Abstract
Study Objectives:
Idiopathic REM sleep behavior disorder (iRBD) is characterized by atypical REM sleep motor activity, vivid dreams and nightmares, and dream-enacting behaviors that can result in injuries to the patient and bed partner. It is also a known predictor of Parkinson disease (PD). Alexithymia has been associated with disturbances in sleep and dreaming (e.g., nightmares) and is a non-motor symptom of PD. We assessed alexithymia and disturbed dreaming in iRBD patients with the aim of determining if these two factors are elevated and interrelated among this population.
Design:
Questionnaire study of clinically diagnosed patients.
Setting:
Clinical sleep disorders center.
Patients or participants:
Thirty-two iRBD patients and 30 healthy age- and sex-matched control participants.
Measurements and Results:
Participants completed the 20-item Toronto Alexithymia Scale (TAS-20), the Dream Questionnaire, and the Beck Depression Inventory. iRBD patients obtained higher TAS-20 total scores (62.16 ± 13.90) than did controls (52.84 ± 7.62; F1,59 = 10.44, P < 0.01), even when controlling for depressive symptoms, and more frequently attained the suggested cutoff for alexithymia than did controls (P < 0.01). iRBD patients obtained higher scores on the Difficulty Identifying Feelings alexithymia subscale. For both iRBD and control groups, the Difficulty Indentifying Feelings subscale correlated positively with the Nightmare Distress scale of the Dream Questionnaire.
Conclusions:
Elevated alexithymia scores among idiopathic rapid eye movement sleep behavior disorder patients, and especially a difficulty in identifying feelings, parallels evidence of dysautonomia in this population. The higher incidence of distressing nightmares and the association of nightmares with alexithymia further extend similar findings for both clinical and non-clinical samples and suggest that an affect regulation disturbance may be common to the two sets of symptoms.
Citation:
Godin I; Montplaisir J; Gagnon JF; Nielsen T. Alexithymia associated with nightmare distress in idiopathic REM sleep behavior disorder. SLEEP 2013;36(12):1957-1962.
Keywords: REM sleep behavior disorder, alexithymia, nightmares, dysautonomia
INTRODUCTION
Idiopathic REM sleep behavior disorder (iRBD) is characterized by potentially injurious sleep motor activity associated with dream mentation1,2 and an intermittent or complete loss of normal REM sleep atonia.1,3 Dream content is vivid.2,5,6 and thought to be more violent in RBD patients than in healthy adults, although the latter finding has been challenged.4 RBD is a known risk factor for neurodegenerative syndromes,7 especially Parkinson disease (PD), multiple-system atrophy, and dementia with Lewy bodies. It often precedes the onset of these syndromes by as much as 10 to 15 years.7
The emotional symptoms of iRBD patients are not yet well understood. Elevated levels of daytime passivity have been noted anecdotally5 and documented as lower scores on aggressiveness questionnaires.2,4 Higher anxiety levels have been reported among children with RBD9 and higher anxiety and depression levels among adults with PD.10 PD patients show higher levels of alexithymia features,11,12 especially patients with postural instability/gait symptoms.13 But alexithymia has not yet been evaluated in iRBD patients.
Alexithymia most commonly refers to a difficulty in identifying and describing feelings, a difficulty in distinguishing feelings from bodily sensations of emotional arousal, a lack of fantasies, and an overly concrete style of thinking.14–18 It is known to be a risk factor for depression,19 anxiety, dissociative symptoms in PTSD,20–22 somatic symptoms,23 eating disorders,24 and poor response to psychotherapy.25 Depressive patients with alexithymia show more severe symptoms than their non-alex-ithymic counterparts.25,26 Alexithymia is also associated with reduced life satisfaction27 and is prospectively associated with all-cause mortality, even among healthy individuals.28
Alexithymia has been associated with general alterations in dreaming,18 e.g., individuals high in alexithymia have poorer recall of their dreams, have simpler and shorter dreams, and show a lack of interest in their dreams.29–32 It has also been associated with many sleep problems, including insomnia, excessive sleepiness, and sleepwalking. In particular, it has been reliably linked to the occurrence of nightmares.33–36
The frequent occurrence of nightmares among RBD patients, and RBD's association with PD, suggest that iRBD patients, too, may suffer from an alexithymia deficit. The aim of this study was therefore to assess alexithymia and nightmare distress in iRBD patients using standardized measures and to compare this group to a matched group of healthy participants. We expected to find iRBD patients to have a higher prevalence and higher levels of alexithymia and greater nightmare distress. We also expected to find a correlation between alexithymia levels and nightmares in both controls and iRBD participants.
METHODS
Participants
Thirty-four iRBD patients (25 men; mean age: 62.0 ± 10.8 years) and 31 healthy age and sex matched control participants (19 men; mean age, 56.9 ± 16.61 years) were studied. Control participants were recruited through a newspaper advertisement or by word of mouth. All were screened for mental, neurologic or medical conditions with a medical history, a neuropsycho-logical battery, polysomnographic (PSG) recording, and the BDI-II. Patients showed no signs of any other neurodegenerative syndrome or medical condition that might have an impact on sleep (sleep apnea syndrome, insomnia, etc). Two patients and one control had missing responses on their questionnaires and were thus removed from the analyses. Thus, the final sample consisted of 32 iRBD patients (23 men; mean age: 61.5 ± 11.12 years; education: 12.97 ± 3.94 years) and 30 controls (19 men; mean age, 57.2 ± 14.47 years; education: 13.59 ± 3.19 years). Six of the iRBD patients had a history of mood disorder, and 3 reported having previously suffered an anxiety disorder. At the time of the PSG, 4 RBD patients took an anticonvulsant medication, and 6 took both an anxiolytic and an antidepressant. Of the control participants, none had a history of psychiatric trouble, and none was taking a psychoactive medication.
RBD was diagnosed by a physician according to the International Classification of Sleep Disorders, second edition (ICSD-II) criteria,37 that is, the presence of excessive muscle activity during REM sleep (> 30% of REM sleep with tonic EMG activity or > 15% of REM sleep with phasic EMG activity) and ≥ 1 of the following: history of disruptive sleep behaviors, abnormal REM sleep behaviors confirmed by PSG monitoring with synchronized videotape.
A university-affiliated hospital ethics review board approved the protocol, and written informed consent to participate was obtained.
Procedures
Alexithymia was assessed with the 20-item Toronto Alexithymia Scale (TAS-20), an extensively validated self-report questionnaire.38–41 The TAS-20 uses 1-5 Likert-type scales where 1 = strongly disagree, 2 = moderately disagree, 3 = neither agree nor disagree, 4 = moderately agree, and 5 = strongly agree. It consists of 3 subscales assessing difficulty identifying feelings (DIF), difficulty describing feelings (DDF), and externally oriented thinking (EOT). The TAS-20 total score has been used38,39 to categorize participants as either non-alexithymic (scores from 20-51), borderline alexithymic (52-60), or alexithymic (≥ 61). The Beck Depression Inventory-II42 was also given to assess comorbid depressive symptoms.
Dreams were assessed with a previously validated Dream Questionnaire35 on which items were scored with the same scales used for the TAS-20. The Dream Questionnaire consists of 3 subscales: Nightmare Distress, Dream Recall, and belief in Dream Meaning. iRBD patients were referred for at least one night of PSG recording in the hospital sleep clinic. Questionnaires were administered on the evening of the first night of recording. Patients and control participants reported themselves to be free of any medications known to influence sleep, vigilance, or motor activity for ≥ 1 week before the PSG evaluation. The recording montage included 2 EEG leads (C3/A2 and O2/A1), left and right electroculogram (EOG), and a chin electromyogram (EMG). All recordings were conducted by trained PSG technicians. Sleep stages 1-4 were scored by a highly proficient PSG technician according to a standard method,43 and REM sleep was scored on the basis of EEG and EOG recordings using a method developed in our center.44,45 Healthy controls and iRBD patients did not differ on any PSG variables other than lower REM sleep atonia in iRBD patients.
Between-groups comparisons on the TAS-20 total score, on age, and on years of education were investigated with 2 × 2 ANOVA designs. A χ2 test was used to compare groups on their alexithymia classification (not alexithymic, borderline, or alexithymic). MANOVAs were used to investigate differences on the 3 scales of the Dream Questionnaire and the 3 scales of the TAS-20 and interactions between group and sex. A 2 × 2 ANCOVA with BDI-II score as covariate was used to control the effect of depressive symptoms on the TAS-20 total score. Pearson correlations were used to assess relationships between scales of the Dream Questionnaire and the TAS-20 variables separately for the 2 groups.
RESULTS
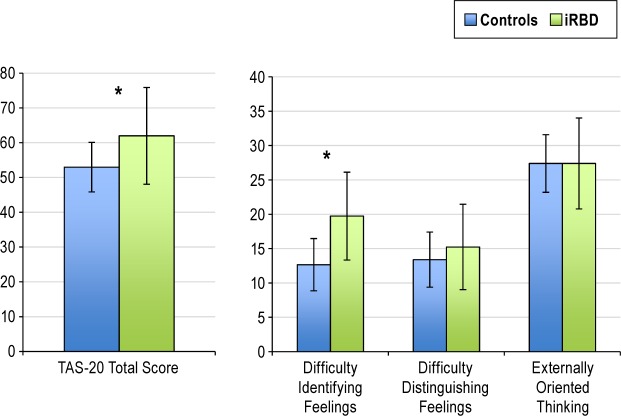
iRBD patients obtained higher TAS-20 total scores (62.16 ± 13.90) than did controls (52.84 ± 7.62; F1,59 = 10.44, P < 0.001; see Figure 1). Men and women did not differ on TAS-20 total score (P > 0.43), and there was no interaction between Group and Sex (P > 0.33). There were no significant between-group differences for years of education (P > 0.82) and age (P > 0.15). Twenty-one iRBD patients (65%) but only 6 controls (20%) attained the cutoff for alexithymia; 5 iRBD (16%) and 10 controls (33%) were borderline alexithymic; and 6 iRBD (18%) and 14 controls (47%) were not alexithymic (χ2 = 11.99, df = 2, P < 0.01). These 3 categories of iRBD patients did not differ on age, education, BDI-II score, psychiatric history, or intake of medication (P > 0.18).
Figure 1.
Comparisons between iRBD and Controls on the Toronto Alexithymia Scale-20 total score and the three TAS-20 subscales: iRBD patients scored higher on TAS-20 total score (left panel) and the Difficulty Identifying Feelings subscale (right panel). *P < 0.05.
When controlling for depressive symptoms, iRBD patients still had higher TAS-20 total scores (67.3 ± 3.82) than did controls (49.84 ± 3.82, F1,20 = 5.49, P < 0.05), and there was no difference between men and women (P > 0.80). iRBD patients (19.74 ± 6.51) scored higher than controls (12.67 ± 3.15) on the DIF subscale of the TAS-20 (F1,56 = 12.79; P < 0.001, Figure 1), but did not differ on the DDF (P > 0.08) or EOT subscales (P > 0.99). iRBD patients scored higher (15.05 ± 4.80) than controls (9.00 ± 3.90) on the Nightmare Distress subscale of the Dream Questionnaire (F1,60 = 22.28; P < 0.001, Figure 2), but not on the Dream Recall (P > 0.97) or Dream Meaning (P > 0.62) subscales. There were again no Sex main effects or Group × Sex interactions for any of the 3 Dream Questionnaire subscales (all P > 0.32).
Figure 2.
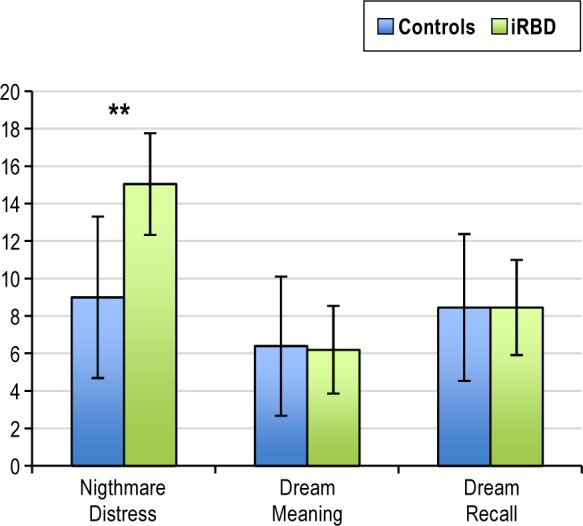
Comparisons between iRBD patients and matched control participants on the Dream Questionnaire subscales. **P < 0.01.
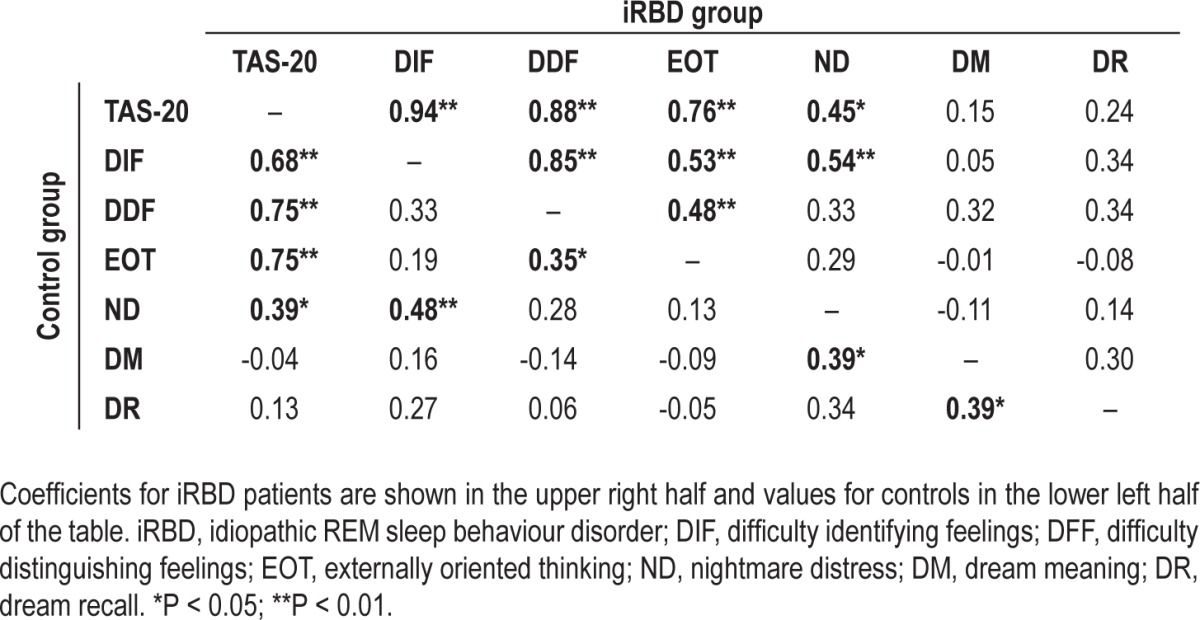
As shown in Table 1, the TAS-20 total and DIF scores correlated positively with Nightmare Distress score for both iRBD patients (r = 0.45, P < 0.05 and r = 0.54, P < 0.01, respectively) and controls (r = 0.39, P < 0.05; r = 0.48, P < 0.01).
Table 1.
Correlations between TAS-20 total score, TAS-20 subscales (DIF, DFF, EOT) and Dream Questionnaire subscales (ND, DM, DR)
DISCUSSION
The results demonstrate substantially higher alexithymia scores and a higher proportion of individuals falling in the alex-ithymic category in a population of iRBD patients relative to matched healthy controls. This finding extends a previous finding that alexithymia scores are elevated in PD patients,11 a population for whom RBD is frequently comorbid or a significant precursor condition. The difference in alexithymia scores was obtained even after controlling for a parallel difference in depressive symptoms, for which RBD patients may also be at risk. Alexithymia and depression are overlapping constructs, but the present results support the idea that they are substantially independent.46 Nonetheless, similar to other patients with comorbid alexithymia and depression, iRBD patients in our sample may have an elevated risk of developing psychiatric and health problems.19,26,47 Further, the most severely alexithymic patients may have a greater incidence of all-cause mortality.28
Our sample of iRBD patients was particularly deficient on the TAS-20 subscale that assesses difficulties in identifying feelings (DIF), a subscale that previous work has shown is elevated for patients possessing a variety of sleep disorder symptoms.33,35,48 Our patients, however, did not differ from controls on any objective measure of NREM sleep. Thus, the alexithymia deficit in iRBD patients may not be a unique comorbid symptom but rather a more general symptom reflective of alterations in REM sleep, such as reduced and variable muscle atonia, strong intermittent muscle twitching, reduced heart rate variability, vivid, repetitive, and stereotypical dreams and nightmares, and overt dream-enactments. This is narrowly consistent with claims that alexithymia is secondary to sleep problems to the extent that such problems affect REM sleep.49–51
The additional findings that our iRBD patients suffer from more nightmare distress than control participants and that their levels of nightmare distress are correlated with severity on the alexithymia total and DIF scales suggest that the alexithymia deficit for these patients may be comorbid even more specifically with the occurrence of nightmares. The higher frequency of nightmare distress reported by our iRBD patients extends results from previous studies in which dream content has been found to be more violent in RBD,2,5,6 although the latter finding has been contested for a sample of medicated patients.4
Confidence in our findings is bolstered by the fact that previous studies have shown high DIF scores to be associated with high nightmare distress in both clinical and non-clinical populations and for men and women considered separately.35 In fact, this DIF-nightmare distress association also replicates the findings of two previous studies demonstrating that both TAS-20 total and DIF scores correlate with nightmare frequency31 and other nightmare symptoms.33
We previously suggested that this relationship between DIF and nightmare distress reflects either a more generalized disposition to react negatively to events (“affect distress” personality style) or a deficit in emotion regulation processes. An affect distress explanation of the present findings seems unlikely because iRBD patients display a contrary style of passivity and non-aggressiveness.2,4,8 Rather, an emotional dysregulation explanation provides a better fit with some iRBD symptoms. To illustrate, emotional dysregulation has been put forward as a factor that leads alexithymic individuals to display excessive, unexpected emotional outbursts when awake and bizarre emotional dreams and nightmares when asleep.15 In the case of iRBD patients, these outbursts may be restricted to REM sleep, although sporadic emotional outbursts during wakefulness have not to our knowledge been assessed for this population. An emotion dysregulation explanation is also broadly consistent with evidence of higher anxiety and depression levels in child RBD patients9 and in PD patients10 and with accumulating evidence that dreaming and REM sleep play roles in the cross-night regulation of negative emotions.52,53
This deficit may be related to dysfunctions in prefrontal regions that regulate emotional expression during various cognitive tasks. For example, alexithymic individuals display a disadvantageous pattern of risky decision-making on the Iowa Gambling Task that is suggestive of a failure to learn from feedback, i.e., poor consolidation of emotional experiences.54,55 Such deficits are consistent with neuroanatomic changes in emotion-relevant brain areas identified for alex-ithymic individuals, such as reduced gray matter volume in the amygdala, anterior insula, and anterior cingulate cortex (ACC).56,57 A similar deficit on the Iowa gambling task was found for idiopathic RBD patients,58 although neuroanatomic studies have proved variable with respect to brain changes associated with RBD. Some report anomalies in frontal or limbic areas59–61 consistent with the cognitive findings; others do not.62,63 However, dysfunction in prefrontal regions known to down-regulate amygdala-related emotions—such as medial prefrontal cortex or ACC—may well explain the preponderance of dysphoric dreams and nightmare distress among RBD patients.64 Nonetheless, the possibility that elevated alexithymia in iRBD patients is due to an emotional deficit linked preferentially to prefrontal regulatory regions, though a viable hypothesis, requires additional neuroanatomic study.
Yet another, related, explanation for the present findings is that the emotional symptoms of iRBD patients are due to dysautonomia.65 iRBD patients show autonomic denervation leading to lower heart rate variability (HRV) compared to controls during wakefulness66,67 and during REM sleep.68 Similarly, PD patients with RBD show reduced HRV during wakefulness.69 A cardiac 123I-mIBG scintigraphy study has further demonstrated loss of cardiac sympathetic innervation in RBD.70 An impoverishment of autonomic afferent pathways leading to diminution of affect-relevant information may have an impact on how well patients are able to identify their own feelings. This would account for their low scores on aggressiveness2 and their high scores on the DIF alexithymia subscale but also, by still unidentified mechanisms, for their distressing nightmares. Like iRBD, reduced HRV has also been found for idiopathic nightmares71 and other affective disturbances such as anxiety, depression,72 and worry,73,74 for which nightmares are often also comorbid.75
In sum, that iRBD patients demonstrate elevated levels of alexithymia and nightmare distress and that these symptoms are correlated may be explained by several factors. An affect distress personality style is less likely than the possibility of a dysregulation of emotions, but an underlying dysautonomia is a possibility consistent with much research and requiring additional study. Dysautonomia may reduce afferent sources of feeling and thus explain the specific difficulty in identifying feelings. However, it remains unknown how nightmares are related to the various explanations of high alexithymia in RBD. The dysautonomia explanation raises the novel possibility that degrees of autonomic afferent reduction may also be implicated in nightmares that are not related to iRBD, e.g., posttraumatic or idiopathic nightmares. The increases in dream vividness and nightmares that have been reported to precede the appearance of RBD symptoms by many years suggests that nightmares associated with alexithymia—DIF scores in particular—may be important potential markers for enhancing diagnoses of prodromal RBD and even Parkinson disease. Similar markers have been sought in disturbed olfaction, constipation, autonomic dysfunction, and other symptoms.76
DISCLOSURE STATEMENT
This was not an industry supported study. This study was supported by grants from the Canadian Institutes of Health Research (CIHR; Tore Nielsen, Jacques Montplaisir, Jean-François Gagnon), the Natural Engineering Research Council of Canada (NSERC; Tore Nielsen) and the Fond de Recherche du Québec sur la Santé (FRSQ; Jean-François Gagnon) and by a scholarship to Isabelle Godin from the Canadian Institutes of Health Research. Dr. Montplaisir has received research grants and/or support from Merck, Sanofi-Aventis, GlaxoSmithKline, and Valeant; has been an advisor from Merck, Servier, Valeant, Impax, Jazz, and Sanofi Aventis; and has received honoraria for speaking engagements from Valeant Pharmaceutical, Boehringer-Ingelheim, Sanofi-Aventis, GlaxoSmithKline, and Otsuka Pharmaceutical. The work was conducted at the Center for Advanced Research in Sleep Medicine, Hôpital du Sacré-Coeur de Montréal, Québec, Canada.
ACKNOWLEDGMENT
The authors thank Tyna Paquette for editorial assistance.
REFERENCES
- 1.Mahowald MW, Schenck CH. REM sleep parasomnias. In: Kryger MH, Roth T, Dement C, editors. Principles and practice of sleep medicine. 3rd ed. Philadelphia: WB Saunders; 2000. pp. 724–41. [Google Scholar]
- 2.Fantini ML, Corona A, Clerici S, Ferini-Strambi L. Aggressive dream content without daytime aggressiveness in REM sleep behavior disorder. Neurology. 2005;65:1010–5. doi: 10.1212/01.wnl.0000179346.39655.e0. [DOI] [PubMed] [Google Scholar]
- 3.Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986;9:293–308. doi: 10.1093/sleep/9.2.293. [DOI] [PubMed] [Google Scholar]
- 4.D'Agostino A, Manni R, Limosani I, Terzaghi M, Cavallotti S, Scarone S. Challenging the myth of REM sleep behavior disorder: no evidence of heightened aggressiveness in dreams. Sleep Med. 2012;13:714–9. doi: 10.1016/j.sleep.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Schenck CH, Mahowald MW. REM sleep behavior disorder: clinical, developmental, and neuroscience perspectives 16 years after its formal identification in Sleep. Sleep. 2002;25:120–38. doi: 10.1093/sleep/25.2.120. [DOI] [PubMed] [Google Scholar]
- 6.Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123:331–9. doi: 10.1093/brain/123.2.331. [DOI] [PubMed] [Google Scholar]
- 7.Postuma RB, Gagnon JF, Montplaisir JY. REM sleep behavior disorder: from dreams to neurodegeneration. Neurobiol Dis. 2012;46:553–58. doi: 10.1016/j.nbd.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Iranzo A, Molinuevo J, Santamaria J, et al. Sixty-four percent of patients with idiopathic REM sleep behavior disorder developed a neurological disorder after a mean clinical follow-up of seven years. Sleep. 2008;31:A280. (Abstract Supplement) [Google Scholar]
- 9.Lloyd R, Tippmann-Peikert M, Slocumb N, Kotagal S. Characteristics of REM sleep behavior disorder in childhood. J Clin Sleep Med. 2012;8:127–31. doi: 10.5664/jcsm.1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reijnders JS, Ehrt U, Weber WE, Aarsland D, Leentjens AF. A systematic review of prevalence studies of depression in Parkinson's disease. Mov Disord. 2008;23:183–9. doi: 10.1002/mds.21803. [DOI] [PubMed] [Google Scholar]
- 11.Costa A, Peppe A, Carlesimo GA, Salamone G, Caltagirone C. Prevalence and characteristics of alexithymia in Parkinson's disease. Psychosomatics. 2010;51:22–8. doi: 10.1176/appi.psy.51.1.22. [DOI] [PubMed] [Google Scholar]
- 12.Assogna F, Palmer K, Pontieri FE, et al. Alexithymia is a non-motor symptom of Parkinson disease. Am J Geriatr Psychiatry. 2012;20:133–41. doi: 10.1097/JGP.0b013e318209de07. [DOI] [PubMed] [Google Scholar]
- 13.Poletti M, Frosini D, Pagni C, et al. The association between motor subtypes and alexithymia in de novo Parkinson's disease. J Neurol. 2011;258:1042–5. doi: 10.1007/s00415-010-5878-8. [DOI] [PubMed] [Google Scholar]
- 14.Taylor GJ, Bagby RM, Parker JD. The alexithymia construct: a potential paradigm for psychosomatic medicine. Psychosomatics. 1991;32:153–64. doi: 10.1016/s0033-3182(91)72086-0. [DOI] [PubMed] [Google Scholar]
- 15.Taylor GJ, Bagby RM, Parker JD. New York: Cambridge University Press; 1996. Disorders of affect regulation: alexithymia in medical and psychiatric illness. [Google Scholar]
- 16.Sifneos PE. The prevalence of “alexithymic” characteristics in psychosomatic patients. Psychother Psychosom. 1973;22:255–62. doi: 10.1159/000286529. [DOI] [PubMed] [Google Scholar]
- 17.Apfel RJ, Sifneos PE. Alexithymia: concept and measurement. Psychother Psychosom. 1979;32:180–90. doi: 10.1159/000287386. [DOI] [PubMed] [Google Scholar]
- 18.Lesser IM. A review of the alexithymia concept. Psychosom Med. 1981;43:531–43. doi: 10.1097/00006842-198112000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. J Psychosom Res. 2000;48:99–104. doi: 10.1016/s0022-3999(99)00083-5. [DOI] [PubMed] [Google Scholar]
- 20.Grabe HJ, Rainermann S, Spitzer C, Gäsicke M, Frayberger HJ. The relationship between dimensions of alexithymia and dissociation. Psychother Psychosom. 2000;69:128–31. doi: 10.1159/000012380. [DOI] [PubMed] [Google Scholar]
- 21.Berthoz S, Consoli S, Perez-Diaz F, Jouvent R. Alexithymia and anxiety: compounded relationships? A psychometric study. Eur Psychiatry. 1999;14:372–8. doi: 10.1016/s0924-9338(99)00233-3. [DOI] [PubMed] [Google Scholar]
- 22.Zlotnick C, Zakriski AL, Shea MT, et al. The long-term sequelae of sexual abuse: support for a complex posttraumatic stress disorder. J Trauma Stress. 1996;9:195–205. doi: 10.1007/BF02110655. [DOI] [PubMed] [Google Scholar]
- 23.Grabe HJ, Schwahn C, Barnow S, et al. Alexithymia, hypertension, and subclinical atherosclerosis in the general population. J Psychosom Res. 2010;68:139–47. doi: 10.1016/j.jpsychores.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 24.Sasai K, Tanaka K, Hishimoto A. Alexithymia and its relationships with eating behavior, self esteem, and body esteem in college women. Kobe J Med Sci. 2010;56:231–8. [PubMed] [Google Scholar]
- 25.Kim JH, Lee SJ, Rim HD, Kim HW, Bae GY, Chang SM. The relationship between alexithymia and general symptoms of patients with depressive disorders. Psychiatry Invest. 2008;5:179–85. doi: 10.4306/pi.2008.5.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Honkalampi K, Saarinen P, Hintikka J, Virtanen V, Viinamäki H. Factors associated with alexithymia in patients suffering from depression. Psychother Psychosom. 1999;68:270–5. doi: 10.1159/000012343. [DOI] [PubMed] [Google Scholar]
- 27.Mattila AK, Poutanen O, Koivisto AM, Salokangas RK, Joukamaa M. Alexithymia and life satisfaction in primary healthcare patients. Psychosomatics. 2007;48:523–9. doi: 10.1176/appi.psy.48.6.523. [DOI] [PubMed] [Google Scholar]
- 28.Kauhanen J, Kaplan GA, Cohen RD, Julkunen J, Salonen JT. Alexithymia and risk of death in middle-aged men. J Psychosom Res. 1996;41:541–9. doi: 10.1016/s0022-3999(96)00226-7. [DOI] [PubMed] [Google Scholar]
- 29.Taylor GJ. Alexithymia: concept, measurement, and implications for treatment. Am J Psychiatry. 1984;141:725–32. doi: 10.1176/ajp.141.6.725. [DOI] [PubMed] [Google Scholar]
- 30.Parker JDA, Bauermann TM, Smith CT. Alexithymia and impoverished dream content: evidence from rapid eye movement sleep awakenings. Psychosom Med. 2000;62:486–91. doi: 10.1097/00006842-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Lumley MA, Bazydlo RA. The relationship of alexithymia characteristics to dreaming. J Psychosom Res. 2000;48:561–7. doi: 10.1016/s0022-3999(00)00096-9. [DOI] [PubMed] [Google Scholar]
- 32.De Gennaro L, Ferrara M, Cristiani R, Curcio G, Martiradonna V, Bertini M. Alexithymia and dream recall upon spontaneous morning awakening. Psychosom Med. 2003;65:301–6. doi: 10.1097/01.psy.0000058373.50240.71. [DOI] [PubMed] [Google Scholar]
- 33.Bauermann TM, Parker JD, Taylor GJ. Sleep problems and sleep hygiene in young adults with alexithymia. Pers Individ Dif. 2008;45:318–22. [Google Scholar]
- 34.Nielsen T, Ouellet L, Warnes H, Cartier A, Malo J-L, Montplaisir J. Alexithymia and impoverished dream recall in asthmatic patients: evidence from self-report measures. J Psychosom Res. 1997;42:53–9. doi: 10.1016/s0022-3999(96)00230-9. [DOI] [PubMed] [Google Scholar]
- 35.Nielsen T, Levrier K, Montplaisir J. Dreaming correlates of alexithymia among sleep-disordered patients. Dreaming. 2011;21:16–31. [Google Scholar]
- 36.Hyyppä MT, Lindholm T, Kronholm E, Ville L. Functional insomnia in relation to alexithymic features and cortisol hypersecretion in a community sample. Stress Med. 1990;6:277–83. [Google Scholar]
- 37.American Academy of Sleep Medicine. The international classification of sleep disorders: diagnostic and coding manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 38.Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 39.Bagby RM, Taylor GJ, Parker JD. The twenty-item Toronto Alexithymia Scale—II. Convergent, discriminant, and concurrent validity. J Psychosom Res. 1994;38:33–40. doi: 10.1016/0022-3999(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 40.Parker JD, Taylor GJ, Bagby RM. The 20-Item Toronto Alexithymia Scale. III. Reliability and factorial validity in a community population. J Psychosom Res. 2003;55:269–75. doi: 10.1016/s0022-3999(02)00578-0. [DOI] [PubMed] [Google Scholar]
- 41.Taylor GJ, Bagby RM, Parker JD. The 20-Item Toronto Alexithymia Scale IV. Reliability and factorial validity in different languages and cultures. J Psychosom Res. 2003;55:277–83. doi: 10.1016/s0022-3999(02)00601-3. [DOI] [PubMed] [Google Scholar]
- 42.Beck AT, Steer RA, Brown GK. San Antonio: Psychological Corporation; 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- 43.Rechtschaffen A, Kales A. Los Angeles: Brain Information Service, Brain Research Institute, UCLA; 1968. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. [Google Scholar]
- 44.Lapierre O, Montplaisir J. Polysomnographic features of REM sleep behavior disorder: development of a scoring method. Neurology. 1992;42:1371–74. doi: 10.1212/wnl.42.7.1371. [DOI] [PubMed] [Google Scholar]
- 45.Montplaisir J, Gagnon JF, Fantini ML, et al. Polysomnographic diagnosis of idiopathic REM sleep behavior disorder. Mov Disord. 2012;25:2044–51. doi: 10.1002/mds.23257. [DOI] [PubMed] [Google Scholar]
- 46.Marchesi C, Brusamonti E, Maggini C. Are alexithymia, depression, and anxiety distinct constructs in affective disorders? J Psychosom Res. 2000;49:43–9. doi: 10.1016/s0022-3999(00)00084-2. [DOI] [PubMed] [Google Scholar]
- 47.Lam SP, Zhang J, Tsoh J, et al. REM sleep behavior disorder in psychiatric populations. J Clin Psychiatry. 2010;71:1101–3. doi: 10.4088/JCP.l05877gry. [DOI] [PubMed] [Google Scholar]
- 48.Kronholm E, Partonen T, Salmien J, Mattila A, Joukamaa M. Alexithymia, depression and sleep disturbance symptoms. Psychother Psychosom. 2008;77:63–5. doi: 10.1159/000110063. [DOI] [PubMed] [Google Scholar]
- 49.Haviland MG, Shaw DG, Cummings MA, MacMurray JP. Alexithymia: subscales and relationship to depression. Psychother Psychosom. 1998;50:164–73. doi: 10.1159/000288115. [DOI] [PubMed] [Google Scholar]
- 50.Wise TN, Mann LS, Mitchell JD, Hryvniak M, Hill B. Secondary alexithymia: an empirical validation. Compr Psychiatry. 1990;31:284–88. doi: 10.1016/0010-440x(90)90035-q. [DOI] [PubMed] [Google Scholar]
- 51.Honkalampi K, Hintikka J, Laukkanen E, et al. Alexithymia and depression: a prospective study of patients with major depressive disorder. Psychosomatic. 2001;42:229–34. doi: 10.1176/appi.psy.42.3.229. [DOI] [PubMed] [Google Scholar]
- 52.Nielsen TA, Lara-Carrasco J. Nightmares, dreaming and emotion regulation: a review. In: McNamara P, Barrett D, editors. The new science of dreams. Westport: Praeger Greenwood; 2007. pp. 253–84. [Google Scholar]
- 53.Walker MP. Sleep, memory and emotion. Prog Brain Res. 2010;185:49–68. doi: 10.1016/B978-0-444-53702-7.00004-X. [DOI] [PubMed] [Google Scholar]
- 54.Kano M, Ito M, Fukudo S. Neural substrates of decision making as measured with the Iowa Gambling Task in men with alexithymia. Psychosom Med. 2011;73:588–97. doi: 10.1097/PSY.0b013e318223c7f8. [DOI] [PubMed] [Google Scholar]
- 55.Ferguson E, Bibby PA, Rosamond S, et al. Alexithymia, cumulative feedback and differential response patterns on the Iowa Gambling Task. J Pers. 2009;77:883–902. doi: 10.1111/j.1467-6494.2009.00568.x. [DOI] [PubMed] [Google Scholar]
- 56.Ihme K, Dannlowskib U, Licheva V, et al. Alexithymia is related to differences in gray matter volume: a voxel-based morphometry study. Brain Res. 2013;1491:60–7. doi: 10.1016/j.brainres.2012.10.044. [DOI] [PubMed] [Google Scholar]
- 57.Paradiso S, Vaidya JG, McCormick LM, Jones A, Robinson RG. Aging and alexithymia association with reduced right rostral cingulate volume. Am J Geriatr Psychiatry. 2008;16:760–9. doi: 10.1097/JGP.0b013e31817e73b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Delazer M, Högl B, Zamarian L, et al. Decision making and executive functions in REM sleep behavior disorder. Sleep. 2012;35:667–73. doi: 10.5665/sleep.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mazza S, Soucy JP, Gravel P, et al. Assessing whole brain perfusion changes in REM sleep behaviour disorder. Neurology. 2006;67:1618–22. doi: 10.1212/01.wnl.0000242879.39415.49. [DOI] [PubMed] [Google Scholar]
- 60.Gagnon JF, Fantini ML, Bédard MA, et al. Association between waking EEG slowing and REM sleep behavior disorder in PD without dementia. Neurology. 2004;62:401–6. doi: 10.1212/01.wnl.0000106460.34682.e9. [DOI] [PubMed] [Google Scholar]
- 61.Lin FC, Liu CK, Hsu CY. Rapid-eye-movement sleep behavior disorder secondary to acute aseptic limbic encephalitis. J Neurol. 2009;256:1174–6. doi: 10.1007/s00415-009-5067-9. [DOI] [PubMed] [Google Scholar]
- 62.Hanyu H, Inoue Y, Sakurai H, et al. Voxel-based magnetic resonance imaging study of structural brain changes in patients with idiopathic REM sleep behavior disorder. Parkinsonism Relat Disord. 2012;18:136–9. doi: 10.1016/j.parkreldis.2011.08.023. [DOI] [PubMed] [Google Scholar]
- 63.Scherfler C, Frauscher B, Schocke M, et al. for the SINBAR (Sleep Innsbruck Barcelona) Group. White and gray matter abnormalities in idiopathic rapid eye movement sleep behavior disorder: a diffusion-tensor imaging and voxel-based morphometry study. Ann Neurol. 2011;69:400–7. doi: 10.1002/ana.22245. [DOI] [PubMed] [Google Scholar]
- 64.Nielsen TA, Levin R. Nightmares: a new neurocognitive model. Sleep Med Rev. 2007;11:295–310. doi: 10.1016/j.smrv.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 65.Siderowf A, Jennings D. Cardiac denervation in rapid eye movement sleep behavior disorder and Parkinson's disease: getting to the heart of the matter. Mov Disord. 2010;25:2269–71. doi: 10.1002/mds.23404. [DOI] [PubMed] [Google Scholar]
- 66.Valappil RA, Black JE, Broderick MJ, et al. Exploring the electrocardiogram as a potential tool to screen for premotor Parkinson's disease. Mov Disord. 2010;25:2296–303. doi: 10.1002/mds.23348. [DOI] [PubMed] [Google Scholar]
- 67.Postuma RB, Lanfranchi PA, Blais H, Gagnon JF, Montplaisir JY. Cardiac autonomic dysfunction in idiopathic REM sleep behavior disorder. Mov Disord. 2010;25:2304–10. doi: 10.1002/mds.23347. [DOI] [PubMed] [Google Scholar]
- 68.Lanfranchi PA, Fradette L, Gagnon JF, Colombo R, Montplaisir J. Cardiac autonomic regulation during sleep in idiopathic REM sleep behavior disorder. Sleep. 2007;30:1019–25. doi: 10.1093/sleep/30.8.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Postuma RB, Montplaisir JY, Lanfranchi P, et al. Cardiac autonomic denervation in Parkinson's disease is linked to REM sleep behavior disorder. Mov Disord. 2010;26:1529–33. doi: 10.1002/mds.23677. [DOI] [PubMed] [Google Scholar]
- 70.Miyamoto T, Miyamoto M, Inoue Y, Usui Y, Suzuki K, Hirata K. Reduced cardiac 123I-MIBG scintigraphy in idiopathic REM sleep behavior disorder. Neurology. 2006;67:2236–8. doi: 10.1212/01.wnl.0000249313.25627.2e. [DOI] [PubMed] [Google Scholar]
- 71.Nielsen TA, Paquette T, Solomonova E, Lara-Carrasco J, Colombo R, Lanfranchi P. Changes in cardiac variability after REM sleep deprivation in recurrent nightmares. Sleep. 2010;33:113–22. doi: 10.1093/sleep/33.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shinba T, Kariya N, Matsui Y, Ozawa N, Matsuda Y, Yamamoto K. Decrease in heart rate variability response to task is related to anxiety and depressiveness in normal subjects. Psychiatry Clin Neurosci. 2008;62:603–9. doi: 10.1111/j.1440-1819.2008.01855.x. [DOI] [PubMed] [Google Scholar]
- 73.Brosschot JF, Van Dijk E, Thayer JF. Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. Int J Psychophysiol. 2007;63:39–47. doi: 10.1016/j.ijpsycho.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 74.Cohen H, Benjamin J. Power spectrum analysis and cardiovascular morbidity in anxiety disorders. Auton Neurosci. 2006;128:1–8. doi: 10.1016/j.autneu.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 75.Levin R, Nielsen T. Disturbed dreaming, posttraumatic stress disorder, and affect distress: a review and neurocognitive model. Psychol Bull. 2007;133:482–528. doi: 10.1037/0033-2909.133.3.482. [DOI] [PubMed] [Google Scholar]
- 76.Postuma RB, Gagnon JF, Montplaisir JY. REM sleep behavior disorder: From dreams to neurodegeneration. Neurobiol Dis. 2012;46:553–8. doi: 10.1016/j.nbd.2011.10.003. [DOI] [PubMed] [Google Scholar]