Abstract
Rationale:
Home respiratory polygraphy (HRP) may be a cost-effective alternative to polysomnography (PSG) for diagnosis and treatment election in patients with high clinical probability of obstructive sleep apnea (OSA), but there is conflicting evidence on its use for a wider spectrum of patients.
Objectives:
To determine the efficacy and cost of OSA management (diagnosis and therapeutic decision making) using (1) PSG for all patients (PSG arm); (2) HRP for all patients (HRP arm); and (3) HRP for a subsample of patients with high clinical probability of being treated with continuous positive airway pressure (CPAP) and PSG for the remainder (elective HRP arm).
Methods:
Multicentric study of 366 patients with intermediate-high clinical probability of OSA, randomly subjected to HRP and PSG. We explored the diagnostic and therapeutic decision agreements between the PSG and both HRP arms for several HRP cutoff points and calculated costs for equal diagnostic and/or therapeutic decision efficacy.
Results:
For equal diagnostic and therapeutic decision efficacy, PSG arm costs were 18% higher than HRP arm costs and 20% higher than elective HRP arm costs. HRP arm costs tended to be lower than elective HRP arm costs, and both tended to be lower than PSG arm costs if patient costs were omitted.
Conclusion:
Home respiratory polygraphy is a less costly alternative than polysomnography for the diagnosis and therapeutic decision making for patients with suspected obstructive sleep apnea. We found no advantage in cost terms, however, in using home respiratory polygraphy for all patients or home respiratory polygraphy for the most symptomatic patients and polysomnography for the rest.
Citation:
Masa JF; Corral J; Sanchez de Cos J; Duran-Cantolla J; Cabello M; Hernández-Blasco L; Monasterio C; Alonso A; Chiner E; Aizpuru F; Vázquez-Polo FJ; Zamorano J; Montserrat JM. Effectiveness of three sleep apnea management alternatives. SLEEP 2013;36(12):1799-1807.
Keywords: Cost efficacy, home respiratory polygraphy, portable monitor, sleep apnea
INTRODUCTION
Obstructive sleep apnea (OSA) is a highly prevalent disease that affects up to 25% of the adult population,1 reduces quality of life,2 and increases cardiovascular3,4 and traffic accident risks.5,6
The gold standard for OSA diagnosis is in-laboratory polysomnography (PSG), but this method is expensive and time-consuming, which may prevent adequate attention for the large number of patients who require sleep studies. Portable monitoring devices, designed for a less complex and faster home diagnosis, have been developed in the past two decades. However, the role of portable monitors in the management of OSA (diagnosis and therapeutic decision making) has not been clearly determined.
The type 3 portable monitoring device is an accepted7 and cheaper8–11 alternative for OSA diagnosis in patients with an intermediate to high clinical probability of OSA. This portable monitoring device,12 also called respiratory polygraphy, includes sensors for airflow, respiratory effort (measured with bands), and pulse oximetry readings. However, in a large study of patients with intermediate to high clinical suspicion of OSA, the therapeutic decision making performed after the diagnosis by home respiratory polygraphy (HRP) was only effective for patients with severe OSA (40% of the total sample).13 Accordingly, studies that selected patients with a high clinical suspicion of OSA (who receive continuous positive airway pressure [CPAP] therapy if OSA could be demonstrated) using HRP14,15 or other portable monitors16–18 showed a similar efficacy with CPAP treatment for patients managed with HRP or PSG.
Some cost-effectiveness studies have compared the cost of OSA management (including diagnosis and treatment) between portable monitors and PSG, using hypothetical cohorts of patients and producing conflicting results.19–22 Two studies have been conducted comparing the costs of the diagnosis and treatment between portable monitors (one with HRP)17,23 and PSG using a real cohort of patients with high clinical probability of OSA. The results favored the portable monitor approach. Therefore, HRP may be a cheaper alternative to PSG for diagnosis and treatment election in patients with high clinical probability of OSA. However, the studies' findings do not tell us whether the same results would be obtained in a wider clinical spectrum of patients. In other words, the study findings do not tell us if the suggested approach (portable monitor for high suspicion and PSG for intermediate suspicion) or the portable monitor for the entire population approach (intermediate and high suspicion) are more cost effective than PSG for the same management (diagnosis and election of treatment) and for the same patients with intermediate and high suspicion.
Therapeutic decision-making is a different process from diagnosis. It consists of recommending CPAP or other treatments. These other treatments are normally hygienic-dietetic measures and, less frequently, surgical approaches or mandibular advance devices. Most guidelines recommend CPAP, depending on the apnea-hypopnea index (AHI) level, clinical symptoms (especially sleepiness), and comorbidities (primarily hypertension and cardiovascular problems).
We ascertained the efficacy and cost of the diagnosis and therapeutic decision making using a real cohort of patients with intermediate to high clinical probability of OSA from a previous multicenter, randomized, blinded, crossover study conducted to understand the role of HRP in comparison with PSG in the management of OSA. We explored the costs of the following approaches: (1) PSG for the total sample; (2) HRP for the entire sample; and (3) HRP for a subsample of patients with a high clinical probability of being treated with CPAP and PSG for the rest of the patients.
METHODS
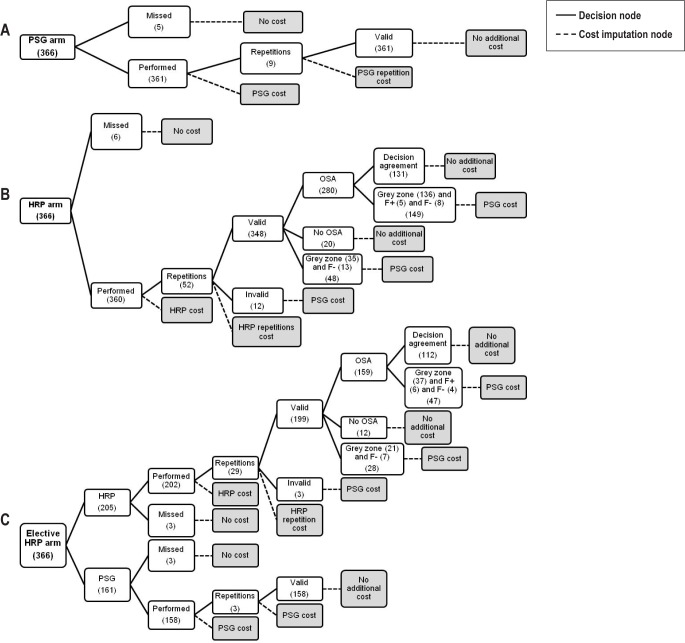
We carried out a post hoc analysis of our database to calculate the efficacy and cost of the three aforementioned approaches to OSA management: PSG, HRP, and elective HRP (Figure 1).
Figure 1.
General flow chart and cost imputation for the 366 included patients distributed into the three study arms (PSG, HRP, and elective HRP) and in the several decision nodes that incorporated cost imputations (cost imputation nodes). (A) Of the 366 included patients, five were lost without adding costs. In the subsequent 361 patients, the costs from PSG tests were included. Nine patients needed to repeat the PSG with the consequent burden. Finally, 361 cases with valid PSG had no additional costs. (B) Of the 366 included patients, six were lost without adding costs. In the subsequent 360 patients, the costs from HRP tests were included. HRP was repeated 52 times, including the correspondent expenditure from HRP repetitions. Of the 360 patients, 12 with invalid HRP underwent PSG with the subsequent additional costs. Patients with valid HRP (348) presented the following three decision situations: (1) OSA diagnosis agreement was reached in 280 patients; of these, 131 reached therapeutic decision agreement (CPAP or no CPAP) ending the branch without adding costs, and there were 149 patients in the group that had no therapeutic decision agreement (136), false- positive (5) and false-negative results (8) in which the PSG cost was added; (2) no OSA diagnosis agreement was reached for 20 patients who ended the branch without additional cost; and (3) patients with no diagnosis agreement (35) or false-negative results (13) who reached the end of the branch with the included costs of PSG. (C) Of the 366 included patients, 205 were selected to undergo HRP and the subsequent 161 were selected to undergo PSG. With the 205 patients, three were lost without adding costs and HRP was repeated 29 times, with the corresponding expenditure for the HRP repetitions. Of the 205 patients, three with invalid HRP underwent PSG, with the consequent additional cost. Patients with valid HRP (199) presented three decision situations: (1) OSA diagnosis agreement was achieved for 159 patients; of these, therapeutic decision agreement (CPAP or no CPAP) was achieved for 112, ending the branch without additional costs. There were 47 patients in the group who had no therapeutic decision agreement (37), false-positive (6), or false-negative results (4) and had added PSG costs. (2) No OSA diagnosis agreement was reached in 12 patients who ended the branch with no additional costs. (3) Patients with no diagnosis agreement (21) or false-negative results (7) reached the end of the branch, with added costs for PSG. Of the 161 patients referred to PSG, three patients were lost with no additional cost. In the subsequent 158 patients, the costs for the PSG test were included. PSG had to be repeated in three patients, with the consequent burden. Finally, 158 cases with valid PSG reached the end of the branch without additional cost. F+ = false positive; F- = false negative; HRP, home respiratory polygraphy; OSA, obstructive sleep apnea; PSG, polysomnography.
We included patients with suspected OSA presenting with (1) snoring or observed apneas; and (2) sleepiness (Epworth sleepiness scale score > 10) or morning fatigue. For the elective HRP arm we selected patients as having high clinical probability of OSA by selecting patients with a high clinical probability of being treated with CPAP (if OSA was demonstrated) based on the Spanish Sleep Network Guidelines24: an Epworth sleepiness scale score ≥ 12, or previous cardiovascular diseases.
The method for our original study was described in previous reports.8,13,23,25 A brief summary of the original methodology and the methodology of the current study are discussed in the following paragraphs.
Original Methodology
Patients
We included patients between 18 and 70 y of age drawn from patients referred to eight sleep centers in Spain for suspected OSA due to the aforementioned criteria (snoring or observed apneas, Epworth Sleepiness Scale score > 10, or morning fatigue) and no other sleep disorders present. We excluded patients with severe and unstable heart disease, those who were unable to set up the HRP device in a trial, and those who refused to participate in the study. The inclusion was sequential and, before starting the procedure, each center selected specific days or weeks per month during the inclusion period to enroll all potential patients.
The ethics committees of the eight centers approved the study. Informed consent was obtained in writing from all patients.
Protocol
All patients underwent PSG and HRP, in random order. PSG and HRP readings were recorded separately, and the technicians were blinded to any identifying information about the patients as well as to any results of the previous method (PSG or HRP).
Home Respiratory Polygraphy
Our HRP (BreastSC20; Breast Medical AB; Mölnlycke, Sweden) measurements included oxygen saturation (model 8000 J; Nonin Medical; Plymouth, MN), airflow through a nasal cannula, and thoracic and abdominal movements measured by piezoelectric bands (Pro-Tech reference 1295; Respironics; Pittsburgh, PA).
All patients were instructed in home use of the HRP device by a technician in the hospital setting before randomization. HRP equipment was moved from home to home by trained personnel from CPAP service companies in each hospital area who were acting as transport companies. No additional support was provided by the transport services to the patients in terms of setting up the HRP devices. The raw data files were electronically transmitted from home to hospital.8 The hospital technicians scored the data files manually.
PSG in Hospital
The PSG recordings were analyzed manually at each participating center, based on standard criteria.7,26–28 The neurological variables were the electroencephalogram (C3-A2; C4-A1; O1-A2; O2-A1; F4-A1; F3-A2), electrooculogram (right and left), and electromyogram (on the chin and both legs). Airflow was measured using a nasal cannula, and thoracoabdominal movement was measured with thoracic and abdominal bands. Oxygen saturation was assessed with a pulse oximeter. Electrocardiogram and body position were also measured.
Definitions
A valid PSG or HRP recording had at least 3 h of recording. An invalid recording could be repeated up to two times.
For PSG, apnea was defined as the absence of airflow (≥ 90% reduction) for ≥ 10 sec, and hypopnea was defined as a discernible airflow or band reduction (≥ 30% and < 90%) lasting at least 10 sec with a ≥ 3% decrease in oxygen saturation or final arousal.27 For HRP, the same definition applied for apnea and hypopnea but without the final arousal criteria for hypopnea. The number of apneas and hypopneas was divided by the valid recording time for HRP and the sleep time for PSG to determine the AHI.
Therapeutic Decision
Therapeutic decisions (CPAP or no CPAP) for HRP and PSG were made by a researcher in each center based on the same set of variables collected from each patient at baseline: age, sex, body mass index, neck circumference, systolic and diastolic blood pressure, comorbidities, occupation, alcohol intake, and tobacco consumption. Subjective nocturnal sleep time and napping time on working days and holidays were determined based on the previous 4 w. Episodes of subjective asphyxia, nocturia, morning headache, morning fatigue, and sleepiness while driving6 were collected for four degrees of intensity (never, occasionally, frequently, and always) based on the previous 4 w. Epworth and American Sleep Disorders Association (ASDA)29 sleepiness scale scores were measured based on the previous 4 w; PSG (recording time, sleep time, sleep periods, AHI [total sleep time and sleep time in the supine position], arousal, and desaturation indexes and time with oxygen saturation < 90%) and HRP (recording and valid recording time, AHI [total valid recording time and valid time in supine position], desaturation index and time with oxygen saturation < 90%). Patients and diagnostic methods (HRP and PSG) were assessed in random order using an electronic database. Each patient was presented twice (with PSG or HRP information), at random and nonconsecutively. Participant identification numbers for patients and other data were hidden. After 1 mo, the same therapeutic decision procedure was repeated.
The criteria for recommending CPAP, according to the Spanish Sleep Network guidelines,24 are (1) an AHI ≥ 5 with significant sleepiness (Epworth Sleepiness Scale score ≥ 12) or previous cardiovascular diseases and (2) an AHI ≥ 30, with clinical symptoms taking on less importance.
Current Methodology
Cost Analysis
We performed a cost minimization analysis for equally effective alternatives.30 This involves calculating the cost when the efficacy is assumed to be equal in all the alternatives. To achieve the same efficacy for the testing protocols (both HRP arms) as the standard protocol (PSG), we added the cost of the necessary tests (i.e. PSG) to the correct diagnosis and therapeutic decision obtained (in accordance with PSG). Figure 1 shows the procedure for the imputation costs of the three alternative approaches for achieving the same efficacy. We analyzed the following cost groups:
Test costs (PSG and HRP): The test costs included the following expenses: personnel (technicians, physicians, and secretaries), a linear 5-y depreciation of equipment (taking into account the number of recordings conducted in this period in each hospital), consumables, and the proportional burden of the sleep laboratory on the general budget of the hospital.
Patients' costs for PSG and HRP: Although the HRP device was moved by the transport company with telematic transmission of raw data in all patients, we also estimated the cost per kilometer resulting from patients transporting the device from home to hospital and vice versa. The cost per kilometer was calculated for each hospital.
Total test cost: The sum of the test (PSG and HRP) and patient costs.
Costs of HRP and PSG for equal diagnostic efficacy: For HRP, the cost was the sum of the following expenditures: (1) the cost of PSG in patients with invalid HRP recordings, after repetitions; (2) the cost of repeated HRPs due to invalid recordings, in patients with a valid final recording; (3) the cost of PSG in patients with unclassified HRP diagnosis (“gray zone”); and (4) the cost of PSG in patients with false-negative results. For PSG, we included the cost of repeated PSGs due to invalid recordings.
Costs of HRP for equal therapeutic decision efficacy: The costs affected only patients diagnosed with OSA. The cost was the sum of the following expenditures: (1) the cost of PSG in patients when a CPAP recommendation by HRP in agreement with the PSG (“gray zone”) was impossible to obtain and (2) the cost of PSG in patients with false negative and false positive results. Given that PSG is the gold standard, no cost imputation was added to the PSG arm in this cost group.
Patients' costs for equal diagnostic and therapeutic decision efficacy: The burden due to transportation caused by repetitions (HRP and PSG) and the PSG transportation cost were included in (1) invalid HRPs; (2) patients with unclassified diagnosis results and with any CPAP recommendations (“gray zone”); and (3) false- negative and false-positive results.
Total cost for equal diagnostic and therapeutic decision efficacy: The sum of equal diagnostic and therapeutic decision costs (PSG and HRP) and patient costs for equal diagnostic and therapeutic decision efficacy.
Total costs: The sum of the total test costs and the total costs for equal diagnostic and therapeutic decision efficacy.
Statistical Analysis
We considered OSA diagnosis for a PSG AHI ≥ 5. To determine the ruling out and the ruling in of HRP cutoff points for OSA diagnosis, we used (1) sensitivity and specificity; (2) negative ([1-sensitivity/specificity] and positive [sensitivity/1-specificity]) likelihood ratios (LR); and (3) the posttest probability of obtaining a true positive diagnosis when the test was positive or negative, which we calculated based on the pretest probability (prevalence) and positive and negative LRs.31 To find the optimal ruling out and ruling in HRP cutoff points, we tested the previous parameters in five-point increments of AHI (i.e., ≥ 5, ≥ 10, ≥ 15, etc.), starting with the value of five, in the HRP and elective HRP arms.
Given that we had a high prevalence (pretest probability) of OSA in our study population (90%), it is probable that we can identify a ruling in HRP cutoff point for OSA. We defined this cutoff point as follows: a positive LR > 5 and a posttest probability close to 100%, which represents a large change in the probability from pre-test to posttest. Given the lower probability of identifying a ruling out HRP cutoff point for OSA in our patients, we defined the cutoff point as a negative LR < 0.1, which represents a very large change in the probability from pretest to posttest.
To evaluate the agreement in the therapeutic decision between HRP and PSG, we used the agreement level (100 – the sum of the percentages of true positives and negatives) in the population in whom OSA was diagnosed. We used the same analysis for the two therapeutic decisions (the two analyses were performed 1 mo apart) based on the PSG results. These PSG results were considered the reference values because they state the variability of the gold standard (PSG) and the ideal outcome for HRP scores. To find the optimal agreement level, we tested these parameters in five-point increments of AHI (starting with the ruling in HRP cutoff point of OSA) in the HRP and elective HRP arms. We considered the HRP cutoff point to be adequate when the agreement level was greater than 90% (which means that the sum of the false-positive and false-negative results was lower than 10%) and close to the reference value.
RESULTS
Initially, 377 patients were selected. Eleven were excluded (seven due to failure in the HRP trial, two due to severe heart disease, and two due to lack of informed consent), and 366 were included to assess costs. Figure 1 contains the flow of patients in each cost imputation arm (PSG, HRP, and elective HRP) in several sequential decision nodes: (1) the number of patients who performed the diagnostic test (HRP or PSG) and the number of missed cases; (2) the number of test repetitions; (3) the number of valid and invalid tests; (4) the diagnostic agreement between HRP and PSG (cases with and without OSA, gray zone and false-negative results–see the following paragraphs); and (5) agreement in the therapeutic decision between HRP and PSG (the number of cases in agreement with PSG, gray zone, false-positive and false-negative results–see the following paragraphs).
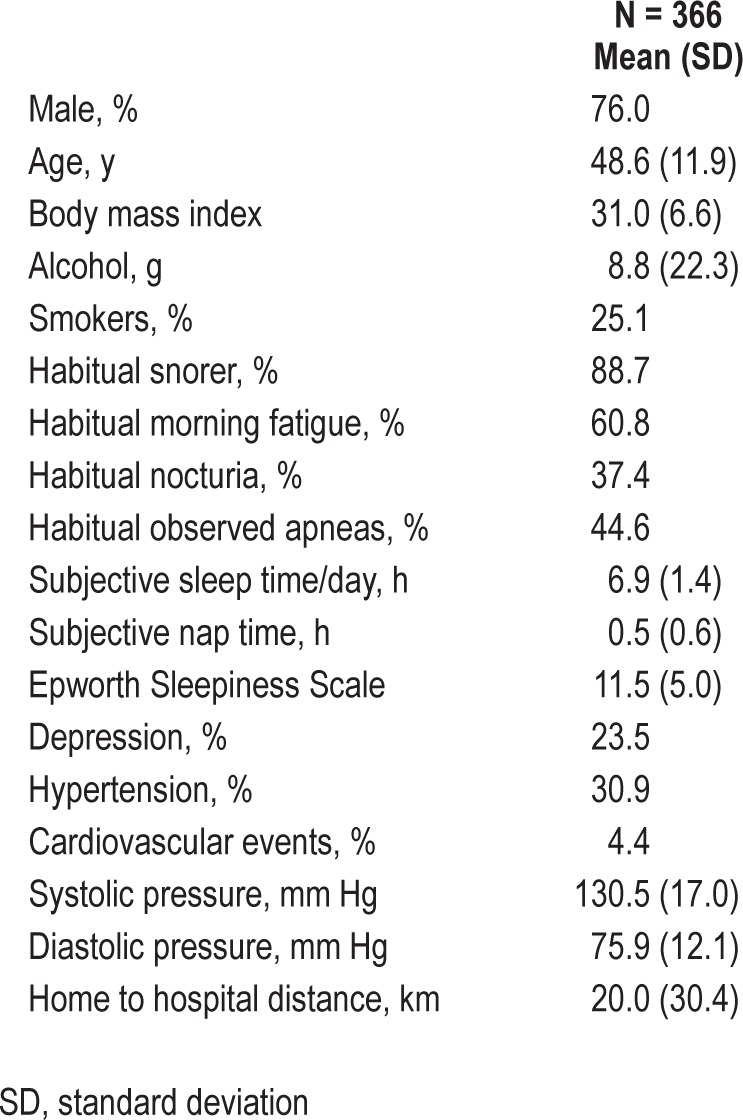
The clinical and anthropometric characteristics of the 366 included patients are shown in Table 1.
Table 1.
Characteristics of the study population
In the PSG arm of 366 included patients (Figure 1A), five were lost without adding costs. In the rest of 361 patients, the costs from PSG tests were incorporated. Nine patients required to repeat the PSG with the resulting load. Finally, 361 cases with valid PSG had no extra costs.
Diagnostic Agreement between HRP and PSG
HRP Arm
Of the 366 enrolled patients, six were lost without adding costs (Figure 1B). In the rest of the 360 patients, the costs from HRP tests were added. HRP was repeated 52 times, including the correspondent costs from HRP repetitions. Of the 360 patients, 12 with invalid HRP underwent PSG with the subsequent supplementary costs and 348 had valid HRP tests being available to explore the diagnostic agreement with PSG. For a PSG AHI cutoff point ≥ 5, the pretest probability (prevalence) was 90% (Table 2). According to our previous definition (see statistical analysis), an AHI < 5 from HRP effectively ruled out OSA. According to our previous definition (see statistical analysis), an acceptable HRP AHI cutoff point for ruling in OSA would be 10. Consequently, there were 20 patients (Figure 1B) with a true negative result (no OSA) and 280 with a true positive result (OSA). There were 48 patients with no positive or negative diagnosis of OSA (gray zone) or false-negative results where PSG costs were included.
Table 2.
Ruling out and ruling in home respiratory polygraphy cutoff points for home respiratory polygraphy and elective home respiratory polygraphy arms with a polysomnography apnea-hypopnea index cutoff point of ≥ 5
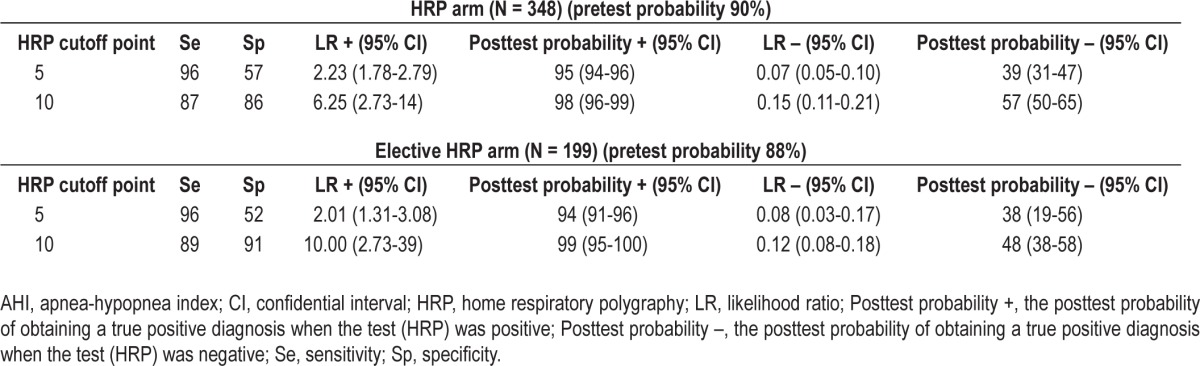
Elective HRP Arm
Of the 366 included patients, 205 met the clinical criteria for a high clinical probability of being treated with CPAP (Figure 1C). These patients were managed with HRP. The rest of the patients (161) were managed with PSG. Of the 205 patients, three were lost without extra costs, HRP was repeated 29 times, with the consequent costs for the HRP repetitions, and 199 had a valid HRP (three invalid HRP) available to explore the diagnostic agreement with PSG. For these 199 patients, the pretest probability of OSA was 88% for a PSG AHI cutoff point ≥ 5 (Table 2). According to our previous definitions, an AHI < 5 from HRP effectively ruled out OSA, and the HRP ruling in cut-off point should be ≥ 10. Twelve patients (Figure 1C) had a true negative result (no OSA) and 159 had a true positive result (OSA). Twenty-eight patients had no positive or negative diagnosis of OSA (gray zone) or had false-negative results where PSG costs were included.
Therapeutic Decision Making
HRP Arm
Figure 2A shows the agreement levels between HRP and PSG (and also for the reference) for the HRP arm for each of the five HRP AHI points, starting with the ruling in HRP cutoff point (≥ 10). The agreement level between HRP and PSG increases according to the AHI level. A value greater than 90% and close to the reference was achieved with an HRP AHI cutoff point ≥ 30. By considering this cutoff point acceptable, 131 of the 280 patients in whom OSA was diagnosed (Figure 1B) received the correct therapy (in agreement with PSG) without supplementary costs. The remaining 149 patients did not have a correct therapeutic decision (including false- positive and false-negative results) and the PSG costs were added.
Figure 2.
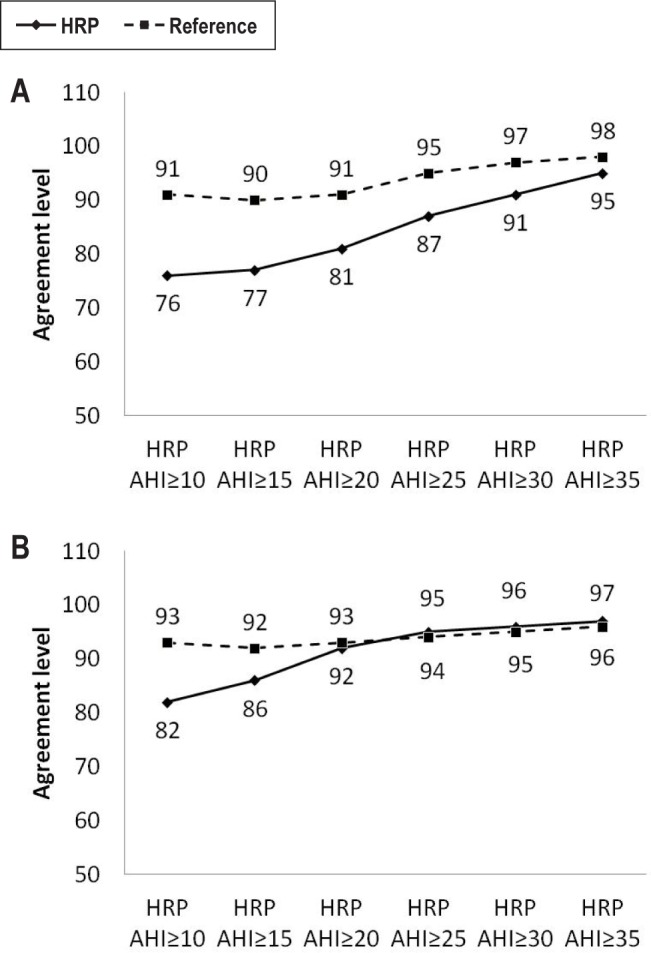
Evolution of the agreement level (100 − sum of the percentages of the true positive and negative results) in the therapeutic decisions between HRP and PSG and the Reference, according to incremental levels of HRP AHI. (A) Home respiratory polygraphy arm. (B) Elective home respiratory polygraphy arm. AHI, apnea-hypopnea index; HRP, home respiratory polygraphy; Reference, agreement between before and after 1 mo by polysomnography.
Elective HRP Arm
Figure 2B shows the agreement levels between HRP and PSG (and also for the reference) for the elective HRP arm for each of the five HRP AHI points, starting with the ruling in HRP cutoff point (≥ 10). An acceptable HRP AHI cutoff point was ≥ 20. Accordingly, 112 of the 159 patients in whom OSA was diagnosed had the correct therapeutic decision (Figure 1C) without supplementary costs. The remaining 47 patients did not have a correct therapeutic decision (including false-positive and false-negative results) and the PSG costs were added.
Cost Analysis
Figure 1 contains the cost imputations in each arm of the study (PSG, HRP, and elective HRP) in the aforementioned sequential nodes. Table 3 shows the costs for the PSG, HRP, and elective HRP arms of the calculated cost groups for the 366 included patients. Figure 3 shows the percentages of the total costs for the HRP and elective HRP arms and their distribution into cost groups compared with the PSG costs. The costs for the PSG arm were 18% higher than for the HRP arm and 20% higher than for the elective HRP arm. The costs for equal diagnostic and therapeutic decision efficacy were significantly higher for the HRP arm than for the elective HRP arm, but the test costs were much lower for the HRP arm than for the elective HRP arm. The HRP arm was 3% more expensive than the elective HRP arm but vice versa if patient costs were not taken into account.
Table 3.
Costs for the 366 randomized patients and for patients in the polysomnography,, home respiratory polygraphy, and elective home respiratory polygraphy arms distributed into various cost imputation groupsa
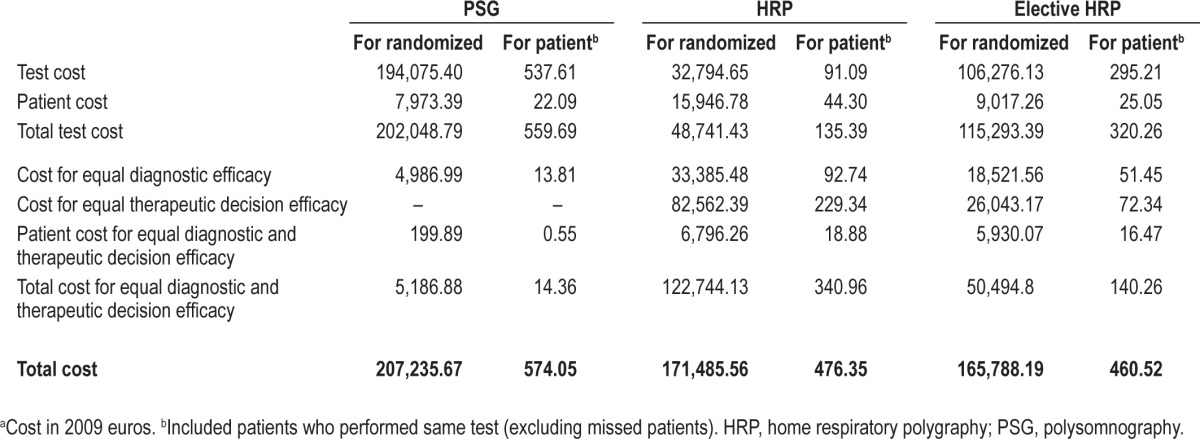
Figure 3.
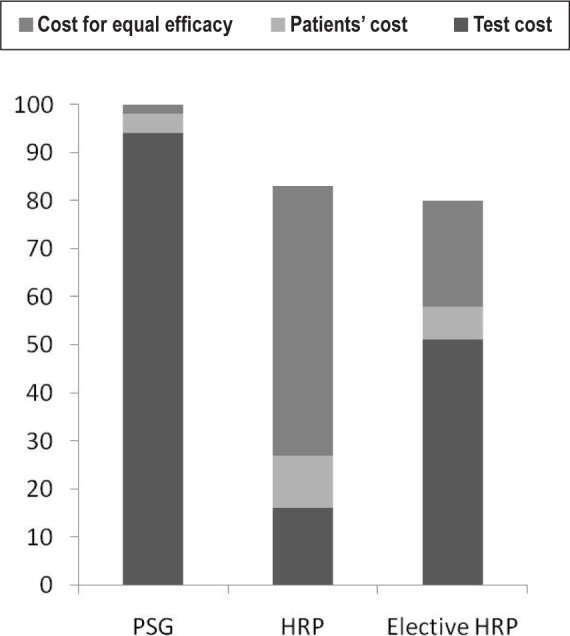
Percentages of the total costs from the HRP and elective HRP arms and their distribution in three groups (test costs, patients' costs, and costs for equal diagnosis and therapeutic decision efficacy) compared with polysomnography costs, which is considered to be 100%. HRP, home respiratory polygraphy; PSG, polysomnography.
DISCUSSION
To our knowledge, this is the first study assessing the efficacy and costs of three OSA management protocols (diagnosis and therapeutic decision) in a real and large population with intermediate to high clinical suspicion of OSA. The principal findings are: (1) HRP performed for all patients with suspected OSA or for a more symptomatic subsample have lower costs than PSG and (2) HRP and elective HRP protocols have similar costs.
We have recently published a study using the same group of patients showing that HRP had lower costs than PSG for OSA diagnosis8 but, however, there was poor agreement with PSG for therapeutic decisions-making, except for patients with severe OSA.13 The results of the current study complete the investigation, extending the cost analysis for the global process of diagnosis and therapeutic decision-making (not only for diagnosis). Despite the commented modest agreement between HRP and PSG in the therapeutic decision making for patients with no severe OSA (AHI ≤ 30)13, if we calculate the costs for the same level of diagnosis and therapeutic diagnosis efficacy, these were lower for the two HRP approaches than for the PSG protocol.
We included the cost derived from patients because this is an actual direct cost. However, the expenses incurred in moving the patients' equipment are generally covered by the patients themselves and not by the hospital. If we exclude the patient costs, the costs of the two HRP approaches tended to be lower in comparison with PSG and similar between the two HRP arms (HRP and elective HRP).
The clinical criteria for selecting patients with a high clinical probability of OSA could include other variables that are used in the current study such as BMI (higher than 30) and age (older than 55 y).13 However, we preferred to use the clinical criteria of being treated with CPAP (if OSA is demonstrated) because these criteria can produce better agreement with PSG in the therapeutic decision and, consequently, higher savings. Thus, although the diagnostic agreement with PSG was similar between both HRP arms, the therapeutic decision agreement was better for the elective HRP arm than for the HRP arm, contributing to decreased costs for equal therapeutic decision efficacy. In addition, to make our protocol more applicable to clinical practice in Spain, we used the standardized criteria for CPAP treatment from the Spanish Sleep Network.24 Moreover, we believe that if we had selected other clinical criteria for high probability of OSA, the cost of the elective HRP arm would not have been significantly different. With more demanding criteria, we would achieve better diagnostic and therapeutic decision agreement with PSG (lower costs) for fewer patients but with more PSGs for the rest of the patients (greater costs) and vice versa for less demanding criteria.
PSG is considered the gold standard for OSA management. The current paper is based on achieving agreement with PSG for diagnosis and therapeutic decision and then imputing the costs accordingly. The fact that PSG is performed in “unnatural environments” has led us to doubt that PSG is really the gold standard. Five randomized control studies have assessed the efficacy of CPAP treatment (over several w) after OSA diagnosis using PSG or HRP14,15 or another type of portable home monitoring device.16–18 Patients were selected to receive CPAP treatment if OSA was confirmed (high clinical probability of OSA). Both protocols (outpatient and in-hospital) showed similar improvements in AHI,16 quality of life, clinical symptoms, and adherence to CPAP treatment.14,15,17,18 Two of these studies carried out cost analysis15,17 with favorable results for portable monitoring. Because these studies included a population with only a high clinical probability of OSA (approximately 40% of patients needing sleep studies), the results do not provide information on what would happen in a population with a wider clinical spectrum. Our results provide conclusive information on this question while considering the PSG as the gold standard; however, the above-mentioned studies regard HRP (or other portable monitoring devices) as an equivalent alternative to PSG. Therefore, to determine whether HRP is an equivalent alternative to PSG, randomized controlled trials with cost analyses are needed to assess the follow-up of patients with intermediate to high OSA suspicion who are treated or untreated with CPAP according to HRP or PSG. If these types of studies have favorable results for HRP, the cost savings could be much higher than in our study.
A number of studies have estimated the costs of HRP as compared with PSG based on simulated models of hypothetical cohorts of patients including diagnosis, CPAP titration, and CPAP adherence, with conflicting results.19–22 Our study had a more solid methodological approach for the cost calculation for the following reasons: (1) the study was carried out on a real and large cohort of patients; (2) only direct costs were included; and (3) no assumptions of cost calculations were incorporated. We preferred not to include the costs for CPAP titration and CPAP treatment because the cost imputation in our study was based on the diagnosis and therapeutic decision agreements with PSG. Therefore, if we include the costs from CPAP titration and treatment, these should necessarily be the costs from the polysomnographic therapeutic decision, no really those originated from both HRP and elective HRP arms. Thus, this cost should increase the total cost in the three arms but in a similar proportion without adding differences among the arms.
One interesting question is whether split-night (diagnosis and CPAP titration in the same night) plus autotitration for the rest of the cases could be cheaper than HRP plus autotitration protocol. Although we did not include split-night in our protocol, if we consider those patients with an AHI ≥ 15 (less demanding criterion) or an AHI ≥ 30 (more demanding criterion) as candidates, the saving for the PSG arm in comparison with the HRP arm would be 8,070 € and 5,730 €, respectively (the cost of autotitration in our consortium is 30 €). Thus, the lower cost of the PSG arm would be 199,165.67 € and that of the HRP arm 171,485.56 €. The savings for the PSG arm in comparison with the elective HRP arm may be even lower because the same patients referred to PSG for lower clinical probability of being treated with CPAP could also be candidates for a split-night protocol, saving the autotitration cost for the elective HRP arm. A similar savings could occur for patients referred for PSG after HRP management failure. Apparently, therefore, HRP plus autotitration may be a better cost alternative than PSG, even with a split-night protocol (whenever possible).
A practical application of our results can be shown as follows: (1) For the HRP approach, all patients should undergo HRP. In patients with an HRP AHI ≤ 5, OSA is considered ruled out, and CPAP treatment should be recommended for patients with an AHI ≥ 30. For the rest of the patients, PSG should be performed. (2) For the elective HRP approach, patients with a high clinical probability of being treated with CPAP should undergo HRP. Patients with an HRP AHI ≤ 5 OSA should be ruled out, and CPAP treatment should be recommended for patients with an AHI ≥ 20. For the rest of the patients, PSG should be performed. A small proportion of false-positive results in the two approaches will be directed to CPAP treatment, although most of them will be borderline cases in the CPAP decision. There are no cost advantages in choosing one or the other approach but the elective HRP protocol seems simpler to complete.
In conclusion, HRP is a less costly alternative than PSG for the diagnosis and therapeutic decision making for patients with suspected OSA. We found no advantage in cost terms, however, in using HRP for all patients or HRP for the most symptomatic patients and PSG for the rest.
DISCLOSURE STATEMENT
This was not an industry supported study. Sources of Funding: Instituto de Salud Carlos III (Healthcare Research Fund, Ministry of Health and Consumption), Spanish Respiratory Society (SEPAR), Telefonica SA (Spain), Air Liquide (Spain) and Breas Medical (Spain). We are grateful for the support of project ECO2009-14152 (Ministerio de Ciencia e Innovación), The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors are indebted to Verónica Rodríguez and Vanessa Iglesias for their assistance in the translation of the manuscript and to Asunción Martín, Elena Sandoval, Soledad Guillen, Trinidad Amigo, Pablo Mejias, and Carmen Lorenzana for technical assistance in the sleep laboratory.
REFERENCES
- 1.Durán J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163:685–9. doi: 10.1164/ajrccm.163.3.2005065. [DOI] [PubMed] [Google Scholar]
- 2.Ballester E, Badia JR, Hernández L, et al. Evidence of the effectiveness of continuous positive airway pressure in the treatment of sleep apnea/ hypopnea syndrome. Am J Respir Crit Care Med. 1999;159:495–501. doi: 10.1164/ajrccm.159.2.9804061. [DOI] [PubMed] [Google Scholar]
- 3.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 4.Barbé F, Durán-Cantolla J, Sánchez-de-la-Torre M, et al. Spanish Sleep And Breathing Network. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307:2161–8. doi: 10.1001/jama.2012.4366. [DOI] [PubMed] [Google Scholar]
- 5.Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 6.Masa JF, Rubio M, Findley LJ. Habitually sleepy drivers have a high frequency of automobile crashes associated with respiratory disorders during sleep. Am J Respir Crit Care Med. 2000;162:1407–12. doi: 10.1164/ajrccm.162.4.9907019. [DOI] [PubMed] [Google Scholar]
- 7.Iber C, Ancoli-Israel S, Chesson A, Quan S. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 8.Masa JF, Corral J, Pereira R, et al. Effectiveness of home respiratory polygraphy for the diagnosis of sleep apnea and hypopnea syndrome. Thorax. 2011;66:567–73. doi: 10.1136/thx.2010.152272. [DOI] [PubMed] [Google Scholar]
- 9.Whittle AT, Finch SP, Mortimore IL, MacKay TW, Douglas NJ. Use of home sleep studies for diagnosis of the sleep apnoea/hypopnoea syndrome. Thorax. 1997;52:1068–73. doi: 10.1136/thx.52.12.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parra O, García-Esclasans N, Montserrat JM, et al. Should patients with sleep apnoea/hypopnoea syndrome be diagnosed and managed on the basis of home sleep studies? Eur Respir J. 1997;10:1720–4. doi: 10.1183/09031936.97.10081720. [DOI] [PubMed] [Google Scholar]
- 11.Alonso Alvarez ML, Terán Santos J, Cordero Guevara J, et al. Reliability of home respiratory polygraphy for the diagnosis of sleep apnea-hypopnea syndrome: analysis of costs. Arch Bronconeumol. 2008;44:22–8. [PubMed] [Google Scholar]
- 12.Ferber R, Millman R, Coppola M, et al. Portable recording in the assessment of obstructive sleep apnea. ASDA standards of practice. Sleep. 1994;17:378–92. doi: 10.1093/sleep/17.4.378. [DOI] [PubMed] [Google Scholar]
- 13.Masa JF, Corral J, Pereira R, et al. Spanish Sleep Network. Therapeutic decision-making for sleep apnea and hypopnea syndrome using home respiratory polygraphy: a large multicentric study. Am J Respir Crit Care Med. 2011;184:964–71. doi: 10.1164/rccm.201103-0428OC. [DOI] [PubMed] [Google Scholar]
- 14.Kuna ST, Gurubhagavatula I, Maislin G, et al. Non-inferiority of Functional Outcome in Ambulatory Management of Obstructive Sleep Apnea. Am J Respir Crit Care Med. 2011;183:1238–44. doi: 10.1164/rccm.201011-1770OC. [DOI] [PubMed] [Google Scholar]
- 15.Rosen CL, Auckley D, Benca R, et al. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep. 2012;35:757–67. doi: 10.5665/sleep.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mulgrew AT, Fox N, Ayas NT, Ryan CF. Diagnosis and initial management of obstructive sleep apnea without polysomnography: a randomized validation study. Ann Intern Med. 2007;146:157–66. doi: 10.7326/0003-4819-146-3-200702060-00004. [DOI] [PubMed] [Google Scholar]
- 17.Antic NA, Buchan C, Esterman A, et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179:501–8. doi: 10.1164/rccm.200810-1558OC. [DOI] [PubMed] [Google Scholar]
- 18.Berry RB, Hill G, Thompson L, McLaurin V. Portable monitoring and autotitration versus polysomnography for the diagnosis and treatment of sleep apnea. Sleep. 2008;31:1423–31. [PMC free article] [PubMed] [Google Scholar]
- 19.Chervin RD, Murman DL, Malow BA, Totten V. Cost-utility of three approaches to the diagnosis of sleep apnea: polysomnography, home testing, and empirical therapy. Ann Intern Med. 1999;130:496–505. doi: 10.7326/0003-4819-130-6-199903160-00006. [DOI] [PubMed] [Google Scholar]
- 20.Reuveni H, Schweitzer E, Tarasiuk A. A Cost-effectiveness analysis of alternative at home or in laboratory technologies for the diagnosis of obstructive sleep apnea síndrome. Med Decis Making. 2001;21:451–8. doi: 10.1177/0272989X0102100603. [DOI] [PubMed] [Google Scholar]
- 21.Deutsch PA, Simmons MS, Wallace JM. Cost-effectiveness of split-night polysomnography and home studies in the evaluation of obstructive sleep apnea syndrome. J Clin Sleep Med. 2006;2:145–53. [PubMed] [Google Scholar]
- 22.Pietzsch JB, Garner A, Cipriano LE, Linehan JH. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep. 2011;34:695–709. doi: 10.5665/SLEEP.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masa JF, Corral J, Gómez de Terreros J, et al. Significance of including a surrogate arousal for sleep apnea-hypopnea syndrome diagnosis by respiratory polygraphy. A large multicenter study. Sleep. 2013;36:249–57. doi: 10.5665/sleep.2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lloberes P, Durán-Cantolla J, Martínez-García MÁ, et al. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Spanish Society of Pulmonology and Thoracic Surgery. Arch Bronconeumol. 2011;47:143–56. doi: 10.1016/j.arbres.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 25.Masa JF, Corral J, Pereira R, et al. Spanish Sleep Group. Effectiveness of sequential automatic-manual home respiratory polygraphy scoring. Eur Respir J. 2013;41:879–87. doi: 10.1183/09031936.00186811. [DOI] [PubMed] [Google Scholar]
- 26.Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. EEG arousals: scoring rules and examples. Sleep. 1992;15:174–84. [PubMed] [Google Scholar]
- 27.Grupo Español de Sueño (GES) Consenso Nacional sobre el síndrome de apneas-hipopneas del sueño. Arch Bronconeumol. 2005;41:3–110. [Google Scholar]
- 28.Rechtschaffen A, Kales A. Los Angeles: Brain information service/Brain research institute, University of California at Los Angeles; 1968. A manual of standardized terminology and scoring system for sleep stages of human subjects. [Google Scholar]
- 29.Diagnostic Classification Steering Committee, American Sleep Disorders Association. Rochester, Minnesota: 1990. The International Classification of Sleep Disorders: Diagnostic and Coding Manual. [Google Scholar]
- 30.Drummond M, O'Brien B, Stoddart GL, Torrance GW. Oxford: Oxford University Press; 1997. Methods for the economic evaluation of health care Programmes. [Google Scholar]
- 31.Flemons WW, Littner MR, Rowley JA, et al. Home diagnosis of sleep apnea: a systematic review of the literature. An evidence review cosponsored by the American Academy of Sleep Medicine, the American College of Chest Physicians, and the American Thoracic Society. Chest. 2003;124:1543–79. doi: 10.1378/chest.124.4.1543. [DOI] [PubMed] [Google Scholar]