt C et al (2012) In-vivo confirmation of the use of the dart thrower’s motion during activities of daily living. J Hand Surg Eur. Oct 11. [Epub ahead of print] [DOI] [PubMed]
- 30.Bickert B, Heitmann C, Germann G. Fibulo-scapho-lunate arthrodesis as a motion- preserving procedure after tumour resection of the distal radius. J Hand Surg (Br) 2002;27:573–576. doi: 10.1054/jhsb.2002.0829. [DOI] [PubMed] [Google Scholar]
- 31.Zachary SV, Stern PJ. Complications following AO/ASIF wrist arthrodesis. J Hand Surg [Am] 1995;20:339–344. doi: 10.1016/S0363-5023(05)80037-1. [DOI] [PubMed] [Google Scholar]