Abstract
Introduction
Cardiovascular diseases are always one of the major causes of mortality in the world affecting all aspects of patients’ lives. Therefore, this study was conducted to summarize and provide a clear view of quality of life in these patients in Iran through a systematic review on the results of previously conducted studies.
Methods
In a systematic review, required information was collected by searching keywords of Iran, quality of life, heart failure, cardiac, heart, and their Persian equivalents in databases of Science Direct, Pubmed, IRAN doc, SID, Medlib and Magiran. The selected time period for searching articles was since 2000 to 2012. Inclusion criteria were: releasing of article during 2000 to 2012, articles reporting patients’ quality of life in any domains of heart diseases, and articles published in Persian and English. Extracted results first were summarized in Extraction Table, and then analyzed manually.
Results
Finally 18 of 1592 found articles were included in the study. A total of 3,797 cardiac patients' quality of life was measured using six different tools, the most important one of which was SF36 questionnaire. Among eight dimensions of SF36 questionnaire, the highest mean was for social role functioning with average score of 58.37 and the lowest for physical limitation (physical role functioning) with score of 42.95. Overall, mean of eight dimensions was 53.19. Among 4 general domains of quality of life, physical activity had the lowest average of 43.63 and average of general dimensions of quality of life was 47.65. The most important factors affecting quality of life were sex, age, education, marital status, occupational status, suffering duration, number of hospitalizations etc.
Conclusion
The results of the studies showed relatively low quality of life of cardiovascular patients in general. Therefore, according to the introduced effective factors in this study, it is necessary to consider regular programs for improving quality of life in these patients and providing suitable and qualitative services.
Keywords: Cardiovascular Patients, Quality of Life, Systematic Review Study, Iran
Introduction
Cardiovascular diseases are one of the most prevalent chronic diseases all around the world accounting for high rates of mortality and disability.1-3 Unfortunately, in spite of increase in developments in prevention, diagnosis, treatment, and rehabilitation of cardiac diseases, there is still a growing trend in mortality rate resulted from these diseases. Mortality rate resulted from these diseases was 10% of total mortality rate in 1910 but it increased to 50% in 2000 and it is predicted to increase to 75% by 2020.4
According to the statistics by World Health Organization (WHO), mortality and disability resulted from cardiovascular diseases and cerebrovascular accident kill more than 12 million people all around the world annually. Also this organization estimates that if no measures are taken to improve cardiovascular health, there will be a 25 percent loss in healthy life years due to the cardiovascular diseases by 2020 and the main part of this loss will be in developing countries.2 About 12 million people suffer from coronary artery disease in America; about 1.5 million people are afflicted by MI annually and also about 600 thousand people per year die of coronary artery diseases.5-7 Cardiovascular diseases are the most prevalent reason of mortality in our country.8
Conducted studies in Iran in 2003 showed that the first mortality reason in terms of number is death resulted from cardiovascular diseases and unintentional accidents come next. In the same year the number of mortality cases resulted from cardiovascular diseases was 72682 for males and 62068 for females and 134750 in total.9 This mortality rate included 35% of total mortality rate in our country.10,11 Also based on estimations, the lost years of life because of cardiovascular diseases are equal to 1183188 years (26% of total lost years) and burden of these diseases are about 1.5 million years.12,13 Beside mortality, disability and high disease burden, these diseases cause severe problems in psychological and social aspects of people’s lives.14,15 For this reason, caring approach of these patients should cover different aspects of their lives.16,17
Measuring and implementing effective steps in order to improve these patients’ quality of life is one of the most important items of these approaches .18,19 The quality of life is defined as perception of people of life, values, goals, standards, and interests.20 Also studies showed that quality of life could be considered as one of the most important components of quality of medical and health care.21 Many studies have been conducted in our country to evaluate quality of life in cardiovascular diseases.22-24 But to the point that studies’ results show, there is not any systematic review study in this field in our country able to summarize the results of these studies and to provide a general and clear cut perspective of patients’ quality of life. For this reason, this systematic review study has been conducted aiming to conclude and provide a general and clear view of the results of these studies to be used in planning and interventions.
Materials and methods
The required information for this systematic review were collected by searching keywords of Iran, quality of life, heart failure, cardiac, heart, and their Persian equivalents in data bases of Science Direct, Pubmed, IRAN DOC, SID, Medlib and Magiran. The selected time period for searching articles was since 2000 to 2012.The reason for choosing such a relatively short period was to control and minimize effect of time on patients’ quality of life, since it could be changed by time because of factors such as medical advancements, changing patients’ knowledge and information level, usage of more utilities, and many other factors. Therefore, by selecting such a relatively short time period the effects of these changes were minimized and subsequently patient quality of life will be more realistic.
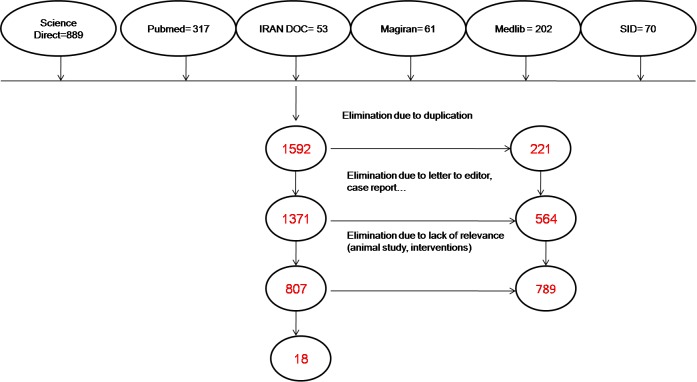
Inclusion criteria were: all articles published from 2000 to 2012, articles reporting patients’ quality of life in any domains of heart diseases, and articles published in Persian and English. Exclusion criteria were: letter to the editors, case reports, and articles presented in seminars and conferences, or resulted from implemented interventions and animal studies. In order to further recognition and coverage of published articles, some of leading journals in this field underwent hand searching after searching databases. After excluding those articles rarely related to the objectives of the study, and selecting main articles. References of selected articles were also searched so that much assurance about finding related articles could be gained. Among 1592 found articles those that had weak relevance to the objectives of the study and contained excluding criteria were eliminated and finally 18 totally related articles were included into the study and were later studied and evaluated (Figure 1). Three of 18 selected articles were published in English Journals. Articles were first categorized chronically and then studied accurately and after extracting the required information, results were summarized in Extraction Table at first and then were analyzed manually.
Figure 1.
Study selection flow diagram
Results
Overall, 1592 articles were found in searched referenses. After studying titles, abstracts, and full texts of articles, and excluding duplicated and irrelivant cases, 18 articles totally relevant to the objectives of the study were selected and evaluated. Among these articles, 3 were published in English journals. Most of the studies (7 cases) were conducted in Tehran. Mean of the conducting years of studies was the year 2009. In 18 investigated articles, totally quality of life for 3797 persons was evaluated and among these numbers, 2081 of cases (56.43%) were males. In investigated articles for evaluating patients quality of life, 6 different tools were used and Short Form Health Survey (SF-36) questionnaire and Minnesota (Minnesota Living with Heart Failure Questionnaire) were applied mostly with 13 and 3 times respectively.
SF-36
The SF-36 is one of the most widely used measures of health-related QOL consisting of 36 items and covering eight dimensions: physical functioning (PF), role limitations caused by physical health problems (RF), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role limitations caused by emotional health problems (RE), and mental health(MH).25 Scores on all the subscales are transformed linearly to a possible range of 0-100;higher scores indicate more favorable physical functioning/psychological well-being.26,27
Minnesota
The Minnesota Living with Heart Failure questionnaire (MLHF) was designed in 1984 to measure the effects of heart failure and for treatments heart failure on an individual’s quality of life.28,29 The content of the questionnaire was selected to be representative of the ways heart failure and treatments can affect the physical, emotional, social and mental aspects of quality of life without being too long to administer during clinical trials or practice. Responsiveness of the MLHF refers to its ability to detect changes in quality of life that clinicians and patients discern and believe to be important. An instrument ability to detect change depends, in part, on the amount of noise or measurement error inherent in repeated assessments. Changes in an individual’s score need to be 2.77 times the standard error of the measurement to be 95% confident that the observed change was not due to measurement error.30,31
Mean of cardiac patients’ quality of life based on eight items of SF36
In this study, scores of each one of octet dimensions of SF36 questionnaire were reported specifically in 8 articles. Mean of each one of dimensions has been showed in Figure 2.
Figure 2.
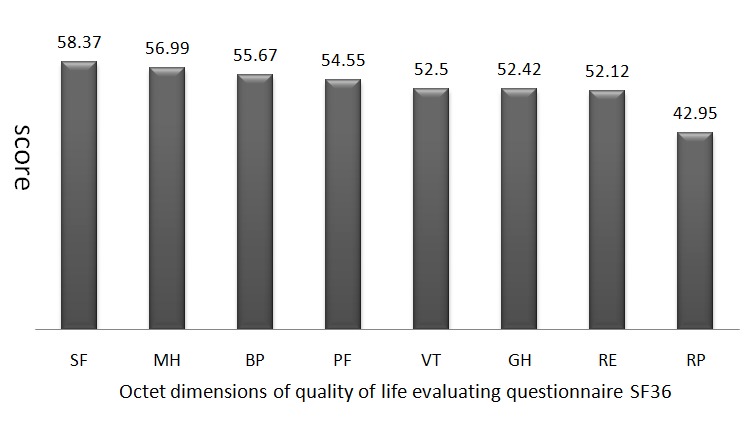
Mean of scores in octet dimensions of cardiovascular patients' quality of life in Iran based on SF36 questionnaire
As it is shown in this diagram, social role functioning with score of 58.37 and physical limitation (physical role functioning) with score of 42.95 have the highest and the lowest scores in octet dimensions for quality of life, respectively. Overall mean of these octet dimensions is 53.19.
Additionaly in a different classification, methods were carried out in investigated articles. Mean scores of quality of life in 4 general dimensions including general status, physical activity, social status, and mental status were obtained by collecting and combining classifications, and were shown in Figure 3.
Figure 3.
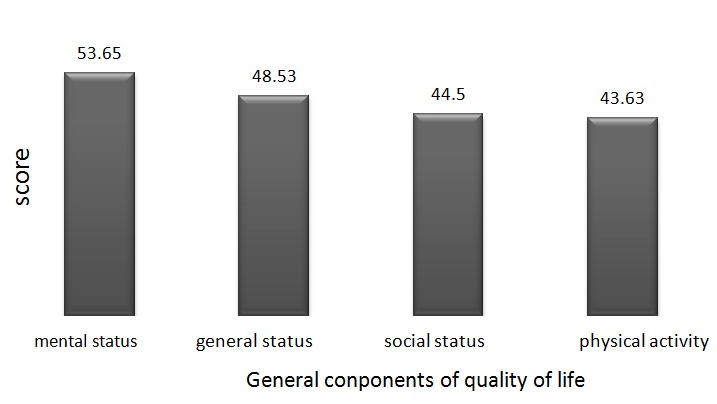
Mean of general dimensions of cardiovascular patients' quality of life in Iran
As it is shown in Figure 3 in general dimensions of life, dimension of mental status with average score of 53.65 and physical activity with average score of 43.63 are the highest and the lowest means respectively. Overall mean for general dimensions of quality of life is also 47.65.
Factors affecting quality of life
In investigated articles, different variables and factors have been reported to be effective on cardiac patients’ quality of life. Some of the most important caseshave been presented here after.
Sex
The role of sex has been considered as an effective factor in most of the investigated studies. Some of them showed signifcant relationship between sex and patients’ quality of life in a way that men’s quality of life is better in many aspects compared with that of women. This is more obvious of physical and mental function.23,32-39 Despite the significant relationship between sex and quality of life observed in most of studies, there was no significant relationship between sex and quality of life in some studies.24,40
Age
Age was one of studied variables that showed a significant relationship with quality of life in most of the studies. By increasing age, a significant decrease occurs in patients’ quality of life.23,33,37,41 Like the case of sex, there was no significant relationship between age and quality of life in some studies.40,42
Education, occupation, and marital status
Higher educational status, having a job, and being married hadsignificant relationship with improving some aspects in cardiac patients’quality of life in some studies.23,36,42 Similar to previously-mentioned variables , these variables also had not any significant relationship with patients’ quality of life in some studies.24
Background diseases and family history of disease
Suffering some background diseases (Hypertension, diabetes, Hyperlipidemia) and family history of heart diseases in some investigated studies had a significant relationship with patients’ quality of life. These conditions caused a significant decrease in patients’ quality of life .23,39,42
Suffering duration, hospitalization frequency
Suffering duration of cardiac disease and referring frequency or hospitalization frequency are of important factors in most of the studies that had significant relationship with decreasing patients’ quality of life .34,37,39
Other factors
It is noteworthy to mention some other factors affecting cardiac patient's quality of life such as patient's quality of sleeping, smoking, patients’ inadequate training on their disease, treatment method, cardiac ejection fraction, and social support level.40,43,44
Discussion
In this study, final 18 articles included total 1592. Totally, quality of life in 3797 patients was measured and reported using 6 different tools. The most important tool was SF36 questionnaire as firstly, it was a standard questionnaire frequently used in studies carried out in this field, and secondly, this tool has been indigenized in Iran and its reliability and validity been fulfilled. Among 8 items of SF36 questionnaire, social role functioning with average score of 58.37 had the highest mean, physical role functioning (physical limitation) with average score of 42.95 had the lowest mean, and overall mean for 8 components was 53.19. General components of quality of life were classified into 4 general domains among which mental status dimension had the highest mean with average score of 53.65 and mean for general components of quality of life equaled 47.65. The most important effective factors on quality of life included sex, age, education, marital status, occupational status, suffering duration, hospitalization frequently, etc.
Many studies have been conducted in the world on measuring cardiovascular patients’ quality of life and some of these studies have focused on systematic reviews of other studies in this field.45-48 Although some studies have been conducted in our country, the results of studies show that there is no systematic review study to collect the results of these studies and to provide a clear view of cardiovascular patients’ quality of life. Overall, mean values of 8 items of SF36 questionnaire and general components of quality of life show that cardiovascular patients’ quality of life is relatively low which is in agreement with results of most of the studies evaluating quality of life for cardiac patients.49-51 Also studies of Brown in England52, Norekval in Norway53, Rubenach in Australia54, Bengtsson in Sweden55, and other studies confirmed cardiovascular patients’ low quality of life; however, there are some studies in some parts of the world that show acceptable quality of life for cardiovascular patients. Veenstra et al. showed patients’ quality of life is favorable after heart attack.56 Study of Folcoze in France also showed this improvement.57 Patients’ low quality of life in our country is possibly related to low quality of provided services for cardiovascular patients and lack of social and economical supports of these people. Therefore, there is a need for improving quality of services and increasing supports for these people. Among 8 items of quality of life and 4 general components of cardiac patients’ quality of life, dimension of physical role functioning (RP) with scores of 42.95 and 43.63 had the lowest mean, respectively. In some other studies, physical problems and limitations had the lowest score.58-61 The cause of this fact could be resulted from patients ‘livelihood problems. Due to high prices of medical cares for cardiovascular diseases and inability of people to provide living costs due to their disease, some patients have to work hard which affects both their physical and mental functioning. Therefore, some supportive policies such as their insurance and low costs of provided cares should be considered for these patients.
In articles investigated in this study, many factors and variables related to cardiovascular patients’ quality of life were evaluated. The most important items included sex, age, education, marital status, occupational status, suffering duration, hospitalization frequencies, etc. In most of the studies, men’s quality of life was higher than that of women’s especially regarding physical and mental components and this is mentioned in most of the studies conducted in this field.62-65 In addition, Reynolds, Howes, and Riedinger showed in different studies that there is a significant relationship between sex and quality of life.66-68 Some of researchers consider this fact as a result of differences in biological and psychological characteristics of men and women. Also the reason of this fact especially in our society could be resulted from cultural differences, since men have more physical activity than women do and men are in communication with the society more than women are. Although hard physical activity could decrease the level of physical quality, lack of activity and functioning could also be a factor in decreasing physical quality of life. In evaluated studies, some items are reported as factors improving patients’ quality of life such as low age, high education, higher income, being married, having a job, no history of disease and background disease, limited frequency of referring to hospital, and low intensity of disease. The results of most conducted studies in this field confirm these items.69-71 In spite of significant relationship between above-mentioned factors, significant relationship could not be obtained in some studies40,58,72 which could be due to study environment or selected samples.
Although this was the first study in the country attempting to summarize and report the results of conducted studies on cardiovascular patients’ quality of life systematically, it faced some limitations. The most important limitation is that the study was not a meta-analysis study which is however difficult to conduct due to the different methods of information collection and reporting. Nevertheless, it is possible to show more clear results about status of these people’s quality of life through a meta-analysis study in this field. In spite of these limitations, in this study it was tried to identify all articles in this field by accurate and complete search. Furthermore, the procedure and required extracted information were controlled and supervised by statistics expert which increased the quality of the results.
Conclusion
Existence of accurate information and a clear view on patients’ quality of life have a significant role in improving supportive programs and preventive, remedial, and rehabilitative actions alongside with helping effective treatment. Nowadays, people seek for higher utilities with acceptable quality of life; therefore, governments all around the world try to reduce disease risk and to provide healthcare services and physical, mental, and social welfare for members of their societies. Investigating on the results of studies show that cardiovascular patients’ quality of life is relatively low in our country. Hence, there should be proper planning in order to increase these patients’ quality of life through more studies and paying attention to the factors mentioned in this study. Additionally, due to the low physical and mental components, there should be basic provisions for providing affordable health insurances, higher and cheaper welfare services, and proper social and mental supports to these people.
For future studies, it is suggested to conduct a study on recognition of quality of provided services to these patients and strategies to increase it. Clinical audit studies could be the best approach for this goal. Also it is suggested to conduct a study with qualitative approach (phenomenology) in this field in order to achieve better and deeper understanding about quality of life from patients’ point of view.
References
- 1.Braunwald S. Heart disease: a textbook ofcardiovascular medicines. 7th ed. Philadelphia: WB Saunders; 2005. [Google Scholar]
- 2.Campbell RL, Banner R, Konick-McMahan J, Naylor MD. Discharge planning and home follow-up of the elderly patient with heart failure. Nurs Clin North Am. 1998;33:497–513. [PubMed] [Google Scholar]
- 3.WHO. cardiovascular diseases. 2010 [cited 2010]; Available from: http://www.who.int/mediacentre/factsheets/fs317/en/index.html.
- 4.Thompson J, McFarland G, Hirsch J, Tucker S. Mosby’s Clinical Nursing. 5th ed. St. Louis: Mosby; 2002. [Google Scholar]
- 5.Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R. et al. Trends and disparities in coronary heart disease and other cardiovascular disease in the united states. Circulation. 2000;102:3137–47. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 6.Heart attack and angina statistics. American Heart Association; 2003 [cited 2006]; Available from: http.wikipedia.org/wiki/Heart_attack.
- 7.Phipps W, Sands J, Marek J. Medical surgical nursing: health and illness perspectives. 7th ed. St Louis: Mosby; 2003. [Google Scholar]
- 8.A national survey on health and diseases in iran. Thran- IRAN: Iranian Ministry of Health and Medical Eucation; 2000.
- 9.Nagavi M. The pattern of mortality within 23 provinces of Iran in 2003. Tehran-IRAN: Health Deputy, Iranian Ministry of Health; 2005.
- 10.Hosseinifar R. Epidemiology principle and cotrol of disease for nurses. Tehran: boshra publication; 2004. [Google Scholar]
- 11.WHO. Cause of death. Center for Global. Int Regional Studies (CGIRS) at the University of California Santa C. 2006. p. 120-4. [Google Scholar]
- 12.Naghavi M, Jafari N. Mortality in the 29 provinces of Iran in 2004. Tehran: Vice-chancellor for health, ministry of health and medical education; 2007. [Google Scholar]
- 13.The Burden of Disease and Injury in Iran. Tehran: Vice-chancellor for health, ministry of health and medical education; 2007. [Google Scholar]
- 14.Mayou RA, Gill D, Thompson DR, Day A, Hicks N, Volmink J. et al. Depression and anxiety as predictors of outcome after myocardial infarction. Psychosom Med. 2000;62:212–9. doi: 10.1097/00006842-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Westin L, Carlsson R, Israelsson B, WillIenheimer R, Cline C, McNeil T. Quality of life in patients with ischaemic heart disease: a prospective controlled study. J Intern Med. 1997;242:239–47. doi: 10.1046/j.1365-2796.1997.00203.x. [DOI] [PubMed] [Google Scholar]
- 16.Rakhshandero S, Ghaffari M. Quality of life. journal of health education. 2004;4:6–24. [Google Scholar]
- 17.Pashkow F, Dafoe W. Clinical cardiac rehabilitation. 2nd ed Baltimor: Williams &wilkin; 2000. [Google Scholar]
- 18.Simpson E, Pilote L. Quality of life after acute myocardial infarction: a comparison of diabetic versus non-diabetic acute myocardial infarction patients in Quebec acute care hospitals. Health Qual Life Outcomes. 2005;3:80. doi: 10.1186/1477-7525-3-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.King C, Hinds P. Quality of life from nursing perspectives. London: Jones & Bartlett; 1998. [Google Scholar]
- 20.Isikhan V, Guner P, Komurcu S, Ozet A, Arpaci F, Ozturk B. The relationship between disease features and quality of life in patients with cancer. Cancer Nurs. 2001;24:490–5. doi: 10.1097/00002820-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Daugherty C, Dewhurst W, Spertus J. Health related quality of life outcomes in clinical research. American Journal of Emidemiology. 1998;51:569–75. [Google Scholar]
- 22.Babaee J, Keshavarz M, Haidarni A, Shayegan M. Effect of a Heahth education Program on quality of life in patients undergoing coronary artery bypass surgery. Acta Media Iranica. 2007;45:69–74. [Google Scholar]
- 23.Esmaili A. Investigation of quality of life after open heart surgery in Sari. JMUMS. 2007;61:170–4. [Google Scholar]
- 24.Hasanpour-Dehkordi A, Delaram M, Foruzandeh N, Ganji F, Asadi Noghani A, Bakhsha F. et al. A survey on quality of life in patients with myocardial infarction, referred to Shahrekord Hagar hospital in 2005. Shahrekord university of medical sciences journal. 2007;9:78–84. [Google Scholar]
- 25.Steptoe A, Mohabir A, Mohan N, Mckenna W. Health related quality of life and psychological wellbeing patients with dilated cardiomyopathy. Heart. 2000;83:645–50. doi: 10.1136/heart.83.6.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ware JE Jr, Sherbourne CD. The MOS 36 item short form health survey (SF-36), conceptual Framework and item Selection. Med Care. 1992;30:473–81. [PubMed] [Google Scholar]
- 27.Montazeri A, Goshtasbi A, Vahdani Nia M. The short form health survey (SF-36): Translation and validation study of the Iranian version. payesh. 2005;5:49–56. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 28.Jaagosild P, Dawson NV, Thomas C, Wenger NS, Tsevat J, Knaus WA. et al. outcomes of Acute Exacerbation of severe Congestive hearth failure: quality of life resource Use and Survival. Arch Intern Med. 1998;158:1081–9. doi: 10.1001/archinte.158.10.1081. [DOI] [PubMed] [Google Scholar]
- 29.Abbasi A, Nasiri H. An Instrument of quality of life Measurement in Heart Failure Patients. J Gorgan Bouyeh Fac Nurs Midwifery. 2006;10:40–5. [Google Scholar]
- 30.Bennet SJ, Oldridge NB, Eckert GJ, Embree JL, Browning S, Hou N. et al. Discriminant properties of commonly used quality of life measures in heart failure. Qual Life Res. 2002;11:349–59. doi: 10.1023/a:1015547713061. [DOI] [PubMed] [Google Scholar]
- 31.Parajon T, Lupon J, Gonzalez B, Urrutia A, Altimir S, Coll R. et al. [Use of the Minnesota Living With Heart Failure Quality of Life Questionnaire in Spain] Rev Esp Cardiol. 2004;57:155–60. [PubMed] [Google Scholar]
- 32.Taghipour H, Naseri M, Safiarian R, Dadjoo Y, Pishgoo B, Mohebbi H. Quality of Life One Year after Coronary Artery Bypass Graft Surgery. Iran Red Crescent Med J. 2011;13:171–7. [PMC free article] [PubMed] [Google Scholar]
- 33.Beyranvand M, Lorvand A, Alipour Parsa S, Motamedi M, Kolahi A. The quality of life after first acute myocardial infarction. Phaghohandeh. 2011;15:264–72. [Google Scholar]
- 34.Taghadosi M, Gilasy H. The general and specific quality of life in patients with Ischemia in Kashan. Journal of Nursing Research. 2008;3:39–46. [Google Scholar]
- 35.Montazer Ghaem H, Asar O, Safaei N. Assessing patient's quality of life after open hart surgery in Bandar Abbass, Iran. Hormozgan Univercity of Medical Science Journal. 2011;15:254–59. [Google Scholar]
- 36.Yousefi P, Sabzevari S, Mohammadalizade S, Haghdoost A. Study of quality of life in heart failure hospitalized patients in Kerman medical university hospital in 2008. Journal of Nursing Research. 2011;6:59–67. [Google Scholar]
- 37.Shojaei F. An investigation quality of life of patients affected with heart failure. J Tehran Univ Med Sci. 2008;2:5–14. [Google Scholar]
- 38.Abedi H, Yasamanalipur M, Abdeyazdan G. Quality of Life in heart failure patients referred to the Kerman outpatient centers;2010. Journal of Shahrekord University of Medical Sciences. 2011;13:55–63. [Google Scholar]
- 39.Hatmi ZN, Shaterian M, Kazemi M. Quality of life in patients hospitalized with heart failure: a novel two questionnaire study. Acta Medica Iranica. 2007;45:469–76. [Google Scholar]
- 40.Hsanpour-Dehkordi A. Factors Influencing Quality of Life in Patients with Myocardial Infraction. IJN. 2009;22:43–52. [Google Scholar]
- 41.Abbasi A, Asayesh H, Hosseini A, Ghorbani A, Rohi G, Rahmani H. The relation of functional ability of patients affected with heart failure and quality of life. Iran South Med J. 2010;1:31–40. [Google Scholar]
- 42.Rahnavard Z, Zolfaghari M, Kazem-Nejad M, Hatamipour K. An investigation quality of life and factors affecting it in patients with heart congestive failure. Hayat. 2006;12:77–86. [Google Scholar]
- 43.Cheraghi M, Davari Dolatabadi E, Salavati M, Moghimbeigi A. Association between Perceived Social Support and Quality of Life in Patients with Heart Failure. IJN. 2012;25:21–31. [Google Scholar]
- 44.Behrouzifar S, Zenouzi S, Nezafati M, Esmaili H. Factors Affecting the Patients’ Quality of Life after Coronary Artery Bypass Graft. IJN. 2009;22:31–41. [Google Scholar]
- 45.Lü MJ, Zhang HY, Zhang Z, Yang GL. [Measurement of health-related quality of life in coronary heart disease: a review] Zhong Xi Yi Jie He Xue Bao. 2011;9:1277–85. doi: 10.3736/jcim20111201. [DOI] [PubMed] [Google Scholar]
- 46.Sbruzzi G, Dal Lago P, Ribeiro RA, Plentz RDM. Inspiratory muscle training and quality of life in patients with heart failure: Systematic review of randomized trials. Int J Cardiol. 2012;156:120–1. doi: 10.1016/j.ijcard.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 47.Elliott VJ, Rodgers DL, Brett SJ. Systematic review of quality of life and other patient-centred outcomes after cardiac arrest survival. Resuscitation. 2011;82:247–56. doi: 10.1016/j.resuscitation.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 48.Liu Z, Doan QV, Blumenthal P, Dubois RW. A Systematic Review Evaluating Health-Related Quality of Life, Work Impairment, and Health-Care Costs and Utilization in Abnormal Uterine Bleeding. Value Health. 2007;10:183–94. doi: 10.1111/j.1524-4733.2007.00168.x. [DOI] [PubMed] [Google Scholar]
- 49.Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W. et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87:235–41. doi: 10.1136/heart.87.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jaarsma T, Halfens R, Huijer Abu-Saad H, Dracup K, Gorgels T, van Ree J. et al. Effects of education and support on self-care and resource utilization in patients with heart failure. Eur Heart J. 1999;20:673–82. doi: 10.1053/euhj.1998.1341. [DOI] [PubMed] [Google Scholar]
- 51.Wielenga RP, Erdman RA, Huisveld IA, Bol E, Dunselman PH, Baselier MR. et al. Effect of exercise training on quality of life in patients with chronic heart failure. J Psychosom Res. 1998;45:459–64. doi: 10.1016/s0022-3999(97)00309-7. [DOI] [PubMed] [Google Scholar]
- 52.Brown N, Gray D, Young T, Munro J, Skene A, Hampton J. Quality of life four years after acute myocardial infarction: short form 36 scores compared with a normal population. Heart. 1999;81:352–8. doi: 10.1136/hrt.81.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Norekvål TM, Wahl AK, Fridlund B, Nordrehaug JE, Wentzel-Larsen T, Hanestad BR. Quality of life in female myocardial infarction survivors: a comparative study with a randomly selected general female population cohort. Health Qual Life Outcomes. 2007;5:58. doi: 10.1186/1477-7525-5-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rubenach S, Shadbolt B, McCallum J, Nakamura T. Assessing health-related quality of life following myocardial infarction: Is the SF-12 useful? J Clin Epidemiol. 2002;55:306–9. doi: 10.1016/s0895-4356(01)00426-7. [DOI] [PubMed] [Google Scholar]
- 55.Bengtsson I, Hagman M, Währborg P, Wedel H. Lasting impact on health-related quality of life after a first myocardial infarction. Int J Cardiol. 2004;97:509–16. doi: 10.1016/j.ijcard.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 56.Veenstra M, Pettersen K, Rollag A, Stavem K. Association of changes in health-related quality of life in coronary heart disease with coronary procedures and sociodemographic characteristics. Health Qual Life Outcomes. 2004;2:56–90. doi: 10.1186/1477-7525-2-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Falcoz PE, Chocron S, Laluc F, Puyraveau M, Kaili D, Mercier M. et al. Gender analysis after elective open heart surgery: a two-year comparative study of quality of life. Ann Thorac Surg. 2006;81:1637–43. doi: 10.1016/j.athoracsur.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 58.Collins E, Langbein W, Dilan-Koetje J, Bammert C, Hanson K, Reda D. Effects of exercise training on aerobic capacity and quality of life in individuals with heart failure. Heart Lung. 2004;33:154–61. doi: 10.1016/j.hrtlng.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 59.Hägglund L, Boman K, Olofsson M, Brulin C. Fatigue and health-related quality of life in elderly patients with and without heart failure in primary healthcare. Eur J Cardiovasc Nurs. 2007;6:208–15. doi: 10.1016/J.EJCNURSE.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 60.Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure. Review and analysis. Eur J Heart Fail. 2005;7:592–603. doi: 10.1016/j.ejheart.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 61.Hobbs FD, Kenkre JE, Roalfe AK, Davis RC, Hare R, Davies MK. Impact of heart failure and left ventricular systolic dysfunction on quality of life: a cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur Heart J. 2002;23:1867–76. doi: 10.1053/euhj.2002.3255. [DOI] [PubMed] [Google Scholar]
- 62.Kristofferzon ML, Löfmark R, Carlsson M. social support and quality of life over time after myocardial infarction. J Adv Nurs. 2005;52:113–24. doi: 10.1111/j.1365-2648.2005.03571.x. [DOI] [PubMed] [Google Scholar]
- 63.Pettersen KI, Reikvam A, Rollag A, Stavem K. Understanding sex differences in health-related quality of life following myocardial infarction. Int J Cardiol. 2008;130:449–56. doi: 10.1016/j.ijcard.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 64.Simpson E, Pilote L. Quality of life after acute myocardial infarction: a comparison of diabetic versus non-diabetic acute myocardial infarction patients in Quebec acute care hospitals. Health Qual Life Outcomes. 2005;3:80. doi: 10.1186/1477-7525-3-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cline CM, Willenheimer RB, Erhardt LR, Wiklund I, Israelsson BY. Health-related quality of life in elderly patients with heart failure. Scand Cardiovasc J. 1999;33:278–85. doi: 10.1080/14017439950141524. [DOI] [PubMed] [Google Scholar]
- 66.Reynolds MR, Lavelle T, Essebag V, Cohen D, Zimetbaum P. Influence of age, sex, and atrial fibrillation recurrence on quality of life outcomes in a population of patients with new-onset atrial fibrillation: the fibrillation registry assessing costs, therapies, adverse events and lifestyle (FRACTAL) study. Am Heart J. 2006;152:1097–103. doi: 10.1016/j.ahj.2006.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Howes CJ, Reid MC, Brandt C, Ruo B, Yerkey MW, Prasad B. et al. Exercise tolerance and quality of life in elderly patients with chronic atrial fibrillation. J Cardiovasc Pharmacol Ther. 2001;6:23–9. doi: 10.1177/107424840100600103. [DOI] [PubMed] [Google Scholar]
- 68.Riedinger MS, Dracup KA, Brecht ML, Padilla G, Sarna L, Ganz PA. Quality of life in patients with heart failure: do gender differences exist? Heart Lung. 2001;30:105–16. doi: 10.1067/mhl.2001.114140. [DOI] [PubMed] [Google Scholar]
- 69.Stewart S, Blue L. Improving outcomes in chronic heart failure. A practical guide to specialist nurse intervention. London: BMJ; 2001. [Google Scholar]
- 70.Meeks S, Murrell SA. Contribution of education to health and life satisfaction in older adults mediated by negative affect. J Aging Health. 2001;13:92–119. doi: 10.1177/089826430101300105. [DOI] [PubMed] [Google Scholar]
- 71.Gott M, Barnes S, Parker C, Payne S, Seamark D, Gariballa S. et al. Predictors of the quality of life of older people with hear failure recruited from primary care. Age ageing. 2006;35:172–7. doi: 10.1093/ageing/afj040. [DOI] [PubMed] [Google Scholar]
- 72.Humphries KH, Kerr CR, Connolly SJ, Klein G, Boone JA, Green M. et al. New-onset atrial fibrillation: sex differences in presentation, treatment, and outcome. Circulation. 2001;103:2365–70. doi: 10.1161/01.cir.103.19.2365. [DOI] [PubMed] [Google Scholar]