Abstract
Background:
Studies have shown an association between parental distress and caretaking of children with developmental cognitive delays. There is little data in developing countries, such as Pakistan, concerning the impact of raising children with intellectual disability upon the quality of parent functioning and risk for psychopathology.
Objective:
To assess the level of psychopathology i.e. anxiety, depression and both anxiety and depression together among parents of children with intellectual disability (ID).
Methods:
This was a cross-sectional study conducted at a tertiary care hospital in Pakistan. The study was approved by the Institutional Research Committee. Participants were 198 parents (99 fathers/99 mothers) of 100 children with the diagnosis of ID. Informed consents were obtained. The parents were assessed for anxiety and depression using DSM IV criteria.
Results:
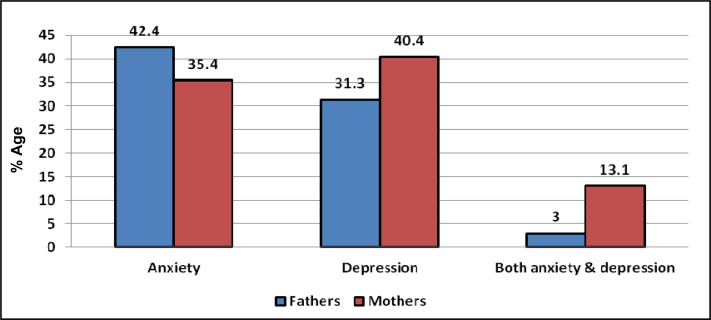
Significantly high proportion of mothers (89%) had anxiety, depression, or both anxiety and depression together as compared to fathers (77%) (p-value <0.05). Among mothers, 35% met criteria for anxiety, 40% for depression and 13% for both anxiety and depression. Among fathers 42% had anxiety, 31% depression and 3% both anxiety and depression. There was a significant association between gender of parent and individual psychiatric diagnosis of anxiety, depression and anxiety and depression together (p-value <0.05). A significant association was also found between mother’s anxiety, depression or both and degree of ID of their children (p-value <0.05).
Conclusions:
1) Significantly high proportion of parents of children with ID has psychiatric diagnosis of anxiety, depression or both; 2) the psychiatric diagnosis of anxiety, depression and anxiety and depression together is associated with gender of parent; and, 3) the diagnosis of anxiety, depression or both in mothers was associated with severity of ID in their children.
Keywords: anxiety, depression, intellectual disability, parents
Résumé
Contexte:
Des études ont montré une association entre la détresse parentale et la garde d’enfants souffrant de retards de développement cognitif. Dans les pays en développement, comme le Pakistan, il existe peu de données au sujet des répercussions d’élever des enfants souffrant de déficience intellectuelle sur la qualité du fonctionnement des parents et le risque de psychopathologie.
Objectif:
Évaluer le niveau de psychopathologie, c.-à-d., l’anxiété, la dépression et l’anxiété et la dépression à la fois chez les parents d’enfants souffrant de déficience intellectuelle (DI).
Méthodes:
Cette étude intersectorielle a été menée à un hôpital de soins tertiaires du Pakistan. Elle a été approuvée par le comité de recherche institutionnelle. Les participants étaient 198 parents (99 pères/99 mères) de 100 enfants ayant reçu un diagnostic de DI. Des consentements éclairés ont été obtenus. Les critères de l’anxiété et de la dépression du DSM-IV ont servi à évaluer ces troubles chez les parents.
Résultats:
Une proportion significativement élevée des mères (89%) souffrait d’anxiété, de dépression ou d’anxiété et de dépression à la fois comparé aux pères (77%) (valeur p < 0,05). Chez les mères, 35 % satisfaisaient aux critères de l’anxiété, 40%, à ceux de la dépression et 13% à ceux de l’anxiété et de la dépression à la fois. Chez les pères, 42% souffraient d’anxiété, 31%, de dépression et 3% d’anxiété et de dépression à la fois. Il y avait une association significative entre le sexe des parents et le diagnostic psychiatrique individuel d’anxiété, de dépression, et d’anxiété et de dépression à la fois (valeur p < 0,05). Une autre association significative a été observée entre l’anxiété, la dépression ou les deux chez la mère et le degré de DI de leurs enfants (valeur p < 0,05).
Conclusions:
1) Une proportion significativement élevée des parents d’enfants souffrant de DI a un diagnostic psychiatrique d’anxiété, de dépression, ou des deux à la fois; 2) le diagnostic psychiatrique d’anxiété, de dépression, ou des deux à la fois est associé au sexe du parent; et 3) le diagnostic d’anxiété, de dépression, ou des deux à la fois chez les mères était associé à la gravité de la DI de leurs enfants.
Keywords: anxiété, dépression, déficience intellectuelle, parents
Introduction
Intellectual Disability (ID), also historically known as mental retardation, is characterized by significant limitations in intellectual functioning, also called intelligence, and in adaptive behavior including conceptual, social and practical skills. This disability originates before the age of 18 (Schalock, Luckasson, & Shogren, 2007). ID can be classified into four classes depending on Intelligence Quotient (IQ) i.e. Mild (IQ 50–70), Moderate (IQ 35-<50), Severe (IQ 20-<35) and Profound (IQ <20). Studies have shown an association between parental distress and caretaking of children with developmental cognitive delays (Cramm & Nieboer, 2011; Khamis, 2007; Saloviita, Itaalinna, & Leinonen, 2003). The skills acquired through parental intervention may be limited dependent upon the level of cognitive delay. Therefore, various demands persist throughout childhood and later into adult years, leading to ongoing parental stress. Additionally, a large number of these children have behavioral issues, which can lead to higher levels of parental stress (Floyd & Gallagher, 1997; Greenberg, Seltzer, Krauss, & Kim, 1997). Parents reported more psychiatric symptomatology when the child showed a high level of dysfunction (Khamis, 2007). Pakistan has one of the highest reported rates of childhood intellectual disabilities in the world, 65/1000 for mild ID (Mirza, Tareen, Davidson, & Rahman, 2009). Studies performed in developing countries have shown reasonably consistently high rates of depressive and anxiety disorders; where 10–44% of people suffer from depression and anxiety (World Health Organization, 2001). High rates of both depression and anxiety disorders among women in Pakistan have been reported (Mumford, Nazir, Jilani, & Baig, 1996; Husain, Creed, & Tomenson, 2000). A study by Mirza and Jenkins reported prevalence rates of 34% for depression and anxiety in Pakistan (Mirza & Jenkins, 2004). Ahmad et al. found in another rural sample in Pakistan, 72% of women and 44% of men reported anxiety and depression (Ahmad, Saeed, & Mubbashar, 2001).
There is little data in developing countries, such as Pakistan, concerning the impact of raising children with ID, upon the quality of parent functioning and their risk of psychopathology. Parental coping styles and presence of social support in relationship with developmental disabilities can impact the level of parental distress (Dabrowska & Pistula, 2010). This risk can be considered within four broad domains: physical health, psychological health, social relationships, and environment, while appreciating that parents function both independently and as a unit throughout the course of a day and across the lifetime of a child with ID. There was found to be high traits of anxiety in parents who have a child with ID (Keskin, 2010). Families with children having ID are in even greater need of help than those who have children with severe chronic illness/physical handicap (Von Gontard et al., 2002). The life-span needs of children with ID and their families, and the impact of cultural and socioeconomic diversity, are not sufficiently understood (Hodapp, 2007). Treatment progress may need to address parental stress, which in turn will help optimize treatment outcome for the child and the family (Rao & Beidel, 2009). In a 2010 study regarding children with autism and their parents, the Brief COPE tool was used, and it was found that use of cognitive reframing produced improved parental well-being in regards to depression and anger (Benson, 2010). More studies are needed to evaluate the impact of rearing children with ID, related behavioral concerns on parental functioning, and the risk for psychopathology.
Methodology
This was a cross-sectional study conducted at a tertiary care hospital in Pakistan after approval from the Institutional Research Committee. Participants were 198 parents (99 fathers/99 mothers) of 100 children, aged 2–18 years with the diagnosis of ID. Parents having history of chronic life-threatening illnesses such as malignancies, chronic liver failure and chronic renal failure were excluded from the study. After getting written informed consent, the parents were recruited from three health centers in Pakistan: Department of Psychiatry and Behavioral Sciences, District Headquarters Hospital, Punjab Medical College, Faisalabad; Almasoom Center in Faisalabad; and, Amin Maktab Special Institute for Children in Lahore. All the parents approached willingly gave consent to participate in the study. IQ of all the children in three centers was assessed using Slosson Intelligence Test. Efforts were made to obtain a broad cross-section of the population based on factors such as age, socioeconomic status, demographic origin and educational level. The parents were assessed for anxiety and depression using DSM-IV criteria. Raters were psychologists from the Department of Psychiatry and Behavioral Sciences, District Head Quarters Hospital, Punjab Medical College, Faisalabad. Psychologists were trained in the collection of bio-data, and administration of DSM-IV diagnostic criteria for depression and anxiety using specially designed forms. The data forms were also translated into Urdu language accompanied by a Punjabi language glossary. Psychiatrists worked in tandem with the psychologists.
The data was entered and analyzed using IBM SPSS Statistics 20. Descriptive statistics of socio-demographic information were determined. For the purpose of analysis, parents were grouped into Mothers and Fathers. Each of these two groups was further sub-divided on the basis of degree of ID of their children and psychiatric diagnosis of anxiety, depression or both. Pearson Chi Square test and Fisher’s Exact Test were used to evaluate associations between various qualitative variables of interest. For all purposes, a p-value of <0.05 was considered statistically significant.
Results
In this study, mean age of mothers was 37.42 (S.D 8.8) years and of fathers was 42.9 (S.D 8.8) years. Twenty-one percent of mothers and 11% of fathers were illiterate. The mean age of the children was 10.5 (S.D 5.0) years (range: 2–18 years), with 30% females and 70% males. Twenty-five percent children had mild ID, 42% moderate ID, 20% severe ID and 13% had profound ID. Comorbid diagnosis included: cerebral palsy 22%; epilepsy 34%; and, autistic disorder 11%. Eighty-two percent of the children had ID since birth. Seventy-nine percent of the children had various behavioral difficulties, including aggression.
A significantly high proportion of mothers (89%) had anxiety, depression or both anxiety and depression together as compared to fathers (77%) (p-value=0.024). Among mothers, 35% met criteria for anxiety, 40% for depression and 13% for both anxiety and depression. Among fathers 42% had anxiety, 31% depression and 3% both anxiety and depression.
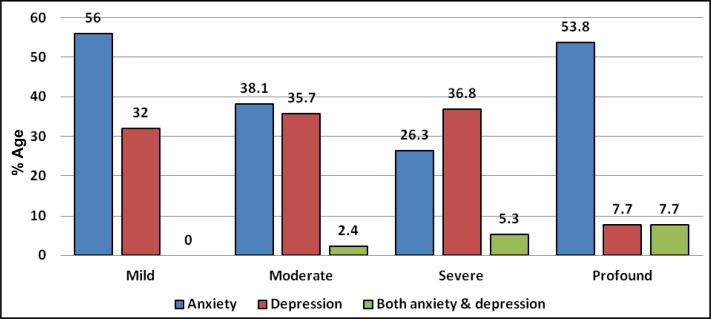
A significant association was found between mother’s anxiety, depression or both and degree of ID of their children (p-value=0.043). The diagnosis of depression was highest among mothers of children with moderate ID (57%), whereas anxiety was highest among mothers of children with profound ID (50%), and both anxiety and depression together were highest among mothers of children with profound ID (25%). There was no association between father’s anxiety, depression or both and degree of ID in their children.
Discussion
A family who has a child with an ID, experiences many challenges such as repeated physical and emotional crises, interactive family issues, ruined schedules, and additional expenses, which can create financial burden and emotional distress for a family (Gohel, Mukherjee, & Choudhary, 2011; Karmanshahi et al., 2008.). Having a child with ID often requires a reorientation and reevaluation of family goals, responsibilities and relationships. A significantly high proportion of parents of children with ID have psychiatric diagnosis of anxiety, depression or both, needing mental health services and support. Nearly 50% of the parents were severely anxious and about two-thirds were clinically depressed (Bitsika & Sharpley, 2004). In a study done in Turkey, Firat et al. reported high rates of depression in mothers of children with autism (72.5%) and in mothers of children with mental retardation (44.7%) (Firat, Diler, Avci, & Seydaoglu, 2002).
The high level of stress or mental health problems experienced by parents of children with ID could be related to subjective factors such as feeling social isolation and life dissatisfaction (Majumdar, Da Silva, & Fernandes, 2005). Parents of these children may struggle with a multitude of emotions interchangeably over years, and often have feelings of guilt that somehow they caused the child to be disabled, for logical or illogical reasons (Upadhyaya & Havalappanavar, 2008). Other factors related to parenting a child with an ID that may negatively impact parent mental health may include disappointment that their child will not reach the career ideals they had envisioned or feelings of embarrassment, shame, and isolation. In this study, higher risk for psychiatric diagnosis of anxiety, depression and anxiety and depression together was associated with the gender of the parent. This can also be explained in cultural context since in Pakistan mothers are the main primary care takers of their children. Within that context, in two parent families, stress and care demands are expected to be strongest for mothers as opposed to fathers because of the greater responsibility; mothers tend to have for direct childcare (Russell, 1986). Accordingly, mothers appear to be more vulnerable to the stress associated with child’s behavioral problems (Floyd & Zmich, 1991). Since mothers are more under pressure to balance child care needs and household chores, physical support from the family is reported as a relief (Peshawaria et al., 1998). Mothers, who are housewives without additional help, can feel restricted in pursuing their social and leisure activities, and experience more stress (Majumdar et al., 2005; Ergun & Ertem, 2012). Fathers have lower rates of anxiety and depression as compared to mothers, but higher rates than males in the general population (Mumford, Saeed, Ahmad, Latif, & Mubbashar, 1997). As typically fathers are the sole bread winners for their immediate and extended families, in Pakistani culture, having a child with ID can impose further financial pressures on fathers. Because of social stigma towards children with ID, parents, especially fathers, can feel shame and embarrassment in taking their child to social and family gatherings. This can lead to social isolation for the whole family, contributing to further stress.
The diagnosis of anxiety, depression or both among mothers was associated with severity of ID in their children, which has been shown in previous studies (Kumar & Akhtar, 2001). In our study, presence of high rates of behavioral issues and comorbid illnesses with ID most likely have contributed to high rates of parental anxiety and depression. Previous studies have reported parental stress and health outcome being related to child characteristics such as the severity of the core disability, main diagnosis, the age of the child, and the extent of coexisting behavioral issues (Freeman, Perry, & Factor, 1991; Hastings, 2002). In a study done by Gupta and Kaur in India, both mothers and fathers of children with ID reported high rates of mental stress as compared to physical stress, especially women (Gupta & Kaur, 2010).
Conclusions
There was a high rate of anxiety and depression among parents of children with ID in this study. Rates of anxiety and depression were even higher among mothers as compared to fathers. Mental health providers need to be aware of these issues, so appropriate mental health screening can be utilized among the care givers of children with ID. The services provided for children with ID need to include appropriate systems interventions and support for their caregivers.
Limitations
Limitations of the study were small sample size and lack of comparison group of parents of healthy children. Future studies are needed which should include multiple sites across the country, encompassing both urban and rural settings with a larger sample size and a control group.
Figure 1.
Individual psychiatric diagnosis in fathers and mothers of children with ID
Figure 2.
Individual psychiatric diagnosis in mothers of children among groups of children with various degrees of ID
Figure 3.
Individual psychiatric diagnosis in fathers of children among groups of children with various degrees of ID
Table 1.
Psychiatric diagnosis in fathers and mothers of children with various degrees of ID
| Degree of ID | Diagnosis | Fathers n (%) | Mothers n (%) |
|---|---|---|---|
| Mild | Anxiety | 14 (56) | 12 (48) |
| Fathers N=25 | Depression | 8 (32) | 5 (20) |
| Mothers N=25 | Both anxiety & depression | 0 (0) | 4 (16) |
| No psychiatric diagnosis | 3 (12) | 4 (16) | |
| Moderate | Anxiety | 16 (38.1) | 11 (26.2) |
| Fathers N=42 | Depression | 15 (35.7) | 24 (57.1) |
| Mothers N=42 | Both anxiety & depression | 1 (2.4) | 4 (9.5) |
| No psychiatric diagnosis | 10 (23.8) | 3 (7.1) | |
| Severe | Anxiety | 5 (26.3) | 6 (30) |
| Fathers N=19 | Depression | 7 (36.8) | 9 (45) |
| Mothers N=20 | Both anxiety & depression | 1 (5.3) | 2 (10) |
| No psychiatric diagnosis | 6 (31.6) | 3 (15) | |
| Profound | Anxiety | 7 (53.8) | 6 (50) |
| Fathers N=13 | Depression | 1 (7.7) | 2 (16.7) |
| Mothers N=12 | Both anxiety & depression | 1 (7.7) | 3 (25) |
| No psychiatric diagnosis | 4 (30.8) | 1 (8.3) |
Acknowledgements/Conflicts of Interest
Results of this study were presented as a poster at the American Psychiatric Association’s 165th Annual Meeting held at Philadelphia, U.S.A in May, 2012. The authors have no financial relationships to disclose.
References
- Ahmad I, Saeed K, Mubbashar MH. Minor psychiatric morbidity and socio-economic factors. Medical Forum Monthly. 2001;12:5–8. [Google Scholar]
- Benson PR. Coping, distress, and well-being in mothers of children with autism. Research in Autism Spectrum Disorders. 2010;4(2):217–228. [Google Scholar]
- Bitsika V, Sharpley C. Stress, anxiety and depression among parents of children with autism spectrum disorder. Australian Journal of Guidance and Counselling. 2004;14(2):151–161. [Google Scholar]
- Cramm J, Nieboer A. Psychological well-being of caregivers of children with intellectual disabilities: Using parental stress as a mediating factor. Journal of Intellectual Disabilities. 2011;15(2):101–113. doi: 10.1177/1744629511410922. [DOI] [PubMed] [Google Scholar]
- Dabrowska A, Pisula E. Parenting stress and coping styles in mothers and fathers of pre-school children with autism and Down syndrome. Journal of Intellectual Disability Research. 2010;54(3):266–280. doi: 10.1111/j.1365-2788.2010.01258.x. [DOI] [PubMed] [Google Scholar]
- Ergun S, Ertem G. Difficulties of mothers living with mentally disabled children. Journal of Pakistan Medical Association. 2012;62(8):776–780. [PubMed] [Google Scholar]
- Firat S, Diler R, Avci A, Seydaoglu G. Comparison of psychopathology in the mothers of autistic and mentally retarded children. Journal of Korean Medical Science. 2002;17:679–685. doi: 10.3346/jkms.2002.17.5.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd FJ, Gallagher EM. Parental stress, care demands, and use of support services for school-age children with disabilities and behavior problems. Family Relations. 1997;46:359–371. [Google Scholar]
- Floyd FJ, Zmich DE. Marriage and the parenting partnership: Perceptions and interactions of parents with mentally retarded and typically developing children. Child Development. 1991;62(6):1434–1448. [PubMed] [Google Scholar]
- Freeman NL, Perry A, Factor DC. Child behaviours as stressors: Replicating and extending the use of the CARS as a measure of stress: A research note. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1991;32(6):1025–1030. doi: 10.1111/j.1469-7610.1991.tb01927.x. [DOI] [PubMed] [Google Scholar]
- Gohel M, Mukherjee S, Choudhary SK. Psychosocial impact on the parents of mentally retarded children in Anand District. Healthline. 2011;2(2):62. [Google Scholar]
- Greenberg JS, Seltzer MM, Krauss MW, Kim H. The differential effects of social support on the psychological well-being of aging mothers of adults with mental illness or mental retardation. Family Relations. 1997;46(4):383–394. [Google Scholar]
- Gupta RK, Kaur H. Stress among parents of children with intellectual disability. Asia Pacific Disability Rehabilitation Journal. 2010;21(2):118–126. [Google Scholar]
- Hastings RP. Parental stress and behaviour problems of children with developmental disability. Journal of Intellectual Developmental Disability. 2002;27(3):149–160. [Google Scholar]
- Hodapp RM. Families of persons with Down syndrome: New perspectives, findings, and research and service needs. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13(3):279–287. doi: 10.1002/mrdd.20160. [DOI] [PubMed] [Google Scholar]
- Husain N, Creed F, Tomenson B. Depression and social stress in Pakistan. Psychological Medicine. 2000;30(2):395–402. doi: 10.1017/s0033291700001707. [DOI] [PubMed] [Google Scholar]
- Karmanshahi SM, Vanaki Z, Ahmadi F, Kazemnezad A, Mordoeh E, Azadfalah P. Iranian mothers perception of their lives with children with mental retardation: A preliminary phenomenological investigation. Journal of Developmental and Physical Disabilities. 2008;20(4):317–326. [Google Scholar]
- Keskin G. The evaluation of anxiety, parental attitude and coping strategy in parents of children with mental retardation. Anatolian Journal of Psychiatry. 2010;11(1):30–37. [Google Scholar]
- Khamis V. Psychological distress among parents of children with mental retardation in the United Arab Emirates. Social Science & Medicine. 2007;64(4):850–857. doi: 10.1016/j.socscimed.2006.10.022. [DOI] [PubMed] [Google Scholar]
- Kumar I, Akhtar S. Rate of anxiety in mothers of mentally retarded children. Indian Journal of Psychiatry. 2001;43(2):27. [Google Scholar]
- Majumdar M, Da Silva PY, Fernandes J. Stress and anxiety in parents of mentally retarded children. Indian Journal of Psychiatry. 2005;47(3):144–147. doi: 10.4103/0019-5545.55937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: A systematic review. British Medical Journal. 2004;328(7443):794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirza I, Tareen A, Davidson LL, Rahman A. Community management of intellectual disabilities in Pakistan: A mixed methods study. Journal of Intellectual Disability Research. 2009;53(6):559–570. doi: 10.1111/j.1365-2788.2009.01176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumford DB, Nazir M, Jilani FU, Baig IY. Stress and psychiatric disorder in the Hindu Kush: A community survey of mountain villages in Chitral, Pakistan. The British Journal of Psychiatry: The Journal of Mental Science. 1996;168(3):299–307. doi: 10.1192/bjp.168.3.299. [DOI] [PubMed] [Google Scholar]
- Mumford DB, Saeed K, Ahmad I, Latif S, Mubbashar MH. Stress and psychiatric disorder in rural Punjab. A community survey. The British Journal of Psychiatry. 1997;170:473–478. doi: 10.1192/bjp.170.5.473. [DOI] [PubMed] [Google Scholar]
- Peshawaria R, Menon DK, Ganguly R, Roy S, Rajam Pillay PRS, Gupta S. A study of facilitators and inhibitors that affect coping in parents of children with mental retardation in India. Asia Pacific Disability Rehabilitation Journal. 1998;9(1):118–126. [Google Scholar]
- Rao PA, Beidel DC. The impact of children with high-functioning autism on parental stress, sibling adjustment, and family functioning. Behavior Modification. 2009;33(4):437–451. doi: 10.1177/0145445509336427. [DOI] [PubMed] [Google Scholar]
- Russell G. Primary caretaking and role-sharing fathers. In: Lamb ME, editor. The father’s role: Applied perspectives. New York, NY: Wiley; 1986. pp. 29–57. [Google Scholar]
- Saloviita T, Itaalinna M, Leinonen E. Explaining the parental stress of fathers and mothers caring for a child with intellectual disability: A double ABCX model. Journal of Intellectual Disability Research. 2003;47(4–5):300–312. doi: 10.1046/j.1365-2788.2003.00492.x. [DOI] [PubMed] [Google Scholar]
- Schalock R, Luckasson R, Shogren K. The renaming of mental retardation: Understanding the change to the term intellectual disability. Intellectual and Developmental Disabilities. 2007;45(2):116–124. doi: 10.1352/1934-9556(2007)45[116:TROMRU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Upadhyaya GR, Havalappanavar NB. Stress in parents of the mentally challenged. Journal of the Indian Academy of Applied Psychiatry. 2008;34(special issue):53–59. [Google Scholar]
- Von Gontard A, Backes M, Laufersweiler-Plass C, Wendland C, Lehmkuhl G, Zerres K, Rudnik-Schöneborn S. Psychopathology and familial stress - comparison of boys with Fragile X syndrome and spinal muscular atrophy. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2002;43(7):949–957. doi: 10.1111/1469-7610.00098. [DOI] [PubMed] [Google Scholar]
- World Health Organization The World Health Report: 2001: Mental health: New understanding, new hope. 2001. [Online] [cited 2001] Available from: http://www.who.int/whr/2001/en/whr01_en.pdf.