Abstract
There has been increasing interest in adjusting CT radiation dose data for patient body size. A method for automated computation of the abdominal effective diameter of a patient from a CT image has previously only been tested in adult patients. In this work, we tested the method on a set of 128 pediatric patients aged 0.8 to 12.9 years (average 8.0 years, SD = 3.7 years) who had CT abdomen/pelvis exams performed on a Toshiba Aquilion 64 scanner. For this set of patients, age-predicted abdominal effective diameter extrapolated based on data from the International Commission on Radiation Units and Measurements was a relatively poor predictor of measured effective diameter. The mean absolute percentage error between the CTDI normalization coefficient calculated from a manually measured effective diameter and the coefficient determined by age-predicted effective diameter was 12.3 % with respect to a 32 cm phantom (range 0.0–52.8 %, SD 8.7 %) and 12.9 % with respect to a 16 cm phantom (range 0.0–56.4 %, SD 9.2 %). In contrast, there is a close correspondence between the automated and manually measured patient effective diameters, with a mean absolute error of 0.6 cm (error range 0.2–1.3 cm). This correspondence translates into a high degree of correspondence between normalization coefficients determined by automated and manual measurements; the mean absolute percentage error was 2.1 % with respect to a 32 cm phantom (range 0.0–8.1 %, SD = 1.4 %) and 2.3 % with respect to a 16 cm phantom (range 0.0–9.3 %, SD = 1.6 %).
Keywords: Computed tomography, Radiation dose, Body imaging, Quality control, Image analysis, Pediatrics
Introduction
Monitoring CT radiation dose in pediatric patients is of particular concern, since radiation exposure in children poses greater lifetime cancer risks than in adults [1]. However, CT radiation dose is typically reported in terms of scanner radiation output related to energy imparted to a reference phantom, which may be either 16 or 32 cm in diameter in pediatric body imaging. Since pediatric body size may vary considerably relative to the size of the reference phantom, accurate dose estimates require normalization with respect to body size.
The American Association of Physicists in Medicine (AAPM) task group 204 reported a method in 2011 for adjusting computed tomography dose index (CTDI) values based on the effective diameter of the patient, where effective diameter is defined as the diameter of the circle whose area is the same as the patient cross section [2, 3]. The effective diameter can be estimated manually as the geometric mean of the lateral and anterior–posterior dimensions of the patient, assuming an elliptical patient cross-section.
Since measurement of these dimensions may be laborious or unavailable in a dose database, an alternative method of estimating effective diameter was provided by the AAPM task group, based on extrapolation of pediatric body size parameters from the International Commission on Radiation Units and Measurements (ICRU) report 74 [4]. Significant variation in patient size with respect to age has been demonstrated, however [5, 6].
We have developed a method of rapid automated estimation of abdominal effective diameter, which has been shown to be accurate in adults [7]. In this report, we hypothesize that automated abdominal effective diameter measurements in children are accurate and may produce dose normalization coefficients that are significantly different from those obtained from age-dependent body size estimates.
Materials and Methods
Institutional review board approval was obtained for the data collection and analysis in this study. A retrospective set of 128 patients aged 0.8 to 12.9 years (average 8.0 years, SD = 3.7 years) was identified, each of whom had a CT abdomen/pelvis exam performed between 2009 and 2012. All patients were scanned on a Toshiba Aquilion 64 scanner. For each patient, a representative axial image of the abdomen centered at the umbilicus was identified by a single abdominal radiologist, and the lateral and anterior–posterior dimensions of the patient cross-section were manually measured on the Fuji Synapse PACS (Fig. 1); the effective diameter was computed from these measurements.
Fig. 1.
Manual measurements of lateral and AP dimensions of the abdomen at the level of the umbilicus used to calculate abdominal effective diameter
We have previously implemented and reported a simple automated effective diameter estimation algorithm [7]. For a given image, we enumerate the number of pixels in the image whose Hounsfield unit value exceeds a threshold of −500 HU and multiply the count by the area of a single pixel to estimate the area of the patient cross-section. The calculated effective diameter is given by the diameter of the circle whose area is the same as this cross section. Specifically, the estimated effective diameter D is given by
 |
1 |
where px and py are the x and y dimensions of a single pixel, and {HU(p) > t} is the set of all pixels p where the Hounsfield unit value exceeds the threshold t. This calculation was performed at the image centered at the umbilicus. Since the determination of the umbilical slice is not easily automated, the calculation was also performed in the middle slice of each study.
Subsequently, the age in fractional years was computed for each patient, and an age-dependent effective diameter was calculated using exponential equation A-3 in Appendix A of AAPM report 204, i.e.,
 |
2 |
where y is the effective diameter in centimeters, x is age in years, a = 18.788598, b = 0.19486455, c = −1.060056, and d = −7.6244784 [2].
Finally, for each measured, calculated, and age-dependent effective diameter, a CT dose normalization coefficient was calculated using coefficients for both 16 and 32 cm phantoms in exponential equation A-1 in Appendix A of AAPM Report 204, i.e.,
 |
3 |
where y is a normalized dose coefficient, x is the effective diameter in centimeters, a = 3.704369 and b = 0.03671937 for the 32 cm phantom, and a = 1.874799 and b = 0.03871313 for the 16 cm phantom [2].
Results
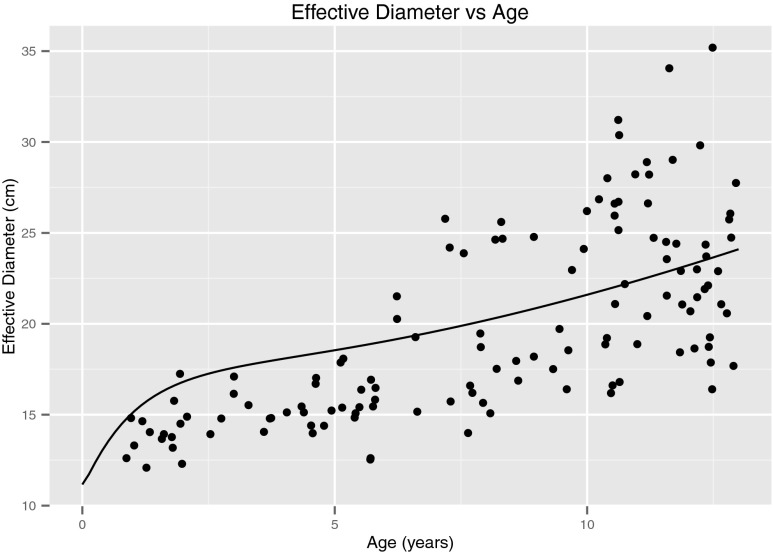
In our patient set, the measured abdominal effective diameter varied significantly with age. Most patients below the age of 6 had abdominal effective diameters less than predicted by the extrapolated ICRU curve. From ages 6 to 12, patients demonstrated a wide range of effective diameters both above and below the ICRU curve (Fig. 2). For instance, the measured abdominal effective diameter for 12-year-old patients ranged from 16.4 to 35.1 cm (mean 22.7 cm, SD 4.4 cm), with a predicted effective diameter of 23.2 cm.
Fig. 2.
Measured effective diameter versus age. The curve represents the age-predicted effective diameter based on extrapolated International Commission on Radiation Units and Measurements data, as given by exponential equation A-3 in Appendix A of AAPM report 204 [2]
The effect of this variance in measured effective diameter with respect to age was similar in magnitude for normalization coefficient calculations with respect to either a 32 or a 16 cm phantom. For a 32 cm phantom (Fig. 3a), the mean absolute percentage error between the coefficient calculated by a measured effective diameter and the coefficient calculated by the ICRU curve extrapolation was 12.3 % (range 0.0–52.8 %, SD 8.7 %). For a 16 cm phantom (Fig. 3b), the corresponding mean absolute percentage error of the normalization coefficient was 12.9 % (range 0.0–56.4 %, SD 9.2 %).
Fig. 3.
CTDI normalization coefficient based on measured effective diameter versus age. The curve represents normalization coefficients derived from the ICRU curve plotted in Fig. 2. a Normalization coefficients with respect to a 32 cm phantom. b Normalization coefficients with respect to a 16 cm phantom
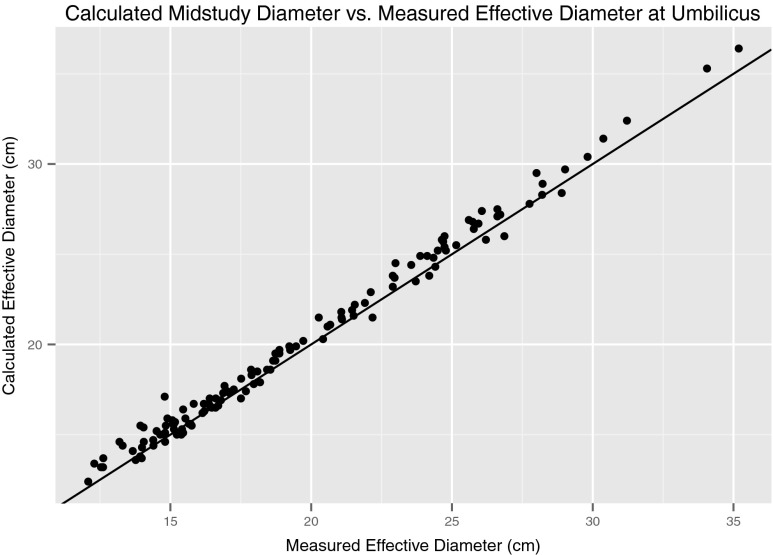
Automated measurements of pediatric abdominal effective diameter demonstrated high accuracy. For calculations taken at the same slice of the manual measurements (i.e., at the umbilicus), the mean absolute error was 0.6 cm (range 0.2–1.3 cm, SD = 0.3 cm). Error levels for calculations taken at the middle slice of the study (a position that can be determined without image analysis) compared to the manual measurements at the umbilicus were similar (Fig. 4); the mean absolute error was 0.6 cm (range 0.0–1.5 cm, SD = 0.4 cm).
Fig. 4.
Calculated diameter in the mid-study slice versus measured diameter at the umbilicus. The line of identity is plotted
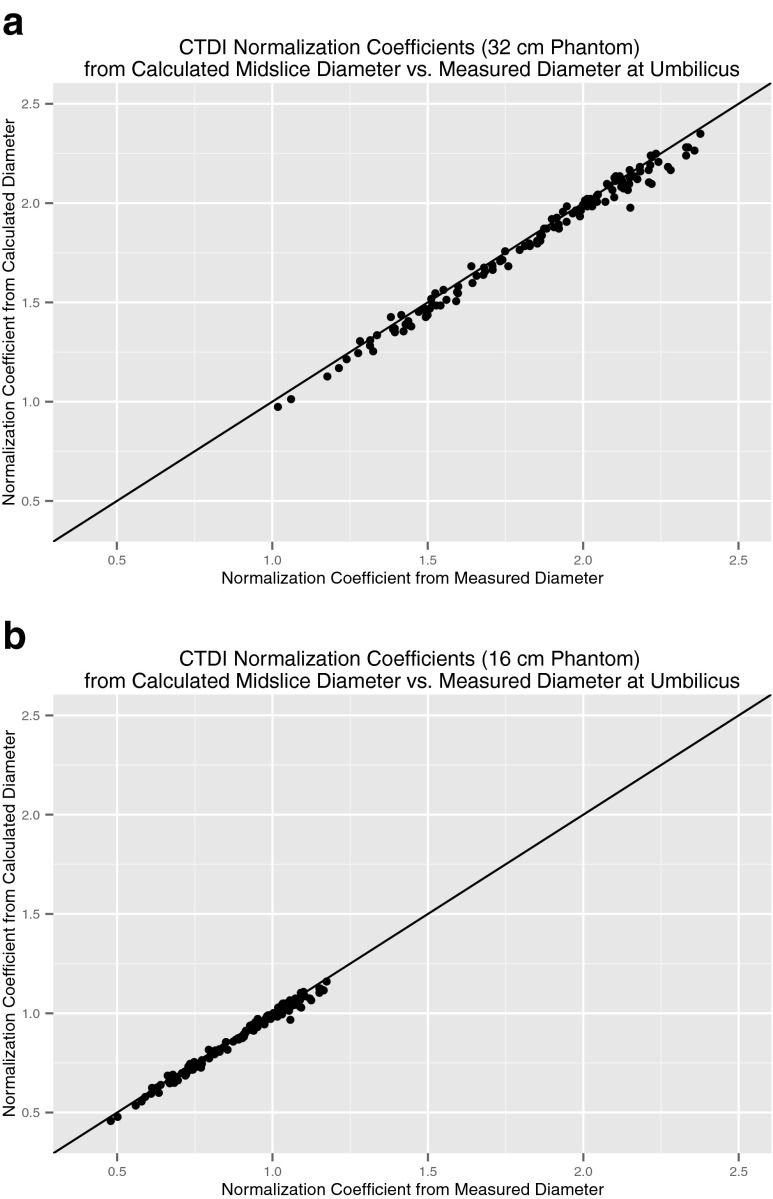
This accuracy in estimating effective diameter translated into high accuracy for the calculated normalization coefficients. For normalization coefficients with respect to the 32 cm phantom (Fig. 5a), the mean absolute percentage error was 2.1 % (range 0.0–8.1 %, SD = 1.4 %). For normalization coefficients with respect to the 16 cm phantom (Fig. 5b), the mean absolute percentage error was 2.3 % (range 0.0–9.3 %, SD = 1.6 %).
Fig. 5.
CTDI normalization coefficient based on calculated diameter in the mid-study slice versus measured diameter at the umbilicus. The line of identity is plotted. a Normalization coefficients with respect to a 32 cm phantom. b Normalization coefficients with respect to a 16 cm phantom
Discussion
Limiting CT radiation dose has long been an important concern for pediatric patients, who are most vulnerable to an elevation in lifetime cancer risk [1]. As a result, automated monitoring of pediatric CT dose has become a prominent imaging informatics concern. However, accurate estimation of CT dose in pediatric patients requires accounting for patient body size. In particular, calculation of size-specific dose estimates per the AAPM task group 204 recommendations requires an estimate of body diameter, which is typically performed manually.
Although patient age is readily available and can be used with body size parameters from the ICRU 74 report to estimate an effective diameter, age does not account for variations in body habitus. This study demonstrates the wide variation in patient size with respect to age. For instance, the range of effective diameters of patients of age 2 overlapped with the range at age 12 (Fig. 2). By comparison, Kleinman et al. calculated 95 % prediction intervals for AP and lateral dimensions of the abdomen as a function of age, and reported that the intervals for a 3-year-old abdomen overlapped with those for a 20-year-old [5]. Brady and Kaufman reported somewhat less variation in effective diameter in the age group less than 13, but nevertheless their range of effective diameters at age 5 overlapped with the range at age 20 [6]. In our study, the size variations result in a significant error range in CTDI normalization coefficients calculated from age-predicted body size compared to coefficients calculated from manual measurements of effective diameter at the umbilicus.
We also demonstrate that a simple algorithm for automated measurement of effective diameter has high accuracy in the pediatric age group, using manual measurements as the reference standard. This accuracy translates into a high degree of correspondence in the calculated normalization coefficients between the automated and manual measurements. We also found that in our patient population, there was little difference between calculating the effective diameter at the umbilicus and calculating the effective diameter in the middle slice of an abdominopelvic CT study, a location readily determined without complex image analysis. These findings support the use of automated body size estimation to adjust pediatric CTDI values in real-time dose monitoring as well as in retrospective dose analysis in a CT dose database.
Other researchers have recently proposed using attenuation data in addition to geometric measurements in the CT image to calculate a “water-equivalent diameter” of the patient for the purpose of more accurate CTDI normalization [8, 9]. However, Monte Carlo simulations using virtual abdomen phantoms do not demonstrate significant differences between the geometric effective diameter and the water-equivalent diameter [9]. Furthermore, the method of thresholding attenuation values used in this work may be less susceptible to artifacts related to motion and beam hardening [7].
This study is limited by the relatively small number of patients examined. However, we believe that our conclusion regarding the inadequacy of age-based patient diameter estimation for CTDI normalization coefficient estimation is unlikely to change with a larger study sample, given the high variance of body habitus that we encountered even in this small set of 128 patients. Further work is required to determine the error arising from the use of a single CT slice for estimating pediatric patient diameter, as recommended in the AAPM report, instead of accounting for the variation of effective diameter over the length of the body.
This work is focused on the problem of estimating patient dose after the scan is performed. However, there is a need to prospectively estimate dose prior to the scan based on body size. Although cross-sectional data may not be available prior to a scan, analogous body size estimation may be possible based on data from the scout tomogram [10].
Conclusion
Automated measurements of pediatric abdominal effective diameter correspond well with manual measurements and result in improved calculation of CTDI normalization coefficients compared to the use of age-predicted body size.
References
- 1.Brody AS, Frush DP, Huda W, Brent RL. Radiation risk to children from computed tomography. Pediatrics. 2007;120:677–682. doi: 10.1542/peds.2007-1910. [DOI] [PubMed] [Google Scholar]
- 2.Size-Specific Dose Estimates (SSDE) in Pediatric and Adult Body CT Examinations: Report of AAPM Task Group 204, American Association of Physicists in Medicine, College Park, MD, 2011
- 3.Strauss KJ, Goske MJ. Estimated pediatric radiation dose during CT. Pediatr Radiol. 2011;41(Suppl 2):472–482. doi: 10.1007/s00247-011-2179-z. [DOI] [PubMed] [Google Scholar]
- 4.International Commission on Radiation Units and Measurements Appendix D: reports produced by the Health Protection Agency (HPA) (formerly National Radiological Protection Board, NRPB) J ICRU. 2005;5:87–92. doi: 10.1093/jicru/ndi032. [DOI] [PubMed] [Google Scholar]
- 5.Kleinman PL, Strauss KJ, Zurakowski D, Buckley KS, Taylor GA. Patient size measured on CT images as a function of age at a tertiary care children’s hospital. AJR Am J Roentgenol. 2010;194:1611–1619. doi: 10.2214/AJR.09.3771. [DOI] [PubMed] [Google Scholar]
- 6.Brady SL, Kaufman RA. Investigation of American Association of Physicists in Medicine Report 204 size-specific dose estimates for pediatric CT implementation. Radiology. 2012;265:832–840. doi: 10.1148/radiol.12120131. [DOI] [PubMed] [Google Scholar]
- 7.Cheng PM: Automated Estimation of Abdominal Effective Diameter for Body Size Normalization of CT Dose. J Digit Imaging 26:406–411, 2013 [DOI] [PMC free article] [PubMed]
- 8.Ikuta I, Sodickson A, Warden GI, Andriole KP, Khorasani R. Automated body size extraction using CT images to calculate water-equivalent diameter. Orlando, FL: Society of Imaging Informatics Annual Meeting; 2012. [Google Scholar]
- 9.Wang J, Duan X, Christner JA, Leng S, Yu L, McCollough CH. Attenuation-based estimation of patient size for the purpose of size-specific dose estimation in CT. Part I. Development and validation of methods using the CT image. Med Phys. 2012;39:6764–6771. doi: 10.1118/1.4754303. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Christner JA, Duan X, Leng S, Yu L, McCollough CH. Attenuation-based estimation of patient size for the purpose of size-specific dose estimation in CT. Part II. Implementation on abdomen and thorax phantoms using cross sectional CT images and scanned projection radiograph images. Med Phys. 2012;39:6772–6778. doi: 10.1118/1.4757586. [DOI] [PubMed] [Google Scholar]