Abstract
Objectives
The objectives of our large observational study were to describe the prevalence of cardiac and noncardiac comorbidities in a community-based population of patients hospitalized with acute myocardial infarction (AMI) at all medical centers in central Massachusetts, and to examine whether multiple comorbidities were associated with in-hospital death rates and hospital length of stay.
Methods
The study sample consisted of 2,972 patients hospitalized with AMI at all eleven greater Worcester medical centers in central Massachusetts during the three study years of 2003, 2005, and 2007.
Results
The average age of this hospitalized population was 71 years, 55% were men, 93% were Caucasian, and approximately one third had developed an ST segment elevation AMI during the years under study. Hypertension (75%) was the most common cardiac condition identified in patients hospitalized with AMI whereas renal disease (22%) was the most common noncardiac comorbidity diagnosed in this study population. Approximately one in every four hospitalized patients had any four or more of the seven cardiac conditions examined, while one in 13 had any three or more of the five noncardiac conditions studied. Patients with four or more cardiac comorbidities were more than twice as likely to have died during hospitalization and have a prolonged hospital length of stay, compared to those without any cardiac comorbidities. Patients with three or more noncardiac comorbidities had markedly increased odds of dying during hospitalization and having a prolonged hospital stay compared to those with no noncardiac comorbidities previously diagnosed.
Conclusion
Our findings highlight the need for additional contemporary data to improve the short-term outcomes of patients hospitalized with AMI and multiple concurrent medical illnesses.
Keywords: population-based study, chronic conditions, acute coronary syndrome
Introduction
More than 140 million Americans have one or more chronic conditions.1 The number of Americans living with multiple chronic conditions will continue to increase as the population ages and fewer patients die from acute manifestations of cardiac and noncardiac conditions.2–4 In general, and among patients with cardiovascular disease, the presence of multiple comorbidities has been associated with increased mortality, greater utilization of health care resources, and larger health care expenditures.5,6
Coronary heart disease (CHD) is the leading cause of death in Americans and is associated with a high burden of comorbidities that play an important role in disease progression and response to treatment.7–9 Although multiple cardiac comorbidities have been associated with adverse post-discharge survival rates in patients hospitalized with acute myocardial infarction (AMI),10 important in-hospital events, including mortality, length of stay, and use of different treatment approaches, have not been extensively studied in patients with AMI according to the presence of multiple cardiac or noncardiac comorbidities.11 The relative lack of data on the magnitude and impact of multiple comorbidities may limit our ability to further improve the targeting of evidence-based therapeutics, thereby improving the outcomes of patients hospitalized with AMI.
The primary objective of our study was to describe the prevalence of cardiac and noncardiac comorbidities in a community-based population of patients hospitalized at all medical centers in central Massachusetts with AMI in 2003, 2005, and 2007. A secondary study objective was to examine whether the presence of multiple cardiac and noncardiac comorbidities was associated with the use of various treatment approaches, in-hospital mortality, and hospital length of stay in patients hospitalized with AMI during the years under study. Data from the population-based Worcester Heart Attack Study were utilized for this investigation.12–14
Methods
The Worcester Heart Attack Study is an ongoing population-based investigation examining long-term trends in the incidence, hospital, and post discharge case-fatality rates of AMI in residents of the Worcester, MA, metropolitan area hospitalized at all greater Worcester medical centers on an approximate biennial basis between 1975 and 2007.12–14 In brief, computerized printouts of patients discharged from all greater Worcester hospitals with possible AMI (International Classification of Disease, Ninth Revision: [ICD 9] codes: 410–414, 786.5) were identified. Cases of possible AMI were independently validated using predefined criteria for AMI. These criteria included a suggestive clinical history, serum enzyme level elevations in excess of the normal range at each participating hospital, and serial electrocardiographic findings during hospitalization consistent with the presence of AMI. Patients who satisfied at least two of these three criteria, and were residents of the Worcester metropolitan area, were included.12–14
The present study population consisted of adult men and women of all ages who were hospitalized with AMI in 2003, 2005, and 2007 at any of eleven medical centers in the Worcester metropolitan area. As mentioned previously, we carry out surveillance of this population on a biennial, not an annual, basis. We restricted our study sample to this relatively recent period because of the availability of data on several important measures of cardiac and noncardiac comorbidity and to provide relatively contemporary insights into the prevalence and impact of various comorbidities in this patient population. This observational study was approved by the Office for the Protection of Human Subjects in Research and Institutional Review Board at the University of Massachusetts Medical School.
Data collection
Trained nurses and physicians abstracted information on patients’ demographic characteristics, medical history, clinical data, and treatment practices through the review of hospital medical records of patients with independently confirmed AMI. These factors included patients’ history of previously diagnosed comorbidities and AMI order (initial versus prior) and type (ST-elevation myocardial infarction [STEMI] versus non-ST-elevation myocardial infarction [NSTEMI]).15,16 Data on treatment practices during hospitalization included the prescribing of six effective cardiac medications (angiotensin converting inhibitors/angiotensin receptor blockers, anticoagulants, lipid lowering agents, beta blockers, aspirin, and thrombolytics) and two coronary interventional procedures (coronary artery bypass grafting [CABG], and percutaneous coronary intervention [PCI]). The main outcomes of interest were in-hospital case-fatality rates (CFRs) and hospital length of stay.
Comorbid conditions that had been previously diagnosed in this patient population were categorized into cardiac and noncardiac comorbidities. For purposes of the present analysis we considered seven cardiac comorbidities, including atrial fibrillation, CHD (prior angina pectoris, CHD, myocardial infarction [MI], CABG, or PCI), diabetes, heart failure, hypertension, peripheral vascular disease, and stroke. The five noncardiac comorbidities that we examined included anemia, depression, cancer, chronic obstructive pulmonary disease (COPD), and chronic kidney disease (CKD). We selected and categorized these cardiac and noncardiac comorbidities based on a review of the prior literature, their established associations with either the development of, or prognosis after, AMI, and their relative frequency in this patient population.10,17,18
Data analysis
We estimated the overall prevalence of individual comorbidities and multiple cardiac and noncardiac comorbidities in this patient population. We further categorized cardiac comorbidities (0, 1, 2, 3, and ≥4), and noncardiac comorbidities (0, 1, 2, and ≥3) according to the number of comorbid conditions previously diagnosed based on the review of information contained in hospital medical records. Differences in patient demographic and clinical characteristics, cardiac medications and interventional procedures received, and hospital CFRs and length of stay (LOS) according to number of cardiac or noncardiac comorbid conditions were examined using the Analysis of Variance test for continuous variables and the chi-square test for categorical variables.
Multivariable logistic regression analyses were performed to examine the association between number of cardiac and noncardiac comorbid conditions and our principal study outcomes of in-hospital mortality (dead versus alive) and LOS (>3 versus ≤3 days), while adjusting for several potential confounding variables. These variables included patient age, sex, race (white versus non-white), marital status, year of hospitalization (2003, 2005, or 2007), and AMI order and type. Sequentially, we began our multivariable adjustment including only cardiac or only noncardiac comorbidities in separate models. We then placed these cardiac and noncardiac factors in a model concurrently to examine associations with our principal hospital outcomes. Multivariable adjusted odds ratios (OR) and 95% confidence intervals (CI) for the risk of dying during hospitalization or having a prolonged hospital stay according to the number of cardiac and noncardiac comorbidities present were calculated in a standard manner. In addition, we examined the relations between various combinations (ie, co-occurrence of specific conditions) of multiple cardiac or noncardiac comorbidities and hospital CFRs and LOS.
Results
Patient characteristics
The study sample consisted of 2,972 residents of the Worcester metropolitan area hospitalized with independently validated AMI at all greater Worcester medical centers during 2003, 2005, and 2007. The average age of this patient population was 70.8 years, 55.1% were men, and most were white (92.5%). About one-third of patients presented with a STEMI (31.6%), almost two-thirds had not experienced a prior AMI (64.5%), and 9.7% died during their acute hospitalization.
In examining differences in selected demographic and clinical characteristics in relation to number of diagnosed cardiac or noncardiac comorbidities (Table 1), patients with multiple cardiac or noncardiac conditions were significantly more likely to be older, female, unmarried, have a history of prior MI, and present with a NSTEMI. These patients were also more likely to have presented with higher serum glucose levels, but lower estimated glomerular filtration rate (eGFR) and serum cholesterol levels, at the time of hospital admission than patients with fewer or no comorbid conditions.
Table 1.
Characteristics of the study population according to number of noncardiac and cardiac comorbidities
| Characteristic | Cardiac comorbidities
|
Noncardiac comorbidities
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 (N = 382) | 1 (N = 587) | 2 (N = 7I8) | 3 (N = 555) | ≥4 (N = 730) | P-value | 0 (N = 1,332) | 1 (N = 95l) | 2(N = 463) | ≥3 (N = 226) | P-value | |
| Age (mean, years) | 59.8 | 65.5 | 73.0 | 74.3 | 76.2 | <0.00l | 66.5 | 73.0 | 75.8 | 77.3 | <0.00l |
| Male (%) | 72.5 | 58.3 | 51.4 | 52.4 | 49.3 | <0.00l | 62.3 | 52.6 | 44.1 | 46.5 | <0.00l |
| White (%) | 94.1 | 92.4 | 94.2 | 92.3 | 90.4 | 0.073 | 92.5 | 92.9 | 92.2 | 92.2 | 0.968 |
| Married (%) | 61.4 | 57.9 | 51.3 | 47.8 | 45.1 | <0.00l | 58.5 | 49.2 | 44.6 | 37.2 | <0.00l |
| ST-segment myocardial infarction (%) | 55.8 | 42.1 | 32.9 | 23.8 | 15.2 | <0.00l | 39.0 | 29.0 | 23.1 | 15.9 | <0.00l |
| Initial myocardial infarction (%) | 100.0 | 90.8 | 66.4 | 49.2 | 34.4 | <0.00l | 73.6 | 62.7 | 51.2 | 45.1 | <0.00l |
| Serum cholesterol* (mean, mg/dL) | 191.8 | 178.5 | 166.0 | 159.6 | 156.5 | <0.00l | 176.4 | 170.5 | 157.3 | 151.3 | <0.00l |
| Serum glucose* (mean, mg/dL) | 136.2 | 149.1 | 166.1 | 186.8 | 208.6 | <0.00l | 163.4 | 177.2 | 185.2 | 190.3 | <0.00l |
| Estimated GFR* (mean, mL/min/1.73 m2) | 76.0 | 68.9 | 60.0 | 56.3 | 44.9 | <0.00l | 68.8 | 57.5 | 45.0 | 40.2 | <0.00l |
| Systolic blood pressure* (mean, mmHg) | 138.7 | 142.7 | 141.9 | 142.3 | 139.5 | 0.175 | 143.2 | 140.4 | 138.8 | 137.5 | 0.013 |
| Diastolic blood pressure* (mean, mmHg) | 81.0 | 80.5 | 76.5 | 74.7 | 71.1 | <0.00l | 79.6 | 75.0 | 71.7 | 70.5 | <0.00l |
Note:
At hospital admission.
Abbreviation: GFR, glomerular filtration rate.
Prevalence of previously diagnosed cardiac and noncardiac comorbidities
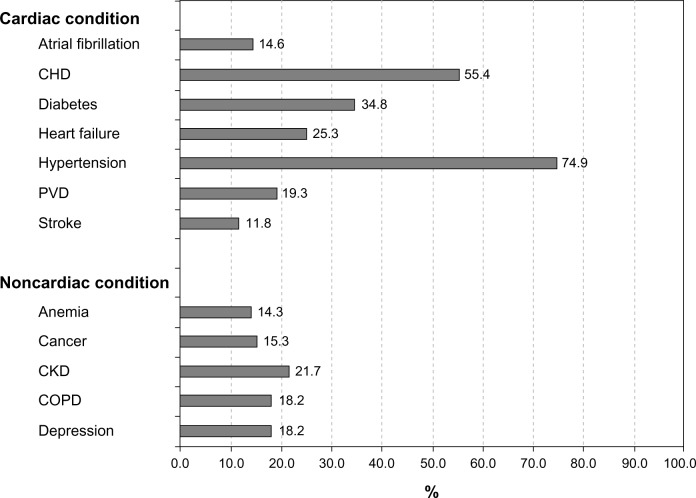
Among all comorbid conditions previously diagnosed at the time of their hospitalization for AMI, hypertension (74.9%) was the cardiac condition most commonly identified, whereas chronic kidney disease (21.7%) was the most common noncardiac comorbidity diagnosed in this patient population (Figure 1).
Figure 1.
Prevalence of cardiac and noncardiac comorbidities.
Abbreviations: CHD, coronary heart disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; PVD, peripheral vascular disease.
In our study population, 12.9% of patients had none of the cardiac comorbidities examined, 19.8% had any one, 24.2% had any two, 18.7% had any three, and 24.6% had any four or more of the cardiac conditions examined. In terms of noncardiac comorbidities, 44.8% of patients had none, 32.0% had any one, 15.6% had any two, and 7.6% had any three or more of the noncardiac conditions examined. Among all patients, 9.6% had neither of the cardiac nor the noncardiac comorbidities studied, while 4.3% had ≥4 cardiac and ≥3 noncardiac comorbidities.
Receipt of cardiac medications and interventional procedures and prior comorbidities
On average, patients received 4.2 of the six cardiac medications (angiotensin converting inhibitors/angiotensin receptor blockers, anticoagulants, lipid lowering agents, beta blockers, aspirin, and thrombolytics) examined during their acute index hospitalization; 79.1% of patients received at least four of these effective cardiac medications.
Each of these cardiac medications, with the exception of thrombolytics, was prescribed to three-quarters or more of patients hospitalized with AMI (Table 2). After multivariable adjustment, patients with two noncardiac (OR = 0.72, 95% CI = 0.53, 0.97) or three or more noncardiac (OR = 0.62, 95% CI = 0.42, 0.92) comorbidities were significantly less likely to have received at least four of the effective cardiac medications, compared with patients without any previously diagnosed noncardiac comorbidity; however, no significant differences in treatment practices were found according to the number of cardiac comorbidities previously diagnosed in this population.
Table 2.
Receipt of cardiac medications and interventional procedures during hospitalization according to number of noncardiac and cardiac comorbidities
| Cardiac comorbidities
|
Noncardiac comorbidities
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 (N = 382) | 1 (N = 587) | 2 (N = 7I8) | 3 (N = 555) | ≥4 (N = 730) | P-value | 0 (N = 1,332) | 1 (N = 95l) | 2 (N = 463) | ≥3 (N = 226) | P-value | |
| Medication (%) | |||||||||||
| ACE-l/ARBs | 68.1 | 75.1 | 70.6 | 75.5 | 74.4 | 0.031 | 74.9 | 71.9 | 70.0 | 72.6 | 0.156 |
| Anticoagulants | 82.5 | 84.5 | 83.1 | 83.6 | 82.7 | 0.908 | 83.6 | 84.2 | 82.5 | 79.6 | 0.387 |
| Aspirin | 97.1 | 96.3 | 93.9 | 91.5 | 92.6 | <0.00l | 96.1 | 93.2 | 91.6 | 90.3 | <0.00l |
| Beta blockers | 93.2 | 94.9 | 92.3 | 93.0 | 93.0 | 0.466 | 94.0 | 93.7 | 90.9 | 91.6 | 0.094 |
| Lipid lowering | 80.4 | 79.6 | 77.0 | 76.8 | 75.1 | 0.203 | 81.2 | 75.4 | 71.9 | 74.8 | <0.00l |
| Thrombolytics | 5.2 | 2.4 | 1.3 | 1.3 | 0.8 | <0.00l | 3.1 | 0.9 | 1.1 | 0.4 | <0.00l |
| ≥3 medications | 93.2 | 92.7 | 91.1 | 91.7 | 92.2 | 0.733 | 93.4 | 91.3 | 90.1 | 91.6 | 0.085 |
| ≥4 medications | 81.4 | 80.4 | 77.7 | 79.6 | 77.7 | 0.452 | 82.2 | 78.2 | 74.5 | 73.5 | <0.00l |
| Procedures (%) | |||||||||||
| Percutaneous coronary intervention | 69.6 | 61.8 | 46.4 | 39.6 | 27.3 | <0.00l | 60.6 | 41.4 | 29.2 | 19.9 | <0.00l |
| CABG surgery | 4.7 | 6.8 | 6.4 | 6.8 | 2.9 | 0.004 | 6.2 | 6.3 | 3.2 | 2.7 | 0.015 |
Abbreviations: ACE-I, angiotensin converting inhibitors; ARBs, angiotensin receptor blockers; CABG, coronary artery bypass grafting.
Nearly one-half of patients underwent a PCI and 5.5% underwent CABG surgery during their index hospitalization. Patients were considerably less likely to have undergone a PCI with increasing cardiac and noncardiac comorbidity burden (Table 2). After multivariable adjustment, patients with four or more cardiac comorbidities (OR = 0.59, 95% CI = 0.41, 0.86) or patients with one noncardiac (OR = 0.67, 95% CI = 0.55, 0.82), two noncardiac (OR = 0.52, 95% CI = 0.40, 0.69), or three or more noncardiac comorbidities (OR = 0.35, 95% CI = 0.23, 0.52) were significantly less likely to have undergone a PCI, compared with patients without any previously diagnosed cardiac or noncardiac comorbidity; however, no significant associations were observed between the likelihood of undergoing CABG surgery according to the number of comorbidities present at the time of hospitalization for AMI.
Hospital death rates and length of stay and prior comorbidities
Having multiple cardiac or noncardiac comorbidities was significantly associated with higher hospital CFRs and longer LOS. There was a dose-response relationship between number of cardiac or noncardiac comorbidities and in-hospital death rates and LOS (Table 3, P for trend <0.001). The hospital CFR increased from 3.7% to 14.2% as the number of cardiac comorbidities increased from zero to four or more conditions; similarly, the hospital CFR increased from 6.9% to 15.9% as the number of noncardiac comorbidities increased from zero to three or more conditions. Approximately two-thirds of patients with four or more cardiac comorbidities had a LOS >3 days, compared with 39.8% of patients without any cardiac comorbidity. Similarly, 70.7% of patients with three or more noncardiac comorbidities had a LOS >3 days compared to 47.8% of patients without any noncardiac comorbidity (Table 3).
Table 3.
Hospital CFRs and length of stay according to number of noncardiac and cardiac comorbidities
| Cardiac comorbidities
|
Noncardiac comorbidities
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 (N = 382) | 1 (N = 587) | 2 (N = 718) | 3 (N = 555) | ≥ 4 (N = 730) | P for trend | 0 (N = 1332) | 1 (N = 951) | 2 (N = 463) | ≥3 (N = 226) | P for trend | |
| Hospital CFR (%) | 3.7 | 6.1 | 10.6 | 11.2 | 14.2 | <0.00l | 6.9 | 10.1 | 14.7 | 15.9 | <0.00l |
| Length of stay | |||||||||||
| Mean (days) | 4.2 | 4.7 | 5.3 | 5.6 | 6.5 | <0.00l | 4.7 | 5.6 | 6.4 | 6.8 | <0.00l |
| >3 days (%) | 39.8 | 48.0 | 55.7 | 60.8 | 68.1 | <0.00l | 47.8 | 58.3 | 68.6 | 70.7 | <0.00l |
Abbreviation: CFRs, case-fatality rates.
In multivariable logistic regression models adjusting for the number of cardiac and noncardiac comorbidities concurrently, patients with any two, three, or four or more cardiac comorbidities were two to three times as likely to have died during hospitalization, compared with those with no cardiac comorbidities (Table 4). Patients with two noncardiac (OR = 1.63, 95% CI = 1.12, 2.37), or three or more noncardiac comorbidities (OR = 1.76, 95% CI = 1.11, 2.78) were also more likely to have died during hospitalization compared with those without any noncardiac comorbidities. In addition, we found that patients with any two, three, or four or more cardiac comorbidities were at increased odds of a prolonged hospital LOS (>3 days) compared with those with no cardiac comorbidities (Table 4). Patients with any one, two, or three or more noncardiac comorbidities were also significantly more likely to have a prolonged hospital course compared with those without any noncardiac comorbidities (Table 4).
Table 4.
Multivariable adjusted association† between frequency of noncardiac and cardiac comorbidities and hospital case-fatality (CF) and length of stay*
| Variable | OR (95% CI) | OR (95% CI) | OR (95% CI)# |
|---|---|---|---|
| Hospital CF | |||
| Cardiac comorbidity | |||
| 0 | 1.00 | 1.00 | |
| 1 | 1.36 (0.69, 2.67) | 1.31 (0.67, 2.57) | |
| 2 | 2.13 (1.12, 4.04) | 2.00 (1.05, 3.82) | |
| 3 | 2.34 (1.20, 4.57) | 2.14 (1.10, 4.20) | |
| ≥4 | 3.35 (1.73, 6.48) | 2.80 (1.43, 5.49) | |
| Noncardiac comorbidity | |||
| 0 | 1.00 | 1.00 | |
| 1 | 1.30 (0.94, 1.80) | 1.20 (0.86, 1.67) | |
| 2 | 1.86 (1.29, 2.69) | 1.63 (1.12, 2.37) | |
| ≥3 | 2.12 (1.36, 3.31) | 1.76 (1.11, 2.78) | |
| Variable | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|
| |||
| Length of stay (>3 days) | |||
| Cardiac comorbidity | |||
| 0 | 1.00 | 1.00 | |
| 1 | 1.20 (0.90, 1.60) | 1.16 (0.87, 1.55) | |
| 2 | 1.43 (1.07, 1.92) | 1.36 (1.01, 1.83) | |
| 3 | 1.81 (1.31, 2.50) | 1.65 (1.19, 2.29) | |
| ≥4 | 2.42 (1.74, 3.37) | 2.03 (1.45, 2.86) | |
| Noncardiac comorbidity | |||
| 0 | 1.00 | 1.00 | |
| 1 | 1.32 (1.10, 1.59) | 1.24 (1.03, 1.50) | |
| 2 | 1.84 (1.44, 2.36) | 1.64 (1.27, 2.11) | |
| ≥3 | 2.04 (1.46, 2.85) | 1.73 (1.23, 2.44) | |
Notes:
Adjusted for age, sex, race, marital status, year of hospitalization, and AMI order and type;
adjusted for age, sex, race, marital status, year of hospitalization, AMI order and type, and the noncardiac and cardiac morbidities examined;
the ORs for the first two table columns refer to the multivariable adjusted estimates when the cardiac comorbidities and noncardiac comorbidities are respectively analyzed separately, whereas the third column presents the adjusted estimates when both the cardiac and noncardiac comorbidities are included together in the model.
Abbreviations: AMI, acute myocardial infarction; CF, case-fatality; CI, confidence interval; OR, odds ratio.
We further examined the association between multiple coexisting conditions and in-hospital mortality and LOS. Due to the limited number of patients with certain comorbidity combinations, we focused on the three most common combinations of previously diagnosed comorbid conditions. The most frequent combination of two or more cardiac comorbidities was “CHD + hypertension” (n = 340, 11.4%) followed by “CHD + diabetes + hypertension” (n = 182, 6.1%) and “diabetes + hypertension” (n = 156, 5.3%). Among patients with these multiple comorbid conditions, 8.2%, 7.7%, and 9.6% of these patients, respectively, died during hospitalization (all were not significantly different than the overall hospital death rate of 9.8%), and 53.7%, 62.6%, and 55.1% had a LOS .3 days, respectively (all were not significantly different than the overall frequency of 56.1%).
Among those with two or more noncardiac conditions, the most frequent combination was “anemia + CKD” (n = 104, 3.5%), followed by “COPD + CKD” (n = 59, 2.0%), and “COPD + depression” (n = 54, 1.8%). Among these patients, 14.4%, 11.9%, and 14.8%, respectively, died during hospitalization (all were not significantly different than the overall hospital death rate of 9.8%), while 76.9%, 69.5%, and 70.4% had a LOS >3 days, respectively (all were significantly [P < 0.05] higher than the overall frequency of 56.1%).
Discussion
The results of this population-based observational study demonstrated that patients with multiple cardiac or noncardiac comorbidities had a higher odds of dying during hospitalization for AMI and having a more prolonged hospital stay compared to those with fewer or no previously diagnosed cardiac or noncardiac conditions. Patients with multiple cardiac or noncardiac comorbidities were significantly less likely to have undergone a PCI than patients with fewer comorbid conditions, but there were no significant differences in medication treatment practices according to the number of cardiac comorbidities present.
Prevalence of cardiac and noncardiac comorbidities
In our study population, the vast majority (87%) had at least one cardiac comorbid condition, whereas slightly more than half (55%) had at least one noncardiac comorbid condition previously diagnosed. More than one-half of patients had a history of CHD or hypertension, and approximately one-fifth had CKD. Among the seven cardiac comorbid conditions examined, hypertension was highly prevalent, irrespective of the number of cardiac comorbidities previously diagnosed, whereas CHD and diabetes were highly prevalent among patients with two or more cardiac comorbidities. Similarly, among the five noncardiac comorbidities examined, CKD was the most prevalent condition whereas anemia was more prevalent among patients with two or more cardiac comorbidities.
Our findings share similar patterns to the results of a recent analysis from the Worcester Heart Attack Study that examined trends in the frequency of multiple cardiovascular comorbidities among patients hospitalized with AMI between 1990 and 2007.10 In that analysis, we showed that hypertension and diabetes were the two most prevalent conditions among these patients.10 The present results are also consistent with the findings from other contemporary investigations that have studied patients hospitalized with AMI, including a community-based study from Kaiser Permanente Northern California that demonstrated a high burden of hypertension, diabetes, and CHD in this large regional population.19 Since the burden of comorbid diseases is associated with an increased risk of adverse outcomes, it is important to recognize the frequency and importance of these common comorbidities and take them into consideration in examining differences in treatment practices and outcomes in patients hospitalized with AMI.
Factors associated with multiple comorbidities
In a prior analysis of data from the Worcester Heart Attack Study we found that older individuals, women, nonwhite, and widowed patients were more likely to have multiple cardiovascular comorbidities previously diagnosed than respective comparison groups.10 In the present study, we extend these findings by showing that similar patient demographic characteristics were associated with multiple cardiac and noncardiac comorbid conditions. In addition, we found that patients with multiple cardiac or noncardiac comorbidities were more likely to have developed a NSTEMI, have had a prior MI, and have higher serum glucose, but lower eGFR and serum cholesterol levels, at the time of hospital admission compared to those without any cardiac or noncardiac comorbidities.
Hospital treatment practices
Characterizing the magnitude and profile of cardiac and noncardiac conditions in patients hospitalized with AMI may help explain differences in acute treatment practices and inform the design of clinical guidelines and disease management practices that are beneficial to these complex and often frail patients. The American College of Cardiology/American Heart Association guidelines for the use of cardiac medications in patients hospitalized with AMI have recommended the utilization of β-blockers and aspirin (1990), angiotensin-converting-enzyme (ACE) inhibitors (1996), and the use of lipid lowering medications in the 2002 and 2004 guidelines for the management of patients with NSTEMI and STEMI, respectively.20–23 In the present study, beta blockers and aspirin were prescribed to the majority of hospitalized patients whereas thrombolytic agents were rarely prescribed; each of the other medications was prescribed to at least three quarters of hospitalized patients.
We observed the frequent use of guideline-directed medications in the treatment of patients hospitalized with AMI, irrespective of the number of cardiac comorbid conditions present. This finding may be due, in part, to a ceiling effect since these cardiac medications were commonly prescribed to all patients hospitalized with AMI. However, our analysis focused on the receipt of cardiac medications during hospitalization for AMI in patients with different cardiac and noncardiac comorbidities, such as hypertension, diabetes, and CKD, which may have been differentially prescribed to these patient subgroups in the outpatient setting. Further studies should be carried out examining the number and type of medications prescribed for outpatients with single and multiple chronic comorbidities over the course of their long-term follow-up visits.
Since patients with multiple comorbidities tend to be older and sicker,10 we observed that patients were less likely to have undergone coronary revascularization procedures as the frequency of cardiac or noncardiac comorbidities increased. Our results suggest that patients with multiple comorbidities have a considerably different clinical presentation than those with fewer comorbid conditions, which may make them less likely to receive evidence-based therapies at the time of hospital admission and, by extension, increase their risk of adverse outcomes. Our results, in combination with prior study findings, emphasize the importance of developing clinical management guidelines specifically tailored for hospitalized AMI patients with multiple cardiac or noncardiac comorbidities given their high risk of adverse outcomes.
Hospital outcomes
There are few published studies describing the relation between multiple comorbidities and short- and long-term outcomes among patients hospitalized with AMI. A recent analysis of data from the Worcester Heart Attack Study found that, among patients hospitalized with AMI between 1990 and 2007, those who had two or more cardiovascular comorbidities were at higher risk for dying within 30 days and at 1 year after hospital admission compared to patients with no comorbid cardiovascular condition.10 A recent analysis of nearly 4,000 patients hospitalized with AMI from the PREMIER-QI study at 19 US hospitals between 2003 and 2004 found that the presence of at least one acute noncardiac condition was associated with a markedly increased risk of dying during hospitalization.24
In the current study, we observed a dose-response relationship between number of cardiac or noncardiac comorbidities and in-hospital mortality and prolonged LOS. Since clinical guidelines and disease management programs typically focus on single conditions, and clinical research often excludes persons with multiple chronic conditions, our observation that patients with multiple cardiac or noncardiac comorbidities were significantly more likely to have experienced adverse hospital outcomes suggests that current clinical guidelines need to take into consideration the comparatively poorer short-term outlook of these high-risk patients. The lack of currently available evidence about the inpatient management of patients with multiple comorbidities reinforces the development of contemporary treatment approaches to improve the in-hospital and longer-term outcomes of these high-risk patients.
Study strength and limitations
The strengths of the present study include its community-based design, its large sample of patients hospitalized with AMI, and its relatively contemporary perspective in examining clinically relevant outcomes and hospital treatment practices according to the frequency of a number of important cardiac and noncardiac comorbidities. Several limitations need to be acknowledged, however, in the interpretation of the present findings. First, since our study population included only patients who had been hospitalized in the Worcester metropolitan area, one needs to be careful to extrapolate our findings to those who died before hospitalization or to those who reside in other geographic areas. Second, since the majority of our study participants were white, the generalizability of our findings to other race/ethnic groups may be limited. Lastly, there is the potential for unmeasured confounding as we did not have information available on several patient-associated characteristics, such as income, education, and psychological factors, that may have affected several of the endpoints examined.25
Conclusion
In this study of nearly 3,000 patients hospitalized with AMI in central Massachusetts, we observed a high frequency of multiple cardiac and noncardiac comorbidities. Presence of multiple comorbidities was associated with a higher likelihood of dying during hospitalization and being hospitalized for a more prolonged period. Given the aging US population, the comorbidity burden in patients with acute coronary disease will likely continue to increase. Our findings highlight the need for further contemporary data to help guide the development of effective treatment modalities for the comprehensive management of patients with AMI and multiple concurrent medical illnesses with the long-term goals of improving the prognosis and quality of life of these individuals.
Acknowledgments
Funding support for this research was provided by the National Institutes of Health (RO1 HL35434). Partial salary support for Drs Saczynski, McManus, Gore, and Goldberg was provided for by the National Institutes of Health grant 1U01HL105268-01. Dr Saczynski was supported in part by funding from the National Institute on Aging (K01 AG33643).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chronic Conditions: Making the Case for Ongoing Care [webpage on the internet] Princeton, NJ: Robert Wood Johnson Foundation; 2010Available from: http://www.rwjf.org/pr/product.jsp?id=50968Accessed May 19, 2013 [Google Scholar]
- 2.Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303:1303–1304. doi: 10.1001/jama.2010.381. [DOI] [PubMed] [Google Scholar]
- 3.Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14(Suppl 1):28–32. doi: 10.1080/13814780802436093. [DOI] [PubMed] [Google Scholar]
- 4.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(Suppl 3):391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119:263–270. doi: 10.1016/j.phr.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolff JL, Starfeld B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 7.Sachdev M, Sun JL, Tsiatis AA, Nelson CL, Mark DB, Jollis JG. The prognostic importance of comorbidity for mortality in patients with stable coronary artery disease. J Am Coll Cardiol. 2004;43:576–582. doi: 10.1016/j.jacc.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 8.Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kostis WJ, Deng Y, Pantazopoulos JS, Moreyra AE, Kostis JB, Myocardial Infarction Data Acquisition System (MIDAS14) Study Group Trends in mortality of acute myocardial infarction after discharge from the hospital. Circ Cardiovasc Qual Outcomes. 2010;3:581–589. doi: 10.1161/CIRCOUTCOMES.110.957803. [DOI] [PubMed] [Google Scholar]
- 10.McManus DD, Nguyen HL, Saczynski JS, Tisminetzky M, Bourell P, Goldberg RJ. Multiple cardiovascular comorbidities and acute myocardial infarction: temporal trends (1990–2007) and impact on death rates at 30 days and 1 year. Clin Epidemiol. 2012;4:115–123. doi: 10.2147/CLEP.S30883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gili M, Sala J, López J, et al. Impact of comorbidities on in-hospital mortality from acute myocardial infarction, 2003–2009. Rev Esp Cardiol. 2011;64:1130–1137. doi: 10.1016/j.recesp.2011.07.010. Spanish. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 13.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 14.Floyd KC, Yarzebski J, Spencer FA, et al. A 30 year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–e304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 16.Antman EM, Hand M, Armstrong PW, et al. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. [DOI] [PubMed] [Google Scholar]
- 17.Page RL, 2nd, Lindenfeld J. The comorbidity conundrum: a focus on the role of noncardiovascular chronic conditions in the heart failure patient. Curr Cardiol Rep. 2012;14:276–284. doi: 10.1007/s11886-012-0259-9. [DOI] [PubMed] [Google Scholar]
- 18.McManus DD, Chinali M, Saczynski JS, et al. 30-year trends in heart failure in patients hospitalized with acute myocardial infarction. Am J Cardiol. 2011;107:353–359. doi: 10.1016/j.amjcard.2010.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 20.Gunnar RM, Passamani ER, Bourdillon PD, et al. Guidelines for the early management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee to Develop Guidelines for the Early Management of Patients With Acute Myocardial Infarction) J Am Coll Cardiol. 1990;16:249–292. doi: 10.1016/0735-1097(90)90575-a. [DOI] [PubMed] [Google Scholar]
- 21.Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute myocardial infarction) J Am Coll Cardiol. 1996;28:1328–1428. doi: 10.1016/s0735-1097(96)00392-0. [DOI] [PubMed] [Google Scholar]
- 22.Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina) Circulation. 2002;106:1893–1900. doi: 10.1161/01.cir.0000037106.76139.53. [DOI] [PubMed] [Google Scholar]
- 23.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 24.Lichtman JH, Spertus JA, Reid KJ, et al. Acute noncardiac conditions and in-hospital mortality in patients with acute myocardial infarction. Circulation. 2007;116:1925–1930. doi: 10.1161/CIRCULATIONAHA.107.722090. [DOI] [PubMed] [Google Scholar]
- 25.Sun WJ, Xu L, Chan WM, Lam TH, Schooling CM. Are Depressive Symptoms Associated With Cardiovascular Mortality Among Older Chinese: A Cohort Study of 64,000 People in Hong Kong? Am J Geriatr Psychiatry. 2013 Feb 6; doi: 10.1016/j.jagp.2013.01.048. Epub. [DOI] [PubMed] [Google Scholar]