SUMMARY
Free fibula flap is the most common free tissue transfer for maxillary and mandibular reconstructions. The distal part of the harvested bone is transferred, while the proximal part is removed by sub-periosteum dissection. The vascularized periosteum attached to the vascular pedicle has osteogenic potential. 61 patients reconstructed with free fibula flaps were divided in 2 groups: 41 flaps performed with a standard technique and 20 flaps performed by dissecting the periosteum from the pedicle. Patients were followed up with orthopantomography and CT scan at 6, 12, 18 and 24 months after surgery. The minimum follow-up time was 18 months. With retrospective analysis of the first group we diagnosed 7 pedicle ossifications on 41 reconstructions (17%). In the second group, no pedicle ossification was observed (p < 0.05). The dissection of periosteum from the vascular pedicle of free fibula flaps avoids the risk of ossification.
KEY WORDS: Free fibula flap, Vascular pedicle ossification, Mandibular reconstruction, Maxillary reconstruction, Microsurgery
RIASSUNTO
Il lembo libero di fibula è il più frequentemente utilizzato per le ricostruzioni maxilla-mandibolari. L'allestimento del suddetto lembo prevede la rimozione della porzione ossea prossimale della fibula attraverso lo scollamento sottoperiosteo dei tessuti molli entro cui è contenuto il peduncolo vascolare. Il tessuto periosteo limitrofo al peduncolo mantiene le sue caretteristiche osteogenetiche. Il presente studio è stato condotto su una popolazione di 61 lembi liberi di fibula utilizzati per ricostruire altrettanti difetti maxilla-mandibolari post-oncologici. La popolazione in esame è stata suddivisa in due gruppi. Il primo, costituito da 41 pazienti, è stato sottoposto ad allestimento del lembo microchirurgico secondo la tecnica classica. Il secondo gruppo, costituito da 20 pazienti, è stato sottoposto a tecnica di dissezione del periostio dal peduncolo vascolare. Ogni paziente è stato valutato mediante esecuzione di rx OPT e TC a 6, 12, 18 e 24 mesi di follow-up. Nel primo gruppo di studio sono stati riscontrati 7 casi di ossificazione del peduncolo vascolare (17%). Nessun caso è stato rilevato nel secondo gruppo sottoposto a dissezione del periostio (p < 0.05). Il fenomeno di ossificazione del peduncolo vascolare del lembo di fibula non è risultato essere così tanto raro nella nostra casistica, come descritto da altri Autori. La dissezione del periostio dal peduncolo può essere fondamentale nel ridurre ilrischio di ossificazione.
Introduction
Free flaps, by combining a high success rate with low donor site morbidity, are considered the gold standard for the reconstruction of tissues lost during oncologic surgery 1. Free fibula flap is routinely used for large jaw reconstructions 2 3. This can be considered a safe surgical procedure even in elderly head and neck cancer patients 4.
The harvested flap transfers almost the full length of bone, while preserving the integrity of the knee and ankle joints. The harvested fibula is contoured to match the shape of the surgical defect by removing the proximal part of the bone, which permits the pedicle to be lengthened to join the neck vessels. For contouring the flap, osteotomies preserve the interconnections between the periosteum and pedicle, while retaining the surrounding muscle to preserve the blood supply to the bone.
The osteogenic potential of vascularized periosteum is well described in the literature, and many factors have been associated with an increased osteogenic activity in periosteal tissue 5.
The vascularized periosteum attached to the vascular fibula pedicle has osteogenic potential, and some reports of this uncommon phenomenon have been cited in the recent literature 6 7, with a maximum reported incidence of 9.3% 8. This study aimed to investigate bony free flap pedicle ossification through a 7-year retrospective study to calculate the frequency of the condition. We also discuss its management and propose a surgical technique, applied prospectively in our cohort of patients, to avoid this phenomenon.
Materials and methods
We performed a retrospective-prospective study on 61 patients who underwent maxillofacial reconstructions with free fibula flaps after oral cancer ablation at "S. Orsola Malpighi" Hospital in Bologna (Maxillo-Facial and Plastic Surgery Units) during 2004 to 2011.
Patients were divided in two groups: in the first we enrolled 41 flaps performed using a surgical standard technique during 2004 to 2007, and assessed retrospectively. Due to the high percentage of pedicle ossifications in the first group, from January 2008 all flaps were harvested in our Unit according to the surgical periosteum dissection technique. In this second group, we enrolled 20 flaps performed by dissecting the periosteum from the vascular pedicle from 2008 to 2011. This second group was evaluated prospectively.
Follow-up included clinical examination and radiographic evaluation. All patients were followed up systematically with orthopantomography and CT scan at 6 and 12, 18 and 24 months after surgery, according to the standard oncological follow-up procedure. The minimum followup time was 12 months.
We evaluated the descriptive statistics of bony free flaps in the two groups, and the percentage of pedicle ossification was assessed. Demographic characteristics were evaluated and univariate analysis was performed. A p < 0.05 was considered statistically significant.
Surgical technique of periosteum dissection
The technique of fibula harvesting is well known and standardized 9. During the harvest of the fibula free flap, approximately 20 cm of bone is harvested 10.
The proximal aspect of this bone is seldom necessary for reconstruction, but is removed with the flap to facilitate vascular pedicle dissection. Subsequently, during flap contouring, the unnecessary proximal fibula is discarded. A subperiosteal dissection is performed along the area of bone to be discarded to avoid damage to the vascular pedicle. This results in up 10 to 15 cm of well-vascularized periosteum along the peroneal vascular pedicle. This tissue can usually be draped along native bone at the side of the reconstruction or placed over the vessels in the neck to protect the anastomoses.
To avoid the risk of pedicle ossification we performed, in our second study group of patients, a periosteum dissection technique by removing the periosteum exceeded from the proximal peroneal vascular pedicle. This was performed before vascular anastomoses, and can be done using optical loop magnification. It takes about 10-15 min more than the standard surgical procedure.
Results
The flap survival rate was 100% in both groups. Microsurgery was performed on the superior thyroidian artery in 79% of cases, and on the lingual artery in 21% of cases. In all patients the recipient vein was the thyrolinguofacial trunk. In the first group of patients, 7 pedicle ossifications were diagnosed (17%); 3 were in men and 4 in women. In 6 cases (85%), the fibula was used for mandible reconstruction; in 1 case (15%), the flap was performed for maxillary reconstruction.
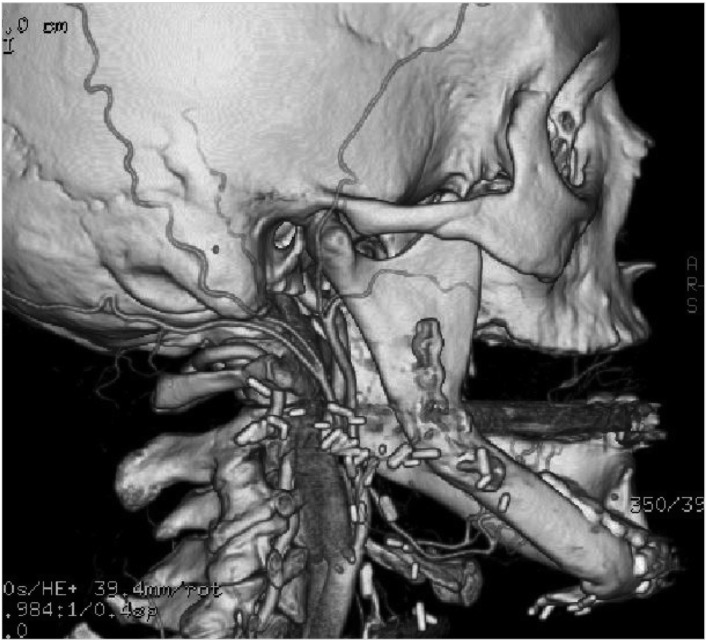
Clinical signs were reported in 2 patients (28%). One patient had hard swelling of submandibular region; one patient had pain in cervical region associated with trismus. Onset of vascular pedicle ossification occurred between 115 and 370 days (median 196 days). Diagnosis was made using orthopantomography (Fig. 1) and CT scan (Fig. 2). In 1 patient, the ossification was diagnosed at the 6 month post-operative follow-up, and in 6 patients at 12 months follow-up.
Fig. 1.
Orthopantomography showing free fibula pedicle ossification of a young patient treated for oral squamous cell carcinoma.
Fig. 2.
3-D CT scan showing sub-mental fibular pedicle ossification 12 months after mandible reconstruction.
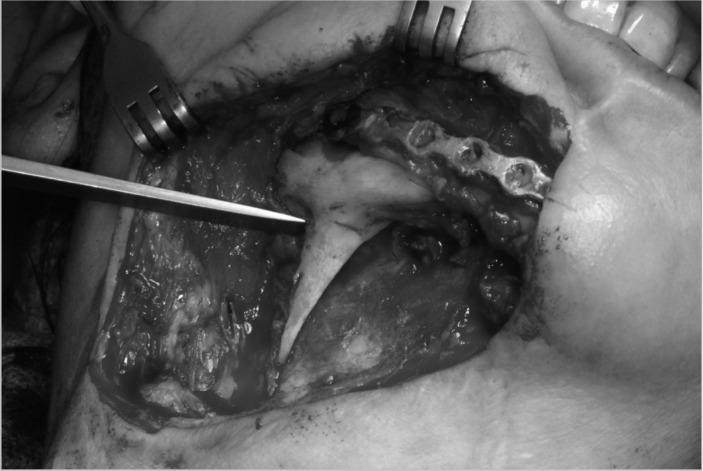
Only the 2 symptomatic patients were surgically treated. Surgical resection of ossified pedicle was performed through submandibular access (Fig. 3). It did not influence the vitality of the flap.
Fig. 3.
Intra-operative image showing clinical aspect of ossificated pedicle before surgical removal.
Asymptomatic patients were also followed up. In the second group of 20 patients, we performed dissection of the periosteum from the vascular pedicle. In this group, to date, no pedicle ossification has been observed. Univariate analysis showed a statistically significant difference (p < 0.05) between the two study groups. No significant increase in operative time was noted, and additional complications were not observed.
Discussion
Only four articles in the literature report ossification of the vascular pedicle in free fibula flaps. Few of the reported cases were symptomatic, presenting trismus, hard swelling, severe pain during mastication and during twisting of the ipsilateral neck.
In one case report ossification was an incidental finding during re-intervention for recurrence 7. The reported symptomatic cases were studied using orthopantomography, CT scan and in one case biopsy for the suspect of recurrence. The maximum incidence reported in literature is of 9.3% 8. The incidence of ossification diagnosis seen in the present study was higher (17%) probably in relation to the systematic radiological follow-up performed in this series.
In our study, 5 of 7 patients were asymptomatic, and most of the time there were no clinical expressions of the calcified pedicle. This is the reason why ossified pedicles are underestimated. Undiagnosed ossified pedicles may potentially lead to complication as pain, trismus and swelling.
Clinically, trismus may be the result of the involvement of masticatory or buccal spaces, subsequent to the disposition of the vascular pedicle in the cheek during the reconstruction of maxillary defects. Swelling of the submandibular region is the typical sign of ossification of pedicle in the reconstruction of mandibular defects. Usually, this sign can be interpreted as a local relapse.
Gonzalez Garcia reported a histological study showing that the bone seems to be mature along the entire pedicle with no gradation, and that bone formation is invasive towards the vascular pedicle 7.
The factors influencing the osteogenic potential of vascularized periosteum have been described 7: contact with vascularized bone, mechanical stimuli, growth factors, systemic steroids and hormones. In all cases presenting vascular pedicle ossification, the contact and continuity between the reconstructed bone and periosteum was preserved, which is fundamental for osteogenesis. In a periosteal free flap in which no contact with bone occurs, the level of ossification is inferior 5. This contact may play a role because progenitor cells and bone morphogenetic proteins (BMPs), factors participating in osteoprogenitor recruitment, proliferation, and differentiation into chondrocytes and osteoblasts have been detected in the site of bone fracture 7. During free flap surgery, osteotomy can be considered a fracture.
Local mechanical tension is another critical factor in bone healing. A recent study suggests that mechanical stress supports BMPs signalling 11. Mechanical forces applied to the stabilized free flap and micromotion, associated with speech or chewing, may enhance bone healing and callus formation. In addition, in our series, for maxillary reconstruction, the pedicle passed through a subcutaneous tunnel in the cheek. This is a potential risk of periosteum stretching. Instead, in mandibular reconstruction, the vascular pedicle, when short, may be stressed by movements of the head. It was postulated that this mechanical stimulus resulted in bone formation by the periosteum 7.
Smith and Funk 12 reported a 12-year-old girl with periosteal ossification and suspected that hormonal factors can also have effect on osteogenesis. Tenenbaum and Heersche demonstrated in an in vitro chick model that brief exposure to dexamethasone promoted periosteal osteogenesis 13. Oestrogen deficiency is also known to lead to osteoporosis, but the exact role of oestrogen in bone metabolism is difficult to quantify 14. In our cases, the female-to-male ratio was 4:3. All females were in an active hormonal status, and one was in the immediate postpartum period.
Finally, inflammation could be a potential factor play an active role in osteogenesis. The mechanism is not well defined, but is possible that the increase of blood flow during inflammation allows osteoprogenitor recruitment.
In our series, correlation with inflammation can be noticed, as in 6 of the 7 ossifications an inflammatory complication occurred. Indeed, all these patients had postoperative infection and inflammation at the reconstructed site. In our experience we did not notice any correlation with gender, as postulated by Autelitano 6. We agree with all prior reports that recommend surgery for the removal of the ossified pedicle only in symptomatic patients. Autelitano 6 proposed to modify the technique and dissect the periosteum from the vascular pedicle to avoid the risk of ossification. Gonzalez Garcia 7 is instead reluctant to perform "extra" dissection of the periosteum that would increase the time and risk of vessel damage.
In our experience, pedicle ossification is not a rare phenomenon, being radiologically present at 12 months in the 17% of free fibula reconstructions performed with the classical technique. Moreover, the dissection of the periosteum from the pedicle avoids the risk of ossification without increasing the rate of complications in this series.
References
- 1.Colletti G, Autelitano L, Tewfik K, et al. Autonomized flaps in secondary head and neck reconstructions. Acta Otorhinolaryngol Ital. 2012;32:329–335. [PMC free article] [PubMed] [Google Scholar]
- 2.Hidalgo DA. Fibula free flap: a new method of mandibular reconstruction. Plast Reconstr Surg. 1989;84:71–79. [PubMed] [Google Scholar]
- 3.Hidalgo DA. Fibula free flap mandibular reconstruction. Clin Plast. Surg. 1994;21:25–35. [PubMed] [Google Scholar]
- 4.Tarsitano A, Pizzigallo A, Sgarzani R, et al. Head and neck cancer in elderly patients: is microsurgical free-tissue transfer a safe procedure? Acta Otorhinolaryngol Ital. 2012;32:371–375. [PMC free article] [PubMed] [Google Scholar]
- 5.Finley JM, Acland RD, Wood MB. Revascularized periosteal grafts-a new method to produce functional new bone without bone grafting. Plast Reconstr Surg. 1978;84:71–79. doi: 10.1097/00006534-197801000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Autelitano L, Colletti G, Bazzacchi R, et al. Ossification of vascular pedicle in fibular free flaps: A report of four cases. Int. J. Oral Maxillofac Surg. 2008;37:669–671. doi: 10.1016/j.ijom.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 7.González-García R, Manzano D, Ruiz-Laza L, et al. The rare phenomenon of vascular pedicle ossification of free fibular flap in mandibular reconstruction. J Craniomaxillofac Surg. 2010;29:1–5. doi: 10.1016/j.jcms.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Myon L, Ferri J, Matthieu G, et al. Consequences of bony free flap's pedicle calcification after jaw reconstruction. J Craniofac Surg. 2012;23:872–877. doi: 10.1097/SCS.0b013e31824ddc68. [DOI] [PubMed] [Google Scholar]
- 9.Pellini R, Mercante G, Spriano G. Step-by-step mandibular reconstruction with free fibula flap modelling. Acta Otorhinolaryngol Ital. 2012;32:405–409. [PMC free article] [PubMed] [Google Scholar]
- 10.Baj A, Youssef DA, Monteverdi R, et al. Reconstruction of partial maxillary defects with the double-barrel fibula free flap. Acta Otorhinolaryngol Ital. 2010;30:299–302. [PMC free article] [PubMed] [Google Scholar]
- 11.Yu YY, Lieu S, Lu C, et al. Bone morphogenetic protein 2 stimulates endochondral ossification by regulating periosteal cell fate during bone repair. Bone. 2010;47:65–73. doi: 10.1016/j.bone.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith RB, Funk GF. Severe trismus secondary to periosteal osteogenesis after fibula free flap maxillary reconstruction. Head Neck. 2003;25:406–411. doi: 10.1002/hed.10236. [DOI] [PubMed] [Google Scholar]
- 13.Tenenbaum HC, Heersche JN. Dexamethasone stimulates osteogenesis in chick periosteum in vitro. Endocrinology. 1985;117:2211–2217. doi: 10.1210/endo-117-5-2211. [DOI] [PubMed] [Google Scholar]
- 14.Jagger CJ, Chow JW, Chambers TJ. Estrogen suppresses activation but enhances formation phase of osteogenic response to mechanical stimulation in rat bone. J Clin Invest. 1996;98:2351–2357. doi: 10.1172/JCI119047. [DOI] [PMC free article] [PubMed] [Google Scholar]