Abstract
Introduction: Various methods have been recommended to prevent hemodynamic instability caused by propofol induction. Current study evaluates hemodynamic effects of ketamine and propofol in comparison to etomidate and propofol during anesthesia induction.
Methods: Sixty-two patients over 50 years old undergoing elective surgeries were randomly assigned to ketamine + propofol (ketofol) (n=30) and etomidate + propofol (etofol) (n=32) groups. Patients in ketofol group were induced with ketamine 0.75 mg/kg and propofol 1 mg/kg. In etofol group, induction was performed with etomidate 0.2 mg/kg and propofol 1 mg/kg. Hemodynamic states before and after induction, first, third and sixth minutes after intubation were measured and compared between groups.
Results: There was no difference between groups in systolic (SAP), diastolic (DAP) and mean arterial pressure (MAP), heart rate (HR) and blood oxygen saturation (SaO2). There was significant decrease in SAP, DAP and MAP after induction and 6 minutes after intubation and in HR after induction than values before induction. There was significant increase in SaO2 in all evaluated periods than before induction in etofol group; however, the difference in ketofol group was not significant.
Conclusion: Both methods of induction -ketamine + propofol and etomidate + propofol- are effective in maintaining hemodynamic stability and preventing hemodynamic changes due to propofol administration.
Keywords: Ketamine, Etomidate, Intubation, Hemodynamic
Introduction
Patient safety has always been a major concern for the physicians of both ancient and modern eras.1 Propofol is a widely administered hypnotic agent that is of unique advantages yet some disadvantages.2-4 Induction of anesthesia with propofol is associated with significant blood pressure reduction and hemodynamic instability especially in patients over 50 years old. In patients with previous hypotension and those with American society of anesthesiologists’ physical status (ASAPS)>II, this drop is more dramatic.3,5 Geriatric patients do require different medical and surgical settings.6 Blood pressure instability in young patients due to propofol administration at different stages of the operation may not have any clinical value, but in older patients and special surgeries it is of great importance to maintain stable hemodynamics both throughout and after the surgery.
Ketamine is used for both induction and maintenance of general anesthesia. Ketamine is known to preserve respiratory drive, and its sympathomimetic properties result in an increase in blood pressure and heart rate making it an appropriate choice for cases in which decrease in heart rate and blood pressure is feared; for instance old patients with compromised cardiac conditions.7,8 The combination of propofol and ketamine for total intravenous anesthesia was shown to minimize the side effects of each drug used alone. Total intravenous anesthesia with propofol and ketamine proved to be very satisfactory from a clinical point of view.9
Etomidate, however, is an anesthesia induction agent with minimal cardiovascular side effects making it especially useful for cardiac-compromised patients and for those in whom hypotension must be avoided during induction of anesthesia.10,11
In this study, we aim to evaluate hemodynamic changes during induction with ketamine + propofol and etomidate + propofol combination in order to find proper drugs establishing more stable hemodynamic.
Materials and methods
In this double blinded randomized clinical trial, 62 patients (>50 years old) undergoing elective general, urology and orthopedic surgeries in Imam Reza Hospital, Tabriz, Iran during 2011 were selected. Those patients with other type of surgery, emergency surgery, pregnant women, addicted to drugs, patients that received sedative and anti-psychotic drugs in the last month and those with personality disorder, obese patients and patients with contraindications to etomidate, ketamine or propofol administration were excluded. Patients were blinded to the induction therapy. Anesthesiologist measuring hemodynamic changes was also blinded. Another anesthesiologist was aware of the induction drugs and performed all stages of the induction.
All patients were NPO for at least 8 hours before surgery and received 1 ml/kg normal saline (NPO deficit) per each NPO hour before induction as a part of fluid therapy in addition to the crystalloids used for the maintenance throughout the operation. All patients received fentanyl (1 mcg/kg), midazolam (0.03 mg/kg) 12 and lidocaine (1 mg/kg) intravenously 13 as premedication. Then patients were randomly assigned into groups receiving ketamine + propofol (ketofol) (n=32) and etomidate + propofol (etofol) (n=32). In ketofol group, patients were induced with 0.75 mg/kg ketamine and 1 mg/kg propofol. Etofol group was induced with 0.2 mg/kg etomidate and 1 mg/kg. All patients received 0.5 mg/kg atracorium for muscle relaxation. Standard capnography was used for all patients.
Demographic findings were recorded for each patient. Hemodynamic variables including systolic and diastolic blood pressure (SAP, DAP), mean blood pressure (MAP), heart rate (HR) and O2 saturation (SaO2) were measured before induction, after induction, one and three minutes after intubation. Findings were compared between groups.
Statistical analysis
Sample size (60 people) was calculated based on the formula and α=0.05 and d=0. 12). Randomization was achieved using Randomly Permuted blocks and software "research randomizer" at http://www.randomizer.org. Continuous data with normal distribution are given as mean ± standard deviation, otherwise as median, Independent t-test for testing the significance of mean for independent continuous scale (of normal distribution) data, Mann-Whitney for the significance of mean for non-normal distribution data, Chi-squared or Fisher exact test for testing the significance of percentages (qualitative data) were used. Hemodynamic changes during time were compared between groups by repeated measure of ANOVA (for normal distribution), Friedman nonparametric test for the significance of non-normal distribution data approach with treatment group and time as the between- and within-group factors. A p value <0.05 was considered significant. Statistical analyses were performed using the Statistical Package for Social Sciences, version 16.0 (SPSS, Chicago, Illinois).
Results
Demographic characteristics of patients in both groups are shown in Table 1. Both groups were matched regarding basic characteristics (P>0.05).
Table 1. Basic characteristics of patients in both groups .
| Ketofol (n=30) | Etofol (n=32) | P-value | ||
| Age (years) | 65.97±9.31 | 63.90±10.05 | 0.41 | |
| Gender | Male | 16 (53.3%) | 21 (65.6%) | 0.43 |
| Female | 14 (46.7%) | 11 (34.4%) | ||
| Weight (kg) | 73.48±8.98 | 72.00±10.73 | 0.57 | |
| Surgery time (min) | 140.00±58.73 | 169.53±65.82 | 0.06 | |
| ASA | I | 6 (20%) | 4 (12.5%) | 0.31 |
| II | 22 (73.3%) | 22 (68.8%) | ||
| III | 2 (6.7%) | 6 (18.8%) |
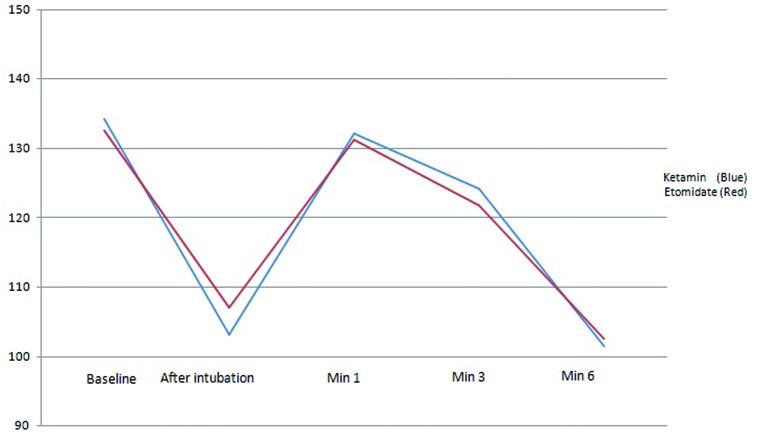
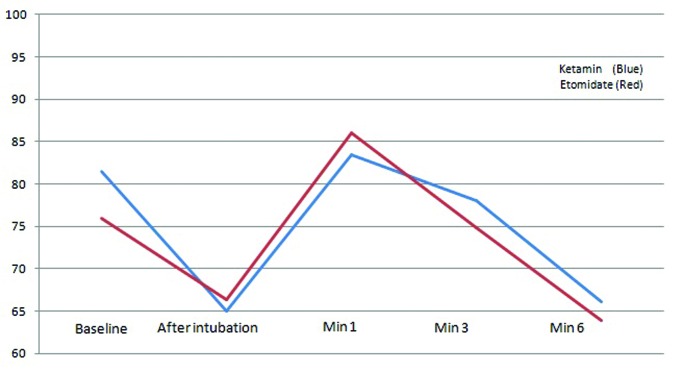
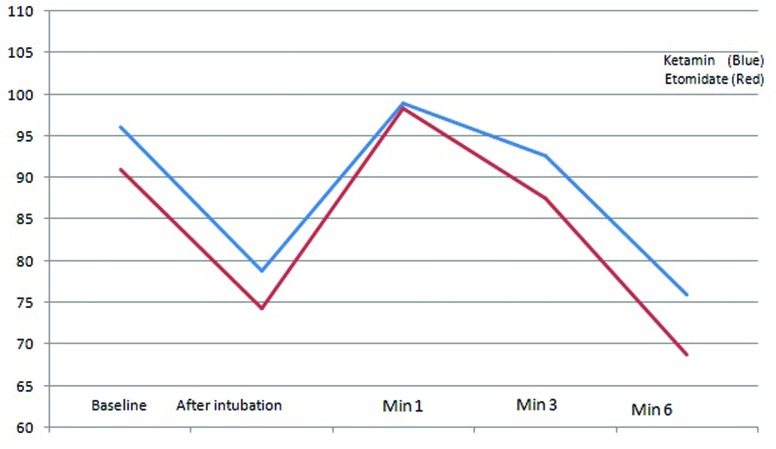
There were no significant differences regarding SAP at any stages between groups. However, repeated measure of ANOVA showed that SAP changes during time were significant in each group separately (P<0.001) (Figure 1). No significant difference regarding DAP could be detected at any stages between groups. However, repeated measure of ANOVA showed that DAP changes during time were significant in each group separately (P<0.001; Figure 2). A significant reduction was observed in MAP after induction in both groups (P<0.001), however the difference between two groups was not significant (Figure 3).
Figure 1 .
The trend of the changes in systolic arterial pressure (SAP) before induction, intubation and different stages after induction of anesthesia (1, 3 and 6 minutes) in both groups
Figure 2 .
The trend of the changes in diastolic arterial pressure (DAP) before induction, intubation and different stages after induction of anesthesia (1, 3 and 6 minutes) in both groups
Figure 3 .
The trend of the changes in mean arterial pressure (MAP) before induction, intubation and different stages after induction of anesthesia (1, 3 and 6 minutes) in both groups
Changes in HR after induction of anesthesia were significant in both groups (P<0.05); however, unlike etofol group, there was a significant increase followed by a decrease in HR one and six minutes after intubation in ketofol group respectively (P<0.05; Figure 4) which could be explained by the inotropic characteristics of ketamine. HR changes were significant in each group at different stages following intubation (P <0.001; Figure 2); however, there was no overall difference between two groups regarding HR changes suggesting the fact that both combinations are suitable to be used in patients with cardiac considerations.
Figure 4 .
The trend of the changes in heart rate (HR) before induction, intubation and different stages after induction of anesthesia (1, 3 and 6 minutes) in both groups
Changes in Sao2 were not significant at any stages between groups. There was a significant increase in Sao2 after induction and 1-6 minutes after intubation than those before induction in etofol group (P <0.05); however, these differences in ketofol group were not significant.
Discussion
Different ages of patients do require different anesthesia concerns in every day practice for anesthesiologists.14 Hemodynamic changes due to anesthesia in various surgeries have become a great concern in physicians of operation room and evidence show that changes in blood pressure, either increase or decrease, independently are associated with side effects and complications in patients undergoing surgery.15 All methods used in anesthesia induction are designed so that the hemodynamic stability is maintained especially in older patients that the need for surgery is increasing and complications of anesthesia are higher.16
Ketamine and etomidate both are drugs with least undesirable effects on hemodynamic changes and could be used with propofol to reduce its undesirable effects. In this clinical trial, we studied effects of ketamine + propofol and etomidate + propofol use for induction of anesthesia on hemodynamic variables. Consequently there was significant decrease in SAP, DAP and MAP after induction and 3-6 minutes after intubation in ketofol group. Kamalipour and coworkers also reported significant decrease after induction of anesthesia in patients inducted with ketamine and propofol.17 This finding indicates that the dose of Ketamine administered during the induction of anesthesia may not be high enough to neutralize the cardio-depressant effect of propofol. Unlike our findings, Bawja and coworkers 18 reported minimal increase in SAP and DAP after induction which slowly reduced to normal values, these minimal changes was proposed to be due to antagonistic properties of propofol (decrease in blood pressure) and ketamine (increase in blood pressure).
We also observed a significant decrease in HR after induction and 6 minutes after intubation and an increase 1 minute after intubation in ketofol group. Similar to our findings, Mi and coworkers 19 reported a decreasing trend of HR in patients induced using ketamine and propofol. However, other reports indicated an increase in HR after induction with ketamine and propofol.18,20 Also in the available only study evaluating effects of ketamine and propofol in old patients, significant increase in HR after induction was reported.17 Increase in heart rate with propofol and ketamine is explained on the basis of cardio stimulant effect of ketamine and stress response during intubation.18 However, the decrease in HR in our study may be due to the difference in the dose of ketamine used in different studies and gentle intubation that would prevent stress response. However, we did not study HR after induction and after intubation separately.
In our study there were no changes in SaO2 after induction with values of 95% in ketofol group which is in line with the other studies reporting similar findings.18,20
In this study, also there was significant decrease in SAP, DAP and MAP after induction and 6 minutes after intubation and significant increase in SaO2 after induction and intubation. We found only one study evaluating effect of etomidate and propofol on hemodynamic changes after induction and intubation.21 Saricaoglu and coworkers 21 observed no reduction in MAP and SAP in comparison to basic values. These results are indicative of hemodynamic stability after induction with etofol.
In our study we found no difference in SAP, DAP, MAP, HR and SaO2 after induction and intubation between groups. Due to these results we can consider similar results for ketamine + propofol and etomidate + propofol in establishing hemodynamic stability in old patients.
Conclusion
Results of current study indicated that induction with both ketamine + propofol and etomidate + propofol are both effective in maintaining hemodynamic stability and preventing hemodynamic changes due to propofol administration.
Acknowledgments
This research was financially supported by Vice Chancellor for Research, Tabriz University of Medical Sciences, Iran. The authors are indebted to Cardiovascular Research Center, Tabriz University of Medical Sciences, Tabriz, Iran for its support.
Footnotes
Ethical issues: The study was approved by the institutional review board, and written informed consent was obtained from all participants.
Competing interests: The authors had no competing interests to declare in relation to this article.
References
- 1.Golzari SE, Khan ZH, Ghabili K, Hosseinzadeh H, Soleimanpour H, Azarfarin R. et al. Contributions of medieval Islamic physicians to the history of tracheostomy. Anesth Analg. 2013;116:1123–32. doi: 10.1213/ANE.0b013e3182884313. [DOI] [PubMed] [Google Scholar]
- 2.Soleimanpour H, Rajaei Ghafouri R, Taheraghdam A, Aghamohammadi D, Negargar S. et al. Effectiveness of intravenous Dexamethasone versus Propofol for pain relief in the migraine headache: A prospective double blind randomized clinical trial. BMC Neurol. 2012;12:114. doi: 10.1186/1471-2377-12-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhungana Y, Bhattarai BK, Bhadani UK, Biswas BK, Tripad M. Prevention of hypotension during propofol induction: A comparison of preloading with 3.5% polymers of degraded gelatin and intravenous ephedrine. Nepal Med Coll J. 2008;10:16–9. [PubMed] [Google Scholar]
- 4.Reich DL, Hossain S, Krol M, Baez B, Patel P, Bernstein A. et al. Predictors of hypotension after induction of general anesthesia. Anesth Analg. 2005;101:622–8. doi: 10.1213/01.ANE.0000175214.38450.91. [DOI] [PubMed] [Google Scholar]
- 5.Yamaura K, Hoka S, Okamoto H, Kandabashi T, Akiyoshi K, Takahashi S. Changes in left ventricular end-diastolic area, end-systolic wall stress, and fractional area change during anesthetic induction with propofol or thiamylal. J Anesth. 2000;14:138–42. doi: 10.1007/s005400070021. [DOI] [PubMed] [Google Scholar]
- 6.Golzari SE, Ghabili K. Geriatric issues after recent twin earthquakes in northwest Iran. J Am Geriatr Soc. 2013;61:308–9. doi: 10.1111/jgs.12113. [DOI] [PubMed] [Google Scholar]
- 7.Mankikian B, Cantineau JP, Sartene R, Clergue F, Viars P. Ventilatory pattern and chest wall mechanics during ketamine anesthesia in humans. Anesthesiology. 1986;65:492–9. doi: 10.1097/00000542-198611000-00007. [DOI] [PubMed] [Google Scholar]
- 8.White PF, Way WL, Trevor AJ. Ketamine-its pharmacology and therapeutic uses. Anesthesiology. 1982;56:119–36. doi: 10.1097/00000542-198202000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Singh Bajwa SJ, Bajwa SK, Kaur J. Comparison of two drug combinations in total intravenous anesthesia: Propofol-ketamine and propofol-fentanyl. Saudi J Anaesth. 2010;4:72–9. doi: 10.4103/1658-354X.65132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liou CM, Hung WT, Chen CC, Hsu SC, Lau HK. Improving the success rate of laryngeal mask airway insertion during etomidate induction by using fentanyl or succinylcholine. Acta Anaesthesiol Taiwan. 2004;42:209–13. [PubMed] [Google Scholar]
- 11.Lui PW. Is etomidate–fentanyl or etomidate–succinylcholine combination suitable for the insertion of laryngeal mask airway? Acta Anaesthesiol Taiwan. 2004;42:183–4. [PubMed] [Google Scholar]
- 12.Sokouti M, Golzari S, Aghdam BA. Surgery of uncomplicated pulmonary hydatid cysts: Capitonnage or uncapitonnage? Int J Surg. 2011;9:221–4. doi: 10.1016/j.ijsu.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Soleimanpour H, Hassanzadeh K, Vaezi H, Golzari SE, Mehdizadeh Esfanjani R, Soleimanpour M. Effectiveness of intravenous lidocaine versus intravenous morphine for patients with renal colic in the emergency department. BMC Urol. 2012;12:13. doi: 10.1186/1471-2490-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azarfarin R, Seyedhejazi M, Golzari SE, Bilehjani E, Ghabili K, Alizadehasl A. Do pediatric patients undergoing cardiac surgeries require larger-size cuffed endotracheal tubes? A prospective study. Paediatr Anaesth. 2013;23:228–32. doi: 10.1111/pan.12112. [DOI] [PubMed] [Google Scholar]
- 15.Felfernig M, Andel D, Weintraud M, Connor D, Andel H, Blaicher AM. Postoperative vigilance in patients with total intravenous anaesthesia with ketamine/propofol. J R Nav Med Serv. 2006;92:64–8. [PubMed] [Google Scholar]
- 16.Passot S, Servin F, Pascal J, Charret F, Auboyer C, Molliex S. A Comparison of Target- and Manually Controlled Infusion Propofol and Etomidate/Desflurane Anesthesia in Elderly Patients Undergoing Hip Fracture Surgery. Anesth Analg. 2005;100:1338–42. doi: 10.1213/01.ANE.0000149542.04833.55. [DOI] [PubMed] [Google Scholar]
- 17.Kamalipour H, Joghataie P, Kamali K. Comparing the Combination Effect of Propofol-Ketamine and Propofol-Alfentanil on Hemodynamic Stability during Induction of General Anesthesia in the Elderly. Iran red crescent med j. 2009;11:176–80. [Google Scholar]
- 18.Singh Bajwa SJ, Bajwa SK, Kaur J. Comparison of two drug combinations in total intravenous anesthesia: Propofol–ketamine and propofol–fentanyl. Saudi J Anaesth. 2010;4:72–9. doi: 10.4103/1658-354X.65132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mi WD, Sakai T, Takahashi S, Matsuki A. Haemodynamic and electroencephalograph responses to intubation during induction with propofol or propofol/fentanyl. Can J Anaesth. 1998;45:19–22. doi: 10.1007/BF03011986. [DOI] [PubMed] [Google Scholar]
- 20.Katz RI, Levy A, Slepian B, Sobel B, Lagasse RS. Hemodynamic stability and ketamine-alfentanil anaesthetic induction. Br Janaesth. 1998;81:702–6. doi: 10.1093/bja/81.5.702. [DOI] [PubMed] [Google Scholar]
- 21.Saricaoglu F, Uzun S, Arun O, Arun F, Aypar U. A clinical comparison of etomidate-lipuro, propofol and admixture induction. Saudi j anaesth. 2012;5:62–6. doi: 10.4103/1658-354X.76509. [DOI] [PMC free article] [PubMed] [Google Scholar]