Abstract
Postoperative hematoma is a rare but potentially life-threatening and unpredictable complication of thyroid surgery. We report two cases of very late postoperative bleeding occurring on the 13th postoperative day in patients treated with low-molecular-weight heparin and acenocoumarol. Patient 1 was readmitted with complaints of progressive anterior neck swelling and bleeding from the cervical wound without respiratory distress. The patient had restarted therapy with Acenocoumarol associated with Nadroparin one day before. Under general anesthesia, cervical exploration allowed detection of a superficial hematoma. Patient 2 returned to our institution with subhyoid ecchymosis and moderate blood loss from the left drainage wound. The patient underwent drainage and was treated conservatively. Although most bleeding occurs within 24 hours, caution should be taken in patients on oral anticoagulants and low-molecular weight heparin and close monitoring should also be advised at home after discharge, particularly if anticoagulant therapy has restarted.
Keywords: hematoma, thyroidectomy, complications, anticoagulant therapy
Introduction
Postoperative hematoma is a rare but potentially life-threatening and unpredictable complication of thyroid surgery;1–7 in a recent territory-wide audit of 1,616 patients in 17 local hospitals, two deaths resulted from thyroidectomy with one directly related to postoperative hematoma.8 It has variably reported incidence in the literature of between 0.1% and 6.5% but in major centers is commonly reported to be approximately 1%.1,2,6,9–11
Relatively fewer studies have focused on prevention and risk factors of postoperative hemorrhage or hematoma after thyroidectomy8 and most of the authors were unable to definitively identify perioperative risk factors for the development of hematomas.7,12
Postoperative hematoma may have a multifactorial etiopathogenesis, including slipping of ligatures, reopening of previously cauterized veins, and bleeding from residual thyroid parenchyma. Among predisposing factors, retching and bucking during recovery and perioperative increased blood pressure are considered the most significant.2,4,12,13
Postoperative bleeding may be the limiting factor for outpatient thyroid surgery or early discharge from the hospital.8
While some series report that most hemorrhagic symptoms occur early in the postoperative period within 6 hours after surgery, significant delays in symptoms have also been noted by others; Burkey9 found that 60% of patients presented with symptoms beyond 6 hours.2,4,9
Anticoagulant therapy is commonly encountered in medical patients planned for surgery. In most instances, temporary perioperative discontinuation of anticoagulant therapy or in recent years “bridging therapy”, or the administration of an appropriate form of heparin while oral anticoagulation is discontinued, has been procured mainly using low-molecular weight heparin (LMWH). Performing thyroid surgery in patients under anticoagulation therapy or with coagulopathy would therefore carry a substantial but unavoidable risk of surgical wound bleeding.1
There have been no reports in the literature of bleeding after the seventh postoperative day.7 We report two cases of very late postoperative bleeding occurring on the 13th postoperative day in patients treated with LMWH (Nadroparin and Enoxaparin) and acenocoumarol.
Clinical Cases
Case 1
A 73-year-old Caucasian man presented to our department for surgical treatment of toxic multinodular goiter, recently diagnosed during a hospitalization for atrial fibrillation. He was also affected by hypertensive cardiopathy and type 2 diabetes mellitus. He was treated with oral anticoagulant (acenocoumarol) and methimazole. No symptoms, including dysphagia, dyspnoea, or dysphonia, were associated. Physical examination revealed an indolent subhyoid swelling. Pre-operative neck ultrasound examination showed an enlarged thyroid gland with a retrosternal left lobe and many nodules; thyroid volume was 52 mL. A thyroid scintigraphy with 99mTc demonstrated diffuse cold areas and a hot peri-isthmic area. Oral anticoagulant was suspended and LMWH was administered. After a few days, as the coagulation tests returned to the normal range, a total thyroidectomy was performed. Parathyroid glands and recurrent nerves were recognized and preserved. Immediate postoperative course was uneventful; suction drainages were removed on the 6th postoperative day and the patient was discharged the same day in good general condition. AntiXa test was not performed. At discharge, serum calcium was 8.8 mg/dL (normal range (nr): 8.6–10.2), serum phosphorus was 3.5 mg/dL (nr: 2.7–4.5). The delay in discharge was caused by the use of LMWH and the amount of drainage (in our institution patients are normally discharged in the second postoperative day). At home, he continued his anticoagulant treatment with twice daily subcutaneous injection of Nadroparin, 5700 anti-Xa IU/mL (Seleparina®, Italfarmaco Spa, Cinisello Balsamo, Italy) as prescribed by the cardiologist. Histopathological examination confirmed the diagnosis of multinodular goiter.
After 7 days of relative wellness, on the 13th postoperative day, he was readmitted as an emergency with complaints of progressive anterior neck swelling and bleeding from the cervical wound without respiratory distress. Vigorous coughing or sneezing or other acute reasons for hemorrhage were not reported by the patient. The patient had restarted therapy with Acenocoumarol associated with Nadroparin the previous day. Blood tests showed that haemoglobin level (15.1 gr/dL [normal range (nr): 13.0–17.5]) and platelet count (nr: 157 × −103/μL [150–450]) were in the normal range, while partial thromboplastin PT (1.25 INR [nr: <1.20]) and activated partial thromboplastin time (aPTT) were moderately increased (34 sec [nr: 20–32]). After a short period of close observation during which the wound continued to bleed and the neck swelling slowly increased, emergency surgery was scheduled on the same day.
Under general anesthesia, cervical exploration allowed detection of a superficial hematoma. Following the removal of several clots, the source of bleeding was identified on the anterior surface of strap muscles and appeared as a diffuse oozing hemorrhage. Deeper exploration by opening the cervical linea alba was also performed, but no hematoma was found. Since application of hemostatic stitches was itself source of further bleeding, hemostasis was obtained using both electrocautery and patches of fibrinogen-thrombin coated collagen fleece (TachoSil®, Takeda, Zurich, Switzerland) covering the entire bleeding surface. Two drains were left in the thyroid bed and in the pre-muscular subcutaneous space.
Anticoagulant medication was restarted 12 hours after surgery at lowest dose (twice daily subcutaneous injection of nadroparin, 3800 anti-Xa IU). Both drains were removed on 4th postoperative day and patient was discharged 6 days after surgery in good condition. After 7 days, he restarted Acenocoumarol in agreement with the indications of the cardiologist and checking the values of PT. At 14-month follow-up, he is well and has no other problems related with the previous thyroidectomy.
Case 2
A 68-year-old Caucasian woman with a history of paroxysmal atrial fibrillation (treated with oral anticoagulant), angina pectoris, and hypertension presented to our department for recent finding of indolent subhyoid swelling and mild disphagia. Ultrasound examination showed an enlarged thyroid gland with a retrosternal left lobe and many round hypoechoic nodules; thyroid volume was 56 mL. Blood tests revealed normal thyroid hormones. With these findings diagnosis of retrosternal multinodular euthyroid goiter was made. The patient substituted oral anticoagulant (Acenocoumarol) with LMWH (Enoxaparin 6.000 UI aXa/die). When a normal PT was achieved, she underwent total thyroidectomy. Parathyroid glands and recurrent nerves were recognized and preserved as usual. Postoperative course was uneventful apart from a transient relapse of atrial fibrillation occurred 2 days after surgery, which was successfully managed with oral intake of antiarrhythmic agent (propafenone). On 5th postoperative day, suction drains were removed and the patient was discharged in good general condition. AntiXa test was not performed. At discharge, serum calcium was 8.7 mg/dL (normal range (nr): 8.6–10.2), serum phosphorus was 3.7 mg/dL (nr: 2.7–4.5). The delay in discharge was caused by the relapse of atrial fibrillation, the use of LMWH, and the amount of drainage.
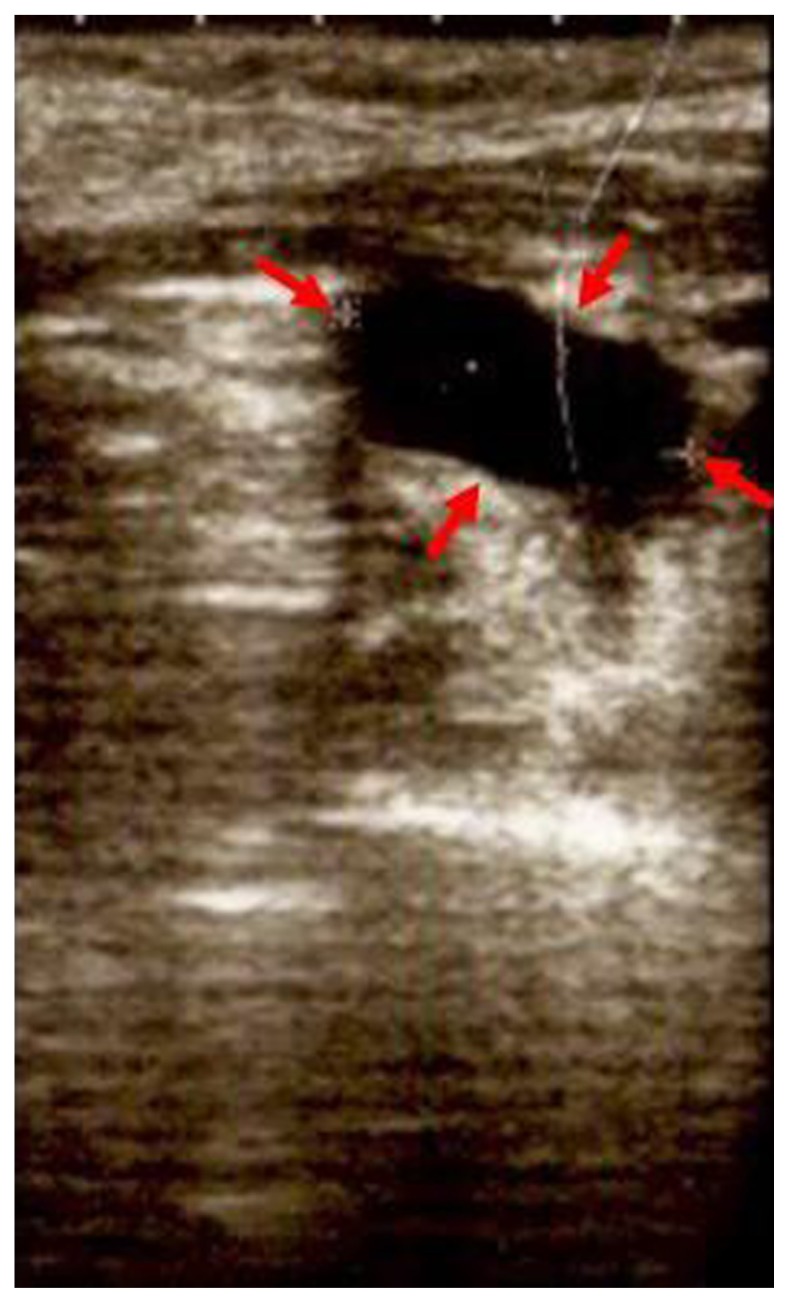
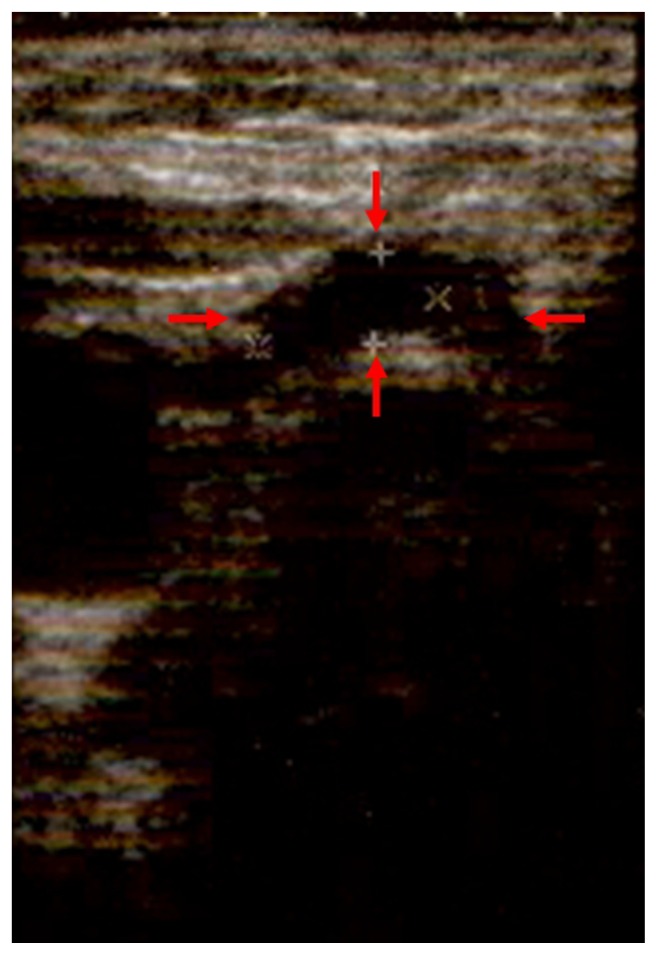
On the 13th postoperative day, the patient was readmitted complaining of subhyoid ecchymosis and moderate blood loss from the left drainage wound in keeping with postoperative neck hematoma. Vigorous coughing or sneezing or other acute reasons for hemorrhage were not reported by the patient. A subsequent ultrasound examination demonstrated that the blood collection was located deeply, beneath the strap muscles (Figs. 1 and 2). Blood tests showed that hemoglobin level, platelet count, PT, and aPTT were in the normal range. Since the hematoma appeared to be stable, after an immediate drainage at the bedside of the patient, conservative management with tranexamic acid medications was effectively carried out. The cervical wound was checked daily until complete healing, and the patient was discharged on the 18th postoperative day in good condition. After 7 days, she restarted Acenocoumarol in agreement with the indications of the cardiologist and checking the values of PT. At her 13-month follow-up, she is well and with no problems related with the previous thyroidectomy.
Figure 1.
Ultrasound examination demonstrated that the blood collection was located deeply, beneath the strap muscles (left).
Figure 2.
Ultrasound examination demonstrated that the blood collection was located deeply, beneath the strap muscles (right). secondary to postoperative bleeding could be prevented by a 24-hour hospitalization compared with a 6-hour observation5,9.
Discussion
Hematoma following thyroid surgery is a rare but potentially life-threatening complication, with a reported rate of 0.1% to 4.7%.3,6,14
Meticulous hemostastic techniques are necessary to prevent this complication; Ligasure, Harmonic Scalpel, and hemostatic agents are currently available for surgeons.2,15
In the last several years, an increased demand for ambulatory and 1-day surgery thyroidectomy has emerged.2 Postoperative bleeding is one of the limiting factors that precludes early discharge.10
It is generally difficult to predict which patients are at risk for developing hematoma after thyroid surgery.2,9 Male gender, hyperthyroidism, intrathoracic goiters, and re-operative surgery were associated with a higher risk of bleeding.2,7–9,16–18
Some authors suggest that in most cases, bleeding was likely due to post-surgical hypertension. Thus, very closely monitoring of pressure during the first 24 hours after surgery and prompt treatment of all manifestation of hypertension with appropriate drugs are recommended.2 It has also been associated with the administration of anticoagulants or coagulation alterations, ie, hemophilia, von Willebrand’s disease, and chronic renal failure.2
Simultaneous thyroid surgery and coagulopathy is underreported in the medical literature.1 In most cases, anticoagulation therapy is temporarily suspended in the perioperative period. A shift to LMWH is commonly practice. Heparin is easily monitored, and usually stops 8–10 hours before surgery.1,8
The most intense postoperative monitoring is necessary during the first six hours, but hematomas occurring after are not rare.2 Surgeons should be aware that neck hematoma may develop later than 24 hours following thyroidectomy, particularly in patients who are being anticoagulated.2
In a study by Promberger,10 80.6% of postoperative bleeds became symptomatic within 6 h and 88.0% within 12 hours after the operation; only 10 (0.03%) patients demonstrated signs of bleeding after 24 hour. Less than half of the symptomatic hematomas in the study of Burkey9 presented within 6 hours of initial operation, and 20% actually presented beyond 24 hours. In a decision analysis with historical outcome data, Schwartz et al19 predicted that for every 100,000 thyroidectomies performed, 94 deaths
Our clinical cases were very interesting. Late bleeding has never been described in the literature since most bleeding occurs within 24–48 hours after surgery. In our patients, the reason for the bleeding is not clear, but we believe that oral anticoagulants and LMWH has been the most important factors. Since most surgeries occur in one day surgery with faster discharge, these clinical cases are very important. The bleeding occurred at home in a period in which such complication was unpredictable; fortunately, timely treatment led to a resolution without further consequences even if bleedings appearing so late have slower evolution. Additionally, scar establishment may have to significantly reduce the dead space in which the blood may collect. One patient had recently restarted therapy with acenocoumarol associated to nadroparin and the PT and PTT were slightly altered at the time of surgery, which was the most important risk factor present (but male sex, hyperthyroidism, retrosternal goiter, and hypertension were also factors). The other patient was treated with Enoxaparin and PT and PTT were in the normal range. Two other risk factors (retrosternal goiter and hypertension) were present in association to anticoagulant therapy. In this case, the hematoma was less extensive and immediate drainage at the bedside was sufficient to solve the problem together with close monitoring during the following days. For these reasons, we think that in patients in therapy with oral anticoagulants and LMWH early discharge is not recommended and despite the current trends in the majority of patients a longer hospitalization give greater security to the patient and the surgeon.
We believe that, although most bleeding occurs within 24 hours, caution should be taken in patients on oral anticoagulants, LMWH, and antiplatelet treatments and close monitoring should also be advised at home after discharge, particularly if anticoagulant therapy had just restarted.
Footnotes
Author Contributions
Wrote the first draft of the manuscript: PGC, EE, FM. Contributed to the writing of the manuscript: GP, MB, MP. Agree with manuscript results and conclusions: PGC, MB, MP, AN. Jointly developed the structure and arguments for the paper: PGC, EE, FM, GP. Made critical revisions and approved final version: PGC, EE, FM, AN. All authors reviewed and approved of the final manuscript.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication the author has provided signed confirmation of compliance with ethical and legal obligations including but not limited to compliance with ICMJE authorship and competing interests guidelines, that the article is neither under consideration for publication nor published elsewhere, of their compliance with legal and ethical guidelines concerning human and animal research participants (if applicable), and that permission has been obtained for reproduction of any copyrighted material. This article was subject to blind, independent, expert peer review. The reviewers reported no competing interests. Written consent was obtained from the patients to reproduce information or photographs appearing in this work.
Funding
Author(s) disclose no funding sources.
References
- 1.Abboud B, Sleilaty G, Braidy C, Melkane A, Nasr F. Thyroidectomy in patients at high-risk of bleeding: can it be safely performed? Minerva Chir. 2009;64:565–71. [PubMed] [Google Scholar]
- 2.Calò PG, Pisano G, Piga G, et al. Postoperative hematoma after thyroid surgery. Incidence and risk factors in our experience. Ann Ital Chir. 2010;81:343–7. [PubMed] [Google Scholar]
- 3.Chin CJ, Franklin JH, Turner B, Sowerby L, Fung K, Yoo JH. Ketorolac in Thyroid Surgery: Quantifying the Risk of Hematoma. J Otolaryngol Head Neck Surg. 2011;40:196–9. [PubMed] [Google Scholar]
- 4.Harding J, Sebag F, Sierra M, Palazzo FF, Henry JF. Thyroid Surgery: post-operative hematoma—prevention and treatment. Langenbecks Arch Surg. 2006;391:169–73. doi: 10.1007/s00423-006-0028-6. [DOI] [PubMed] [Google Scholar]
- 5.Leyre P, Desurmont T, Lacoste L, et al. Does the risk of compressive hematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg. 2008;393:733–7. doi: 10.1007/s00423-008-0362-y. [DOI] [PubMed] [Google Scholar]
- 6.Morton RP, Mak V, Moss D, Ahmad Z, Sevao J. Risk of bleeding after thyroid surgery: matched pairs analysis. J Laryngol Otol. 2012;126:285–8. doi: 10.1017/S0022215111001460. [DOI] [PubMed] [Google Scholar]
- 7.Rosenbaum MA, Haridas M, McHenry CR. Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg. 2008;195:339–43. doi: 10.1016/j.amjsurg.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Lang BHH, Yih PCL, Lo CY. A review of risk factors and timing for post-operative hematoma after thyroidectomy: Is outpatient thyroidectomy really safe? World J Surg. 2012;36:2497–502. doi: 10.1007/s00268-012-1682-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burkey SH, Van Heerden JA, Thompson GB, Grant CS, Schleck CD, Farley DR. Reexploration for symptomatic hematomas after cervical exploration. Surgery. 2001;130:914–20. doi: 10.1067/msy.2001.118384. [DOI] [PubMed] [Google Scholar]
- 10.Promberger R, Ott J, Kober F, et al. Risk factors for postoperative bleeding after thyroid surgery. Br J Surg. 2012;99:373–9. doi: 10.1002/bjs.7824. [DOI] [PubMed] [Google Scholar]
- 11.Shaha AR, Jaffe BM. Practical management of post-thyroidectomy hematoma. J Surg Oncol. 1994;57:235–8. doi: 10.1002/jso.2930570406. [DOI] [PubMed] [Google Scholar]
- 12.Bononi M, Bonapasta SA, Vari A, et al. Incidence and circumstances of cervical hematoma complicating thyroidectomy and its relationship to post-operative vomiting. Head Neck. 2010;32:1173–7. doi: 10.1002/hed.21313. [DOI] [PubMed] [Google Scholar]
- 13.Lee HS, Lee BJ, Kim SW, et al. Patterns of post-thyroidectomy hemorrhage. Clin Exp Otorhinolaryngol. 2009;2:72–7. doi: 10.3342/ceo.2009.2.2.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbas G, Dubner S, Heller KS. Re-operation for bleeding after thyroidectomy and parathyroidectomy. Head Neck. 2001;23:544–6. doi: 10.1002/hed.1076. [DOI] [PubMed] [Google Scholar]
- 15.Calò PG, Pisano G, Medas F, Tatti A, Tuveri M, Nicolosi A. The use of the harmonic scalpel in thyroid surgery. Our experience. Ann Ital Chir. 2012;83:7–12. [PubMed] [Google Scholar]
- 16.Calò PG, Pisano G, Medas F, Tatti A, Tuveri M, Nicolosi A. Risk factors in reoperative thyroid surgery for recurrent goitre. G Chir. 2012;33:335–8. [PubMed] [Google Scholar]
- 17.Calò PG, Tatti A, Medas F, Petruzzo P, Pisano G, Nicolosi A. Forgotten goiter. Our experience and a review of the literature. Ann Ital Chir. 2012;83:487–90. [PubMed] [Google Scholar]
- 18.Godballe C, Madsen AR, Pedersen HB, et al. Post-thyroidectomy hemorrhage: a national study of patients treated at the Danish departments of ENT Head and Neck Surgery. Eur Arch Otorhinolaryngol. 2009;266:1945–52. doi: 10.1007/s00405-009-0949-0. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz AE, Clark OH, Ituarte P, Lo Gerfo P. Therapeutic Controversy: Thyroid surgery—the choice. J Clin Endocrinol Metab. 1998;83:1097–105. doi: 10.1210/jcem.83.4.4740-1. [DOI] [PubMed] [Google Scholar]