Abstract
Objectives
Using the Proactivity Model of Successful Aging, we examined how internal and external resources contribute to the maintenance of psychological well-being and social activities among older adults who experience normative stressors of aging. Outcome variables in this study are collectively referred to as quality of life (QOL). We also examined the mediating role of proactive adaptations between internal and external resources and QOL indicators.
Method
Based on five annual interviews of a sample of 1,000 community dwelling older adults in Florida (effective N = 561), we tested the lagged effects of stressors on two indicators of QOL, four years later. In the full longitudinal model, using structural equations, we estimated the direct effects of internal and external resources on QOL, along with indirect effects through proactive adaptations.
Results
Stressors negatively influenced QOL four years later. Internal and external resources led to better QOL four years later, both directly and indirectly through proactive adaptations of marshaling support and planning for the future.
Conclusion
These findings lend support to the Proactivity Model of Successful Aging by documenting the value of proactive adaptations (i.e., exercise, planning ahead and marshaling support) as proximate influences on QOL outcomes (i.e., depressive symptomatology and social activities). Findings suggest that older adults can maintain successful aging even in the face of health-related and social stressors by invoking accumulated resources to deal actively with the challenges of aging.
Keywords: Successful aging, adaptation to stress, proactivity, quality of life
Introduction
During late life older adults are exposed to stressors of social losses and increasing frailty, which can threaten their quality of life (QOL) (Kahana & Kahana, 2003a). To deal with these normative developmental challenges and with potential reduction in reserves in late life, developmental psychologists have emphasized the value of invoking dispositional resources such as “selective optimization with compensation” (Baltes & Baltes, 1993) and “socioemotional selectivity” (Carstensen, 1992). These orientations are predicated on an assumption of shrinking life space and the need for adaptation aimed at conserving resources (Birren, 1969). Unlike these approaches, the Model of Proactive Adaptation emphasizes the value of planful engagement in anticipation of, and in response to, age-related stressors (Aspinwall & Taylor, 1997). It proposes that older adults utilize personal and social resources with both preventive and corrective intent (Kahana & Kahana, 1996). This focus is consistent with approaches that value “agency” (Thoits, 2006) and “planful competency” (Clausen & Jones, 1998) for maintaining good QOL in old age in the face of stressors. There has been little prior research to help specify the types of behavioral adaptations that translate social and psychological resources into good QOL in old age.
Successful aging may be alternatively defined based on outcomes (Rowe & Kahn, 1998; Pruchno, Wilson-Genderson & Cartwright, 2010) or based on processes to deal with challenges (Baltes & Baltes, 1993; Schultz & Hechhausen, 1996). Outcome based orientations can preclude older persons who encounter stressors of frailty or social losses from being considered as aging successfully. We argue that processes and outcome can each play important roles in understanding successful aging.
The Proactivity Model of Successful Aging (Kahana & Kahana 1996; 2001; 2003) was developed to emphasize the potential of all older adults to meet challenges of aging through the use of enacted resources in the form of proactive adaptation. This focus overcomes the exclusionary orientation of prevalent models (Rowe & Kahn, 1998) that place good health and absence of disability center-stage as prerequisites for successful aging (Young, Frick, & Phelan, 2009).
The Proactivity Model of Successful Aging is distinctive as it brings preventive and corrective behavioral adaptations that are generally studied in the framework of behavioral health (Marquez, Bustamante, Blissmer & Prohaska, 2009) to inform stress theory. The Proactivity Model explores pathways to maintenance of psychological wellbeing and engagement in social activities, even for older adults who are exposed to stressors of illness, frailty, and social losses.
In the conceptual model we consider chronic illnesses, recent illness events, and functional limitations, along with social losses, to be among the normative stressors of aging that threaten QOL of older persons (Kahana & Kahana, 2003). We also hypothesize that older adults who experience such stressors benefit from social and psychological resources and from engaging in proactive efforts to help normalize their lives (Gerhardt, 1991). Furthermore, we propose that internal and external resources may impact QOL both directly and indirectly through proactive adaptations (Kahana & Kahana 1996; 2003). As such, proactive adaptations are viewed as the engine that drives successful aging (Aspinwall, 2011).
The Proactivity Model is anchored in the stress paradigm (Pearlin, Menaghan, Liberman & Mullan, 1981) that has been widely used by gerontological researchers to help understand the ill effects of stressful life circumstances on QOL outcomes (Chou & Chi, 2000). Traditional resources studied in the context of the stress paradigm include social supports (Sherman, Shumaker, Rejeski, Morgan, Applegate & Ettinger, 2006) and psychological resources (e.g. active coping orientations) (Hewitt & Flett, 1996).
In a separate realm of the health behavior literature, personal actions such as health promotion have been proposed as important influences on good quality of late life (Blumenthal & Gullette, 2002; Marquez, Bustamante, Blissmer & Prohaska, 2009). However, such behavioral adaptations have seldom been conceptualized and studied within the framework of the stress paradigm. A unique contribution of the Proactivity Model is the integration of proactive behavioral adaptations such as health promotion, planning ahead, and marshaling social supports into stress theoretical formulations (Kahana & Kahana 1996; 2003). We further recognize that dispositional, behavioral, and environmental resources play distinctive roles to promote QOL in old age.
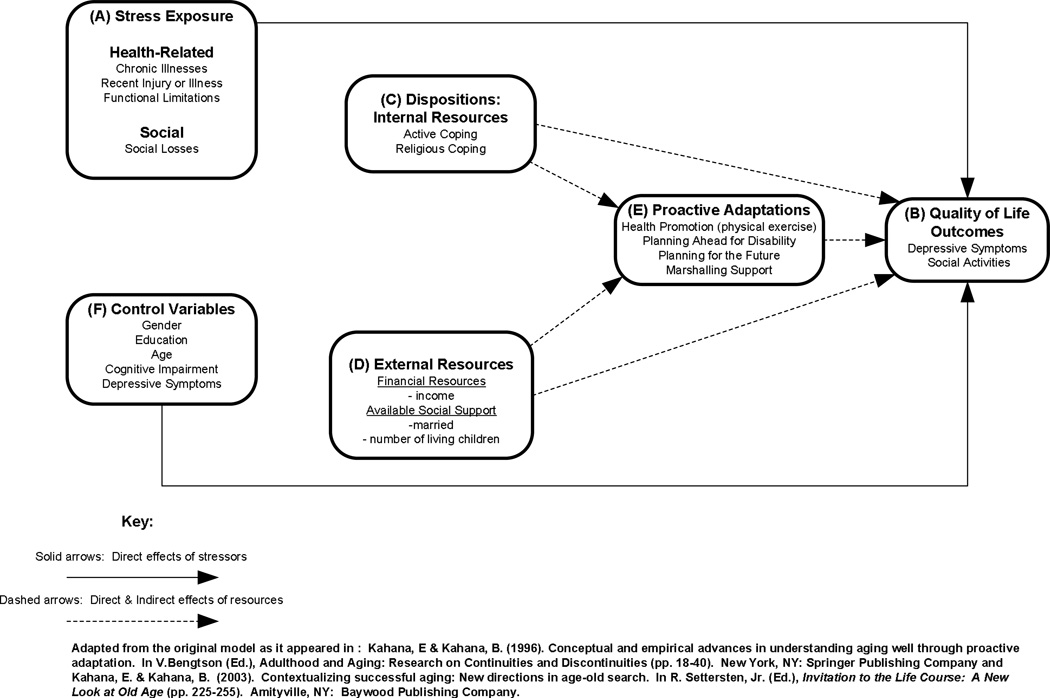
The Proactivity Model that we test in this paper (Figure 1) specifies how health-related and social stressors (component A) lead to adverse psychological and social QOL outcomes (component B). This model reflects traditional hypotheses about the positive roles that internal resources (component C) and external resources (component D) play in enhancing QOL. We further expand the conceptualization, specifying proactive adaptation (component E) as a proximal and potentially mediating influence, whereby external and internal resources influence QOL outcomes, both directly and indirectly, by enacting specific proactive strategies (Figure 1). Components of the broader Proactivity Model and their rationale have been described in prior publications (Kahana & Kahana, 1996; 2003; Kahana, Kahana & Kercher, 2003). Below we summarize the rationale for the specific model components explored in the present study.
Figure 1.
Longitudinal Operational Model of Strees Exposure, Buffers, and Quality of Life Outcomes.
A. Stress Exposure
The Proactivity Model is built on the recognition that with increasing age, older adults are likely to encounter chronic health conditions. Chronic illnesses can develop into functional limitations which are reflected in restricted abilities to perform activities of daily living (ADL) (Verbrugge & Jette, 1994). Along with the growing probability of chronic illnesses and functional limitations, older adults also encounter health-related life events such as falls or accidents (Ferraro, 2006). In addition to illness-related stressors, old age is also associated with social losses, as older friends and family members may die, encounter disabling illness, or may move to long-term care facilities (Krause, 2006). These cumulative stressors pose threats to QOL of the elderly individual (Kahana & Kahana, 1998; Kasen, Chen, Sneed & Cohen, 2010).
B. Quality of Life Outcomes
We consider the absence of depressive symptomatology as a key indicator of psychological well-being (Blazer, 2009). Furthermore, we also recognize participation in social activities as another important dimension of good QOL (Williamson, 2005). Stress exposure is expected to diminish QOL outcomes.
C. Internal Resources
The model we test focuses on active coping (Knight, Silverstein, McCallum & Fox, 2000) and religious coping (Bussing, 2009; Koenig, 1991) as internal dispositional resources, which can promote proactive behaviors, resulting in good QOL outcomes, even for older adults confronting normative stressors (Kahana & Kahana, 1996).
D. External Resources
We consider financial and social resources as environmental factors related to one’s structural position in society that can promote proactive adaptations in later life (Cohen 2004). Availability of social supports (Rook, 2009) and financial resources (Pudrovska, Schieman, Pearlin & Nguyen, 2005) have been found to predict late life well-being, particularly in stressful life situations. We conceptualize both internal and external resources as long-term and cumulative over the life course. We do not imply that stressors cause internal and external resources, but rather stressors may invoke their salutary benefits.
E. Proactive Adaptations
In contrast to internal and external resources, proactive adaptations are temporally proximate behaviors that an older adult may engage in order to help enhance their QOL. These behaviors are drawn from his/her existing resources such as active coping styles or family support resources. In this way, it is possible that later life well-being is influenced directly by internal and external resources available to the older adult and indirectly through proactive adaptations. No study of which we are aware examined these multiple pathways through which older adults maintain or achieve well-being. In this paper, we focus on three proactive adaptations drawn from the Proactivity Model: health promotion (exercise), planning ahead, and marshaling support (Kahana & Kahana, 2003; Kahana et al., 2002).
Health promotion/exercise
Among diverse proactive efforts to promote QOL outcomes in late life, physical activity consistently yields benefits (McAuley, Konopack, Motl, Morris, Doerksen & Rosengren, 2006). Even among frail older adults and those dealing with chronic illnesses, engaging in exercise in late life has long-term benefits for maintenance of psychological well-being and social functioning (Kahana, Lawrence, Kahana, Kercher, Wisniewski, Stoller, Tobin & Stange, 2002).
Planning Ahead
An important aspect of proactivity is planning ahead, because anticipation of future needs allows older adults to take more effective action (Aspinwall, 2011). Financial, environmental, and lifestyle related plans also reflect future orientation that may enhance QOL (Kahana, Kahana & Zhang, 2005).
Marshaling support
Marshaling support refers to actions taken by older people to mobilize available social resources (Greene, Jackson & Neighbors, 1993). Help seeking reflects social resourcefulness that contributes to receipt of both instrumental and affective support (Rapp, Shumaker, Schmidt, Naughton & Anderson, 1998).
Summary of Rationale
This paper extends previous investigations of late-life well-being among older adults by focusing on deployment of resources and agentic behaviors over time. The potential value of proactive behaviors during stressful life situations has been increasingly recognized (Ouwehand, de Ridder & Bensing, 2007; Spira, 2006). However, much of the empirical literature to date has conceptualized and tested models without regard to time, resulting in little evidence for understanding how internal and external resources and proactive behaviors work separately or together to maintain well-being. We advance this line of inquiry by moving past single-wave correlational studies to examine the temporal ordering of resource enactment and potential proactive behaviors to diminish the long-term effects of social stressors. Ouwehand et al., (2007) explicitly note the likely temporal ordering of proactive adaptations in the face of stressors, specifically hypothesizing that internal and external resources, accumulated over the life course, are used by the older adult to enact specific behaviors and adaptations that diminish the effect of current stressors and prevent or delay the occurrence of new stressors. Despite this articulation of a temporal process in successful maintenance of good QOL, no empirical study to our knowledge has actually tested this model.
Based on both the conceptual and empirical literature, we hypothesize that external and internal resources influence well-being in late life, both directly and indirectly, through proactive behaviors. While the scaffolding of external and internal resources likely represents an accumulation over the life course (e.g., income, learned coping skills) and therefore temporally precedes social and health stressors, we hypothesize that the impact of the resources are most observable once the older adult experiences social and health stressors. This is a time when the older adult may mobilize these resources to directly influence well-being or enact a series of proactive adaptations that subsequently help preserve QOL. Proactivity is the proximate influence on wellbeing, but these are specific behaviors drawn from an older adult’s social, psychological, and economic resources.
Methods
Sample
Data for this research are obtained from the Florida Retirement Study, a panel study which focuses on late-life adaptation of retirement community-dwelling elderly persons (Borawski, Kinney, & Kahana, 1996; Kahana et al., 2002). The retirement community was designed to attract active, healthy residents aged 55 years or older and does not offer any support services (e.g., meals and housekeeping). Participants resided in condominiums, most of which were one bedroom units (850 square feet) in three-story buildings, without elevators. Respondents generally migrated after retirement from the Midwest and most lived dispersed from their extended families.
A total of 3,905 households were randomly selected from residential listings of the retirement community. Selected households were contacted by telephone to determine if a member of the household met eligibility criteria (see Kahana et al., 2002). Eligibility criteria included; (a) age 72 years or older at baseline, (b) living in Florida at least nine months out of the year, and (c) reporting that they were “sufficiently healthy” to complete a ninety minute face-to-face interview. Of the 3,905 households contacted, 48.9% (n=1,909) did not meet eligibility criteria (25.8% due to age, 15.5% due to part-time residency, and 7.6 % due to self-report of poor health). Additionally, 13.4% (n=522) of households contacted refused participation and 14.5% of households could not be reached after a series of five attempts by the research staff.
The response rate for those approached and invited to participate in the Florida Retirement Study at baseline was 77.3%. At the start of the study, 1,000 respondents, representing 908 households completed an in-home, face-to-face interview. Interviews were conducted annually by trained interviewers. Respondents were contacted and reinterviewed regardless of their residential status (i.e., moved or residentially stable). During the four-year follow-up, 21% made a residential move. Death was the primary source of attrition for this sample. Indeed, loss to follow-up for other reasons (e.g., moving with no forwarding address) accounted for only 7% of annual attrition. This study uses data from Waves 1 through 5 of our panel study (N = 561).
The average age of respondents at the start of the study was 79.35 years with a standard deviation of 4.82. Almost 2/3 of the sample (65.8%) were female. All study respondents were of Caucasian race. About half of the sample (47.2%) were married with the vast majority of the remainder, 46.5%, widowed. Only 2.2% were separated or divorced; 4.1% had never been married. Reflecting the marital status characteristics noted above, 51.4% lived alone and 45.5% lived with their spouse. Only 2.5% of the sample lived with other relatives and 1.3% lived with non-family. In terms of educational background 12.9% reported less than a high school education, 27.7% were high school graduates, 14 9.5% had at least some college training, and 9.9% reported having a post-college education. Most of the respondents participating in our study were of modest financial means: 10.1% of the sample reported an annual income (before taxes) below $10,000, 35.8% reported an income between $10,000 – $19,000 and 39.4% reported an income between $20,000 – $29,000 per year. Only 14.7% reporting an income (before taxes) of over $40,000 per year. In terms of total family assets 27.8% reported assets of over $225,000. About a quarter of the sample 21.8% reported assets of under $75,000. In terms of work status 80.3% were retired, 3.1% were working part-time, and 16.6% never worked for pay. Average length of time respondents lived at the Florida retirement community was 10.9 years (SD=5.69). The majority of respondents (76%) obtained fee-for-service healthcare. The remaining 24% participated in HMO health services. All were eligible for Medicare. In terms of religious affiliation, 68.2% were Protestant, 20.4% were Catholic, 5.6% were Jewish, and 4% reported “no religious affiliation”. The remaining 1.8% of respondents reported “other” or “refused”. While the generalizability of findings are limited by sample characteristics, it is notable that this was not a particularly affluent and advantaged group of older adults.
Measurement
Outcomes were measured at Wave 5 (5th annual follow-up) and predictor variables were measured at prior annual waves (1, 2, 3, or 4). This temporal ordering allowed us to explicate the causal processes more clearly than designs where all variables are measured at the same time point. The effective N for these analyses is 561, based on the Wave 5 interview. All analyses were adjusted for nonrandom attrition using the Heckman two-stage estimator.
Figure 1 depicts the conceptual relationships between the stressors, internal and external resources, proactive adaptations, and QOL outcomes. Table 1 presents the variables for each domain with their coding, mean, and standard deviation.
Table 1.
Mean, Standard Deviation, and Coding for Variables in Proactive Adaptations Conceptual Model
| Variable | Coding | Mean | Standard Deviation |
|---|---|---|---|
| Psychosocial QOL | |||
| Depressive Symptoms W5 | Range 0 – 40 | 8.97 | 5.67 |
| Social Activities W5 | Range 0 (no engagement) to 36 (high engagement) | 15.53 | 3.64 |
| Physical/Social Stressors | |||
| Total Chronic Illness W1 | Range 0 conditions to 10 conditions | 1.54 | 1.21 |
| Injury or Illness in Past Year W1 | 1 = Yes; 0 = No | .12 | --a |
| ADL & IADL Disability W1 | Range 0 (No Limitations) to 33 (Unable to Perform Any Domains) | 1.25 | 3.72 |
| Social Losses in Past Year W1 | Range 0 to 4 | 1.25 | 1.00 |
| Internal Resources | |||
| Active Coping W2 | Range 0 to 32 | 17.93 | 4.30 |
| Religious Coping W2 | Range 0 to 12 | 8.68 | 3.62 |
| External Resources | |||
| Income W1b | 1 = <$2,500; 15 = >$50,000 | 8.25 | 2.90 |
| Married W2 | 1 = Married; 0 = Other | .46 | -- |
| Total Living Children W2 | Range from 0 to 12 | 1.79 | 1.54 |
| Proactive Adaptations | |||
| Marshaling Support W3 | 1 = Very Difficult; 5 = Very Easy | 2.90 | 1.02 |
| Planning Ahead for Disability W4 | 1= Yes; 0 = No | .60 | -- |
| Planning for the Future W3 | 1= Yes; 0 = No | .59 | -- |
| Physical Exercise W4 | 1 = Rarely/Never; 5 = Several hours per day | 3.02 | 1.23 |
| Control Variables | |||
| Female | 1 = Female; 0 = Male | .66 | -- |
| Age | Range 72 to 98 | 79.35 | 4.82 |
| Highest Degree Earned | 1 = Less than HS; 6 = Graduate Degree | 2.88 | 1.30 |
| Cognitive Impairment W1 | Range 0 to 6 Errors | .19 | .59 |
| Depressive Symptoms W1 | Range 0 to 30 | 7.09 | 5.11 |
Standard deviations not reported for binary variables.
Income not measured at W2.
Effective N = 561
There were two QOL outcomes for these analyses: depressive symptoms and participation in social activities. Both were measured at Wave 5. Depressive symptoms were measured with the CES-D ten-item short scale (Irwin, Haydari & Oxman, 1999). Respondents stated the degree to which statements like the following were true for them: “I could not shake off the blues.” Response categories ranged from “Never” (0) to Always (4). Items were summed, creating a composite score ranging from 0 (Never on all items) to 40 (Always on all items). Depressive symptoms at Wave 1, used as a control variable, were measured identically. Reliability is high for both (W1 alpha = .86; W5 alpha =.85).
The second outcome was participation in social activities measured at Wave 5. Respondents were asked to report the amount of time they spent engaged in nine different activities including participating in church or synagogue, work, volunteer activities, and hobbies. Response categories ranged from “Never” (0) to “Several hours per day” (4). Items were summed, creating a composite score with a range from 0 to 36. Engagement in social activities was not measured until Wave 5, so the baseline level of activity could not be considered in these analyses.
The independent variables included physical and social stressors, internal resources, and external resources, proactive adaptations, and control variables. Health-related stressors and social stressors were measured at baseline. The former contained three variables: chronic illness, serious injury or illness in the past year and functional limitations.
Chronic illness was measured by a modified version of the OARS (Fillenbaum & Smyer, 1981) summing the prevalence of ten health conditions at baseline, including arthritis, heart trouble, cancer, and diabetes. The potential range of the variable was 0 to 10, although the maximum number of conditions in this sample was seven.
Recent injury or illness was measured as a binary variable indicating whether the respondent had experienced such an event in the past year. Those who had were coded 1 and all others were coded 0.
Functional limitations were measured by combining two scales: Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) (Lawton & Brody, 1969). Respondents were asked about their level of difficulty performing five ADL tasks (e.g., washing, bathing and eating without assistance) and six IADL tasks (e.g., getting from room to room and doing one’s own housework). Response categories ranged from never having difficulty (0) to having difficulty all of the time (3). Eleven items were summed, creating a single measure of limitations ranging from no limitations (0) to difficulty on all of the time on all items (33). Due to the multi-collinearity between the IADL and ADL measures, a combined functional score provided the best model fit. The inter-rater reliability of all eleven items was .93, indicating a high level of agreement among the individual indicators.
Social stressors were measured with a single variable; a count of the number of social losses experienced by the respondent during the previous year. These included the following four events: illness or injury of a friend or relative, death of a close friend, death of a close family member, and divorce of a child or grandchild.
Internal resources were operationalized as active and religious coping measured at Wave 2. These variables were measured by subscales of the Carver Coping Inventory (Carver, Scheier & Kumari-Weintraub, 1989). In preliminary analyses, we tested the full scale but these two subscales, measured separately, produced the best fitting model. Active coping was a summed scale of eight strategies used to cope with challenges including “I do what has to be done, one step at a time.” Religious coping (α = .92) was a summed scale comprised of three items including “I put my trust in God.” Respondents indicated the degree to which they were inclined to use each of the strategies when confronted with stressful situations. Responses ranging for each item from 0 (never) to 4 (very often) were summed. The Active Coping (α = .71) scale ranges from 0 to 32. The Religious Coping scale ranges from 0 to 12.
External resources had two categories: financial and social. We measured financial resources by Wave 1 (annual) income, which was a categorical variable ranging from “Less than $2,500” (1) to “More than $50,000” (15). Social resources were measured by number of living children at baseline, which was a count ranging from 0 to 12. A second indicator of social resources was whether the respondent was married at Wave 2. We used the Wave 2 marital status for two reasons. First, recent loss of spouse was captured in our measurement of recent social losses at Wave 1 so baseline marital status was confounded with recent role transition of widowhood. Second, consistent with our conceptualization of marital status as an external resource, we anticipated that those who were married at Wave 2 would likely enact the resources associated with that social role in the use of proactive adaptations. Changes in marital status, a normative event among the oldest old, can have significant impact on our measured outcomes, so it was important to isolate the specific temporal frame in which such proactive actions occurred. In this sample, the “other” category was predominantly those who were widowed.
Proactive adaptations had four measures. Marshaling support was measured with a single question asking “How easy do you find it to ask others for help?” Responses ranged from “Very difficult” (1) to “Very easy” (5).
Planning ahead was measured with two indicators. First, respondents were asked if they had, in the past year, made any future plans such as taking a trip, or starting a new project. Second, respondents were asked if they made any plans in the past year to prepare for possible future physical disability. For both of these questions, “Yes” was coded 1 and “No” was coded 0.
Physical exercise was our indicator of health promotion. Respondents self-reported the frequency with which they exercise across five categories ranging from never/rarely (1) to several hours per day (5). In our data analyses, we used the Wave 4 measures of these proactive adaptations so that these behaviors were measured temporally after the internal and external resources.
Finally, we included several control variables. Females were identified in a binary variable where 1 designated women and 0 designated men. Age was measured in years and ranged from 71 to 98. Education level was a categorical variable indicating the highest degree earned that ranged from less than a high school diploma (1) to a graduate degree (6). Cognitive impairment was assessed using Pfeiffer’s (1975) mental status questionnaire. Incorrect answers were summed, creating a single measure potentially ranging from zero to ten wrong answers.
Analysis
To address our research questions, we undertook a path analysis to estimate the direct, indirect, (through proactive adaptations) and total impact of internal and external resources on well-being in W5. We generated maximum likelihood model estimates based on an asymptotic covariance matrix generated from polychoric and polyserial correlations. Specific indicators within each domain (e.g., proactive adaptations) were allowed to freely correlate. For each of the QOL outcomes (i.e., depressive symptoms and engagement in social activities), we estimated two models. Model 1 tested the impact of the physical and social stressors on QOL four years later, with control variables. Model 2 tested the full conceptual model, including the potential mediating effect of proactive adaptations in the relationship between internal and external resources and well-being over time. We report the direct, indirect (through proactive adaptations), and total impact of these resources on QOL, as estimated in Model 2 for each outcome. Since most variables in the model are specific indicators rather than standardized scales, we report the unstandardized slope coefficients and standard errors throughout the results for ease in interpretation since it allows us to retain the original scale of each variable (Bollen 1989).
We elected to conduct a path analysis using structural equation models for several reasons. First, we were able to estimate simultaneously the direct, indirect, and total effects on QOL, which is the best test of the conceptual model. Second, we accounted for the potential correlated error within each domain (e.g. internal resources). These results are not presented here because they did not add substantively to the findings. However, the full model estimates, including residuals, are available from the first author. Third, the independent variables in this study were measured as binary, ordinal, and continuous. In addition, neither of the outcome variables was normally distributed. The resulting model estimates might be sensitive to such departures from normality, so we used polychoric and polyserial correlations to generate the input covariance matrix for final estimation. Preliminary analyses indicated that such an approach produced the most efficient model solutions.
In this sample of the oldest-old, attrition due to mortality was quite high. By Wave 5, more than 20 percent of the sample had died. Preliminary analyses and previous published work (e.g. Kahana et al., 2002; Kelley-Moore et al., 2006) indicated that mortality risk was lower for those who have higher levels of internal resources, and external resources and proactive adaptations, which could have introduced potential selection bias into our longitudinal analyses. To adjust for this, each model was adjusted for nonrandom attrition using a hazard rate instrument based on the inverse Mills ratio expressing the likelihood of not remaining in the study for all five waves (Heckman, 1979). A probit equation estimated the likelihood of completing all five waves of the study instrumented with the following covariates: retired more than 20 years ago; unintentional weight loss of 5lbs or more in past year; experienced a recent fall; frequency of attending religious services; male. Based on that likelihood, an inverse Mills ratio was calculated for each case so that high values indicated a strong likelihood of not completing the study. This variable was entered into the substantive model as a covariate (Berk, 1983). This technique was used in previous panel studies of older adults and has been shown to be an efficient and sensitive technique to adjust for nonrandom selection bias due to mortality (Fitzgerald, Gottschalk & Moffitt, 1998).
Results
Table 2 presents the total effects in Models 1 and 2 for both outcomes: depressive symptoms and social activities. In Model 1, those who had experienced an injury or serious illness, during the year prior to baseline, had increases in depressive symptoms four years later (Wave 5). Those who had experienced social losses, during the year prior to baseline, also exhibited more depressive symptoms four years later. Among the control variables, women experienced greater increases in depressive symptoms than men. Baseline depressive symptoms were positively related to depressive symptoms four years later (Wave 5).
Table 2.
Maximum Likelihood Estimates of Stressors, Resources, and Proactive Adaptations on Quality of Life: Total Effectsa
| Depressive Symptoms | Social Activities | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Variables | ||||
| Physical/Social Stressors | ||||
| Injury/Illness in Past Yr | 3.15 (1.47)* | 3.01 (1.64) | −2.20 (.65)*** | −1.90 (.89)* |
| Total Chronic Illness W1 | 8.01 (5.46) | 7.91 (5.49) | −2.74 (.66)*** | −2.39 (.87)** |
| ADL/IADL Disability W1 | −.51 (.39) | −.43 (.40) | −.53 (.18)** | −.31 (.26) |
| Social Losses in Past Yr W1 | 1.16 (.35)*** | .99 (.51) | −.03 (.04) | −.12 (.14) |
| Internal Resources | ||||
| Active coping W2 | -- | 1.02 (1.31) | -- | 1.94 (.64)** |
| Religious Coping W2 | -- | −4.98 (1.65)** | -- | .23 (.74) |
| External Resources | ||||
| Married W2 | -- | −1.01 (.26)*** | -- | −.62 (.12)*** |
| Total Living Children W2 | -- | −6.32 (2.20)** | -- | 4.80 (.98)*** |
| Income W1 | -- | −1.76 (.79)* | -- | 1.44 (.35)*** |
| Proactive Adaptations | ||||
| Marshaling Support W3 | -- | −4.26 (1.18)*** | -- | 1.86 (.52)*** |
| Planning Ahead for Disability W4 | -- | .94 (2.09) | -- | −1.60 (.92) |
| Planning for the Future W3 | -- | −3.17 (.99)*** | -- | 1.50 (.44)*** |
| Physical Exercise W4 | -- | −2.11 (1.01)* | -- | 1.74 (.68)** |
| Control Variables | ||||
| Female | 4.36 (.43)*** | 4.04 (.48)*** | 1.46 (.15)*** | 1.32 (.21)*** |
| Age | .91 (.58) | 1.05 (.60) | −.76 (.29)** | −.31 (.26) |
| Highest Degree Earned | .49 (.26) | .50 (.22)* | .06 (.03)* | .03 (.10) |
| Cognitive Impairment W1 | −.22 (.61) | −.28 (.83) | −.33 (.31) | −.38 (.37) |
| Depressive Symptoms W1 | 1.87 (.20)*** | 1.60 (.22)*** | −.52 (.13)*** | −.39 (.10)*** |
| Mortality λ | .42 (1.27) | .72 (1.76) | −7.26 (.31)*** | −6.49 (.78)*** |
| R2 | .28 | .34 | .25 | .36 |
| χ2 (df) | 437.97 (53) | 391.35 (43) | 478.63 (57) | 410.52 (46) |
| Goodness of Fit Index | .96 | .99 | .95 | .98 |
| Incremental Fit Index | .96 | .98 | .96 | .98 |
| Root Mean Square Error of Approximation (RMSEA) | .04 | .01 | .04 | .02 |
There is some variation in degrees of freedom across models due to constrained error terms to maximize model fit. The full results are available from the first author.
Turning to Model 1 for engagement in social activities, we found that those who had experienced an illness or injury prior to baseline, those with more chronic illnesses, and with more ADL/IADL limitations were engaged in lower levels of social activities four years later (Wave 5). Some older adults engaged in higher levels of social activities: women, those who were younger, those with more education, and those with fewer depressive symptoms.
To summarize the findings of Model 1 for both outcomes, physical and social stressors were associated with poorer QOL four years later. Model statistics indicated a good fit for both models. For depressive symptoms, the model chi-square was 437.97 with 53 degrees of freedom. The Goodness of Fit Index (GFI) was .96 and the Root Mean Square Error of Approximation (RMSEA) is .04, which was below the recommended .05 threshold. Likewise for social activities, the model chi-square was 478.63 with 57 degrees of freedom. The GFI was .95 and the RMSEA was .04.
Although our focus in this study is on the long-term impact of stressors, to contextualize our findings we also examined the effect of more temporally proximate stressors on quality of life in W5. Not surprisingly, depression is higher for those who have experienced 3 or more social losses in the prior year (W4) relative to those who experienced 3 or more social losses at W1. However, there is no significant difference in depression scores for those who experience 0, 1, or 2 social losses respectively. Likewise, there is minimal difference in participation in social activities at W5 based on social losses at W1 versus W4. As for the other stressors, chronic illness is relatively stable over the observation period, as is its effect on depression in bivariate tests.
We now turn to Model 2, which includes internal resources, external resources and proactive adaptations to determine whether these resources are mediated by the proactive adaptations for long-term QOL. This model simultaneously estimated the direct impact of each domain and the indirect impact of resources through proactive adaptations on QOL at Wave 5. The total effects of Model 2 are presented for each outcome first, then the direct and indirect partial effects.
For depressive symptoms, Model 2 indicates that with the addition of internal resources, external resources, and proactive adaptations, the stressors of prior injury or illness and social losses no longer significantly influenced change in depressive symptoms four years later. Among the internal resources, only religious coping was associated with lower levels of depressive symptoms. All three external resources (being married, total number of living children, and higher income) were associated with fewer depressive symptoms at Wave 5. Three of the proactive adaptations led to decreases in depressive symptoms: marshaling support, planning for the future, and physical exercise. Women with higher education and higher baseline depressive symptoms had greater increases in depressive symptoms by Wave 5. Fit statistics indicate that Model 2 was a significantly better specification. RMSEA improved from .04 to .01, and GFI improved from .96 to .99.
Model 2 for social activities demonstrates that the internal and external resources and the proactive adaptations of older adults lessened, but did not completely eliminate the impact of the stressors on social activities four years later. ADL/IADL limitations no longer limit participation in social activities, but chronic illnesses and recent injury or illness at Wave 1 were still associated with fewer social activities at Wave 5. Among the internal resources, active coping was the only one associated with greater participation in social activities three years later. As with depressive symptoms, all three external resources influenced QOL at Wave 5. A larger number of living children and higher income was associated with more social activities at Wave 5. Being married, however, was associated with less participation in social activities. Among the proactive adaptations marshaling support, planning for the future, and physical exercise positively influenced participation in social activities. Planning for disability was the only proactive adaptation that did not influence level of social activities one year later.
The conceptual model (Figure 1) illustrates our argument that internal and external resources influence QOL up to four years later both directly and indirectly through proactive adaptations. We decomposed the total, direct, and indirect effects of internal and external resources to demonstrate the mediating effects of proactive adaptations. The results in Table 2 show the total effects for resources and proactive adaptations on QOL. Table 3 presents the maximum likelihood estimates of resources on proactive adaptations (Component B in the conceptual model).
Table 3.
Maximum Likelihood Estimates of Internal and External Resources on Proactive Adaptationsa
| Marshaling Support |
Planning for the Future |
Planning for Disability |
Physical Exercise |
|
|---|---|---|---|---|
| Variables | ||||
| Internal Resources | ||||
| Active Coping W2 | .14 (.05)**b | .16 (.06)** | .06 (.03)* | .44 (.18)* |
| Religious Coping W2 | .13 (.04)** | −.04 (.05) | .05 (.02) | .19 (.18) |
| External Resources | ||||
| Married W2 | .02 (.01)* | −.01 (.01) | −.03 (.001)*** | .16 (.02)*** |
| Living Children (#) W2 | .17 (.07)* | .54 (.09)*** | .12 (.04)*** | .68 (.26)* |
| Income (Annual) W1 | .02 (.03) | .03 (.03) | .07 (.01)*** | .11 (.06) |
| R2 | .08 | .09 | .13 | .18 |
Overall, these findings indicate that an older adult’s internal and external resources strongly influenced the willingness and ability to invoke proactive adaptations in the face of stressors. There is some variation in the exact resources that positively influenced specific types of proactive adaptations. Marshaling support, the first of the four proactive adaptations, was influenced by both internal resources: active coping and religious coping. Among the external resources, those who were married and those who had a greater number of living children were more willing to marshal support. Planning for the future was only influenced by two resources: active coping and having more living children. Planning for disability, on the other hand, shared active coping as an influence but was also associated with all three external resources: being married (albeit negatively), having more living children, and more income. Finally, reported frequency of physical exercise was higher among those who were married, those who had more children, and those who engaged in active coping.
The final component of the conceptual model (Figure 1) are the direct and indirect (through proactive adaptations) influences of Wave 2 resources on QOL at Wave 5. In the conceptual model, these paths are labeled with “C.” Table 4 presents these results. We turn first to depressive symptoms. Active coping did not directly influence depressive symptoms at Wave 5, but it had a strong and negative influence through proactive adaptations. Those who reported using active coping strategies exhibited fewer depressive symptoms, but the mechanism works through proactive adaptations to stressors. Religious coping worked the other way: there was a direct relationship between more religious coping and fewer depressive symptoms, but no indirect relationship through proactive adaptations. Marriage had a direct and negative influence on depressive symptoms, while number of living children had an indirect influence on such symptoms over time via proactive adaptations. Those who were married and those with more living children had fewer depressive symptoms over time.
Table 4.
Impact of Internal and External Resources on Quality of Life Outcomes: Direct and Indirect Effectsa
| Depressive Symptoms W5 | Social Activities W5 | |||
|---|---|---|---|---|
| Direct Effect |
Indirect Effect |
Direct Effect | Indirect Effect |
|
| Variables | ||||
| Internal Resources | ||||
| Active coping W2 | 2.19 (1.45) | −1.22 (.40)*** | 1.61 (.64)* | .33 (.19) |
| Religious Coping W2 | −4.01 (1.66)** | −.53 (.33) | .18 (.73) | .05 (.15) |
| External Resources | ||||
| Married | −.99 (.27)*** | −.01 (.09) | −.72 (.12)*** | .09 (.04)* |
| Living Children (#) W2 | −4.30 (2.26) | −2.02 (.79)* | 3.74 (1.00)*** | 1.06 (.36)** |
| Income (Annual) W1 | −1.55 (.80) | −.20 (.22) | 1.51 (.35)*** | .03 (.11) |
For social activities, active coping had a positive and direct influence. Religious coping did not influence participation in social activities. External resources had a more mixed influence on social activities. Being married at Wave 2 had a negative direct effect on social activities but a positive impact on social activities through proactive adaptations. This is because marital status had both a positive and negative effect on proactive adaptations. Those who were married were significantly more likely to marshal support and exercise more frequently but were less likely to plan for disability (see discussion section for more detail). Number of living children had a positive direct and indirect influence on social activities at Wave 5. Finally, total income positively influenced social activities through a direct relationship, but had no indirect relationship through proactive adaptations.
Discussion
In this research we found compelling support for the Proactivity Model (Kahana & Kahana, 2003), affirming the role of preventive and corrective behaviors reflecting agency in late life (Thoits, 2006). Our results confirm stress theory based expectations that stressors (e.g. injury or illness, chronic conditions, ADL/IADL disability and social losses) have an enduring negative influence on QOL (Pearlin et al.,1981) However, this sample of old-old persons used their existing resources to invoke proactive adaptations and in some cases eliminate the long-term negative influence of these stressors on QOL. Of particular note is the specification of processes regarding the mediating effect of proactive adaptations. Thus our findings reveal that internal and external resources influence subsequent depressive symptoms and social activities both directly and indirectly through proactive adaptations. Indeed, older adults invoke these resources to take positive action for their own well-being (Thoits, 2006). In this context, it is useful to note that external and internal resources were generally found to be stable in this sample over time. This finding allows for a refinement of the original Proactivity Model (Kahana & Kahana, 2003) by supporting a mediating role for proactivity.
This study advances our understanding of aging and well-being in several ways. First, we examine the long-term impact of stressors, resources, and proactive adaptations on QOL (Wheaton, 1996). By spacing the domains at sequential waves, we were able to move beyond cross-sectional data and make inferences about the sequencing of variables without risking potentially recursive or concurrent relationships. This model also allows us to observe the interplay of existing internal and external resources and the more temporally-proximate proactive adaptations, something that cannot be done when all domains are measured at the same wave. A further contribution of this study is that we examined the direct influence of internal and external resources on QOL four years following baseline and demonstrated the mediating effect of proactive adaptations. Gerontologists and social scientists have long been aware that internal and external resources such as active coping, marriage, and income can influence QOL in the short- and long-term (Pudrovska et al., 2005). However, there has been little research on how these domains work together when an older adult faces social and health stressors. This study is one of the first to examine the dynamic process of using internal and external resources to invoke specific proactive adaptations in the face of health and social stressors, an area of research called for by scholars in this field (George, 2005).
Overall, our findings support the value of both personal agency and interpersonal agency in contributing to successful aging in the face of normative stressors of aging (Smith, Kohn, Savage-Stevens, Finch, Ingate & Lim, 2000). Our findings also confirm linkages between social or health-related stressors and QOL outcomes posited in the Proactivity Model of Successful Aging (Kahana &Kahana, 1996; 2003). We also found support for prior findings that outcomes of depressive symptoms and activities are significantly influenced by social losses and acute illness or injury (Greenglass, Fiksenbaum & Eaton, 2006). It is notable that in the absence of resources and proactive adaptations, chronic illnesses or functional limitations did not result in diminished psychological QOL, as reflected by depressive symptoms. However, these social and health stressors – specifically chronic illnesses, health events, and functional disabilities – did impinge on subsequent participation in social activities. These findings are consistent with prior research linking stress exposure to poor quality of social life (George, 2005).
Our analysis regarding the role of internal, dispositional resources on two dependent variables affirm the value of active and religious coping as benefiting QOL among older adults, thus generally confirming elements of the proactivity conceptual framework. The mechanism by which social resources enhance QOL may involve interplay between coping and social resources as friends or family may help the older person utilize better or novel coping responses (Krause, 2006). Availability of potential strong ties implied by marriage and presence of children may also contribute to maintenance of interpersonal skills reflected in proactive adaptations (e.g. marshaling support). For the old-old (75+) and oldest-old (85+), who are typically reluctant to accept aid from others (Meredith & Schewe, 2002), the ability to marshal support is particularly important.
Our findings also support findings of prior research that psychological resources and coping efforts are effective in promoting psychological well-being outcomes even in the face of ill health, but are less successful for maintaining social activities that are dependent on mobility and stamina (Darling, 2003). It is noteworthy that availability of social resources facilitated proactive coping efforts and thereby contributed to goal attainment for frail older adults and for those who experienced social losses. External resources, as defined by higher income and availability of social support (i.e., being married and having more living children), proved to exert a significant influence on both psychological and social outcomes for elders facing stressful health events and social losses (Aspinwall, 2011).
Our expectations regarding marriage as a social resource were confirmed in relation to reduced depressive symptoms. However, contrary to expectations, being married led to making fewer plans for care needs and also to reduced social activities. On closer scrutiny, these are meaningful patterns, as the availability of a spouse may make the couple feel more self-contained and offer a sense of security regarding care needs (Kahana, Kahana, Wykle & Kulle, 2009). Nevertheless, in future research it will be useful to consider at greater depth relational aspects of family (both spousal and parent-child relationships) that have been shown to shape well-being (Umberson, 1992; Umberson, Williams, Powers, Chen & Campbell, 2005).
Our findings provide consistent support for the hypothesized mediating roles of diverse proactive adaptations which are the fundamental innovative components of the Proactivity Model. Specifically, we found that while internal and external resources that accumulated over the life course directly influenced well-being outcomes, these resources also worked through proactive adaptations. It is noteworthy that the same proactive adaptations enhanced both the psychological and social outcomes, even though the exact internal and external resources varied. In considering the relative importance of specific proactive adaptations, general planning for the future and marshaling support were shown to be the strongest predictors. We tested an alternative model with only the direct effects specified. Although there were few substantive differences in direct effects across the models, the full model with both direct and indirect effects specified fit the data significantly better. This is because proactive adaptation partially mediates the relationship between internal/external resources and well-being. Studies with only one or two waves of data may not be sensitive enough to detect the process of preserving well-being by using existing resources to invoke temporally proximate and behaviorally-oriented proactive adaptations.
Marshaling support is a key behavioral manifestation of instrumental coping in late life, facilitating the receipt of social supports that can help with specific problems faced (Kahana et al., 2009).This proactive behaviors had a consistent and strong positive effect on both QOL outcomes, reflecting the value of active help seeking in late life.
Planning for the future proved to be the second important element for maintaining good QOL in the face of stressors. This finding underscores the value of future-oriented planning behaviors in self-regulation, problem solving, and promoting successful aging (Aspinwall & Taylor, 1997). Significant benefit is derived from making positive, forward-looking discretionary plans for the future. Both of the most effective proactive adaptations (planning for discretionary activities and marshaling support) have in common a willingness to act on positive outcome expectations (Moen, Huang, Plassmann & Dentinger, 2006). The person who marshals support anticipates responsiveness by those approached to provide help. The person planning for positive future goals anticipates that their plans will come to fruition (Elavsky, McAuley, Konopack, Marquez, Hu, Jerome & Diener, 2005). This common thread also implies that future-oriented time perspectives may serve as a dispositional resource in late life (Kahana et al., 2005).
In discussing our findings, we note that sequencing of measures reflects expectations that stressors assessed at Wave 1 will have long-term and lasting effects on outcomes and adaptation processes draw from existing internal and external resources to create more temporally proximate proactivity. While the extent or level of resources an older adult may draw might be influenced by the experience of stressors we envision many of these resources to be long-term and ongoing sources of strength and support (e.g. living children). Outcomes measured four years after the assessment of stressors would likely reflect long-term impact of both stressors and of existing resources. This temporal sequencing that has been suggested in prior literature (Ouwehand et al., 2007) was confirmed in the present study.
Despite the analytic advantage of being able to isolate the temporal ordering of stressors, internal and external resources, proactive adaptations, and well-being, we recognize that the time lag between stressors, resources, and outcomes is likely to lead to conservative estimates of causal linkages. We conducted post-hoc analyses to determine the effect of more temporally proximate stressors on quality of life in W5. Not surprisingly, depression is higher for those who have experienced 3 or more social losses in the prior year (W4; relative to those who experienced 3 or more social losses at W1). However, there is no significant difference in depression scores for those who experience 0, 1, or 2 social losses respectively. Likewise, there is minimal difference in participation in social activities at W5 based on social losses at W1 versus W4. As for the other stressors, chronic illness is relatively stable over the observation period, as is its effect on depression in bivariate tests. These findings underscore both the importance and the unique opportunity to examine long-term impact of social and health stressors and how internal and external resources and proactivity may buoy quality of life. This work may spur future research that further examines the differential impact of stressors on subsequent QOL outcomes at different time points.
We also recognize that there is a potential for selective survival in our panel study, meaning those who have more resources or enact proactive behaviors effectively could have lower risk of death. Although we adjusted our estimates for observed sample selection based in part on the Wave 1 stressors (e.g. adverse health), we recognize that patterns of survival over a five-year period are complex and likely include resources and proactivity. We believe the risk of a “ceiling effect” where all of the panel study survivors have substantial resources and effectively enact proactive behaviors is still low because, even among the survivors in later waves, there is still substantial variability in these domains.
We recognize that our relatively homogenous, primarily Caucasian, retirement community dwelling sample limits generalizability of our findings. At the same time, we note that in a subsequent study of urban elders strong similarities were found in stress exposure, coping dispositions, and QOL outcomes between urban dwelling African American and Caucasian elders (Kahana, Kahana, Kercher, King, Lovegreen & Chirayath, 1999).
In summary, our research calls attention to the usefulness of simultaneously considering both outcomes and processes of successful aging (Schulz & Heckhausen, 1996; Depp & Jeste, 2009). Our findings confirm the important role of stressors posed by late-life disability, manifested in functional limitations, as threatening QOL four years after baseline, even for older adults who survive with the disability. At the same time, our study offers compelling support for the Proactivity Model of Successful Aging (Kahana & Kahana, 1996; 2003). Internal and external resources facilitate maintenance of good QOL directly, but more importantly indirectly through proactive adaptation. Recent empirical support for the Proactive Adaptation Model has been found in qualitative research focused on older adults aging with HIV disease (Emlet, Tozay & Raveis, 2011). These results are consistent with Elder’s (1994) articulation of life course theory that recognizes planful choices made by people as they interact with changing and challenging environments throughout the life course. Findings of this research also support arguments of Justice (1998) voiced in A Different Kind of Health, that older adults can use human agency in the form of proactive adaptations to find well-being despite illness.
Implications for Policy and Practice
Findings of our study support an optimistic view of old age as a period of continuing adaptability and plasticity and counteract ageist orientations that stigmatize late life (Nelson, 2002). It is now understood among mental health professionals that patient perceived stigma can interfere with willingness to marshal support and utilize mental health services (Corrigan, 2006). Empirical support for our “agency” based conceptual model of Proactive Adaptations underscores the value of patient empowerment for self-care and for active involvement of older patients in medical and mental health care (Lord & Hutchison, 2003; Tomes, 2006).
The observed value of planning ahead and of marshaling support by older adults for maintenance of psychological well-being points to the potential of educational interventions to enhance patient initiatives for communication with both health care providers and family members (Kahana & Kahana, 2003b). Such communication can facilitate marshaling support in the face of illness and social losses. Indeed, there is growing evidence of the potential efficacy of interventions that increase proactive competencies and orientations among older adults and improve future oriented anticipatory coping and self-regulation in late life (Bode, de Ridder & Bensing, 2006; Bode, de Ridder, Kuijer & Bensing, 2007). Our findings also call attention to the potential of modifiable behavioral adaptations for enhancing both the psychological and social quality of late life. This augers well for diverse mental health interventions targeting proactive adaptations among older adults.
References
- Aspinwall LG, Taylor SE. A stitch in time: self-regulation and proactive coping. Psychological Bulletin. 1997;121(3):417–436. doi: 10.1037/0033-2909.121.3.417. [DOI] [PubMed] [Google Scholar]
- Aspinwall LG. Future-oriented thinking, proactive coping, and the management of threats to health and well-being. In: Folkman S, Nathan P, editors. The Oxford Handbook of Stress, Health, and Coping. New York: Oxford University Press; 2011. pp. 334–365. [Google Scholar]
- Baltes PB, Baltes MM. Successful aging: perspectives from the behavioral sciences. New York, NY: Cambridge University Press; 1993. [Google Scholar]
- Berk RA. An introduction to sample selection bias in sociological data. American Sociological Review. 1983;48(3):386–398. [Google Scholar]
- Birren The Gerontologist. 1969 [Google Scholar]
- Blazer DG. Depression in Late Life: Review and Commentary. Journal of Lifelong Learning in Psychiatry. 2009;2(1):118–137. [Google Scholar]
- Blumenthal JA, Gullette ECD. Exercise interventions and aging: psychological and physical health benefits in older adults. In: Schaie K, Leventhal H, Willis S, editors. Effective Health Behavior in Older Adults. New York, NY: Springer Publishing Company, Inc.; 2002. pp. 157–178. [Google Scholar]
- Bode C, De Ridder DTD, Bensing JM. Preparing for aging: development, feasibility, and preliminary results of an educational program for midlife and older based on proactive coping theory. Patient Education and Counseling. 2006;61:272–278. doi: 10.1016/j.pec.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Bode C, de Ridder DTD, Kuijer RG, Bensing JM. Effects of an intervention promoting proactive coping competencies in middle and late adulthood. Gerontologist. 2007;47:42–51. doi: 10.1093/geront/47.1.42. [DOI] [PubMed] [Google Scholar]
- Bussing A, Fischer J, Ostermann T, Matthiessen PF. Reliance on God’s help as a measure of intrinsic religiosity in healthy elderly and patients with chronic diseases. Correlations with health-related quality of life? Applied Research in Quality of Life. 2009;4(1):77–90. [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Carstensen LL. Social and emotional patterns in adulthood: support for socioemotional selectivity Theory. Psychology and Aging. 1992;7(3):331–338. doi: 10.1037//0882-7974.7.3.331. [DOI] [PubMed] [Google Scholar]
- Chou KL, Chi I. Stressful events and depressive symptoms among women and men: a longitudinal study. International Journal of Aging and Human Development. 2000;51(4):275–293. doi: 10.2190/VNJC-TQ4W-6T3R-6V9K. [DOI] [PubMed] [Google Scholar]
- Clausen JA, Jones CJ. Predicting personality stability across the life span: the role of competence and work and family commitments. Journal of Adult Development. 1998;5(2):73–83. [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Corrigan PW. Impact of consumer-operated services on empowerment and recovery of people with psychiatric disorders. Psychiatry Services. 2006;57:1493–1496. doi: 10.1176/ps.2006.57.10.1493. [DOI] [PubMed] [Google Scholar]
- Darling RB. Toward a model of changing disability identities: a proposed typology and research agenda. Disability & Society. 2003;18(7):881–895. [Google Scholar]
- Depp CA, Jeste DV. Definitions and predictors of successful aging. Focus. 2009;7:137–150. doi: 10.1097/01.JGP.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- Elavsky S, McAuley E, Motl RW, Konopack JF, Marquez DX, Hu L, Jerome GJ, Diener E. Physical activity enhances long-term quality of life in older adults: efficacy, esteem, and affective influences. Annals of Behavioral Medicine. 2005;30(2):138–145. doi: 10.1207/s15324796abm3002_6. [DOI] [PubMed] [Google Scholar]
- Elder GH. Time, human agency and social change: perspectives on the life course. Social Psychology Quarterly. 1994;57(1):4–15. [Google Scholar]
- Emlet CA, Tozay S, Raveis VH. “I’m not going to die from the aids”: resilience in aging with HIV disease. The Gerontologist. 2011;51(1):101–111. doi: 10.1093/geront/gnq060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF. Health and Aging. In: Binstock RH, Georgein LK, editors. Handbook of Aging and the Social Sciences, 6th edition. Amsterdam, Netherlands: Elsevier; 2006. pp. 238–256. [Google Scholar]
- Fillenbaum GG, Smyer MA. The development, validity and reliability of the Oars Multidimensional Functional Assessment Questionnaire. Journal of Gerontology. 1981;36(4):428–434. doi: 10.1093/geronj/36.4.428. [DOI] [PubMed] [Google Scholar]
- Fitzgerald J, Gottschalk P, Moffitt R. An analysis of sample attrition in panel data. The Michigan Panel Study of Income Dynamics. Journal of Human Resources. 1998;33(2):S251–S259. [Google Scholar]
- George LK. Stress and coping. In: Johnson ML, editor. The Cambridge Handbook of Age and Aging. New York, NY: Cambridge University Press; 2005. pp. 292–300. [Google Scholar]
- Gerhardt U. Stress and stigma explanations of illness. In: Gerhardt U, Wadsworth MEJ, editors. Stress and Stigma. NY: St. Martin’s Press; 1991. pp. 161–204. [Google Scholar]
- Greene RL, Jackson JS, Neighbors HW. Mental health and help-seeking behavior. In: Jackson JS, Chatters LM, Taylor RJ, editors. Aging in Black America. Newbury Park, CA: Sage Publications; 1993. pp. 185–200. [Google Scholar]
- Greenglass E, Fiksenbaum L, Eaton J. The relationship between coping, social support, functional disability and depression in the elderly. Anxiety, Stress and Coping. 2006;19(1):15–31. [Google Scholar]
- Heckman JJ. Sample Selection bias as a specification error. Econometrica. 1979;47(1):153–161. [Google Scholar]
- Hewitt PL, Flett GL. Personality traits and the coping process. In: Zeidner M, Endler NS, editors. Handbook of Coping: Theory, Research, Applications. New York: John Wiley & Sons, Inc.; 1996. pp. 410–433. [Google Scholar]
- Irwin M, Haydari K, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159(15):1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Justice B. A Different Kind of Health: Finding Well-being Despite Illness. Houston, TX: Peak Press; 1998. [Google Scholar]
- Kahana B, Kahana E. Toward a temporal-spatial model of cumulative life stress: placing late life stress effects in life course perspective. In: Lomranz J, editor. Handbook of Aging and Mental Health: An Integrative Approach. New York: Plenum; 1998. pp. 153–178. [Google Scholar]
- Kahana E, Kahana B. Conceptual and empirical advances in understanding well-being through proactive adaptation. In: Bengtson V, editor. Adulthood and Aging: Research on Continuities and Discontinuities. New York, NY: Springer Publishing Company, Inc.; 1996. pp. 18–41. [Google Scholar]
- Kahana E, Kahana B. Successful aging among people with HIV/AIDS. Journal of Clinical Epidemiology. 2001;54:S53–S56. doi: 10.1016/s0895-4356(01)00447-4. [DOI] [PubMed] [Google Scholar]
- Kahana E, Kahana B. Contextualizing successful aging: new directions in an age-old search. In: Settersten R Jr, editor. Invitation to the Life Course. Amityville, NY: Baywood; 2003a. pp. 225–255. [Google Scholar]
- Kahana E, Kahana B. Patient proactivity enhancing doctor-patient-family communication in cancer prevention and care among the aged. Patient Education & Counseling. 2003b;2075:1–7. doi: 10.1016/s0738-3991(03)00083-1. [DOI] [PubMed] [Google Scholar]
- Kahana E, Kahana B, Kercher K. Emerging lifestyles and proactive options for successful aging. Ageing International. 2003;28(2):155–180. [Google Scholar]
- Kahana E, Kahana B, Kercher K, King C, Lovegreen L, Chirayath H. Evaluating a model of successful aging for urban African American and White elderly. In: Wykle M, editor. Serving Minority Elders in the 21st Century. New York, NY: Springer Publishing Company, Inc.; 1999. pp. 287–322. [Google Scholar]
- Kahana E, Kahana B, Wykle M, Kulle D. “Care-getting”: a missing link to completing the lifecycle in social gerontology. Journal of Family Social Work Special Issue. 2009;12(2):168–193. doi: 10.1080/10522150902874834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahana E, Kahana B, Zhang J. Motivational antecedents of preventive proactivity in late life: linking future orientation and exercise. Journal of Motivation & Emotion Special Issue: The Psychology of Future-Oriented Thinking. 2005;29(4):438–459. doi: 10.1007/s11031-006-9012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahana E, Lawrence RH, Kahana B, Kercher K, Wisniewski A, Stoller E, Tobin J, Stange K. Long-term impact of preventive proactivity on quality of life of the old-old. Psychosomatic Medicine. 2002;64(3):382–394. doi: 10.1097/00006842-200205000-00003. [DOI] [PubMed] [Google Scholar]
- Kasen S, Chen H, Sneed JR, Cohen P. Earlier stress exposure and subsequent major depression in aging women. International Journal of Geriatric Psychiatry. 2010;25:91–99. doi: 10.1002/gps.2304. [DOI] [PubMed] [Google Scholar]
- Kelley-Moore JA, Schumacher JG, Kahana E, Kahana B. When do older adults become “disabled”? Acquiring a disability identity in the process of health decline. Journal of Health & Social Behavior. 2006;47:126–141. doi: 10.1177/002214650604700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight BG, Silverstein M, McCallum TJ, Fox LS. A sociocultural stress and coping model for mental health outcomes among African-American caregivers in Southern California. Journals of Gerontology Series B: Psychological & Social Sciences. 2000;55:142–150. doi: 10.1093/geronb/55.3.p142. [DOI] [PubMed] [Google Scholar]
- Koenig HG. Religion and prevention of illness in later life. Prevention and Human Services. 1991;10(1):69–89. [Google Scholar]
- Krause N. Social relationships in late life. In: Binstock RH, George LK, editors. Handbook of Aging and the Social Sciences, 6th Edition. San Diego, CA: Academic Press; 2006. pp. 182–210. [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- Lord J, Hutchinson P. ‘Individualized support and funding: building blocks for capacity building and inclusion’. Disability and Society. 2003;18(1):71–86. [Google Scholar]
- Marquez DX, Bustamante EE, Blissmer BJ, Prohaska TR. Health promotion for successful aging. American Journal of Lifestyle Medicine. 2009;3(1):12–19. [Google Scholar]
- McAuley E, Konopack JF, Motl RW, Morris KS, Doerksen SE, Rosengren KR. Physical activity and quality of life in older adults: influence of health status and self-efficacy. Annals of Behavioral Medicine. 2006;31(1):99–103. doi: 10.1207/s15324796abm3101_14. [DOI] [PubMed] [Google Scholar]
- Meredith GE, Schewe CD. Defining Markets, Defining Moments: America’s 7 Generational Cohorts, their Shared Experiences, and Why Businesses Should Care. New York: Hungry Minds; 2002. [Google Scholar]
- Moen P, Huang QL, Plassmann V, Dentinger E. Deciding the future: do dual-earner couples plan together for retirement? American Behavioral Scientist. 2006;49(10):1422–1443. [Google Scholar]
- Nelson 2002 [Google Scholar]
- Ouwehand C, de Ridder DTD, Bensing JM. A review of successful aging models: proposing proactive coping as an important additional strategy. Clinical Psychology Review. 2007;27:873–834. doi: 10.1016/j.cpr.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22(4):337–356. [PubMed] [Google Scholar]
- Pfeiffer E. A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatric Society. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Wilson-Genderson M, Cartwright F. A two-factor model of successful aging. Journals of Gerontology Series B. 2010;65(6):671–679. doi: 10.1093/geronb/gbq051. [DOI] [PubMed] [Google Scholar]
- Pudrovska T, Schieman S, Pearlin LI, Nguyen K. The sense of mastery as a mediator and moderator in the association between economic hardship and health in late life. Journal of Aging and Health. 2005;17(5):634–660. doi: 10.1177/0898264305279874. [DOI] [PubMed] [Google Scholar]
- Rapp SR, Shumaker SA, Schmidt S, Naughton M, Anderson R. Social resourcefulness: its relationship to social support and well-being among caregivers of dementia victims. Aging & Mental Health. 1998;2(1):40–48. [Google Scholar]
- Rook KS. Gaps in social support resources in later life: an adaptational challenge in need of further research. Journal of Social & Personal Relationships. 2009;26(1):103–112. doi: 10.1177/0265407509105525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe JW, Kahn RL. Successful Aging. New York: Pantheon; 1998. [Google Scholar]
- Schulz R, Heckhausen J. A lifespan model of successful aging. American Psychologist. 1996;51(7):702–714. doi: 10.1037//0003-066x.51.7.702. [DOI] [PubMed] [Google Scholar]
- Sherman AM, Shumaker SA, Rejeski WJ, Morgan T, Applegate WB, Ettinger W. Social support, social integration, and health-related quality of life over time: results from the Fitness and Arthritis in Seniors Trial (FAST) Psychology and Health. 2006;21(4):463–480. [Google Scholar]
- Smith GC, Kohn SJ, Savage-Stevens SE, Finch JJ, Ingate R, Yeon-Ok L. The effects of interpersonal and personal agency on perceived control and psychological well-being in adulthood. The Gerontologist. 2000;40:458–468. doi: 10.1093/geront/40.4.458. [DOI] [PubMed] [Google Scholar]
- Spira M. Mapping your future—a proactive approach to aging. Journal of Gerontological Social Work. 2006;47(1–2):71–87. doi: 10.1300/J083v47n01_06. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Personal agency in the stress process. Journal of Health and Social Behavior. 2006;47(4):309–323. doi: 10.1177/002214650604700401. [DOI] [PubMed] [Google Scholar]
- Tomes N. The patient as a policy factor: a historical case study of the consumer/survivor movement in mental health. Health Affairs. 2006;25(3):720–729. doi: 10.1377/hlthaff.25.3.720. [DOI] [PubMed] [Google Scholar]
- Umberson D. Relationships between adult children and their parents: psychological consequences for both generations. Journal of Marriage and the Family. 1992;54:664–674. [Google Scholar]
- Umberson D, Williams K, Powers DA, Chen MD, Campbell AM. As good as it gets? a life course perspective on marital quality. Social Forces, B. 2005;4(1):493–512. doi: 10.1353/sof.2005.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science and Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wheaton B. The Domains and boundaries of stress concepts. In: Kaplan HB, editor. Psychosocial Stress: Perspectives on Structure, Theory, Life-course, and Methods. San Diego, California: Academic Press, Inc.; 1996. pp. 29–58. [Google Scholar]
- Williamson GM. Aging well: outlook for the 21st century. In: Snyder C, Lopez S, editors. Handbook of Positive Psychology. New York: Oxford University Press; 2005. pp. 676–686. [Google Scholar]
- Young Y, Frick KD, Phelan EA. Can successful aging and chronic illness co-exist in the same individual? a multidimensional concept of successful aging. Journal of the American Medical Directors Association. 2009;10(2):87–92. doi: 10.1016/j.jamda.2008.11.003. [DOI] [PubMed] [Google Scholar]