Abstract
Introduction:
Sleep duration and quality have been associated with obesity. Sleep disturbance has been reported to be associated with stress and depression among non-obese populations, but these relationships have not been previously examined in the obese population. The objective of the current study was to examine the complex associations among sleep disturbance, quality of life, anxiety, and depression in a patient sample with severe obesity.
Methods:
Two hundred seventy consecutively recruited patients with a mean body mass index (BMI) of 47.0 kg/m2 were studied. The correlation coefficient, multiple linear regressions, and structural equation modeling (SEM) analysis were used to evaluate the association between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), Impact of Weight on Quality of Life-Lite (IWQOL-Lite) and Hospital Anxiety and Depression Scale (HADS).
Results:
The mean (standard deviation; SD) PSQI score was 8.59 (5.11), and mean ESS score was 8.84 (5.79). After controlling for potential confounders, poor sleep quality and excessive daytime sleepiness were found to be significantly associated of all the components of IWQOL-Lite; physical function (β = -0.32, β = -0.27; P < 0.01), self-esteem (β = -0.23, β = -0.30; P < 0.05), sexual-life (β = -0.30, β = -0.35; P < 0.05), public distress (β = -0.39, β = -0.39; P < 0.01), and work (β = -0.26, β = -0.48; P < 0.01). We also found that the PSQI global score had a positive significant association with anxiety (β = 0.29; P = 0.01) and depression (β = 0.31; P = 0.01) components of HADS.
Conclusion:
Poor sleep quality was strongly associated with mood disturbance and poor quality of life among extremely obese patients. Future interventions are needed to address sleep disturbance to prevent further development of psychological co-morbidity and potentially worsening of obesity among these individuals.
Citation:
Araghi MH; Jagielski A; Neira I; Brown A; Higgs S; Thomas GN; Taheri S. The complex associations among sleep quality, anxiety-depression, and quality of life in patients with extreme obesity. SLEEP 2013;36(12):1859-1865.
Keywords: Extreme obesity, sleep duration, sleep quality, mental health, quality of life
INTRODUCTION
The number of people with obesity is increasing at an alarming rate worldwide. The prevalence of more severe obesity (body mass index [BMI] ≥ 35.0 kg/m2) is increasing most rapidly.1 Severe obesity is associated with increased risk of co-morbidities including diabetes, cardiovascular disease, and cancer, which ultimately result in reduced life expectancy. Additionally, individuals with severe obesity are more likely to experience psychological morbidity,2 self-reported disability, and reduced quality of life.3 To prevent and manage severe obesity, there is a need for greater understanding of factors that could contribute to the development and perpetuation of obesity in this clinically challenging population.
Recently, there has been great interest in the role of both sleep duration4–7 and quality8 in the onset and progression of obesity. In the Wisconsin Sleep Cohort Study (WSCS), a U-shaped association between sleep duration and BMI was observed.9 It was also reported that short sleep duration was associated with higher ghrelin and lower leptin levels, which could potentially promote excessive food intake, unhealthy food selection, and subsequent obesity.9 Several other mechanisms for the association between sleep and obesity have been proposed, including increased opportunity to eat, increased fatigue and reduced physical activity, and psychological distress, but these remain to be confirmed.10
There are a few studies of the association of sleep quality and obesity.8,11,12 In the WSCS, polysomnographic measures of sleep quality were associated with ghrelin levels.9 Jennings and colleagues8 reported an association between poor global sleep quality, measured through the Pittsburgh Sleep Quality Index (PSQI) and increased BMI and the metabolic syndrome. The associations among sleep duration, sleep quality, and obesity are bidirectional. Once obesity occurs, sleep is likely to be disturbed and weight loss has been observed to reduce sleep disturbance and obesity associated sleep disordered breathing.13
Apart from the relationship with obesity, sleep duration and quality are related to other health outcomes including psychological problems.14 A number of studies have reported bidirectional relationships between sleep and depression, with some suggesting that that sleep quality may initiate and/or exacerbate mood disturbance, and that by improving sleep, it may be possible to improve mood.15,16 The link between sleep and depression has been previously examined in non-obese populations by a number of studies.17–20 In obese individuals, depression could hinder weight loss and its maintenance. Price and colleagues21 have reported that depressive symptoms could potentially predict weight regain among overweight individuals who are successful with initial weight loss.
Although sleep quality may impinge on body weight regulation, little is known about its role in the context of severe obesity, which is complicated by several comorbidities. To our knowledge, no previous study has investigated the complex relationships among poor sleep quality and daytime sleepiness, anxiety and depressive symptoms, and quality of life among individuals with severe obesity. We hypothesized that the sleep problems that accompany severe obesity are associated with increasing psychological morbidity and reduced quality of life. Currently, the potential role of sleep in health and well-being of individuals with severe obesity is underappreciated. An understanding of interrelationships among sleep, mood, and quality of life could inform a more tailored approach to the prevention and management of severe obesity.
METHODS
Patients
Analyzed data had been collected as part of the evaluation of a regional specialist weight management service. Two hundred seventy adult patients (17 to 80 y old) consecutively enrolled into the service from January 2009 to October 2011 were included. Criteria for service enrolment were BMI ≥ 35 kg/m2 with a comorbidity (e.g., diabetes mellitus) or BMI ≥ 40 kg/ m2 without a comorbidity, based on recommended criteria from the UK National Institute for Health and Clinical Excellence guidance (NICE CG43).22 There was also a requirement for patients to have previously attended other weight management services (commercial/community/primary care) without successful results. Self-reported questionnaires assessing sleep habits (during the past month), anxiety-depression, and quality of life were collected at the first visit where detailed clinical information and anthropometric measures were collected from all patients. The study was done as part of service evaluation; therefore, no formal ethical approval was needed.
Measurements
Data collected included demographic information, height, weight, BMI, blood pressure, obesity comorbidities, and questionnaire information.
Questionnaire Evaluations
Sleep disturbance was assessed using the PSQI23 and daytime sleepiness using the Epworth Sleepiness Scale (ESS).24 Mood was assessed using the Hospital Anxiety and Depression Scale (HADS),25 and quality of life was assessed using Impact of Weight on Quality of Life-Lite (IWQOL-Lite).26
Sleep Disturbance
Sleep quality and sleep disturbance were assessed using the PSQI, a validated self-rated questionnaire that assesses sleep problems in seven aspects including sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction.23 A global score ranging from 0 to 21 is generated from the sum of the component scores. Individuals with total PSQI scores of ≥ 5 are identified as having severe sleep problems.23 Daytime sleepiness was also assessed using ESS, a validated self-report questionnaire with the maximum score of 24. It consists of eight questions with a four-point scale, which ask participants to rank the chance of dozing off in different situations (e.g., sitting and reading; as a passenger in a car for 1 h without a break). The higher the scores indicates the greater daytime sleepiness.24
Mood
Mood (anxiety, depression) was assessed using HADS, a 14-item questionnaire that has been developed to screen nonpsychiatric patients.25 It consists of two subscales; anxiety subscale (HADS-A) and depression subscale (HADS-D) each including seven items. Each item is measured on a four-point Likert scale, each ranging from 0 to 3, resulting in a maximum score of 21. A score above seven on each subscale implies the presence of potential distress. The following cutoff points were used to categorize the participants: 0-7 (noncase), 8-10 (borderline case), ≥ 11 (case).25
Quality of Life
Quality of life was assessed using the weight-specific IWQOL-Lite, a 31-item self-rated questionnaire.26 It measures weight-related quality of life in five areas: physical function, self-esteem, sexual life, public distress, work, and a total score. Each component was measured on a five-point scale, ranging from 1 to 5 (from “never true” to “always true”). The total score ranges from 0 to 100, with a higher score indicating better health-related quality of life.26
Data Analysis
Data were analyzed using the SPSS Version 18.0 (SPSS, Inc., Chicago, IL). Spearman correlation coefficients were used to assess associations between socio-demographic variables, clinical variables, and questionnaires scores. Associations among HADS-Anxiety and HADS-Depression and components of PSQI and ESS were assessed using multiple linear regression. Associations among components of IWQOL-Lite (physical function, self-esteem, sexual life, public distress, and work) and PSQI global score and ESS total score were also assessed using multiple linear regression. Analyses were adjusted for age, sex, hypertension, diabetes, and obstructive sleep apnea (OSA).
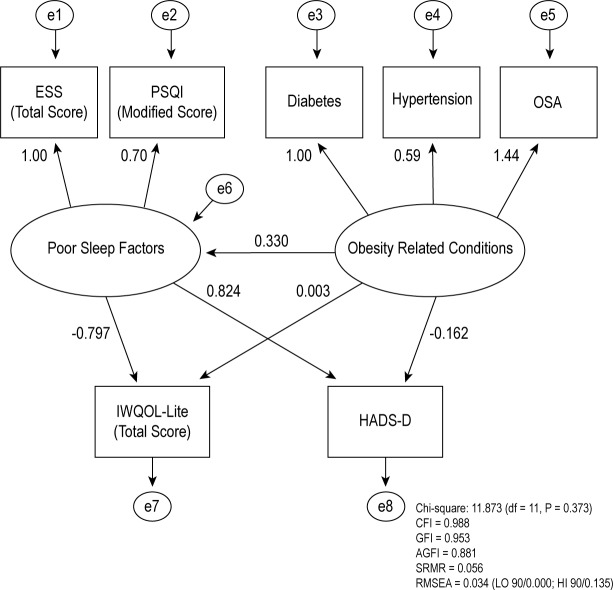
In general, common statistical analysis methods such as linear regression analysis, analysis of covariance, and factor analysis are widely used to examine the association between independent variables and outcome of interest, but these methods do not necessarily provide an explanation of how these variables relate to one another and what their overall effect is on outcome variables. Structural equation modeling (SEM) is a methodological tool used to overcome these limitations.27 We used SEM to determine whether our hypothesized model is valid. In our hypothesized model, the possible associations between poor sleep factors (PSQI and ESS) and obesity-related conditions (diabetes, hypertension, and OSA) in predicting HADS-Depression and IWQOL-Lite total score was assessed based on the proposed theoretical model using statistical package SPSS/ AMOS (Analysis of Moment Structures). We removed one of the questions of the PSQI “During the past month, how much of a problem has it been for you to keep up enough enthusiasm to get things done?” due to the similarity with one of the HADS questions “I have lost interest in things, definitely, sometimes, not much, not at all”. Poor sleep factors latent was defined by two variables; ESS score and modified score of PSQI, and obesity-related conditions was defined by three variables; hypertension, diabetes, and OSA. The total score of IWQOLLite and HADS depression score were assessed by both latent factors (endogenous factors). Maximum likelihood (ML) estimation approach28 was applied for the models with interaction terms that include a latent variable. A bootstrap method was utilized to investigate the direct, indirect and total effects between poor sleep factors and obesity-related conditions with the total score of IWQOL-Lite and HADS depression score.29 The advantage of bootstrapping is that it can create accurate standard errors that are independent of assumptions for a normal distribution of data, required for calculation of regression weight by AMOS/SEM. It can also provide the probability levels for direct, indirect, and total effect.29 Five fit indices were used to assess the adequacy of model fit: (1) the comparative fit index (CFI) > 0.90; (2) goodness-of-fit statistic (GFI) > 0.95; (3) adjusted goodness-of-fit statistic (AGFI) > 0.90; (4) standardized root mean square residual (SRMR) < 0.08; and (5) root mean square error of approximation (RMSEA) < 0.05 and the upper bound of its 90% confidence interval < 1 values indicate a good fit.27 Two-tailed tests were used throughout and a P < 0.05 was considered statistically significant.
RESULTS
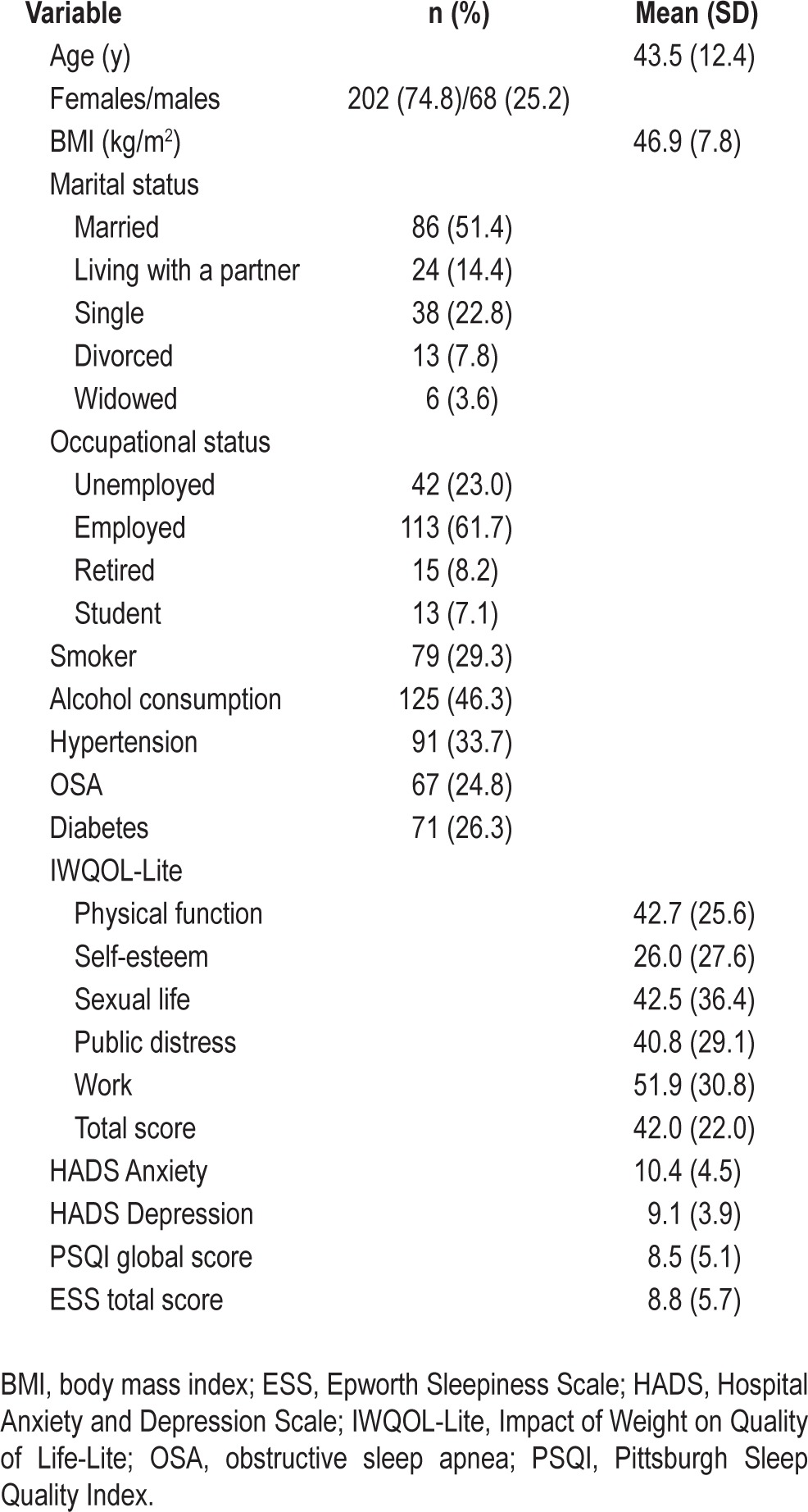
A total of 270 patients (202 female) were enrolled. The baseline characteristics of the participants are presented in Table 1. The mean (standard deviation; SD) age was 43.3 (12.6) y. The mean BMI was 46.9 (7.8) kg/m2. The mean PSQI global score was 8.6 (5.0) and 74.8% of patients were poor sleepers (PSQI total score ≥ 5). The mean ESS score was 8.8 (5.7). Approximately, 52% of all participants were considered anxious (HADS-Anxiety, subscore > 7) and 43% were depressed (HADS-Depression, subscore > 7). The self-esteem component of IWQOL-Lite with the score of 26.0 (27.6) had the lowest score compared to the other components (Table 1).
Table 1.
Descriptive characteristics of 270 participants of the study
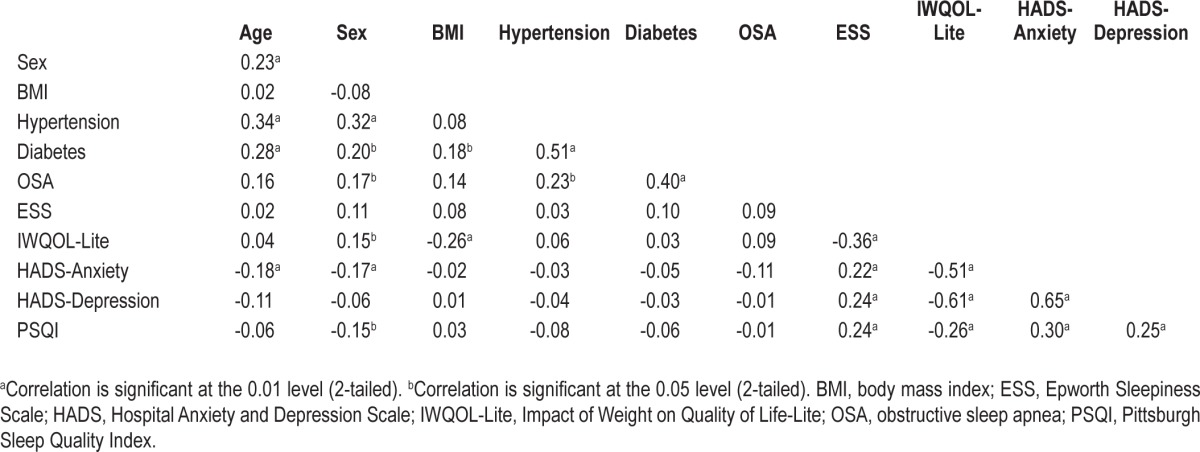
PSQI continuous score was significantly associated with IWQOL-Lite continuous (r = -0.26; indicating that poor sleep was associated with worse quality of life score), and significantly with HADS-Anxiety (r = 0.30), and also significantly with HADS-Depression (r = 0.25), indicating poor sleep quality was associated with mood disturbance (Table 2). ESS continuous score also showed a significant association with IWQOL-Lite (r = -0.36), HADS-Anxiety (r = 0.22), and HADS-Depression (r = 0.24) (Table 2).
Table 2.
Bivariate correlations between sociodemographic and clinical variables, and questionnaire scores
A series of multiple linear regression analyses was performed in order to evaluate the associations among levels of anxiety and depression symptoms with components and total score of PSQI and ESS; they are summarized in Table 3 and Table 4. Our analyses demonstrated that HADS-Anxiety and HADS-Depression scores (outcome variables) were significantly associated with all the components of PSQI except sleep disturbance, use of sleeping medication, and daytime dysfunction. The PSQI global score had a positive significant association with anxiety (β = 0.29; P = 0.01) and depression (β = 0.31; P < 0.01) components of HADS (Table 3).
Table 3.
Association between the Hospital Anxiety and Depression Scale (HADS) anxiety and depression scores with components and global score of Pittsburgh Sleep Quality Index (PSQI)
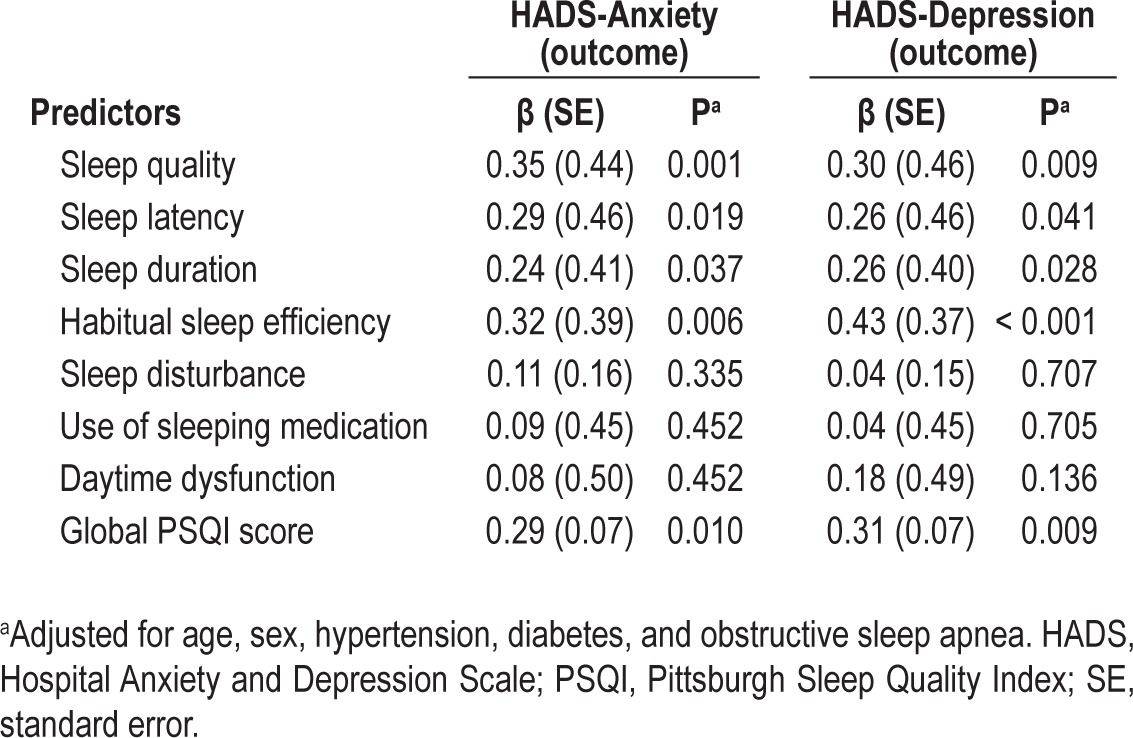
Table 4.
Association between the Hospital Anxiety and Depression Scale anxiety and depression scores with components and total score of Epworth Sleepiness Scale
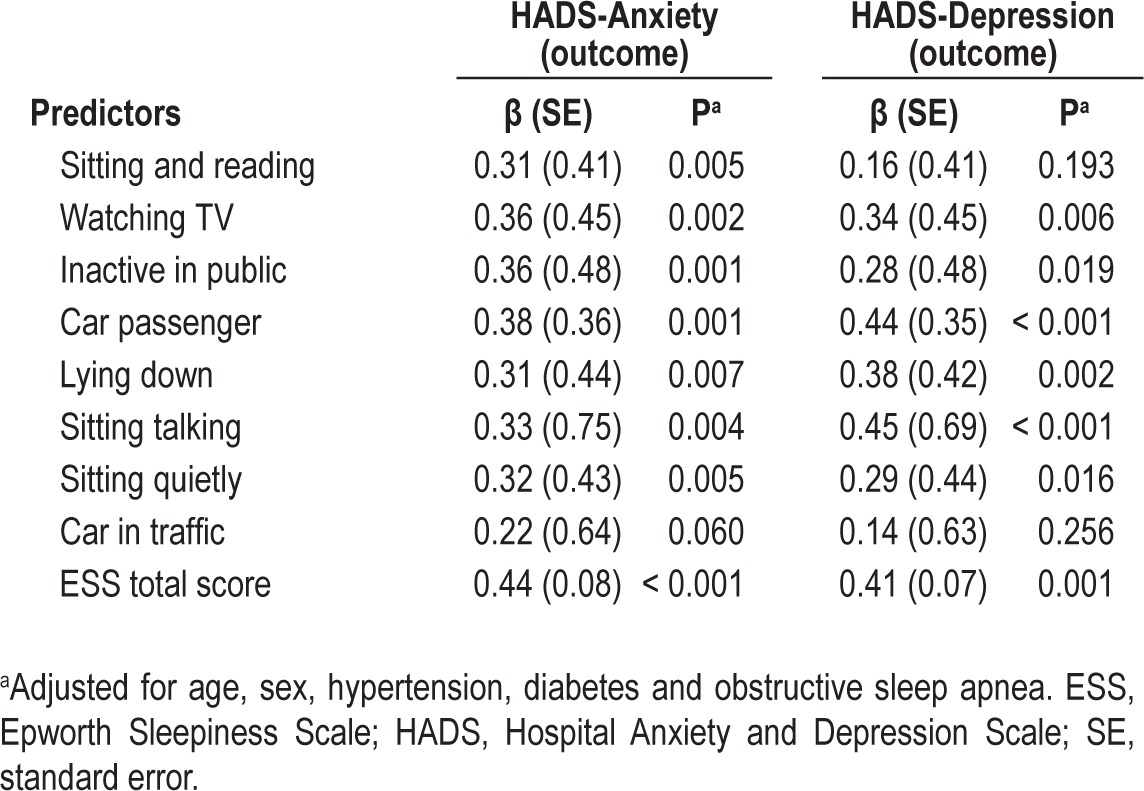
HADS-Anxiety was associated with all the components of ESS except the score of dozing off in the situation “car in traffic”. HADS-Depression was associated with all the components of ESS except the score of dozing of in the situations of “sitting and reading” and “car in traffic”. Excessive daytime sleepiness was highly associated with anxiety (β = 0.44; P < 0.001) and depression (β = 0.41; P = 0.01) components of HADS (Table 4). The above models were adjusted for age, sex, hypertension, diabetes, and OSA.
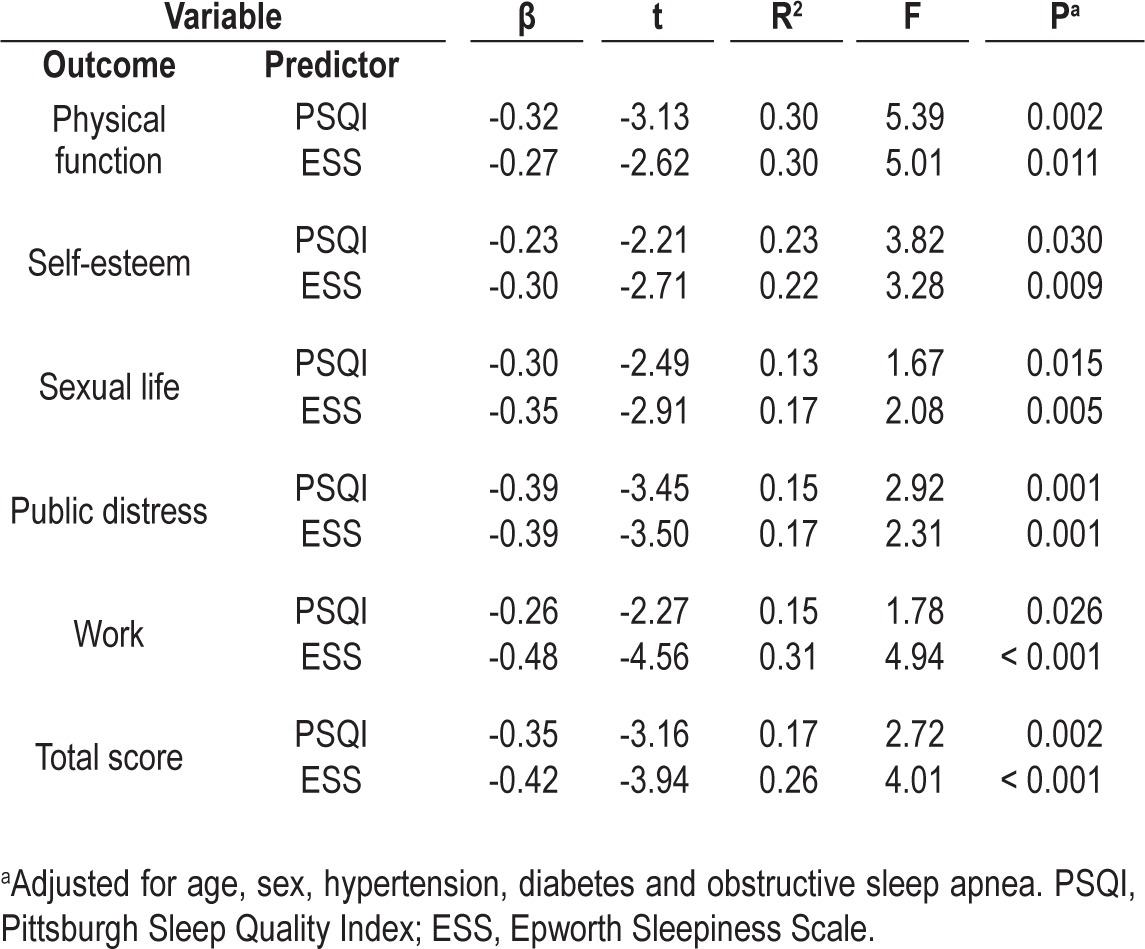
The association of IWQOL-Lite (outcome variable) with PSQI global score and ESS total score are presented in Table 5. After adjusting for age, sex, hypertension, diabetes and OSA, PSQI was significantly associated with physical function (β = -0.32; P < 0.01), self-esteem (β = -0.23; P = 0.03), sexual life (β = -0.30; P = 0.01), public distress (β = -0.39; P < 0.01), work (β = -0.26; P = 0.02), and total score (β = -0.35; P < 0.01). Similarly, ESS were also associated with physical function (β = -0.27; P < 0.01), self-esteem (β = -0.30; P < 0.01), sexual life (β = -0.35; P < 0.01), public distress (β = -0.39; P = 0.001), work (β = -0.48; P < 0.001), and total score (β = -0.42; P < 0.001).
Table 5.
The association between subjective sleep disturbances (Pittsburgh Sleep Quality Index global score and excessive daytime sleepiness) with components of Impact of Weight on Quality of Life
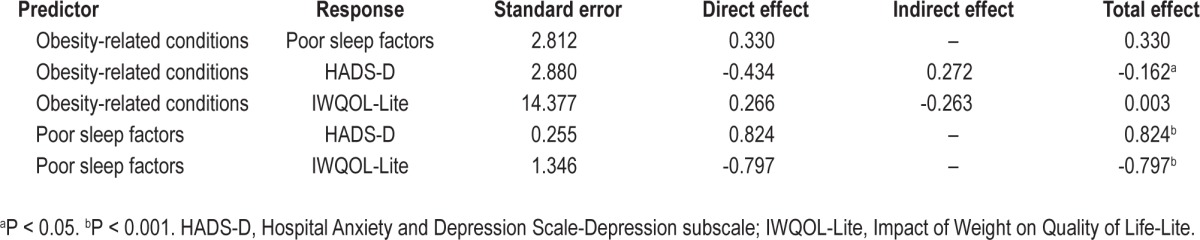
We tested an SEM (Figure 1), representing the hypothesized model in which poor sleep factors latent was defined by two variables; ESS and PSQI, and obesity- related conditions was defined by three variables (hypertension, diabetes, and OSA) set to predict the total IWQOL-Lite score and HADS-Depression score (endogenous variables). The results postulated that our hypothesized model had a good fit to the data. The CFI was 0.988, the GFI was 0.953, the AGFI was 0.881, the SRMR was 0.056, and the RMSEA was 0.034, with a 90% confidence interval of 0.000-0.135 indicating a good fit of the model. Obesity-related conditions was negatively associated with HADS-D (β = -0.16; P < 0.05), poor sleep factors was positively associated with HADS-D (β = 0.82; P < 0.001) and was negatively associated with IWQOL-Lite (β = -0.79; P < 0.001). A summary of standard errors, direct effects, indirect effects, and total effects based on 1000 bootstrap sample is presented in Table 6. The strongest standardized total (direct and indirect) effect was of poor sleep factors on HADS-D and was 0.82.
Figure 1.
Measurement model (standardized estimates).
Table 6.
Standardized effect size based on 1,000 bootstrap samples
DISCUSSION
Obesity is a complex condition associated with biological, psychological, and social complications. Associations among sleep duration and sleep quality, and obesity and its complications are increasingly described. Although greatest attention has been paid to sleep potentially predisposing to obesity, apart from studies on sleep disordered breathing, little is known about the effect of sleep duration and quality once obesity has occurred. In a population of patients with severe obesity, we examined the associations among sleep, mood, and quality of life.
The current study found that poor sleep quality, anxiety and depression symptoms, and reduced quality of life were highly prevalent among patients with severe obesity. More than two-thirds of patients with severe obesity reported poor sleep quality and the mean (standard deviation) self-reported sleep duration was 6 h and 20 min (1 h and 30 min). We also found that poor sleep quality and excessive daytime sleepiness were strongly associated with mood disturbance and poorer quality of life. After controlling for age, sex, hypertension, diabetes, and OSA, sleep quality and daytime sleepiness were significantly associated with mood disturbance and quality of life impairment.30
A growing body of epidemiological evidence indicates that both sleep quantity and quality are associated with increased risk of obesity.4 Several potential mechanisms have been proposed for the sleep-obesity relationship, including alterations in metabolic hormones.31 Once severe obesity occurs, the management of obesity through lifestyle change and medical approaches becomes more difficult; thus, bariatric surgery is recommended by several international guidelines for this patient population.32 Despite the success of bariatric surgery in weight loss, significant psychological morbidity may still remain. To improve success with interventions, including bariatric surgery, to treat severe obesity, a greater understanding of factors that maintain obesity and its comorbidities is necessary.
Our findings demonstrate that severely obese individuals obtained less sleep and reported poor sleep quality. This is in agreement with recent observations by Toor and colleagues33 who evaluated sleep duration of individuals with extreme obesity compared to nonobese controls, and reported that obese individuals slept less and also had higher PSQI score less than nonobese controls. They also reported that bariatric surgery dramatically improved both duration and quality of sleep. Bidulescu and colleagues,34 in an analysis of data from 1,515 residents of metropolitan Atlanta in the Cardiovascular Health Epidemiology Study, demonstrated that perceived stress mediated with the associations between reduced sleep quality and obesity. Another similar study investigated the correlates of poor sleep quality among 2,803 individuals. The study demonstrated that being female and being overweight/obese were strong predictors of poor sleep quality among these individuals even after controlling for potential confounders such as cardio-metabolic risk factors.35 A recent published randomized controlled study12 highlighted the role of sleep quantity and quality in prediction of weight loss among women with a mean age of 45 y. The results indicated that poor sleep quality (PSQI scores above the clinical cutoff of 5) or sleep ≤ 7h/night were associated with a 28% lower probability of continuation with a successful weight loss programmes at 18 mo from the baseline.
The severely obese individuals in our study also reported high anxiety and depressive symptoms and low quality of life. The results from a cross-sectional study of McDonough and colleagues36 demonstrated that compared to individuals with normal weight, over-weight, and obese individuals reported lower health-related quality of life (HRQoL). There is a close link between obesity and depression. Algul and colleagues37 postulated that compared to healthy controls, the obese group are more depressed, had lower quality of life, and higher sleep disturbance.
The bidirectional association between sleep and depression makes it difficult to infer any causal pathways between them.16 A great number of longitudinal studies16,38–40 have consistently highlighted the role of insomnia in prediction of depression over time. Szklo-Coxe and colleagues39 assessed the associations between insomnia and incidence of depression in a sample of 555 nonobese participants age 33 to 71 y, who were free of any depression symptoms at baseline. They reported that insomnia was strongly associated with higher odds for incident of depression up to fivefold after 4-y follow-up.
The mechanism underlying the association between sleep disturbance and reduced quality of life is not known. Sleep disturbance, and particularly daytime sleepiness, can result in low energy level, which could be a potential marker for impaired physical function of HRQoL. In the Sleep Heart Health Study41 assessing the association between sleep difficulties, including difficulty initiating and maintaining sleep, daytime sleepiness, and quality of life, individuals with higher levels of sleepiness (ESS ≥ 11) reported poorer quality of life in all of the subscales of 36-Item Short Form Health Survey (SF-36).41
Our study demonstrated that sleep disturbance was strongly associated with anxiety and depressive symptoms and also was associated with reduced quality of life among severely obese individuals. Thus, there is a need to screen for sleep problems among severely obese individuals. The prevalence of sleep problems such as excessive daytime sleepiness and short sleep duration is relatively high among these obese subjects.42 Although short sleep duration has been recognized as an important risk factor for obesity, data on the effect of sleep improvement on obesity are lacking. Improving sleep duration and quality could potentially prevent worsening obesity and prevent initiation and progression of psychological comorbidities such as depression and anxiety. In a randomized controlled trial, Reid and colleagues43 investigated the effectiveness of aerobic exercise and sleep hygiene education program on sleep, mood, and quality of life among nonobese adults aged ≥ 55 y. They observed that, compared to the control group, the intervention group had significant reductions in daytime sleepiness, depressive symptoms, and improvements in quality of life.43
We investigated the potential link between PSQI and ESS with HADS-Anxiety, HADS-Depression scores, and IWQOLLite via the utilization of linear regression models. The data are cross sectional and causal pathways among these variables cannot be inferred. We used SEM analysis to test whether poor sleep factors negatively influence mood or vice versa. Interestingly, our hypothesized SEM model that was presented earlier supported our prior linear model findings. We hypothesized that sleep can be influenced by obesity-related conditions, and both poor sleep factors and obesity-related conditions may influence quality of life and mood of the participants.
Our study has merit in sample size and a detailed statistical analysis. Our study has also has several limitations. The main limitation is the cross-sectional design, so direct causal relationship between sleep disturbances and anxiety and depressive symptoms cannot be inferred. Another limitation is using self-report questionnaires. PSQI is a reliable and validate instrument; however, it cannot be used as an accurate diagnostic tool.
In conclusion, sleep disturbance characterized by poor sleep quality and daytime sleepiness is independently associated with mood disturbance and reduced quality of life among extremely obese patients. The role of sleep in psychosocial health and well-being is less appreciated in general clinical practice. Our findings suggest that routine screening for sleep disorders in obese populations would be beneficial. The early detection of such problems could prevent the potential development and perpetuation of psychological disorders among these individuals that may affect their efforts to address their obesity.
DISCLOSURE STATEMENT
This was not an industry supported study. Marzieh Hosseini Araghi, Alison Jagielski, and Shahrad Taheri are funded by the National Institute for Health Research (NIHR) through the Collaborations for Leadership in Applied Health Research and Care for Birmingham and Black Country (CLAHRC-BBC) program. The views expressed in this publication are not necessarily those of the NIHR, the Department of Health, NHS South Birmingham, University of Birmingham or the CLAHRC BBC Theme 8 Management/Steering Group. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors are grateful to the patients attending the weight management service and service staff of Heart of England NHS Foundation Trust.
Contributions
Shahrad Taheri developed the clinical patient evaluation plan. Shahrad Taheri and Marzieh Hosseini Araghi designed the study plan. Marzieh Hosseini Araghi, Alison Jagielski, Iraida Neira, and Adrian Brown contributed to data collection, data entry, and data cleaning. Marzieh Hosseini Araghi and Shahrad Taheri devised the analysis plan. Marzieh Hosseini Araghi carried out the analysis and produced the first manuscript draft. Shahrad Taheri and G. Neil Thomas contributed to early revisions. All authors contributed to the interpretation of the data, discussion, and preparation of final manuscript.
REFERENCES
- 1.Sturm R. Increases in morbid obesity in the USA: 2000-2005. Public Health. 2007;121:492–6. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–47. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Taheri S, Thomas GN. Is sleep duration associated with obesity-where do U stand? Sleep Med Rev. 2008;12:299–302. doi: 10.1016/j.smrv.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 6.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB. Self-reported sleep quality is associated with the metabolic syndrome. Sleep. 2007;30:219–23. doi: 10.1093/sleep/30.2.219. [DOI] [PubMed] [Google Scholar]
- 9.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–4. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta NK, Mueller WH, Chan W, Meininger JC. Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol. 2002;14:762–8. doi: 10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- 12.Thomson CA, Morrow KL, Flatt SW, et al. Relationship between sleep quality and quantity and weight loss in women participating in a weight-loss intervention trial. Obesity (Silver Spring) 2012;20:1419–25. doi: 10.1038/oby.2012.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vgontzas AN, Bixler EO, Chrousos GP, Pejovic S. Obesity and sleep disturbances: meaningful sub-typing of obesity. Arch Physiol Biochem. 2008;114:224–36. doi: 10.1080/13813450802521507. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton NA, Nelson CA, Stevens N, Kitzman H. Sleep and psychological well-being. Social Indicators Research. 2007;82:147–63. [Google Scholar]
- 15.Wiebe ST, Cassoff J, Gruber R. Sleep patterns and the risk for unipolar depression: a review. Nat Sci Sleep. 2012;4:63–71. doi: 10.2147/NSS.S23490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64:443–9. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 17.Mystakidou K, Parpa E, Tsilika E, Gennatas C, Galanos A, Vlahos L. How is sleep quality affected by the psychological and symptom distress of advanced cancer patients? Palliat Med. 2009;23:46–53. doi: 10.1177/0269216308098088. [DOI] [PubMed] [Google Scholar]
- 18.Dorheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32:847–55. doi: 10.1093/sleep/32.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shao MF, Chou YC, Yeh MY, Tzeng WC. Sleep quality and quality of life in female shift-working nurses. J Adv Nurs. 2010;66:1565–72. doi: 10.1111/j.1365-2648.2010.05300.x. [DOI] [PubMed] [Google Scholar]
- 20.Thulin H, Kreicbergs U, Wijkstrom H, Steineck G, Henningsohn L. Sleep disturbances decrease self-assessed quality of life in individuals who have undergone cystectomy. J Urol. 2010;184:198–202. doi: 10.1016/j.juro.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Price DW, Ma Y, Rubin RR, et al. Depression as a predictor of weight regain among successful weight losers in the diabetes prevention program. Diabetes Care. 2013;36:216–21. doi: 10.2337/dc12-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute for Health and Clinical Excellence. CG43 obesity: full guideline, section 1—introduction, methods and recommendations. 2006. http://guidance.nice.org.uk/CG43/Guidance/Section/1/pdf/English.
- 23.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 24.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 25.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 26.Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9:102–11. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 27.Kline BP. 2nd ed. New York City: The Guilford Press; 2005. Principles and practice of structural equation modeling. [Google Scholar]
- 28.Klein A, Moosbrugger H. Maximum likelihood estimation of latent intraction effects with the LMS mthod. Psychometrika. 2000;65:457–74. [Google Scholar]
- 29.Byrne BM. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. Structural equation modeling with AMOS:Basic concepts, applications, and programming. [Google Scholar]
- 30.D'Ambrosio C, Bowman T, Mohsenin V. Quality of life in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure-a prospective study. Chest. 1999;115:123–9. doi: 10.1378/chest.115.1.123. [DOI] [PubMed] [Google Scholar]
- 31.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. 2008;31:1087–96. [PMC free article] [PubMed] [Google Scholar]
- 32.NICE. London: National Institute for Health and Clinical Excellence; 2006. Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. [Google Scholar]
- 33.Toor P, Kim K, Buffington CK. Sleep quality and duration before and after bariatric surgery. Obes Surg. 2012;22:890–5. doi: 10.1007/s11695-011-0541-8. [DOI] [PubMed] [Google Scholar]
- 34.Bidulescu A, Din-Dzietham R, Coverson DL, et al. Interaction of sleep quality and psychosocial stress on obesity in African Americans: the Cardiovascular Health Epidemiology Study (CHES) BMC Public Health. 2010;10:581. doi: 10.1186/1471-2458-10-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, Chang CJ. The association between self-reported sleep quality and overweight in a Chinese population. Obesity (Silver Spring) 2013;21:486–92. doi: 10.1002/oby.20259. [DOI] [PubMed] [Google Scholar]
- 36.McDonough C, Dunkley AJ, Aujla N, Morris D, Davies MJ, Khunti K. The association between body mass index and health-related quality of life: influence of ethnicity on this relationship. Diabetes Obes Metab. 2013;15:342–8. doi: 10.1111/dom.12033. [DOI] [PubMed] [Google Scholar]
- 37.Algul A, Ates MA, Semiz UB, et al. Evaluation of general psychopathology, subjective sleep quality, and health-related quality of life in patients with obesity. Int J Psychiatry Med. 2009;39:297–312. doi: 10.2190/PM.39.3.f. [DOI] [PubMed] [Google Scholar]
- 38.Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Yoon JS. Insomnia, depression, and physical disorders in late life: a 2-year longitudinal community study in Koreans. Sleep. 2009;32:1221–8. doi: 10.1093/sleep/32.9.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Szklo-Coxe M, Young T, Peppard PE, Finn LA, Benca RM. Prospective associations of insomnia markers and symptoms with depression. Am J Epidemiol. 2010;171:709–20. doi: 10.1093/aje/kwp454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- 41.Baldwin CM, Ervin AM, Mays MZ, et al. Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. J Clin Sleep Med. 2010;6:176–83. [PMC free article] [PubMed] [Google Scholar]
- 42.Vgontzas AN, Bixler EO, Tan TL, Kantner D, Martin LF, Kales A. Obesity without sleep apnea is associated with daytime sleepiness. Arch Intern Med. 1998;158:1333–7. doi: 10.1001/archinte.158.12.1333. [DOI] [PubMed] [Google Scholar]
- 43.Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010;11:934–40. doi: 10.1016/j.sleep.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]