Abstract
Objective:
To investigate how attitudes towards psychostimulant medication influence the adherence to psychostimulant treatment in children with Attention-Deficit/Hyperactivity Disorder (ADHD).
Method:
Thirty-three children with ADHD were prospectively recruited to take part in this study. The children and their parents filled questionnaires at both baseline and at a three-month follow-up to assess the severity of ADHD symptoms in the child and attitudes towards psychostimulant medication. Adherence to medication was assessed through standardized interviews of parents.
Results:
Parental perceived psychosocial benefits of psychostimulant medication at the three-month follow-up were found to be positive predictors of adherence to medication. Parental perceived psychosocial benefits of medication at the three-month follow-up was in turn predicted by parental medication acceptability at three months and child’s perceived psychosocial benefits of medication at three-months.
Conclusion:
Improving parents’ awareness of psychosocial benefits of psychostimulant medication may increase adherence to psychostimulant medication in children with ADHD. Age of the child and severity of symptoms did not significantly affect medication adherence.
Keywords: Attention-Deficit/Hyperactivity Disorder (ADHD), medication adherence, psychostimulants, attitudes
Résumé
Objectif:
Rechercher comment les attitudes à l’égard des psychostimulants influencent l’observance du traitement par psychostimulants chez les enfants souffrant du trouble de déficit de l’attention avec hyperactivité (TDAH).
Méthode:
Trente-trois enfants souffrant du TDAH ont été recrutés prospectivement pour prendre part à cette étude. Les enfants et leurs parents ont répondu à des questionnaires au départ et au suivi de trois mois afin d’évaluer la gravité des symptômes du TDAH chez l’enfant et les attitudes à l’égard des psychostimulants. L’observance des médicaments a été évaluée par des entrevues normalisées avec les parents.
Résultats:
La perception des parents des avantages psychosociaux des psychostimulants au suivi de trois mois s’est révélée être un prédicteur positif de l’observance des médicaments. La perception des parents des avantages psychosociaux des médicaments au suivi de trois mois a été prédite à son tour par l’acceptation parentale des médicaments à trois mois et par la perception de l’enfant des avantages psychosociaux des médicaments à trois mois.
Conclusion:
Sensibiliser davantage les parents aux avantages psychosociaux des psychostimulants peut améliorer l’observance des psychostimulants chez les enfants souffrant du TDAH. L’âge de l’enfant et la gravité des symptômes n’influaient pas significativement sur l’observance des médicaments.
Keywords: trouble de déficit de l’attention avec hyperactivité (TDAH), observance des médicaments, psychostimulants, attitudes
Introduction
Affecting between 8 and 12% of children worldwide, Attention-Deficit/Hyperactivity Disorder (ADHD) is the most commonly diagnosed mental disorder in children (Faraone, Sergeant, Gillberg, & Biederman, 2003). ADHD is a chronic neurobehavioural disorder associated with symptoms of inattention, impulsiveness, and hyper-activity which can persist into adulthood if left untreated. The symptoms of ADHD often lead to school dysfunction, difficulties with peers, and familial problems. Comorbid disorders, particularly oppositional defiant disorder (ODD), anxiety disorders, and learning disabilities, are common in ADHD (Biederman & Faraone, 2005).
The symptoms of ADHD are usually treated with psycho-stimulant medication and a variety of psychological/educational interventions, either individually or in combination. The effectiveness of psychostimulants is well demonstrated with 70 to 80% of children responding well (Brown et al., 2005; MTA Cooperative Group, 1999). Charach et al. demonstrated that children symptomatic for ADHD derived benefits from medication in terms of reduction of symptoms even five years after the initiation of treatment (Charach, Ickowicz, & Schachar, 2004). Powers et al. have furthermore shown that children with ADHD who are treated with psychostimulants perform better at school than those who are not and that this advantage is maintained at least until high school (Powers, Marks, Miller, Newcorn, & Halperin, 2008).
Nonetheless, adherence to medication remains relatively low. Adherence to psychostimulant, as reported in the literature, effectively ranges between 52% and 86.1% for a one-year period, gradually decreases to 52–65% for a three-year period and reaches 61% for a five-year period (Corkum, Rimer, & Schachar, 1999; Faraone, Biederman, & Zimmerman, 2007; Gau et al., 2008; Thiruchelvam, Charach, & Schachar, 2001). Studies have shown that the main predictors of low adherence to psychostimulant medication are increasing age, low starting dose of psychostimulants, minority status, fewer baseline ADHD symptoms, previous family history of ADHD, and paternal education of college or higher (Gau et al., 2008; Thiruchelvam et al., 2001).
It is nonetheless difficult for clinicians who wish to increase the adherence to medication of their patients to make use of this information because these factors are essentially immutable. Attitude towards psychostimulants is a factor that is currently under-investigated for its influence on adherence to psychostimulant medication in children with ADHD. Furthermore, contrarily to the other factors mentioned above, attitude towards psychostimulants is a factor that could potentially be influenced by clinicians.
Pharmacological treatment consistently rates as less acceptable than non-pharmacological alternatives in populations of parents of children with ADHD (Johnston, Hommersen, & Seipp, 2008; Krain, Kendall, & Power, 2005). Bennet et al., using the ADHD Knowledge and Opinion Scale – Revised (AKOS-R) to assess parental “medication acceptability,” did not find any correlation between this factor at intake and adherence to treatment four months later (Bennett, Power, Rostain, & Carr, 1996). In their study of 81 children with ADHD and their parents, Corkum, Rimer and Schachar found a positive correlation between a higher medication acceptability and enrolment in medication treatment. Adherence to pharmacological treatment was not found to be predicted by parental opinions of the treatment. The children participating in this study were however being evaluated for a double-blind medication treatment study, it is thus possible that the opinions of their parents regarding medication may differ from a patient population following standard community-based practice. The opinion of the children was furthermore not investigated in these studies and “medication acceptability” was considered as a whole rather than divided into its components, for instance “perceived psychosocial benefits of medication” (Corkum et al., 1999).
Some studies, on the other hand, suggest that not only does medication acceptability correlate to higher medication enrolment, but it could lead to a higher adherence with psychostimulant medication in the long-term (Ibrahim, 2002; Krain et al., 2005). These two studies by Krain et al. and Ibrahim had samples of, respectively, 55 and 51 children. The former study used the Treatment Acceptability Questionnaire (TAQ) to assess parental attitudes towards medication, while the latter used the Compliance with Treatment Opinion and Attitudes Scale (CTOS). Since these two questionnaires were either adapted from an existing questionnaire or simply created for this particular study, it is hard to compare them with other studies that used different questionnaires.
Some studies prefer to look at “perceived benefits of medication” rather than medication acceptability. It has been suggested that parental perceived medication benefits are positively related to higher concerns regarding illness, (Mc-Neal, Roberts, & Barone, 2000) but negatively related to parental stigma toward medication and parental inconsistency in giving medication to their child (Harpur, Thompson, Daley, Abikoff, & Sonuga-Barke, 2008). Harpur et al. also suggest that parental “perceived psychosocial costs of medication” are positively related to their stigma toward medication and their resistance to give medication to their child. The few studies which investigated children attitudes toward medication agree that parents consistently see more benefits in ADHD medication than their children (Harpur et al., 2008; McNeal et al., 2000). Finally, a study by Corkum et al. reported no change in attitude toward medication between initiation of treatment and a 12-month follow-up (Corkum et al., 1999).
The analysis of these studies reveals that the precise role of attitudes towards psychostimulant medication in influencing adherence to medication treatment in children with ADHD remains for the most part unclear. This is particularly evident when it comes to the role of the child’s attitudes towards psychostimulants. The aim of this study is therefore to clarify the influence of attitudes towards psychostimulant medication, of both parents and child, on adherence to medication and compare it with more widely-acknowledged predictive factors of adherence, such as severity of ADHD symptoms at baseline and age of the child. We believe that this is necessary as this could have therapeutic applications for clinicians who wish to improve the adherence to medication of their patients with ADHD.
Methods
Population
Thirty-three children with ADHD from the Douglas Mental Health University Institute ADHD Clinic and their parents were prospectively followed-up three months after initiation of treatment between 2010 and 2012. All children and parents coming to the clinic during that period were offered to participate in this study. Thirty-five accepted and there were only two losses to follow-up during the three-month period they participated in this study. The children were diagnosed with ADHD based on a clinical interview with a child psychiatrist, school reports and the Diagnostic Interview Schedule for Children (DISC-version IV). DSM-IV criteria were used to make the diagnosis (American Psychiatric Association, 2000). Exclusion criteria included having a diagnosis of pervasive developmental disorder, psychosis or Tourette’s syndrome or having an IQ of less than 70 on the fourth edition of the Weschler Scale for Children (Weschler, 2003). After diagnosis of ADHD and having accepted to take part in this study, information on the child’s demographics (i.e. gender, age, father’s years of education, mother’s years of education, income, and number of stressful life events) and on previous history of psychostimulants use were collected. Parents were asked to fill the Child Behaviour Checklist (CBCL), and the Conners’ Global Index – Parent version (CGI-P) to assess, respectively, the children’s behavioural difficulties, and the severity of ADHD symptoms. A copy of the Conners’ Global Index – Teacher version (CGI-T) was also faxed to the children’s teachers for them to complete. In order to assess their opinion towards ADHD and medication at baseline, parents were asked to complete the ADHD Knowledge and Opinion Survey (AKOS).
Children and their parents were tested by the research team three months after baseline. During that three-month period, medication was adjusted by the child psychiatrist. Children were seen weekly until the appropriate medication dose was established. A medication log, including names of medication and dosages, was kept for each patient by the research team using the information from the patient’s chart. At the three-month follow-up, parents participated in a standardized interview during which they were asked to list the number of side effects engendered by the ADHD medication and to assess their child’s adherence to medication. Parents were reassured that answers to these questions would not influence the treatment their child was receiving and that it was normal to forget to administer the medication. At this three-month follow-up, parents were asked to complete the CGI-P, AKOS, and the Southampton ADHD Medication Behaviour and Attitude Scale (SAMBA-P) while teachers and children filled, respectively, the CGIT and the children version of the SAMBA (SAMBA-C). Approval for the study was given by the Douglas Mental Health University Institute Ethics and Research Board. Written informed consent and assent were given by the parents and the children respectively.
Measures
Adherence to medication was entered as a continuous percentage variable (# of days on medication per week/7 days per week) following the answers to the standardized parents’ interviews. The CBCL was used to assess the severity of the children’s behaviour problems at baseline. Symptoms are divided into internalizing and externalizing. This 113-item questionnaire has an inter-rater reliability of 0.93 to 0.96, and test-retest reliability of 0.95 to 1.00 (Achenbach, 1991). The CGI-P and CGI-T are 10-item questionnaires which assesses the severity of the ADHD symptoms (Conners, Sitarenios, Parker, & Epstein, 1998a; 1998b). Components of the questionnaire are divided into two categories: “emotional lability” and “restlessness-impulsiveness behaviour.” Each item is scored on a four-point Likert scale and is then normalized into T-scores, with T-scores over 65 in the problem range.
The AKOS is a frequently used questionnaire to assess parental knowledge and attitudes of ADHD medications for research purposes. It consists of a 17-item true-or-false ADHD knowledge section followed by a 26-item ADHD opinion section which uses a six-point Likert scale. Questions from the opinion section are divided into four categories: “medication acceptability,” “counselling acceptability,” “counselling feasibility,” and “parent competence.” This study focused on parental “medication acceptability,” assessed through questions such as “I believe that medication could help my child with ADHD.” Scores of each domain are simply added to yield a domain score. Each domain has an internal consistency greater than 0.8 (Bennett et al., 1996).
The SAMBA, Child and Parent versions, are questionnaires that are used to assess the perceptions of treatment of both parents and children. It is commonly used in the rare studies that looked at children’s attitudes towards ADHD and psychostimulant medication. The following scales are assessed for both parent and children versions: “perceived psychosocial benefits of medication,” “perceived psychosocial costs of medication,” “patient’s stigma,” and “resistance to medication.” The parental version has the additional scales of “parental stigma,” “inconsistency in administering medication,” and “dosing flexibility.” Statements such as “The ADHD pills help my child to get on better with their family” were used to assess parental “perceived psychosocial benefits of medication” while these statements were simplified in the children version, for instance “The ADHD pills help me to be good.” For this study, high “perceived psychosocial benefits of medication” was defined as a score greater or equal to ten (on maximum of 20) for this measure on the SAMBA. Except for the inconsistency in using medication which had a reliability alpha of 0.67, all scales had a good internal reliability (α > 0.7) (Harpur et al., 2008).
Statistical Analysis
Statistical Package for Social Sciences (SPSS) was used to perform the statistical analysis. Pearson bivariate correlation test was first performed to search for correlations between adherence to medication and the following variables: AKOS “medication acceptability score” at baseline and three months, demographics, previous history of ADHD medication, initial CBCL total score, number of side effects, SAMBA-P, SAMBA-C, CGI-P and CGI-T (baseline, three-month, and change). Stepwise linear regressions were performed for variables that showed significant correlation in order to analyse how they predicted adherence to medication. Independent samples T-Tests were also performed to compare the differences between certain groups in their adherence to medication. Paired sample T-Tests were performed to assess the evolution of CGI and AKOS scores between baseline and the three-month follow-up.
Results
The study included 33 participants, with seven females and 26 males. Their demographic information can be seen in Table 1.
Table 1.
Description of the sample
| N or mean (SD) | % | |
|---|---|---|
| Age | 8.78 (1.77) | |
| Gender | ||
| Male | 26 | 78.8 |
| Female | 7 | 21.2 |
| Ethnicity | ||
| Arabic | 6 | 18.1 |
| Black | 3 | 9.1 |
| Caucasian | 22 | 66.7 |
| Hispanic | 1 | 3.0 |
| Other | 1 | 3.0 |
| Baseline CBCL T-Scores | ||
| Total | 63.09 (10.72) | |
| Externalizing | 60.55 (10.40) | |
| Internalizing | 57.73 (12.03) | |
| Previous history of psychostimulants use | 12 | 36.4 |
| Adherence to medication %: # of days on medication per week/7 days per week | 83.7 (21.98) |
The three long-acting psychostimulants prescribed in this study were slow-release methylphenidate (Concerta and Biphentin), and lisdexamfetamine (Vyvanse). At baseline 15 patients were prescribed methylphenidate (Concerta) at a median daily dose of 27 mg (range: 18–54 mg), 16 patients were prescribed methylphenidate (Biphentin) at a median daily dose of 15 mg (range: 10–25 mg) and two patients were prescribed lisdexamfetamine (Vyvanse) at a median daily dose of 25 mg (range: 20–30 mg). Three patients, all of them taking methylphenidate (Biphentin), had their prescription changed to either increase the prescribed dose by 5 mg (n=2) or decrease it by 5 mg (n=1). Mean adherence to psychostimulant medication for the sample was 83.7%. Using stepwise linear regression, a significant model emerged (adjusted R2=.301; F2,30=17.532; p=.002) in which male gender of the child (β=−18.097, SE=8.316, t=−2.176, p=.038) and “parental perceived psychosocial benefits of medication” at the three-month follow-up, as assessed by the SAMBA questionnaire, (β=1.954, SE=.818, t=2.389, p=.023) were found to be predictors of adherence to medication. Parental “medication acceptability,” as assessed by the AKOS at both baseline and at the three-month follow-up, was not found to be a statistically significant direct predictor of medication adherence. Children of parents with low “perceived psychosocial benefits of medication” at the three-month follow-up were moreover found to have a rate of adherence that was 18% lower than children of parents with high “perceived psychosocial benefits of medication” (p=0.35; Cohen’s d=0.56).
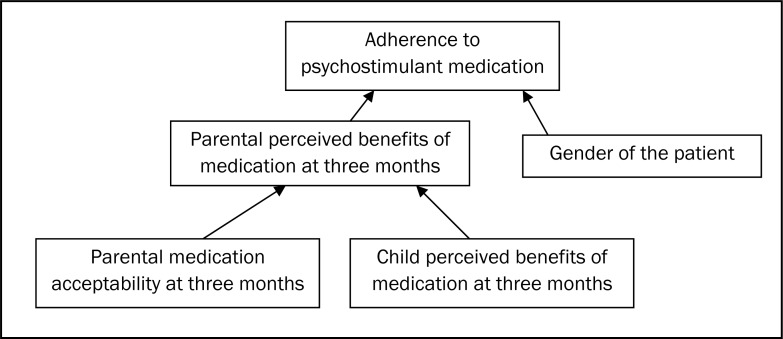
“Parental perceived psychosocial benefits of medication” at the three-month follow-up, as assessed by the SAMBA, was in turn found to be predicted (adjusted R2=.508; F2,30=8.760; p<.0005) by parental “medication acceptability” at three months, as assessed by the AKOS, (β=.542, SE=.106, t=5.126, p<.0005) and Child’s “perceived psychosocial benefits of medication” at three-months, as assessed by the SAMBA (β=1.954, SE=.123, t=2.364, p=.025).
A weak correlation (r=.397, p=.022) was found between symptoms of “restlessness and impulsiveness” at baseline, as assessed by the teachers on the CGI, and “medication acceptability,” as assessed by the AKOS at baseline. There was also a correlation (r=.345, p=.049) between symptoms of “emotional lability” at baseline, as assessed by the parents on the CGI, and adherence to medication. In most cases, however, severity of symptoms of ADHD, as assessed by the CGI, did not significantly correlate with medication adherence or “medication acceptability,” as assessed by the AKOS. Concerning parental and child “stigma,” as assessed by the SAMBA, a significant correlation was found between parental “medication acceptability” at the three-month follow-up, as assessed by the AKOS, and parental “stigma” in regard to medication, as assessed by the SAMBA (r=−.422, p=.014).
Discussion
Mean adherence for this sample was relatively high when compared with the literature (see introduction). This may be explained by the close monitoring of the subjects and the relatively short period (three months) of time being investigated, thus implying the importance of providing a regular and close follow-up to patients with ADHD and their family. Male gender of the child and higher parental “perceived psychosocial benefits of medication” (as a continuous variable) at the three-month follow-up, as assessed by the SAMBA, were found to be positive predictors of adherence to psychostimulant medication. Due to the small number of girls in this study (n=7), conclusions regarding the influence of gender of the child on adherence to psychostimulants are nonetheless limited and should be repeated with a greater sample size. It was however noted that, within this sample, boys did not differ significantly from girls in their ethnicity, age, SES, the severity of their symptoms or their initial presentation, except for boys being reported as having more inattentive and easily distracted behaviour initially. Secondly, and most importantly, this study suggests that clinicians who wish to improve the adherence to psychostimulant medication in children with ADHD could do so by working towards increasing the parental perceived psychosocial benefits of the medication as soon as possible after initiation of treatment.
The next question thus becomes how to influence parental “perceived psychosocial benefits of medication.” The answer to this question can be divided in two parts and is simplified in Figure 1. First, the results of this study suggest that improving parental general “medication acceptability,” as assessed by the AKOS, will lead to an improvement in “perceived psychosocial benefits of medication,” essentially a subset of medication acceptability measured by the SAMBA. Second, the results of this study suggest that in order to improve adherence to medication, the clinician should not ignore the attitudes of children regarding their pharmacological treatment but should in fact try to make them understand the purpose and benefits of their medication, in particular regarding psychosocial skills.
Figure 1.
Interplay of factors influencing adherence to medication
Clinicians may also want to pay attention to parental stigma, as this factor was negatively correlated with parental “medication acceptability,” as assessed by the AKOS. Parental “stigma” was assessed by the SAMBA through rating of statements such as “I am concerned that people think I am a bad parent because my child takes ADHD pills.”
Contrarily to what is suggested in the literature (Gau et al., 2008; Thiruchelvam et al., 2001), severity of symptoms was usually not found to influence adherence with medication in this study, nor was it found to influence parental “medication acceptability,” as assessed by the AKOS. The results of this study however suggest that the relation between severity of ADHD symptoms and medication adherence may be more complex than initially thought. Even though in some families higher symptoms may lead to greater medication adherence may be sound, it is also possible that in other families higher severity of symptoms of ADHD might render administration of the medication more difficult and thus negatively impact both adherence and attitudes to medication. Also unlike what is suggested in the literature (Gau et al., 2008; Thiruchelvam et al., 2001), age of the subject was not found to influence adherence to psychostimulant medication, although it must be noted that the age range of this sample was limited as shown by the standard deviation for age of only 1.77.
The key strengths featured in the unique approach adopted by this study included assessment of the child’s attitudes towards medication for ADHD in comparison to the parent’s, use of two different means of assessing opinions and attitudes towards ADHD, namely the AKOS and the SAMBA, and an in-depth analysis into both parental and children stigma towards ADHD and psychostimulants. This study also has some limitations including a relatively small sample size (N=33), a short follow-up of only three months, and assessment of adherence to medication through standardized interview instead of methods less susceptible to recall bias, such as pill count.
Conclusions
The results of this study suggest that children with ADHD with parents having high perceived psychosocial benefits of psychostimulant medication three months after initiation of treatment are more likely to have a high adherence to psychostimulant medication. Parental perceived psychosocial benefits of psychostimulant medication was in turn increased by higher parental “medication acceptability” and higher child’s perceived psychosocial benefits of medication.
Table 2.
CGI and AKOS medication acceptability scores at baseline and three months
| Variable | Baseline score (SD) | 3-month score (SD) | t(32) | p | |
|---|---|---|---|---|---|
| CGI-Parents | Restlessness-Impulsiveness | 68.72 (11.61) | 63.00 (12.43) | 3.531 | .001 |
| Emotional lability | 58.84 (11.68) | 57.47 (12.68) | .744 | .463 | |
| Total | 67.58 (11.66) | 62.38 (12.06) | 3.414 | .002 | |
| CGI-Teachers | Restlessness-Impulsiveness | 65.97 (8.84) | 55.50 (8.50) | 5.683 | .000 |
| Emotional lability | 56.41 (13.02) | 53.66 (11.57) | 1.107 | .277 | |
| Total | 65.06 (10.99) | 55.50 (9.59) | 4.368 | .000 | |
| AKOS Medication Acceptability | 28.54 (4.40) | 28.36 (4.98) | .249 | .805 |
Acknowledgements/Conflicts of Interest
We would like to thank Michael Grizenko-Vida, Johanne Bellingham, and Shalaka Shah for their help in data collection. The authors have no financial relationships to disclose.
References
- Achenbach T. The Child Behaviour Checklist/4-18. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington DC: 2000. [Google Scholar]
- Bennett DS, Power TJ, Rostain AL, Carr DE. Parent acceptability and feasibility of ADHD interventions: Assessment, correlates, and predictive validity. Journal of Pediatric Psychology. 1996;21(5):643–657. doi: 10.1093/jpepsy/21.5.643. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet. 2005;366(9481):237–248. doi: 10.1016/S0140-6736(05)66915-2. [DOI] [PubMed] [Google Scholar]
- Brown RT, Amler RW, Freeman WS, Perrin JM, Stein MT, Feldman HM. Treatment of attention-deficit/hyperactivity disorder: Overview of the evidence. [Review] Pediatrics. 2005;115(6):e749–757. doi: 10.1542/peds.2004-2560. [DOI] [PubMed] [Google Scholar]
- Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: Adherence, effectiveness, and adverse effects. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(5):559–567. doi: 10.1097/00004583-200405000-00009. [DOI] [PubMed] [Google Scholar]
- Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised Conners’ Parent Rating Scale (CPRS-R): Factor structure, reliability, and criterion validity. Journal of Abnormal Child Psychology. 1998a;26(4):257–268. doi: 10.1023/a:1022602400621. [DOI] [PubMed] [Google Scholar]
- Conners CK, Sitarenios G, Parker JD, Epstein JN. Revision and restandardization of the Conners Teacher Rating Scale (CTRS-R): Factor structure, reliability, and criterion validity. Journal of Abnormal Child Psychology. 1998b;26(4):279–291. doi: 10.1023/a:1022606501530. [DOI] [PubMed] [Google Scholar]
- Corkum P, Rimer P, Schachar R. Parental knowledge of attention-deficit hyperactivity disorder and opinions of treatment options: Impact on enrollment and adherence to a 12-month treatment trial. Canadian Journal of Psychiatry. 1999;44(10):1043–1048. doi: 10.1177/070674379904401011. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Zimmerman B. An analysis of patient adherence to treatment during a 1-year, open-label study of OROS methylphenidate in children with ADHD. Journal of Attention Disorders. 2007;11(2):157–166. doi: 10.1177/1087054706295663. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: Is it an American condition? World Psychiatry. 2003;2(2):104–113. [PMC free article] [PubMed] [Google Scholar]
- Gau SS, Chen SJ, Chou WJ, Cheng H, Tang CS, Chang HL, Huang YS. National survey of adherence, efficacy, and side effects of methylphenidate in children with attention-deficit/hyperactivity disorder in Taiwan. Journal of Clinical Psychiatry. 2008;69(1):131–140. doi: 10.4088/jcp.v69n0118. [DOI] [PubMed] [Google Scholar]
- Harpur RA, Thompson M, Daley D, Abikoff H, Sonuga-Barke EJS. The Attention-Deficit/Hyperactivity Disorder medication-related attitudes of patients and their parents. Journal of Child and Adolescent Psychopharmacology. 2008;18(5):461–473. doi: 10.1089/cap.2008.023. [DOI] [PubMed] [Google Scholar]
- Ibrahim ESR. Rates of adherence to pharmacological treatment among children and adolescents with attention deficit hyperactivity disorder. Human Psychopharmacology: Clinical and Experimental. 2002;17(5):225–231. doi: 10.1002/hup.406. [DOI] [PubMed] [Google Scholar]
- Johnston C, Hommersen P, Seipp C. Acceptability of behavioral and pharmacological treatments for attention-deficit/hyperactivity disorder: Relations to child and parent characteristics. Behavior Therapy. 2008;39(1):22–32. doi: 10.1016/j.beth.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Krain AL, Kendall PC, Power TJ. The role of treatment acceptability in the initiation of treatment for ADHD. Journal of Attention Disorders. 2005;9(2):425–434. doi: 10.1177/1087054705279996. [DOI] [PubMed] [Google Scholar]
- McNeal RE, Roberts MC, Barone VJ. Mothers’ and children’s perceptions of medication for children with attention-deficit hyperactivity disorder [Comparative Study] Child Psychiatry and Human Development. 2000;30(3):173–187. doi: 10.1023/a:1021347621455. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group Multimodal Treatment Study of Children with ADHD. Archives of General Psychiatry. 1999;56(12):1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Powers RL, Marks DJ, Miller CJ, Newcorn JH, Halperin JM. Stimulant treatment in children with attention-deficit/hyperactivity disorder moderates adolescent academic outcome. Journal of Child and Adolescent Psychopharmacology. 2008;18(5):449–459. doi: 10.1089/cap.2008.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiruchelvam D, Charach A, Schachar RJ. Moderators and mediators of long-term adherence to stimulant treatment in children with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(8):922–928. doi: 10.1097/00004583-200108000-00014. [DOI] [PubMed] [Google Scholar]
- Weschler D. Weschler Intelligence Scale for Children - Fourth Edition: Manual. San Antonio, TX: Psychological Corporation; 2003. [Google Scholar]