Abstract
An understanding of the latent structure of oppositional defiant disorder (ODD) is essential for better developing causal models, improving diagnostic and assessment procedures, and enhancing treatments for the disorder. Although much research has focused on ODD—including recent studies informing the diagnostic criteria for DSM-5—research examining the latent structure of ODD is sparse, and no known study has specifically undertaken a taxometric analysis to address the issue of whether ODD is a categorical or dimensional construct. To address this gap, the authors conducted two separate studies using a set of taxometric analyses with data from the NICHD Study of Early Child Care and Youth Development (child study; N = 969) and with data from a large mixed sample of adults, which included participants reporting psychiatric difficulties as well as healthy controls (adult study; N = 600). The results of a variety of non-redundant analyses across both studies revealed a dimensional latent structure for ODD symptoms among both children and adults. These findings are consistent with previous studies that have examined latent structure of related constructs (e.g., aggression, antisocial behavior) as well as studies that have examined the dimensional versus categorical structure of ODD using methods other than taxometric analysis.
Keywords: oppositional defiant disorder, taxometric analysis, latent structure
Introduction
Oppositional defiant disorder (ODD), a common childhood disorder marked by argumentativeness, hostility, and noncompliance, has been tied to concurrent and future academic, social, and behavioral difficulties (Burke et al., 2010; Greene et al., 2002). Many children with ODD later meet criteria for conduct disorder (CD; Burke et al., 2010), including engaging in serious violent or criminal behavior and experiencing legal and substance use problems (Loeber et al., 2010). With the recent release of, the DSM-5 (APA, 2013), there has been renewed discussion of the appropriateness of a categorical versus dimensional classification of behavioral disorders and questions about whether appropriate statistical procedures were used to inform these decisions (Walters, 2013). Although ODD has received much attention in the literature—including issues related to changes in DSM-5 (e.g., Pardini et al., 2010)—research on its latent structure is in its infancy (Frick and Nigg, 2012). Specifically, does ODD exist on a continuum, or is it a qualitatively discrete condition that is either present or absent? Although researchers have called for investigations to advance our understanding of the clinical utility of a dimensional versus categorical conceptualization of ODD (e.g., Pardini et al., 2010), most research has focused on outcomes based on those conceptualizations, whereas the specific question regarding the latent structure of ODD itself remains largely unanswered by the literature.
Such a question is important to answer in that determining the latent structure of ODD will (a) help to further refine the diagnostic criteria for ODD, (b) aid with the development of instruments used to assess symptoms of ODD, (c) have implications for understanding the etiology of ODD, and (d) contribute to the development of treatments for children with ODD. For example, knowing the latent structure of ODD can inform whether psychometric research should focus on determining the most accurate cut score for case assignment (if taxonic) or on examining the correlates of a measure (if dimensional). Furthermore, dimensional findings could support the study of subclinical populations for understanding the etiology and treatment of ODD, whereas a taxonic structure would indicate that research on ODD should be limited to those who meet full diagnostic criteria (see Ruscio and Ruscio, 2004). Thus, a better understanding of the latent structure of the disorder has obvious clinical implications. Furthermore, it is an important issue for research given that most studies use a dimensional approach to symptom measurement (Frick and Nigg, 2012) despite the categorical treatment of ODD in the DSM-5 (APA, 2013) and its predecessor the DSM-IV-TR (APA, 2000), the latter of which did not even include an ODD severity index (Pardini et al., 2013). As such, evidence for a dimensional latent structure of ODD would bolster the decision to treat measurement of the construct on a continuum. Likewise, use of a categorical classification (particularly a dichotomy, such as having a diagnosis or not) for a naturally dimensional construct, would minimize the predictive validity of measures assessing that construct when they are used to form categories (cf. Fergusson et al., 2010). Thus, evidence of a dimensional latent structure of ODD would contraindicate the dichotomization of otherwise continuous measures for the purposes of forming groups (i.e., with and without ODD) in research.
Despite the obvious advantages of detecting whether ODD is categorical (taxonic) or is the extreme of an underlying existing continuum (dimensional), research investigating the latent structure of ODD is sparse. Some researchers have examined questions pertinent to the issue. For example, Fergusson et al. (2010) examined the differential relation between ODD among older adolescents (14 to 16 years) and outcomes during late adolescence and early adulthood (primarily 18 to 25 years) when treating ODD dimensionally (i.e., symptom counts based on either self- or mother-report) versus categorically (i.e., meeting diagnostic criteria based on endorsement of four or more symptoms in a given 12-month period by either respondent). Even when controlling for a range of covariate factors, the associations between ODD and a host of subsequent potentially related outcomes—including property and violent offenses, arrests, substance use, mental health disorders, pregnancy or parenthood by age 20, interpartner violence, and poor educational or employment outcomes—were consistently higher when ODD was treated dimensionally. Furthermore, on average, the categorical models estimated only about a half as much variance in the outcomes as the dimensional models.
Such findings are consistent with research on other externalizing behavior problems [e.g., attention-deficit/hyperactivity disorder (ADHD); Frazier et al., 2007; Marcus and Barry, 2011], indicating that dimensional models demonstrate stronger validity coefficients with criterion measures than dichotomous models. Other studies (e.g., Fergusson and Horwood, 1995) also have found that dimensional measures of externalizing behavior, defined more broadly, are better predictors of subsequent problems than are categories of diagnoses and that associated features, and outcomes appear to relate to such behaviors in a linear fashion. Despite the compelling nature of such studies and the support they render for a dimensional approach to assessing ODD, they, nevertheless, do not directly address the issue of the latent structure of ODD. For example, ODD may have a categorical latent structure even if there are varying levels of severity within the taxon. Such a latent structure would not be inconsistent with the research to date finding that a dimensional treatment of ODD better predicts outcomes. To more directly address the issue of its underlying structure, taxometric analyses, which allow an examination of the latent structure of a theoretical construct via a set of indicators for that construct, can be used (Meehl, 1995; Waller and Meehl, 1998).
Although no known study to date has used taxometric analyses to examine ODD, taxometric studies of other externalizing problems including attention-deficit/hyperactivity disorder (as well as inattention and hyperactivity/impulsivity separately) in children (Marcus and Barry, 2011) and adults (Marcus et al., 2012), juvenile psychopathy (Edens et al., 2011; Murrie et al., 2007), and antisocial personality disorder (Walters, 2009) have revealed support for a dimensional structure for these problems. Another study made use of self- and teacher-reports to examine the latent structure of childhood aggression, a correlate of ODD, and concluded that childhood aggression also exists on a continuum (Walters et al., 2010b).
Even more relevant to the structure of ODD, a recent study by Witkiewitz et al. (2013) utilized factor mixture modeling (FMM) to examine lifetime diagnoses (i.e., data collected longitudinally) of externalizing disorders (ODD, CD, ADHD, substance use disorders, and adult antisocial behavior) along the dimensional-categorical spectrum. Fully continuous latent variable models fit the observed data better than fully categorical or mixed models. Furthermore, ODD fell on a factor with ADHD, CD, and adult antisocial behavior, whereas another factor emerged for substance use disorders and adult antisocial behavior (i.e., adult antisocial behavior shared variance with both factors). The findings by Witkiewitz et al. (2013) suggest that ODD, at least within the context of other externalizing disorders across the period from age 6 years to early adulthood, has a dimensional latent structure. Nonetheless, research specifically examining the latent structure of ODD is needed. In fact, replicating such findings using taxometric analyses would be ideal given that taxometric procedures and FMM are mathematically distinct, are based on different sets of assumptions, and may arrive at qualitatively different results that are not directly comparable—even when using the same data for one construct (e.g., FMM may yield a 3 group structure, whereas taxometric methods can only result in either a dimensional or a 2 group structure; Lubke and Muthén, 2005; Waller and Meehl, 1998; but see McGrath and Walters, 2012; Walters et al., 2010a for ways to integrate taxometrics with other latent modeling methods to identify polytomous constructs).
DSM-5 has tweaked the diagnostic criteria so that the symptoms better capture ODD among adults (e.g., adding “authority figures” not just “adults” to the “often argues” criterion; APA, 2013, p. 462). Likewise, recent studies have examined ODD symptoms among adults (e.g., Harpold et al., 2007; Reimherr et al., 2013; Witkiewitz et al., 2013) and concluded that ODD is a valid diagnosis for adults and is relatively common among adults, especially those with ADHD. Still, the preponderance of studies on ODD have been conducted on child and adolescent samples. When examining the issue of the underlying structure of the disorder itself, however, it is apropos to do so within both a child sample and an adult sample to address developmental questions that have been raised in the research (e.g., Frick and Nigg, 2012).
The primary objective of the present set of studies is to address the gap in the literature regarding our understanding of the latent structure of ODD through an examination using taxometric analyses. Furthermore, to consider a developmental perspective, data from both a large child community sample and data from a large adult mixed psychiatric/control sample were used. Each of the two data sets included a measure directly assessing the eight symptoms (i.e., indicators) of ODD. For the child data set, multiple informants (including mother- and teacher-reports) were available; for the adult data set, ratings were self-report of current symptoms.
Study 1
Method
Participants
Data on ODD symptom ratings from at least one informant (mother or teacher) were provided on 969 children who participated in Phase III of the NICHD Study of Early Child Care and Youth Development (SECCYD), a study that ran from birth through sixth grade. The SECCYD sample comprises a diverse group of children born in 1991 in 10 locations across the United States. The taxometric analyses were conducted using data collected when the children were in sixth grade. Details about how the participants were sampled, data collection procedures, and the demographics of the group can be found in the NICHD Early Child Care Research Network (2005).
Measure
Disruptive Behavior Disorders Questionnaire (DBQ; Pelham et al., 1992). This scale includes all 8 DSM-IV-TR symptoms of ODD rated on a 0–3 Likert scale and is consistent with the 8 DSM-5 symptoms (APA, 2013). Two versions of the DBQ—parent (mother as informant) and teacher—were used as primary indicators of ODD. The mothers and teachers completed the DBQ independently. Although data were available for 969 children, both mother- and teacher-reports were available for 571 children, teacher-report only was available for 254 children, and mother-report only was available for 144 children. Inter-rater reliability for the two raters (n = 571) was r = .30, p < .001, ICC = .20; this magnitude is consistent with the moderate correlations typically found between mothers and teachers when rating child behaviors (Frick et al., 2010). The mother- and teacher-reports were combined by using the higher scoring response for each item, a common method for combining data from multiple informants (Bird et al., 1992; Piacentini et al., 1992). In the cases where only one informant’s report was available, the ratings from that informant (mother or teacher) were used. These combined ODD items were internally consistent in the current sample (α = .92).
Taxometric Data Analysis
We used mean above minus mean below a cut (MAMBAC; Meehl and Yonce, 1994), maximum eigenvalue (MAXEIG; Waller and Meehl, 1998), and latent mode (L-Mode; Waller and Meehl, 1998) for the taxometric analyses reported in this study and in Study 2. These three taxometric procedures are non-redundant, so consistent results across all three procedures provides compelling evidence for the study's findings. In MAMBAC, one variable is selected as the input indicator, and the data are sorted along the x-axis using this indicator. A series of cuts are then made along the x-axis (50 in the current studies), and at each cut, the difference between the mean of the output variable above the cut and the mean of the output variable below the cut is plotted along the y-axis. Because the indicators in both studies were eight individual items (i.e., the ODD symptoms), the input indicator was constructed by summing the seven items that were not used as the output indicator (Walters and Ruscio, 2009). The MAMBAC analysis is then repeated selecting a different item as the output indicator, resulting in eight MAMBAC graphs for each study. A taxonic construct should yield graphs with an inverse U-shape, with the highest point representing the taxon base rate. A dimensional construct prototypically yields a U-shaped curve.
In MAXEIG, the sample is also sorted along the x-axis using an input indicator, but here the sample is divided into a series of overlapping windows (25 windows with .90 overlap in the current studies, Walters and Ruscio, 2010). For each slice, the y-axis value is the eigenvalue of the first principle component from a principal component analysis of the other seven output variables, generating eight MAXEIG graphs for each study. If the construct is taxonic, the slices that are more evenly divided between taxon and complement members should have the largest eigenvalues, yielding a graph with an inverse U-shape, with the peak representing the taxon base rate. A U-shaped, flat, or irregular MAXEIG graph is indicative of a dimensional construct. Finally, all eight indicators are factor analyzed, and scores on the first principal factor are graphed in L-Mode. A taxonic L-Mode graph is bimodal, whereas a dimensional L-Mode graph is unimodal or irregular (see Ruscio et al., 2006 for additional details regarding these taxometric procedures).
It is often difficult to interpret taxometric graphs because factors other than the construct's latent structure (e.g., skew, correlations among the indicators) can influence the shape of these graphs. To guide the interpretation of taxometric graphs, one strategy that has received considerable empirical support is to simulate data sets that reproduce many of the features of the actual data while varying its latent structure (taxonic or dimensional). These simulated data sets can then be analyzed using MAMBAC, MAXEIG, and L-Mode (Ruscio et al., 2007), and the graphs can be compared to the graphs from the research data. In each of the present studies, we generated 100 samples of simulated taxonic and dimensional comparison data and used comparison curve fit indices (CCFI) to assess the goodness-of-fit between the research data and the simulated taxonic and dimensional graphs. CCFI values greater than .55 support a taxonic structure, and those less than .45 support a dimensional latent structure. In a Monte Carlo study using 100,000 data sets, the latent structure was correctly classified 99.9% of the time when the three taxometric procedures all yielded CCFIs greater than .55 or less than .45 (Ruscio et al., 2010). Ruscio’s (2012) program for R was used to conduct the taxometric analyses.
Results
The indicators used for a set of taxometric analyses should demonstrate at least 1.25 standard deviation units (SDU) of separation between the presumptive taxon and complement groups (Meehl, 1995). In the SECCYD sample, 94 (9.7%) of the children met the DSM-IV-TR criteria for ODD based on the mother and teacher responses to the DBQ, which is within the range of prevalence rates of ODD in the general population (1 to 11%; APA, 2013; Canino et al., 2010)—and is generally consistent with an estimate in the United States based on a structured diagnostic interview (7.1%; Canino et al., 2010). Using these case classifications, the eight DBQ items had excellent indicator validity (Table 1, which also includes the average correlations among the eight indicators in the full sample, the putative taxon group, and the putative complement group). Alternatively, when the MAMBAC and MAXEIG procedures were used to generate a base rate estimate, this average estimate of 19% also yielded strong indicator coefficients (Table 1). Each set of taxometric analyses was run twice, first using simulated taxonic data derived from the diagnostic classifications and second using simulated taxonic data based on the average base rate estimates from MAMBAC and MAXEIG (the graphs provided in Figures 1 and 2 are from the first sets of simulated data).
Table 1.
Summary of the Taxometric Analyses Examining the Latent Structure of Oppositional Defiant Disorder
| CCFI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample | n | BR | skew | d (range) | r | rc | rt | MAMBAC | MAXEIG | L-Mode | MEAN |
| Child | 969 | .097a | 1.13 | 2.34 (2.12–2.61) | .59 | .42 | .26 | .311 | .380 | .329 | .340 |
| 969 | .190b | 1.13 | 2.08 (1.89–2.27) | .59 | .33 | .30 | .254 | .300 | .319 | .291 | |
| Adult Full | 600 | .207a | 1.19 | 2.15 (1.42–2.68) | .59 | .37 | .19 | .340 | .364 | .317 | .340 |
| 600 | .230b | 1.19 | 2.16 (1.40–2.53) | .59 | .32 | .19 | .304 | .309 | .286 | .300 | |
| Adult Clinical | 432 | .287a | 0.81 | 1.80 (1.12–2.27) | .54 | .32 | .19 | .325 | .365 | .331 | .340 |
| 432 | .307b | 0.81 | 1.82 (1.13–2.16) | .54 | .28 | .18 | .301 | .348 | .328 | .326 | |
Note. n = sample size; BR = base rate; skew = average skew of the indicators; d = indicator validity in SD units; r = average correlation among the indicators in the full sample; rc = average correlation among the indicators in the putative complement; rt = average correlation among the indicators in the putative taxon; CCFI = comparison curve fit index.
Based on the number of cases meeting the symptom threshold for Oppositional Defiant Disorder.
Based on the average of the MAMBAC and MAXEIG base rate estimates.
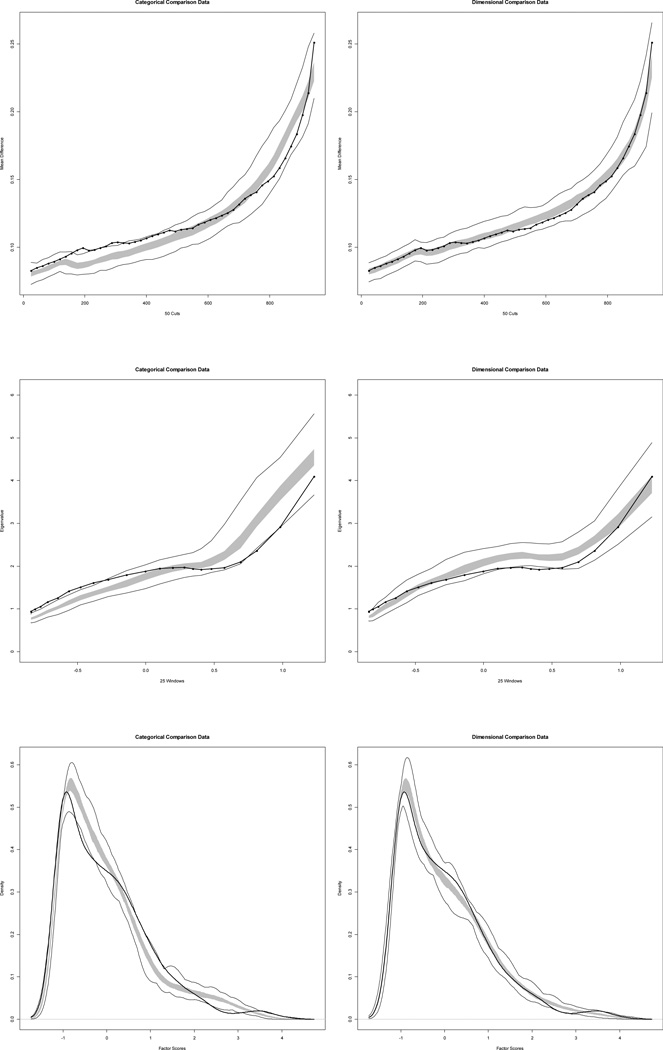
Figure 1.
Average MAMBAC, MAXEIG, and L-Mode curves for the research data along with taxonic and dimensional comparison data for the eight Disruptive Behavior Disorders Questionnaire Oppositional Defiant Disorder items. For MAMBAC, the x-axis represents the cases ordered along the input indicator, and the values along the y-axis are the mean differences on the output indicator between those above the cut and those below the cut on the x-axis. For MAXEIG, the data were ordered along the x-axis by the scores on the input indicator and then grouped into 25 subsamples using overlapping windows (0.90 overlap). The y-axis is the eigenvalue of the first principle component from a principal component analysis of the output variables for each subsample. For L-Mode the x-axis is the scores on the first factor of a factor analysis of the indicator set, and the y-axis is the relative frequency of each score. For all of the graphs, dark lines on the curves represent the actual data, the outer lines show the minimum and maximum values generated by the 100 simulated data sets, with the grey band containing the middle 50% of data points from these simulated data.
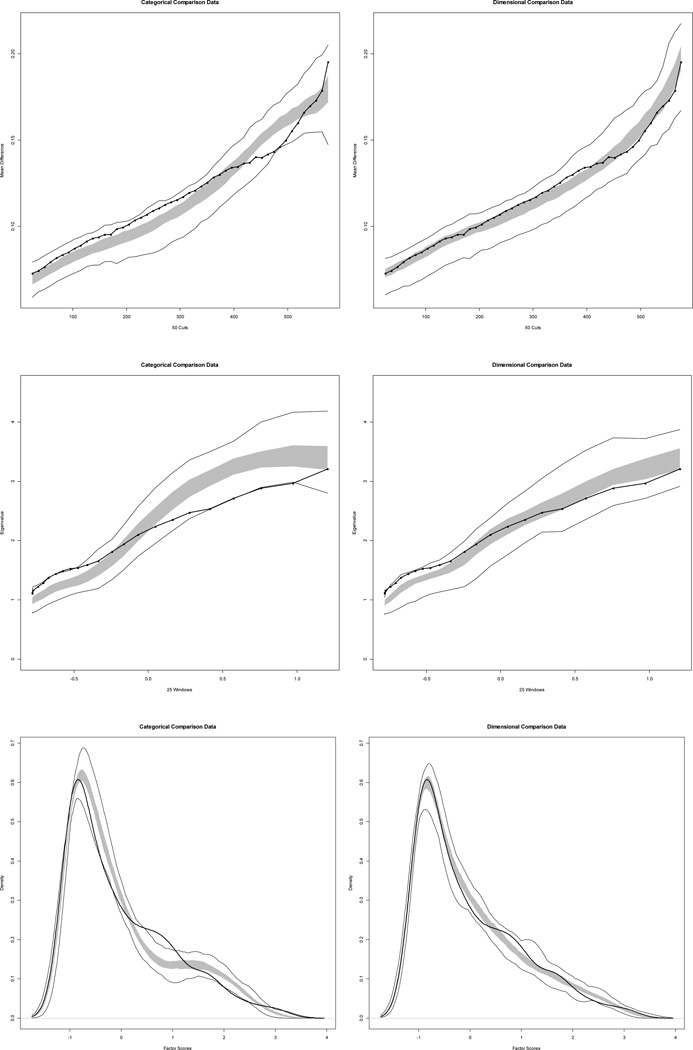
Figure 2.
Average MAMBAC, MAXEIG, and L-Mode curves for the research data along with taxonic and dimensional comparison data for the eight Self-Report Wender-Reimherr Adult Oppositional Defiant Disorder items. The axes of these graphs are the same as in Figure 1. Dark lines on the curves represent the actual data, the outer lines show the minimum and maximum values generated by the 100 simulated data sets, with the grey band containing the middle 50% of data points from these simulated data.
All eight MAMBAC curves had a rising cusp on the right side of the graph, which could result from either a low base rate taxon or positively skewed indicators. However, the average of these eight curves appeared considerably more similar to the simulated dimensional data than to the simulated taxonic data, and the CCFIs (Table 1) confirmed the similarity to the simulated dimensional data (Figure 1, top panel). Similarly, the eight MAXEIG graphs all appeared to rise on the right side of the graph without demonstrating a clear peak. Again, the average MAXEIG curve was more similar to the simulated dimensional data than to the simulated taxonic data, (Figure 1, middle panel). Finally, the L-Mode graph was unimodal and appeared more similar to the simulated dimensional data (Figure 1, bottom panel).
Study 2
Method
Participants
The participants were 600 physically healthy subjects who were evaluated as part of a larger research program examining the correlates of impulsive and aggressive behaviors. Roughly 70% of the sample (n = 432) were recruited from clinical settings or through newspaper advertisements seeking individuals with psychiatric difficulties. The remaining 168 participants were healthy controls who reported little evidence of psychopathology.
Most of the participants were Caucasian (55.8%), followed by African-American (33.7%). There were slightly more men (53.7%; mean age 35.3 years) than women (mean age 34.2 years) in the sample. This same sample was also used in a recent taxometric study of the latent structure of adult attention deficit/hyperactivity disorder (Marcus et al., 2012). Additional details about the demographic features, diagnostic assessment, and study procedures may be found in that report.
Measure
The Self-Report Wender-Reimherr Adult Attention Deficit Disorder Scale (SR-WRAADDS; Reimherr et al., 2007) also includes eight items that correspond to the eight DSM-IV-TR ODD symptoms rated on a 0–3 Likert-type scale. Thus, in format and content, the SR-WRAADDS ODD items correspond directly to the DBQ ODD items. It should be noted that respondents to the SR-WRAADDS answer based on their current adult behavior, not retrospectively; thus, it examined adult ODD symptoms. These ODD items were internally consistent in the current sample (α = .92).
Results
One hundred twenty-four participants (20.7%) met the diagnostic threshold for ODD on the WRAADDS. Using these case assignments to estimate indicator validity, the eight SR-WRAADDS ODD items had very good indicator validity (Table 1). Alternatively, when the MAMBAC and MAXEIG procedures were used to generate a base rate estimate, this average estimate of 23% also yielded strong indicator coefficients (Table 1).
As was the case with the child ODD data, all eight MAMBAC curves had a rising cusp on the right side of the graph. Once again, the average of these eight curves was more similar to the simulated dimensional data than to the simulated taxonic data (Table 1; Figure 2, top panel). Four of the eight MAXEIG graphs were flat, and the other four graphs all appeared to rise on the right side of the graph without demonstrating a clear peak. Again, the average MAXEIG curve was more similar to the simulated dimensional data than to the simulated taxonic data, (Table 1; Figure 2, middle panel). The L-Mode graph was unimodal and was more similar to the simulated dimensional data, (Table 1; Figure 2, bottom panel).
Because the full sample included both a clinical sample and a healthy control group, we repeated the taxometric analyses limited to the 432 clinical subjects. In this clinical sample 28.7 met the diagnostic criteria for ODD. These analyses also yielded consistently dimensional results (Table 1).
Discussion
The results from both a large community-based child sample and a large mixed psychiatric/control adult sample converged on a dimensional model of ODD. These findings, which included robust indicator validity coefficients and consistently low CCFIs, indicate that ODD should be assessed and diagnosed along a continuum and that attempts to distinguish between clinical and subclinical levels of ODD are likely to be arbitrary. Diagnostic classification systems need to better recognize the dimensionality of constructs, such as ODD, in an effort to improve how such systems are used in guiding decisions for individuals (Frick and Nigg, 2012). The recently published DSM-5 (APA, 2013) still yields a discrete diagnosis of ODD based on meeting a criterion number of symptoms and, thus, passing the symptom threshold for the disorder (versus not having the diagnosis). That is, a DSM-5 diagnosis of ODD is based on a dichotomized, categorical decision. Somewhat improved over its predecessor, an ODD diagnosis in DSM-5 includes a current severity index (mild, moderate, or severe, which is a required specifier for the diagnosis; APA, 2013), which at least recognizes dimensionality within the disorder. However, severity is based on number of settings in which symptoms and impairment take place (i.e., pervasiveness) once an individual meets the diagnostic cut-off for the condition of ODD, rather than considering subclinical levels of ODD. The latter consideration is the more pertinent one for a dimensional latent structure of ODD.
Notably, our dimensional results converged with previous taxometric analyses of other childhood externalizing disorders including childhood aggression (Walters et al., 2010), childhood psychopathy (Edens et al., 2011; Murrie et al., 2007), and ADHD (Marcus and Barry, 2011) as well as with FMM results of lifetime (child and adult) externalizing disorders, which included ODD (Witkiewitz et al., 2013). Certainly, our findings for the isolated construct of ODD within a child and adult cross-sectional sample using taxometric analyses, combined with the Witkiewitz et al.’s (2013) findings for broadly defined externalizing disorders (including ODD) within a longitudinal sample spanning from childhood to adulthood using FMM, provide robust evidence for the dimensional structure of ODD. Thus, it can be concluded that a diagnosis of ODD reflects a deviation in severity of behaviors that are found, at some level, in typical development, rather than reflecting the presence of some qualitatively distinct behavior that is typically not present.
Our findings of a higher base rate of ODD among the adult sample (20.7%) compared to the child sample (9.7%) most likely reflects the different ways in which each sample was recruited (i.e., an attempt to recruit a cross-section of children in the SECCYD samples versus an attempt to oversample individuals with impulse and aggression problems in the adult sample). However, the overall finding of a dimensional structure of ODD for both the child and adult samples suggests that, the underlying structure of the construct remains the same. Our findings have important implications for the assessment and diagnosis of ODD across the lifespan and can inform further developments for treatments of the disorder for children and adults. Specifically, dimensional approaches to the assessment of ODD, with items that assess the full range of ODD symptomatology should be superior to assessment instruments designed to determine if respondents meet a diagnostic threshold (i.e., determining the ideal cut score for identifying those with ODD is likely to be a futile exercise). Additionally, because dimensional constructs likely result from the combination of multiple etiological factors, research on the etiology and treatment of ODD should focus on identifying various risk factors that may contribute to the development of this set of behaviors, instead of focusing on a single causal factor. Furthermore, research on ODD does not need to be limited to clinical samples. Instead, community samples that include the full range ODD severity may help inform this literature.
Despite its clear implications, our study has several limitations. We may have missed a very low base rate ODD taxon. However, this possibility is unlikely given the size of the samples and the expected base rate of ODD. Although a strength was the use of multiple informants (mother and teacher), thereby circumventing the issue of mono-informant bias, data were missing from one respondent for 398 of 969 (over 40%) of the children. Thus, the indicators in the child study were a mix of mother/teacher-report [with the only the highest rating considered for each item], mother-report only, or teacher-report only (the latter two taken indiscriminately because data from the other respondent was missing). Although the ODD items based on taking the highest rating at the item level (or taking the only item rating available in the event one was missing) yielded excellent internal consistency, such a finding is only a precursor for validity. Future research should continue to examine the latent structure of ODD using multiple methods from multiple informants to provide further evidence of the dimensional nature of this construct.
Acknowledgments
Role of Funding Source
This work was supported, in part, by grants from the National Institute of Mental Health to Dr. Coccaro (RO1 MH46848, RO1 MH47495, RO1 MH60836, and RO1 MH66984).
This child ODD data used in this study was drawn from research conducted by the NICHD Early Child Care Research Network, supported by NICHD through a cooperative agreement that calls for scientific collaboration between the grantees and the NICHD staff.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors of the present study, "The Latent Structure of Oppositional Defiant Disorder in Children and Adults," have no conflicts of interest, financial, personal, or otherwise, that could inappropriately influence, or be perceived to influence, their work.
Contributors
All four authors conceived of the study in collaboration. Dr. Coccaro provided the data for the adult sample and wrote that portion of the Method section. Dr. T. Barry provided the data for the child sample and wrote that portion of the Method section. Dr. Marcus conducted the taxometric analyses and wrote the Results section. Drs. T. Barry and C. Barry wrote most of the Introduction and Discussion. All four authors contributed to and have approved the final manuscript.
References
- Achenbach TM. Manual for the child behavior checklist and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental health disorders: Fifth edition (DSM-5) Arlington, VA: Author; 2013. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental health disorders: Fourth edition, text revision (DSM-IV-TR) Washington, DC: Author; 2000. [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Burke JD, Waldman I, Lahey BB. Predictive validity of childhood oppositional defiant disorder and conduct disorder: Implications for the DSM-V. Journal of Abnormal Psychology. 2010;119:739–751. doi: 10.1037/a0019708. [DOI] [PubMed] [Google Scholar]
- Canino G, Polanczyk G, Bauermeister JJ, Rohde LA, Frick PJ. Does the prevalence of CD and ODD vary across cultures? Social Psychiatry and Psychiatric Epidemiology. 2010;45:695–704. doi: 10.1007/s00127-010-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edens JF, Marcus DM, Vaughn MG. Exploring the taxometric status of psychopathy among youthful offenders: Is there a juvenile psychopath taxon? Law and Human Behavior. 2011;35:13–24. doi: 10.1007/s10979-010-9230-8. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Classification of behavior disorders in adolescence: Scaling methods, predictive validity, and gender differences. Journal of Abnormal Psychology. 2010;119:699–712. doi: 10.1037/a0018610. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Naugle RI. The latent structure of attention-deficit/hyperactivity disorder in a clinic-referred sample. Neuropsychology. 2007;21:45–64. doi: 10.1037/0894-4105.21.1.45. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Barry CT, Kamphaus RW. Clinical assessment of children’s personality and behavior. 3rd edition. New York: Springer; 2010. [Google Scholar]
- Frick PJ, Nigg JT. Current issues in the diagnosis of attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder. Annual Review of Clinical Psychology. 2012;8 doi: 10.1146/annurev-clinpsy-032511-143150. 877-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene RW, Biederman J, Zerwas S, Monuteaux M, Goring JC, Faraone SV. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. The American Journal of Psychiatry. 2002;159:1214–1224. doi: 10.1176/appi.ajp.159.7.1214. [DOI] [PubMed] [Google Scholar]
- Harpold T, Biederman J, Gignac M, et al. Is oppositional defiant disorder a meaningful diagnosis in adults?: Results from a large sample of adults with ADHD. Journal of Nervous and Mental Disease. 2007;195:601–605. doi: 10.1097/NMD.0b013e318093f448. [DOI] [PubMed] [Google Scholar]
- Loeber R, Burke J, Pardini DA. Development and etiology of disruptive and delinquent behavior. Annual Review of Clinical Psychology. 2009;5:291–310. doi: 10.1146/annurev.clinpsy.032408.153631. [DOI] [PubMed] [Google Scholar]
- Lubke GH, Muthén BO. Investigating population heterogeneity with factor mixture models. Psychological Methods. 2005;10:21–39. doi: 10.1037/1082-989X.10.1.21. [DOI] [PubMed] [Google Scholar]
- Marcus DM, Barry TD. Does attention-deficit/hyperactivity disorder have a dimensional latent structure? A taxometric analysis. Journal of Abnormal Psychology. 2011;120:427–442. doi: 10.1037/a0021405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus DM, Norris A, Coccaro E. The latent structure of attention deficit/hyperactivity disorder in an adult sample. Journal of Psychiatric Research. 2012;46:782–789. doi: 10.1016/j.jpsychires.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath RE, Walters GD. Taxometric analysis as a general strategy for distinguishing categorical from dimensional latent structure. Psychological Methods. 2012;17:284–293. doi: 10.1037/a0026973. [DOI] [PubMed] [Google Scholar]
- Meehl PE. Bootstraps taxometrics: Solving the classification problem in psychopathology. American Psychologist. 1995;50:266–275. doi: 10.1037//0003-066x.50.4.266. [DOI] [PubMed] [Google Scholar]
- Meehl PE, Yonce LJ. Taxometric analysis: II. Detecting taxonicity using covariance of two quantitative indicators in successive intervals of a third indicator (MAXCOV procedure) Psychological Reports. 1996;78:1091–1227. [Google Scholar]
- Murrie DC, Marcus DM, Douglas KS, Lee Z, Salekin RT, Vincent G. Youth with psychopathy features are not a discrete class: A taxometric analysis. Journal of Child Psychology and Psychiatry. 2007;48:714–723. doi: 10.1111/j.1469-7610.2007.01734.x. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Child care and child development: Results of the NICHD study of early child care and youth development. New York: Guilford Press; 2005. [Google Scholar]
- Pardini DA, Frick PJ, Moffitt TE. Building an evidence base for DSM–5 conceptualizations of oppositional defiant disorder and conduct disorder: Introduction to the special section. Journal of Abnormal Psychology. 2010;119:683–688. doi: 10.1037/a0021441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III—R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Piacentini JC, Cohen P, Cohen J. Combining discrepant diagnostic information from multiple sources: Are complex algorithms better than simple ones? Journal of Abnormal Child Psychology. 1992;20:51–63. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- Reimherr FW, Marchant BK, Olsen JL, Wender PH, Robison RJ. Oppositional defiant disorder in adults with ADHD. Journal of Attention Disorders. 2013;17:102–113. doi: 10.1177/1087054711425774. [DOI] [PubMed] [Google Scholar]
- Reimherr FW, Williams ED, Strong RE, Mestas R, Soni P, Marchant BK. A double-blind, placebo-controlled, crossover study of osmotic release oral system methylphenidate in adults with ADHD with assessment of oppositional and emotional dimensions of the disorder. Journal of Clinical Psychiatry. 2007;68:93–101. doi: 10.4088/jcp.v68n0113. [DOI] [PubMed] [Google Scholar]
- Ruscio J. Taxometric program documentation, R language [Computer software and manual] 2012 Retrieved from http://www.tcnj.edu/~ruscio/taxometrics.html. [Google Scholar]
- Ruscio J, Haslam N, Ruscio A. Introduction to the taxometric method: A practical guide. Mahwah, NJ: Erlbaum; 2006. [Google Scholar]
- Ruscio J, Ruscio AM. Clarifying boundary issues in psychopathology: The role of taxometrics in a comprehensive program of structural research. Journal of Abnormal Psychology. 2004;113:24–38. doi: 10.1037/0021-843X.113.1.24. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Ruscio AM, Meron M. Applying the bootstrap to taxometric analysis: Generating empirical sampling distributions to help interpret results. Multivariate Behavioral Research. 2007;42:349–386. doi: 10.1080/00273170701360795. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Walters GD, Marcus DK, Kaczetow W. Comparing the relative fit of categorical and dimensional latent variable models using consistency tests. Psychological Assessment. 2010;22:5–21. doi: 10.1037/a0018259. [DOI] [PubMed] [Google Scholar]
- Tackett JL. Toward an externalizing spectrum in DSM–V: Incorporating developmental concerns. Child Development Perspectives. 2010;4:161–167. [Google Scholar]
- Waller NG, Meehl PE. Multivariate taxometric procedures: Distinguishing types from continua. Thousand Oaks, CA: Sage Publications, Inc.; 1998. [Google Scholar]
- Walters GD. Commentary: Dimensions vs. categories in psychiatric diagnosis. Journal of Nervous and Mental Disease. 2013;201:532–533. doi: 10.1097/NMD.0b013e318294832c. [DOI] [PubMed] [Google Scholar]
- Walters GD. Latent structure of a two-dimensional model of antisocial personality disorder: Construct validation and taxometric analysis. Journal of Personality Disorders. 2009;23:647–660. doi: 10.1521/pedi.2009.23.6.647. [DOI] [PubMed] [Google Scholar]
- Walters GD, McGrath RE, Knight RA. Taxometrics, polytomous constructs, and the comparison curve fit index: A Monte Carlo analysis. Psychological Assessment. 2010a;22:149–156. doi: 10.1037/a0017819. [DOI] [PubMed] [Google Scholar]
- Walters GD, Ronen T, Rosenbaum M. The latent structure of childhood aggression: A taxometric analysis of self-reported and teacher-rated aggression in Israeli schoolchildren. Psychological Assessment. 2010b;22:628–637. doi: 10.1037/a0019779. [DOI] [PubMed] [Google Scholar]
- Walters GD, Ruscio J. To sum or not to sum: Taxometric analysis with ordered categorical assessment items. Psychological Assessment. 2009;21:99–111. doi: 10.1037/a0015010. [DOI] [PubMed] [Google Scholar]
- Walters GD, Ruscio J. Where do we draw the line? Assigning cases to subsamples for MAMBAC, MAXCOV, and MAXEIG taxometric analyses. Assessment. 2010;17:321–333. doi: 10.1177/1073191109356539. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, King K, McMahon RJ, et al. Evidence for a multi-dimensional latent structural model of externalizing disorders. Journal of Abnormal Child Psychology. 2013;41:223–237. doi: 10.1007/s10802-012-9674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]