Abstract
Introduction
The aim of this study was to determine incidence of cardiovascular disease (CVD) risk factors [hypertension (HTN), obesity, Dyslipidemia (DLP), diabetes mellitus (DM) and smoking] in Oskoo.
Methods
This study was planned according to WHO protocol “WHO CVD-risk management package for low and medium-resource settings” and named “East Azerbaijan healthy heart program”. The pilot study of this program was done in Oskoo in 2007-2009. In this study, demographic data and CVD risk factors of 37,329 adults aged ≥30 years old living in Oskoo were collected. In addition, blood samples of 17,388 adults ≥40 years old were taken (free of charge) for assessment of serum glucose and lipid profile.
Results
The study covered 93.52% of Oskoo town population aged≥30 years old. We studied 18637 male (91.50% coverage) and 18692 female (95.52% coverage) participants. The incidence of HTN [SBP≥140 & DBP≥90 mmHg] was 16.25% (M:15.08%, F:17.29%), pre-hypertension [SBP=120-139 & DBP=80-89 mmHg] =37.78% (M:41.38%, F:34.18%), DM [fast blood glucose (FBS)≥126mg/dl] was 7.45% (M:6.35%, F:8.54%), smoking was 9.40% (M:17.00%, F:1.57%), hypercholesterolemia (>200mg/dl) was 47.64% (M:42.46%, F:52.81%) and obesity [body mass index (BMI) ≥27] was 50.47% (M:38.79%, F:62.09%).
Conclusion
Considering high incidence of CVD risk factors (except smoking) in Oskoo adults ≥30 years, it is recommended that this pilot study expanded to all of East Azerbaijan. Free of charge taking blood samples from people ≥ 40 years to evaluate lipid profile and glucose levels is worthy to early detecting the prevalent DM or DLP in this target population.
Keywords: Cardiovascular Disease, Risk Factor, Prevalence, Community-based Study
Introduction
In September 2011, new World Health Organization (WHO) report: “Global atlas on cardiovascular disease(CVD) prevention and control” states that CVDs are the leading causes of death and disability in the world.1 Although a large proportion of CVDs is preventable, they continue to rise mainly because preventive measures are inadequate. In this report an estimated 17.3 million people died from.1 about ninety percent of the world’s total disease burden rises in middle-income countries, while only ten percent of global health expenditure is assigned in these countries.2
There has been change over the last two decades in the geographical distribution of the CVD incidence with obvious decline in the developed countries and rise in the developing countries including the Middle East region. The Islamic Republic of Iran, as Middle East country was adopting the western lifestyle such as nutrition habits, smoking and physical inactivity that led to higher incidence of CVD risk factors in the related population. Such changes coupled with improvement in health services have resulted in improving the life expectancy and the emergence of non-communicable diseases (NCDs) including CVDs. The CVDs are considered as the leading cause of death in Iran in the past 10 years.3 There are two protocols to decrease the burden of CVDs. The population strategy that includes community-based strategies, health promoting strategies and that minimal modification in CVD risk in community can remarkable reduce the incidence of CVD. The alternative is to screening the risk factors in “high risk” adults undergo prophylactic therapies.4 As we implemented in our study, these alternative strategies, “population” (recruitment of all adults) and “high risk” (adults ≥30 years old), can of course be considered as complementary to achieve the best results.
Most of community-based programs on CVD risk factors in Iran, including “Healthy Heart Programs”,3,5,6 were undertaken on limited samples of the target population and then tried to integrate the results to entire population. On the other hand, frequently, the focus was on single or limited number of risk factors, rather than on comprehensive cardiovascular risk. For CVD prevention and control activities to achieve the greatest impact, a paradigm shift is required from the “treatment of risk factors in isolation” to “comprehensive cardiovascular risk management”. To facilitate this shift, WHO developed the CVD-Risk management package through an iterative process with collaborating experts that is named “WHO CVD-risk management package for low and medium-resource settings”.7
According to above-mentioned package, a population-based survey of CVD risk factors was conducted in Oskoo town near to Tabriz (northwest Iran) on entire population aged ≥30. The study was implemented under the supervision of Cardiovascular Research Center, Tabriz University of Medical Sciences from March 2007 to March 2009. Two novel aspects of this study were selecting adults aged ≥30 years old rather than 15-64 years old to have better cover the at-risk population, and including all rural and urban population (health CVD-risk census) of Oskoo town rather than sampling a small number of general populations.
Materials and methods
After approval of the study proposal in Cardiovascular Research Center (Tabriz University of Medical Sciences), this population-based survey was carried out in East Azarbaijan province and named “East Azerbaijan province healthy heart program”. The pilot study of this community-based program was done in Oskoo town near Tabriz (northwest Iran) in 2007-2009. The study population comprised people aged ≥30 years old living in rural and urban areas of Oskoo. Oskoo is at 10 km south of Tabriz with a population of 88,433 according to the national census in 2006. According to the census results, the number of Oskoo people aged ≥30 years old was 37,329 consisting of 18,637 male and 18,692 female.
We planned the study according to WHO protocol “WHO CVD-risk management package for low and medium-resource settings”.7 The package is aimed to carry out in a range of healthcare facilities in low- and middle-resource departments, in developing countries, therefore, it has been planned for three situations that mirror usually encountered resource accessibility strata in such settings. Full text of this package was translated to Persian, copied and distributed in all rural and urban “Health and Treatment Centers”. The three main scenarios of this package were explained in detail at several meetings in Oskoo to the health managers, practitioners, and staff.
In addition, the WHO steps of risk factors for NCDs were explained to health practitioners and staff. This protocol utilizes stratified levels of risk factor appraisal including gathering information applying questionnaires (step 1), physical assessments (step 2), and taking blood samples for biomedical check-up (step 3).8
We also coordinated the Oskoo three main biomedical laboratories to refer to target rural and urban “health and treatment centers” to in-site taking blood samples for biomedical assessment of fasting blood glucose (FBS), cholesterol (Chol), triglyceride (TG), high density lipoprotein (HDL) and low density lipoprotein (LDL) in 17,388 adults ≥40 years old. These biochemical assessments were free of charge and majority of the study cost was spent to 17,388 laboratory assessments of FBS and full lipid profile.
Through two years (March 2007 to March 2009) the questionnaires of 37,329 participants were completed by health practitioners and staff and transmitted to Cardiovascular Research Center in Tabriz to entering the data in SPSS statistical package data-sheet (SPSS Inc, Chicago, IL, USA; v. 16.0). Moreover, the results of 17,388 biochemical tests were collected and entered to SPSS data-sheet. The descriptive data of participants such as demographic characteristics and frequencies of various CVD risk factors consisting: hypertension (HTN), obesity [body mass index(BMI) ≥27], dyslipidemia (DLP), diabetes mellitus (DM) [FBS ≥126mg/dl] and smoking and some pre-risk factors including: pre-hypertension (Pr-HTN) [SBP=120-139 & DBP=80-89 mmHg] in both genders and different age groups were determined. The definitions of all CVD risk factors and biochemical measurements were made according to WHO protocol “WHO CVD-risk management package for low and medium-resource settings”.7 The reader is referred to full text package for detail study of CVD-risk management in three consecutive scenarios.7
Results
The study covered 93.52% of Oskoo town population aged ≥30 years. We studied 18,637 male (M; 91.50% coverage) and 18,692 female (F; 95.52% coverage) participants. Figure 1 shows the age pyramid of the adults ≥ 30 years in both men and women. The summary of risk factors incidences are presented in Table 1. These risk factors incidences include: hypertension [SBP≥140 and DBP≥90 mmHg] =16.25%, pre-hypertension [SBP=120-139 and DBP=80-89 mmHg] =37.78%, diabetes mellitus [fast blood glucose (FBS) ≥126mg/dl] =7.45%, smoking=9.40%, hypercholesterolemia (>200mg/dl) =47.64% and obesity [body mass index (BMI) ≥27] = 50.47%. The prevalence of morbid obesity (BMI>30) in the present study in men was 18.2% and women was 37.2% (in total=27.6%).
Figure 1.
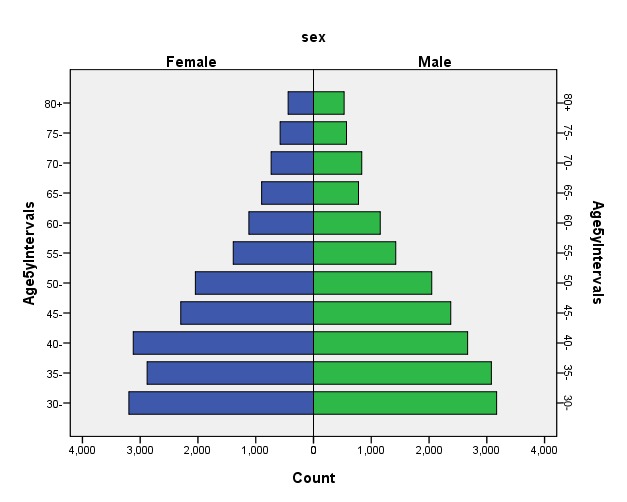
Age pyramid of Oskoo population≥30 years old in men and women (each bar is 5-year interval).
Table 1. Incidence of cardiovascular risk factors in Oskoo adults ≥30 years old.
| Men n=18637 |
Women n=18692 |
Total n=37329 |
|
| Hypertension (SBP≥140 or DBP≥90) |
15.35% | 17.29% | 16.25% |
| Diabetes Mellitus (FBS≥126mg/dl)a |
06.35% | 08.54% | 07.45% |
| Cigarette smoking | 17.00% | 01.57% | 09.40% |
| Hypercholesrolemia (>200mg/dl)b |
42.46% | 52.81% | 47.64% |
| Obesity (BMI≥27) | 38.79% | 62.09% | 50.47% |
a,bFast blood glucose (FBS) and cholesterol measurements were done in adults≥40 years old.
Blood pressure (BP) of all population aged ≥ 30 years were measured by standard protocol and recorded. The classification of stages of systolic and diastolic BP was done according to Chobanian et al. 9 definition(Table 2). One of the most important finding of this study is detecting the very high incidence of systolic and diastolic pre-hypertension in both men (41.38% and 28.31%, respectively) and women (34.18% and 27.20%, respectively; Table 3).
Table 2. Classification of Systemic Blood Pressure for Adults.
| Category | Systolic Blood Pressure (mm Hg) |
Diastolic Blood Pressure (mm Hg) |
| Normal | <120 | <80 |
| Pre-hypertension | 120–139 | 80–89 |
| Stage 1 hypertension | 140–159 | 90–99 |
| Stage 2 hypertension | ≥160 | ≥100 |
Reprinted with permission from Chobanian AV, et al: Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
Table 3. Incidence of pre-hypertension, hypertension stage 1 and 2* in Oskoo adults≥30 years old.
| Men | Women | Total | ||
| Systolic blood pressure |
Pre- hypertension |
41.38% | 34.18% | 37.78% |
| Stage 1 | 8.23% | 9.14% | 8.69% | |
| Stage 2 | 4.29% | 5.05% | 4.68% | |
| Diastolic blood pressure |
Pre- hypertension |
28.31% | 27.20% | 27.75% |
| Stage 1 | 7.75% | 8.87% | 8.31% | |
| Stage 2 | 3.84% | 4.43% | 4.14% |
Table 4 demonstrates the incidence of diabetes mellitus, smoking and obesity in different age groups (in 5 years intervals) in both genders. The incidences of DM and obesity gradually increased by advancing age from 30 to 75 years and then decreased in both gender. Women have higher incidences of DM and obesity in all age groups than men. The incidences of cigarette smoking in men were significantly higher among women in all age groups. Highest frequency of smoking in men were in age between 40-60 years old (about 20%) and in women in ages higher than 55 years old (about 2%; Table 4).
Table 4. Incidence of diabetes mellitus*, smoking and obesity in Oskoo adults≥30 years old.
| Diabetes mellitus (FBS≥126 mg/dl) |
Smoking | Obesity (BMI≥27) |
||||
| Age groups |
Men | Women | Men | Women | Men | Women |
| 30- | 1.8 | 1.6 | 13.75 | 1.06 | 26.5 | 58.3 |
| 35- | 2.4 | 3.3 | 15.80 | 1.13 | 33.4 | 68.9 |
| 40- | 4.0 | 4.6 | 20.61 | 1.08 | 44.2 | 67.5 |
| 45- | 4.9 | 7.4 | 21.03 | 1.94 | 50.1 | 68.6 |
| 50- | 5.9 | 10.0 | 19.64 | 1.66 | 49.5 | 66.6 |
| 55- | 9.1 | 10.6 | 19.30 | 2.39 | 43.9 | 58.7 |
| 60- | 9.6 | 13.5 | 13.31 | 2.20 | 45.8 | 49.4 |
| 65- | 7.3 | 9.8 | 14.36 | 2.22 | 38.0 | 46.9 |
| 70- | 9.0 | 14.8 | 15.19 | 2.09 | 31.6 | 40.3 |
| 75- | 5.6 | 9.0 | 10.60 | 1.95 | 28.0 | 39.4 |
| 80+ | 5.7 | 5.2 | 11.25 | 2.05 | 30.6 | 25.3 |
Fast blood sugar (FBS) was measured in adults≥40 years old.
The unique aspect of this survey was measuring of lipid profile in 17,388 adults aged more than 40 years that spent most of the study cost including total cholesterol, triglyceride, low density lipoprotein (LDL), and high density lipoprotein (HDL). Table 5 shows detail of incidences of dyslipidemia in different age groups in both genders. The incidences of dyslipidemia were distributed homogenously in all age groups. We faced high incidence of hypercholesterolemia, very high frequency of hypertriglyceridemia, relatively low incidence of “High LDL” and vey high frequency of “Low HDL” on both sex in all age groups. Women have higher incidences of hypercholesterolemia, hypertriglyceridemia and “High LDL” than men; however, men showed lower levels of HDL (and higher incidence of “Low HDL”). In this study, we considered cut-off point of 160 mg/dl for defining of “High LDL” and if regarding the cut-off point of 130 mg/dl in adults with more than two CVD risk factors and cut-off point of 100 mg/dl in diabetics, it is possible to obtain the higher incidence of “High LDL” in target population.
Table 5. Incidence of dyslipidemia in Oskoo adults ≥40 years old.
| Hypercholestrolemia (>200 mg/dl) |
Hypertriglyceridemia (>150 mg/dl) |
High LDL (>160 mg/dl) |
Low HDL | |||||
| Age groups | Men | Women | Men | Women | Men | Women | Men (≤40mg/dl) |
Women (≤50mg/dl) |
| 30- | 38.2 | 40.5 | 54.6 | 59.0 | 13.0 | 11.9 | 53.8 | 32.8 |
| 35- | 40.3 | 48.2 | 52.9 | 48.7 | 15.1 | 19.0 | 64.3 | 37.6 |
| 40- | 38.1 | 45.5 | 51.8 | 53.4 | 11.5 | 16.5 | 61.9 | 43.5 |
| 45- | 43.5 | 48.6 | 57.5 | 53.5 | 15.3 | 17.3 | 63.1 | 46.0 |
| 50- | 47.5 | 55.8 | 51.6 | 60.8 | 17.0 | 25.4 | 65.2 | 47.9 |
| 55- | 44.8 | 62.9 | 50.7 | 64.5 | 17.8 | 31.2 | 66.1 | 50.6 |
| 60- | 44.2 | 58.4 | 47.3 | 65.6 | 15.8 | 25.2 | 65.4 | 44.4 |
| 65- | 45.1 | 58.9 | 46.9 | 58.0 | 18.2 | 23.0 | 65.8 | 47.2 |
| 70- | 42.2 | 55.5 | 43.9 | 55.2 | 14.3 | 24.4 | 70.9 | 46.3 |
| 75- | 41.59 | 47.4 | 43.2 | 59.8 | 11.9 | 27.3 | 66.4 | 52.7 |
| 80+ | 32.9 | 50.8 | 42.4 | 57.8 | 13.7 | 18.9 | 63.7 | 38.1 |
Discussion
This study has examined the CVD risk factor status of urban and rural people aged 30 years old and over in Oskoo town in northwest Iran. In general, there was a high prevalence of CVD risk factors in particular, such as Obesity, high cholesterol, low-HDL cholesterol, and hypertension, especially in women.
About ninety percent of the world’s disease burden including CVD occurs in developing countries, while only ten percent of global health expenditure is assigned in these countries.4 About 78% of all NCD deaths occur in low and middle-income countries. CVD accounts for 48% of all NCD deaths and among the six WHO regions, the Eastern Mediterranean region has the highest CVD age-standardized mortality rate.4,10 The CVD has become a leading cause of death in under-developed states and rates are expected to increase further over the next years. In addition, it has been estimated that high blood pressure accounts for as much as five percent of the total death rate in developing countries, smoking for 4.0%, hypercholestrolemia for 2.1% and obesity for 2.7%.4
Hypertension
The prevalence of hypertension among Oskoo adults aged 30 and over was 16.25%, and higher in women (17.29%) than in men (15.35%). Our overall prevalence rates for hypertension were similar to Seyffarshad et al.11 study of CVD risk factors in East Azarbaijan province in 2007 that reported the incidence of 22.35% for HTN (Men=19.4% and women=21.9%). Sadeghi-Bazargani et al.6 also reported the similar prevalence rate of HTN (18.0%) from Ardabil in 2011. Our results were somewhat lower than that reported in other literature. Rodriguez-Ojea et al.12 in 2011 showed the prevalence of self –reported HTN in 23.5% of adults aged 45-60 years old and Bovet et al.4 reported the rate of 31.6% in Republic of Seychelles in east of Kenya. McDonald and Pickart 10 reported rate of 23% for HTN in Eastern Mediterranean adults with age 30 years old and over in low and middle-income population group in 2004. In an analysis, Perdigao et al.13 revealed that in Portugal, women reported high BP more often than men with prevalence of 23.2% and 16.1% in women and men, respectively.
Diabetes mellitus
In the present study the prevalence of DM was 7.45% (men=6.35 and women=8.54%). Seyffarshad et al.11 reported the prevalence rate of 5.52 for East Azerbaijan’s men and 4.64% in this province’s women. Bovet et al.4 showed the prevalence of 9.3% (men 9.6%; women 9.0%) in east African region. In our study women have higher rate of DM but these two surveys demonstrated the vice versa. The prevalence rates of diabetes in the Perdigao’s study 13 in different regions of Portugal were 4.6% to 8.9%. Comparing the prevalence rates of DM in East Azarbaijan province (Seyffarshad study11) in population 15-64 years old and our study of Oskoo adults aged ≥ 40 years, it is revealed that higher prevalence of DM in our study somewhat could be related to higher age of participants in Oskoo study.
In a report from all WHO regions (Africa, The Americas, Eastern Mediterranean, Europe, South-East Asia, and Western Pacific), in Eastern Mediterranean region, population with age 30 years old and over in low and middle-income groups in 2004, the prevalence of DM was highest (17%) among the regions; in other regions the prevalence of DM ranged between 4 to 9%. Africa showed the lowest prevalence (4%) but has the highest mortality rate for diabetes.10
Obesity
In the present study if the definition of the obesity was considered as BMI ≥27, then the rates were 38.79% in men and 62.09% in women (50.47% in total). However, in some studies the definition of obesity was BMI >30 and considering this cut-off point the prevalence rates of obesity in our study were 18.20% in men and 37.20% in women aged 30 years and over.
The overall prevalence rates of obesity and overweight population were similar to Hajian et al.14 study that reported the rates of 18.8% and 34.8% in men and women, respectively in urban population aged 20-70 years, in the north of Iran in 2007. In these two studies, the rate of obesity in women was higher in men. Also in these two surveys, in both genders, particularly in females, the rate of obesity was raised by increasing age.14 Sadeghi-Bazargani et al. reported the prevalence rate of overweight and obesity of 58.9% in Ardabil (northwest Iran) in 2011.6 Seyffarshad et al. reported the rate of obesity (BMI >30) 17.29 in women and 8.79 in men aged 15-64 years old in East Azarbaijan province in 2007.11 These rates lower than our study results even considering higher age of our study participants (30 years old). Rodriguez-Ojea et al. also reported the prevalence of obesity 23% in males and 45% females in an urban Cuban population aged 45-60 years, regarding the age group of participants; the results are similar to our findings.12
Smoking
The overall prevalence of current smokers was 9.4% (17.0% in men; 1.6% in women), and was lower than studies conducted with a similar methodology in East Azarbaijan (14.9% [20.3% in men; 1.1% in women]11 and also in neighboring provinces (15.7% [29.0% in men; 2.6% in women] in Ardabil)6 , as well as the country as a whole (19% [31% in men; 6% in women]).15
Farzadfar et al. in a national and sub-national survey reported the prevalence of smoking in different regions in Iran as follows: In southeast region was 25% (men=35%, women=14%); north and northeast was 20% (men=32%, women=7%); west 21% (men=33%, women=6%) and central region 17% (men=31%, women=3%).15 This study was done in 2011 according to registered data of 2005 and as presented above, all prevalence rates were higher than our study results in both genders.
Dyslipidemia
Comparison of hypercholesterolemia prevalence rates is complicated for reasons related to the criteria used to define it, the demographic structure of the studied population, and the methods used for diagnosis. For example, we defined hypercholesterolemia as levels >200 mg/dl while in other studies levels such as >190 mg/dl16 to levels >232 mg/dl10 or >240mg/dl11 were considered as cut-off values. In addition, some researchers report the prevalence rates from target population based on self-reporting of this variable, but the others, collect the data from blood samples of the participants.
In the present study in Oskoo population aged 40 years and over, the overall prevalence of hypercholesterolemia (>200 mg/dl) was 47.46%. Women had higher frequency of hypercholesterolemia (52.81%) than men (42.46%). In a 2003 systematic review of previous studies16, the proportion of individuals with total cholesterol ≥190 mg/dl was 64%, and in the study in the Central region of Portugal17, individuals with a mean age of 47±12 years, 46.7% had hypercholesterolemia that is similar to our findings.
Limitations
The present study had some limitations. It was a pilot study in a small city near Tabriz in northwest Iran. However, this study covered nearly all population≥30 years old and provided a complete database of the target population. It was also not a representative sample of East Azarbaijan province population but served as a pilot study of the application of epidemiological research methods and the determination of novel cardiovascular risk factor status in this province. For that reason, the conclusions are only valid for the population studied (i.e. adults aged ≥30 years old). This study was a cross-sectional study in nature, and therefore, no causal relationships can be directly assessed.
Conclusion
Considering high incidence of CVD risk factors (except smoking) in Oskoo rural and urban population aged 30 years and over, it is recommended that this pilot study should be expanded to all of East Azerbaijan province or could be conducted in other states with low-middle income. It is emphasized that free of charge taking blood samples from all people ≥ 40 years old to evaluate lipid profile and glucose levels is worthy to early detecting the undiagnosed and prevalent DM or DLP in this target population.
Acknowledgments
The study was funded by Cardiovascular Research Center, Tabriz University of Medical Sciences (Tabriz, Iran).
Footnotes
Ethical issues: Not applicable in this research.
Conflict of interests: No conflict of interest to be declared.
References
- 1.Global atlas on cardiovascular disease prevention and control (cited 2011 November) available from:http://www.who.int/cardiovascular_diseases/en/
- 2.Murray CJL, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Cambridge: Harvard University Press; 1996. [Google Scholar]
- 3.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H. et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bovet P, Shamlaye C, Gabriel A, Riesen W, Paccaud F. Prevalence of cardiovascular risk factors in a middle-income country and estimated cost of a treatment strategy. BMC Public Health. 2006;6:9. doi: 10.1186/1471-2458-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bozorgmanesh M, Hadaegh F, Sheikholeslami F, Azizi F. Cardiovascular risk and all-cause mortality attributable to diabetes: Tehran lipid and glucose study. J Endocrinol Invest. 2012;35:14–20. doi: 10.3275/7728. [DOI] [PubMed] [Google Scholar]
- 6.Sadeghi-Bazargani H, Jafarzadeh H, Fallah M, Hekmat S, Bashiri J, Hosseingolizadeh G. et al. Risk factor investigation for cardiovascular health through WHO STEPS approach in Ardabil, Iran. Vasc Health Risk Manag. 2011;7:417–24. doi: 10.2147/VHRM.S22727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO CVD-risk management package for low – and medium-resource settings (cited 2007 March) Available from:http://whqlibdoc.who.int/publications/2002/9241545852.pdf. [DOI] [PMC free article] [PubMed]
- 8.Bonita R, Decourten M, Dwyer T, Jamrozic K, Winkelmann R. Surveillance of risk factors for noncommunicable diseases: the WHO STEPwise approach. Geneva: World Health Organization; 2002. [Google Scholar]
- 9.Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F. et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health. 2009;9:167. doi: 10.1186/1471-2458-9-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonald M, Pickart F. The Global Burden of Noncommunicable Diseases. (cited 2011 December) Available from: http://www.pfizer.pt/Files/Billeder/Pfizer%20P%C3%BAblio/Not%C3%ADcias/Global%20Burden%20of%20Noncommunicable%20Diseases.pdf.
- 11.Seyffarshad M, Kousha A, Pourdowlati S, Karamouz M, Farahbakhsh M, Hakimi S. et al. Cardiac Risk Factor Analysis in East Azerbaijan, Iran. Cardiology. 2007;3:1–4. [Google Scholar]
- 12.Rodriguez-Ojea A, Alonso C, Yarnell JW, Woodside JV. Status of novel cardiovascular risk factor and cardiovascular disease risk in an urban Cuban population--a pilot study. J Health Popul Nutr. 2011;29:510–5. doi: 10.3329/jhpn.v29i5.8905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perdigão C, Rocha E, Duarte JS, Santos A, Macedo A. Prevalence and distribution of the main cardiovascular risk factors in Portugal--the AMALIA study. Rev Port Cardiol. 2011;30:393–432. [PubMed] [Google Scholar]
- 14.Hajian-Tilaki KO, Heidari B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20-70 years, in the north of Iran: a population-based study and regression approach. Obes Rev. 2007;8:3–10. doi: 10.1111/j.1467-789X.2006.00235.x. [DOI] [PubMed] [Google Scholar]
- 15.Farzadfar F, Danaei G, Namdaritabar H, Rajaratnam JK, Marcus JR, Khosravi A. et al. National and subnational mortality effects of metabolic risk factors and smoking in Iran: a comparative risk assessment. Popul Health Metr. 2011;9:55. doi: 10.1186/1478-7954-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Costa J, Borges M, Oliveira E, Gouveia M, Carneiro AV. Incidence and Prevalence of Hypercholesterolemia in Portugal:A Systematic Review. Part I. Rev Port Cardiol. 2003;22:569–77. [PubMed] [Google Scholar]
- 17.Santiago LM, Serra e Silva P. coronary heart disease risk: the result of population screening by the central region branch of the Portuguese heart foundation. Rev Port Cardiol. 2003;22:1039–48. [PubMed] [Google Scholar]


