Abstract
High-quality medical photography plays an important role in teaching and demonstrating the functional capacity of the hands, as well as in medicolegal documentation. Obtaining standardized, high-quality photographs is now an essential component of many surgery practices. The importance of standardized photography in facial and cosmetic surgery has been well documented in previous studies, but no studies have thoroughly addressed the details of photography for hand surgery. In this paper, we will provide a set of guidelines and basic camera concepts for different scenarios to help hand surgeons obtain appropriate and informative high quality photographs. A camera used for medical photography should come equipped with a large sensor size and an optical zoom lens with a focal length ranging anywhere from 14-75mm. In a clinic or office setting, we recommend six standardized views of the hand and four views for the wrist, and additional views should be taken for tendon ruptures, nerve injuries, or other deformities of the hand. For intra-operative pictures, the camera operator should understand the procedure and pertinent anatomy in order to properly obtain high-quality photographs. When digital radiographs are not available, and radiographic film must be photographed, it is recommended to reduce the exposure and change the color mode to black and white to obtain the best possible pictures. The goal of medical photography is to present the subject in an accurate and precise fashion.
Keywords: Hand surgery, Medical photography, Pictures
Introduction
The advent of photography in the early 1800's served to enhance our perceptual ability, and this new technology would make a similar impression in the field of medicine. In 1845, less than 20 years after the first photograph was taken, the first pre- and postoperative photographs in plastic and reconstructive surgery were printed in a medical journal by Gurdon Buck(1). These images were daguerreotypes, the first real form of photography, accomplished through a lengthy chemical interaction between iodine, bromine, and chlorine that required up to ten minutes to generate a picture. In April of 1850, Charles Gilbert reported several cases in the American Journal of Dental Science using photographs to demonstrate pre- and postoperative results of reconstructive procedures, including a forehead flap for nasal reconstruction and a jaw reconstruction following a tumor excision(1). James Balossa was probably the earliest surgeon to present nasal reconstruction with photography in a book in 1863(2). During the first international congress of plastic surgery in 1955, Sir Harold Gillies stated that the greatest advancement in plastic surgery to date was the use of photography in medical applications(3). Recent advancements in computer and film technology have culminated in the complete digitization of photographs, and in the modern era, clinical photography has become an indispensable tool in the hand surgeon's arsenal. The advent of the digital camera provides rapid and efficient dissemination of clinical pictures into the research and teaching environment. Now, surgeons rely heavily on pre-operative, intra-operative, and post-operative photographs as a teaching tool and to help evaluate outcomes. Obtaining standardized, high-quality photographs has become an essential component of success to many surgical practices.
Importance of Medical Photography
There are many advantages to obtaining high quality photographs in the medical setting: 1) Photographs can be used for scientific presentations and manuscripts. 2) Preoperative and postoperative photographs can be used to demonstrate functional deficits or improvements and operative results, providing a tool for evaluation by the surgeon(4). 3) Intraoperative photographs of procedures provide evidence and examples that can prove important for education, communication, and medicolegal purposes. Occasionally, surgeons present their clinical work at conferences featuring pictures that are blurry, or containing blood-stained backgrounds or extraneous surgical instruments with no pertinence to the subject of the photograph. All of these oversights detract attention from the theme the photographer is trying to depict, and diminish the educational value that a picture is able to provide. Even the best presentation can be compromised by a poor series of pictures, and this same concept applies to medical textbooks and journal manuscripts.
Previous studies that have reported on obtaining photographic documentation in plastic and cosmetic surgery(5-9) mainly discussed the technical aspects of the camera, such as the lens and lighting(10). In 1984, Zarem (11) described details regarding photography of the hand, stating, “Photographs of the hand may be specialized depending on the specific function in question” and that “The hand should not be touching the background material, so that the position is a true anatomic position.” Although this article is not a comprehensive guide for photography in hand surgery, this may be the first paper that mentions how best to obtain medical photographs of the hand(11). However, over the past several decades, numerous advancements have taken place in the hand surgery specialty that necessitate documentation, and now most highly regarded journals, such as the Journal of Hand Surgery, have begun to institute standardized criteria for medical photography. It is now generally understood that high quality photographs of both hands should be obtained in the clinical setting so that any differences in the function or appearance of both hands can be documented before and after operative intervention. In addition, it is important to remember that the goal of medical photography is to present the subject in an accurate and precise fashion, rather than a favorable manner as is done in portrait photography(12). We aim to provide a set of guidelines that will delineate the critical steps and essential components for hand surgeons to obtain appropriate and informative high quality photographs that will help them better educate and evaluate treatment options.
Camera
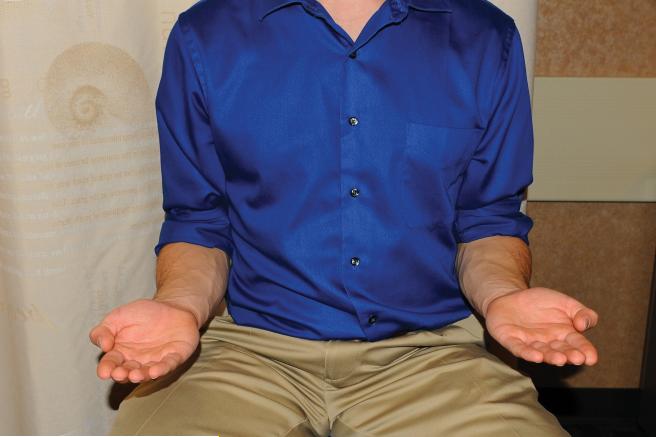
The ideal camera for medical photography should feature a large sensor size (minimum pixel pitch of 4.8 microns) which permits more light per pixel, thus providing better images and containing a higher range of contrast as well as better color depth. For obtaining photographs in the medical setting, a camera that is easy to operate with a built-in flash is preferred. For intraoperative photography, it is very beneficial for the camera to have a swivel screen that will enable the operator to shoot at a wide array of angles. (Fig. 1) We recommend for clinical and surgical photography, the point and shoot digital camera over a single-lens reflex (SLR) camera because it is easy to operate, cheaper on average, and is able to provide high quality images that easily satisfy the requirements for medical photography.
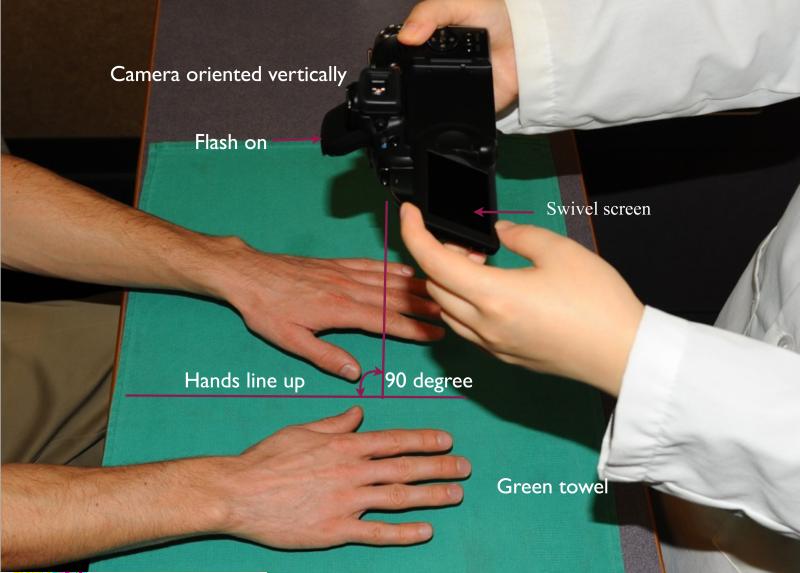
Figure 1.
During clinical photography, the patient should sit directly across from the photographer, with their hands held 2-3 inches above the background material, while the camera is positioned directly above the patient's hands. A camera featuring a swivel screen enables the photographer to shoot pictures from a variety of angles.
Basic Concepts
Aperture and depth of field
It is important for the camera operator to have a basic knowledge of the camera and associated lens equipment. Proper aperture and shutter speed are critical for obtaining high quality photographs, especially when attempting to highlight the minute details of multiple structures in a small, crowded space, such as the hand compartments(10). The aperture is the diameter of the opening in the lens, and controls the amount of light that passes through the lens, thereby determining the depth of field. The depth of field is the area between the closest and farthest objects in an image that will appear sharp in the picture, and is quantified as an inverse ratio to the aperture. The aperture is typically designated by a specific f-number (f is the focal length of the lens), and the camera can be set to a series of f-stops that will adjust the depth of field(10). A large aperture, such as f/2.8, will result in a shallow depth of field and the camera will only focus on a small area, while leaving the background out of focus(12). A small aperture, such as f/8, will produce a larger depth of field, enabling the camera to keep the entire scene in focus. A large depth of field is preferred for medical photography to capture all of the important anatomic and functional details of a subject.
Optical and Digital Zoom
The zoom capability of a camera can be divided into two categories, optical zoom and digital zoom. Digital zoom functions to digitally alter an image by enlarging and cropping a portion of the image to achieve the effect of magnification. Digital zoom is not a real form of zoom because it only enlarges the existing pixels of an image instead of adjusting the lens itself to create a new image. Owing to the mechanical constraints of digital zoom, the result will always be a lower quality image. Optical zoom, on the other hand, is achieved by adjusting the magnification optically through the lens, serving to bring the object closer. Optical zoom will result in a clear, high quality image even at longer distances since it has the capability to focus on distant objects. For medical photography, optical zoom is always preferred over digital zoom(13). If using a camera with digital zoom, it is not recommended to use the zoom feature, but instead the picture will be clearer if the camera is simply moved closer to the object being photographed.
Lens
The quality of a lens is determined by two fundamental parameters, the aperture and the focal length. A lens with a larger aperture is generally preferred for medical photography. A standard zoom lens with a focal length anywhere between 14-70 mm is acceptable to quickly and properly frame and obtain pictures. A prime lens has a focal length that is fixed, making adjustments difficult. The fixed focal length forces the photographer to change shooting positions in order to focus on an object and achieve the desired photograph, and therefore this lens is not recommended for medical photography.
Lighting and International Organization of Standardization (ISO)
Lighting is a crucial factor when taking high quality photographs. Standardized photographs require appropriate light sources to provide optimal contrast and detail of the anatomy, functional posture, and appearance of the hands. As previously described, a large image sensor is ideal, especially under low light conditions. Generally, under the same light conditions, images taken by a camera with a larger sized sensor are of better quality due to a smaller amount of “noise” being picked up by the camera. Image “noise” refers to the random variations of color and brightness that degrade image quality, caused by extraneous information picked up by the electronic sensor of a camera. In a well-lit room, the built-in flash on a camera is sufficient to produce high quality photographs. In poor lighting conditions, the built-in camera flash tends to create shadows and uneven lighting, and a longer exposure time is needed which will likely result in a blurred image. In addition, a larger aperture is required to achieve sufficient light exposure, but this can decrease the depth of field and possibly result in blurred images. Therefore, in this condition, a small size and lightweight external flash or ring flash should be considered to help produce acceptable pre-, intra, and post-operative images(14,15). The amount and angle of light from the camera flash and external sources should be held consistent to produce comparable photographs(11).
The ISO number is a measure of the film speed in a digital camera, determined by the sensitivity of a camera's sensor to light. Typically, digital cameras will have ISO numbers ranging from 100 to 6400, with high numbers representing a greater sensitivity to light. The higher ISO numbers are accomplished by amplifying the image signal and image noise. When most point and shoot cameras are set above 400 ISO, the image noise may be increased to a level that can drastically reduce image quality. In order to prevent image quality reduction, it is suggested to keep the ISO under 400, with a recommended setting around 200.
Background
The background of a surgical picture can have a substantial effect on the quality of the photograph. An ideal background must not be distracting and should always feature the same tones when used in a series of pictures. Previous studies have shown that either a medium or sky blue tone background is an acceptable color (16,17). We prefer to use the same size 60 cm by 40 cm green surgical towel as a background for all pre-, intra-, and post-operative photographs whenever possible. We recommend removing any creases or wrinkles that are disrupting the background material before pictures are taken, as this can decrease the overall quality of the image. In the clinical setting, we iron a green towel to remove creases and wrinkles. When obtaining intraoperative images, because we are not able to iron the sterile green surgical towel, we simply pull the corners of the towel tightly to minimize or remove creases and wrinkles. As previously mentioned, any debris such as surgical instruments, gauze, and blood should be taken away from the focal point of the picture to avoid the potential for distraction by the viewer.
Clinical Photography
Clinical photos, including the pre- and post-operative photographs, can be obtained when a patient is awake and cooperative according to the following steps:
In order to comply with Health Insurance Portability and Accountability Act (HIPAA) regulations, consent should be requested from all patients before medical photographs are taken (Fig. 2). The consent form should also include permission to publish all photographs of the patient or use them for academic purposes.
Any accessories on the hand such as bracelets, rings, and watches should be removed if possible.
To achieve optimal positioning, the patient should be seated on a stool, directly facing the camera operator.
Both hands should then be held a few inches above a table with the appropriate background underneath.
Once it is time to take the picture, the patient's hands need to be lined up at the finger tips as accurately as possible, and the patient should avoid touching the background to prevent any possible distortion of the natural finger posture.
The camera should be positioned directly above the patient's hands and the picture can be captured (Fig. 1).
It is imperative that these steps are followed during each photographic session so that a series of pictures is taken in a standardized manner.
Figure 2.
An example of a photograph consent form that also provides permission to publish or use for academic purposes.
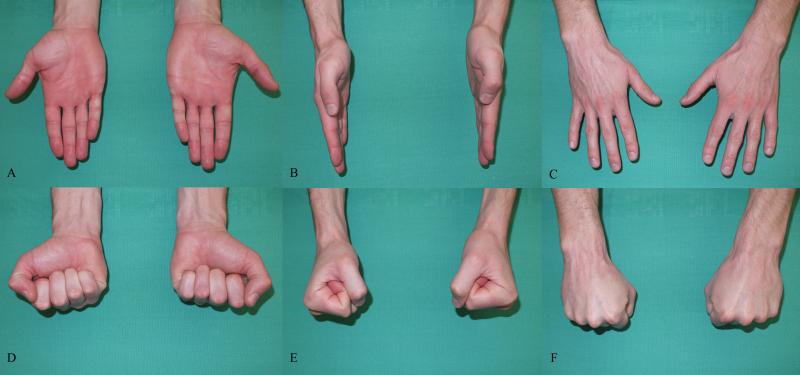
Medical photographs play an important role in determining and evaluating hand function, and a wide range of pictures satisfy this role for a variety of hand disorders. Irrespective of a patient's condition, a set of six standard views should always be photographed of both hands, including an anterior (palmar view), posterior (dorsal view), and a lateral view, with the patient having a clenched fist and open hand at each individual view (Fig. 3A-F). These six views are essential to demonstrate pre-and postoperative functional posture and appearance.
Figure 3.
These are the six standardized views of both hands in the clinical setting A. Fingers straight in palmar view. B. Fingers straight in lateral view. C. Fingers straight in dorsal view. D. Clenched fist in palmar view. E. Clenched fist in lateral view. F. Clenched fist in dorsal view.
For a patient experiencing a nerve injury or tendon laceration, in addition to the six standard views, a series of photographs should be taken that reflect the functional status of the muscles and accompanying structures by displaying different posture views. Table 1 highlights the assorted pictures that are useful to demonstrate the function of the various tendons and muscles of the hand. To demonstrate the function of the nerves, pictures should be taken as described in Table 2. For patients with a hand deformity, additional views should be taken from orientations that demonstrate any deformities and resulting dysfunction of the hand. These views should include the natural hand posture and any other views that help to demonstrate the functional limitations or deformed appearance of the hand (Fig. 4A-B).
Table 1.
Pictures used to demonstrate the functional views of individual tendons or muscles in the hand.
| Tendon or muscle group being tested | Functional view | Hand position |
|---|---|---|
| Flexor pollicis longus | Actively flex the IP joint of the thumb | Palm up |
| Flexor digitorum superficialis | Flex the PIP joint of the involved finger while keeping the DIP joints of the adjacent fingers in extension | Palm up |
| Flexor digitorum profundus | Flex the DIP joint of the finger while extending the PIP joint of the same finger and keeping the adjacent fingers in flexion | Palm up |
| Flexor carpi ulnaris and flexor carpi radialis | Flex the wrist | Lateral view |
| Abductor pollicis longus and extensor pollicis brevis | Hold the thumb in abduction | Palm down |
| Extensor carpi radialis longus and extensor carpi radialis brevis | Make a fist and extend the wrist | Lateral view |
| Extensor pollicis longus | With the hands resting flat on a table, raise the thumb off the surface | Palm down |
| Extensor indicis proprius | Point the index finger out straight, keeping the rest of the fingers clenched in a fist | Lateral view |
| Extensor digitorum minimi | Point the small finger out straight, keeping the remaining fingers clenched in a fist | Palm up or lateral view |
| Extensor carpi ulnaris | Deviate the hands dorsally and ulnarly | Palm down |
| Thenar muscle | Touch the thumb to the small finger | Palm up |
| Interosseous and lumbrical muscles | Cross with the finger adjacent to the finger being tested | Palm up or palm down |
Table 2.
Photographs used to demonstrate the functional capacity of the median nerve and ulnar nerve.
| Nerve being tested | Functional view | Hand position |
|---|---|---|
| Median nerve | Raise the thumb up straight to form a 90-degree angle with the palm | Palm up |
| Ulnar nerve | Spread the fingers apart or cross with one of the adjacent fingers | Palm up or palm down |
Figure 4.
Demonstration of the special views required for a hand disorder. A. Metacarpophalangeal joint subluxation of the small and ring fingers while the patient's hand is held in the natural posture. B. The subluxed fingers are reduced and held back into the normal anatomic position.
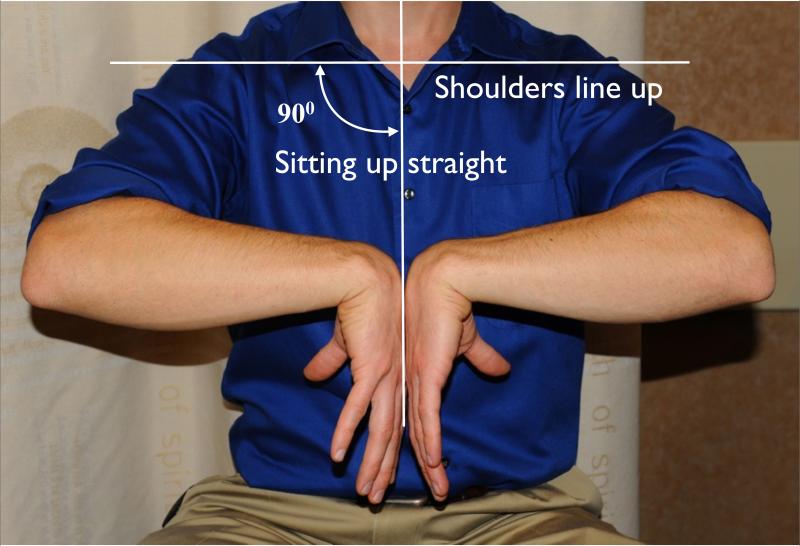
The motion of the wrist is a sum of all the movements of the radiocarpal joint, midcarpal joint, ulnocarpal joint, and radioulnar joint. When obtaining wrist photographs, it is recommended to include the elbow, wrist, and the hands. The patient must be sitting up straight, and the shoulders should be lined up perpendicular to the sagittal plane (Fig. 5A). Standardized views need to demonstrate pronation, supination, flexion, and extension of the wrist, which can represent the wrist range of motion in this series of pictures (Fig. 5A-D).
Figure 5.
Standard wrist views used to demonstrate the functional capacity of the wrist. Patients should sit up straight directly across from the photographer, with their shoulders lined up perpendicular to the sagittal plane. A. Flexion of the wrist is tested. B. Extension of the wrist is tested. C. Supination of the wrist is tested. D. Pronation of the wrist is tested.
Intra-operative Photography
Intra-operative photographs are a great resource for demonstrating a dynamic series of procedures. It is difficult and sometimes impossible for a surgeon to take consistent intra-operative photographs during a procedure, and therefore it is useful to have a dedicated photographer for each case. The camera operator must possess a basic understanding of the procedure and pertinent anatomy in order to properly obtain relevant high quality photographs. The suggested position for the camera operator is directly behind the surgeon, shooting from the surgeon's view. While taking pictures, the surgical light source should be turned off in order to avoid shadows caused by the camera that could affect color balance. Similar to clinical pictures, we prefer a green surgical towel for every procedure, removing redundant instruments and excess blood whenever possible. It is important to keep the surgeon's and assistant's hands and fingers out of the surgical field by using hooks and retractors to move erroneous muscle, tendons, and tissue from the focus of the picture(18) (Fig. 6A-B). Typically, most hand surgeries are performed under tourniquet control which substantially reduces bleeding. In this scenario, intraoperative pictures can be taken after cleaning the entire surgical area of debris, and having cleaned up any blood stains on the patient's and surgeon's hand. The background should be a clean green (or previously recommended color) towel with the creases removed by pulling on all four corners, free of water or blood stains. It is better to take a full view of the hand to effectively present the orientation and relationship of tissue and structures to the viewer.
Figure 6.
These are examples of good and bad surgical pictures. A. In this picture, the surgeon's and assistant's hand, excess blood, and erroneous gauze and surgical instruments are all distracting to the viewer. B. This picture provides an unobstructed view of the hand, and therefore the viewer is drawn to the focal point of the picture.
If more details of the tissue are to be reflected in the photograph, another picture can be taken while moving the camera closer to the subject. In surgical pictures, the hand should be parallel to the axis of the photograph. To demonstrate the different layers of the tissue, sufficient depth of field should also be taken into account(19). Typically, in the hand surgery scenario, the tissue layers are close and the distance from the plane of focus to the background (or fore-ground) tissue is small, necessitating a smaller aperture setting and large depth of field. One should adjust the parameters beforehand to spare time during the procedure. When pictures are used to demonstrate the geometry of a defect, a surgical specimen, or a graft, a ruler will aid in providing a reference for the size of such objects. Surgical specimens should be photographed in two separate locations, in close proximity to the extraction site of the specimen and isolated on the background. Similarly, grafts should be photographed next to the donor site and alone on the background. A sterile marking pen may be used to identify pertinent information, or this information can be input digitally with editing software.
Photography for Radiographic Film
When digital radiographs are not available, and photographs of radiographic film need to be obtained, the following steps are recommended:
Place the X-ray into the X-ray box, and be sure the room and X-ray box lights are on.
Turn off the camera flash and change to the camera's black and white mode.
Reduce the exposure to the minus setting because overexposure would reduce details of the X-rays.
The camera's light sensor tends not to be as accurate on direct light sources, and can lead to overexposure of the photograph. Therefore, it is important to position the camera in the best possible orientation so as to achieve adequate lighting throughout the whole picture.
Settings
For clinical and intraoperative photography, we prefer the aperture priority mode, which allows the user to choose a specific aperture value while the camera selects a shutter speed to match. This mode can easily provide a consistent depth of field, an important consideration when taking medical pictures (Table 3). It is difficult to recommend a specific aperture number because the lens aperture varies by focal length, but a good general rule is the lower the f-stop number, the larger depth of field the camera will provide. For a modern high quality point and shoot digital camera, an aperture setting ranging from f/4.5-f/5.6 is adequate to achieve a sufficient depth of field. Aperture priority mode with the “Macro” setting on can be helpful for intraoperative photography when the camera is positioned close to the subject. The “P” mode with the “Macro” setting on makes it convenient to obtain radiographic film photographs. Once the optimal mode for the photographer has been established, each photograph should be taken with the same settings to provide consistent photographs.
Table 3.
Camera settings for different photographic environments.
| Suggested Setting | Macro | Flash | ISO | Shutter | |
|---|---|---|---|---|---|
| Clinical photography | Aperture priority (A or AV) mode | On or Off | On | ≤400 | ≤l/60 |
| Intra-operative photography | Aperture priority (A or AV) mode | On or Off | On | ≤400 | ≤l/60 |
| Radiographic photography | P mode, switch the color to black and white (BW) and adjust exposure to minus | On | Off | Auto | Auto |
ISO: Internationa Organization for Standardization
P: Program mode
Image Formatting
After obtaining medical photographs or digital radiographs, it is imperative to properly format the image in order to attain the highest quality product. Images should be oriented in the same plane that a surgeon would view them when in a particular setting. Clinical pictures, and radiographs downloaded from a database (X-rays, CT, MRI), should be oriented vertically (Fig. 3). However, in the operating room, the picture should be oriented horizontally because this is the view the surgeon will actually see while operating (Fig. 6B). It is not appropriate to publish pictures that are at random angles, as this can be confusing for the reader, and therefore images should always be rotated vertically or horizontally to a 90 degree angle. It is also recommended that images are digitally cropped, leaving only the essential aspects of the photograph, and measures should be taken to crop or cover a patient's face or eyes because these elements have no relevance to a hand condition.
Summary
High-quality photographic documentation is an integral aspect of hand surgery for the purposes of demonstrating hand function, evaluating surgical results, and academic communication. An appropriate camera and lens are essential to producing the best photographic results. The six standard hand views should be obtained for each patient to compare natural posture, operative results, and functional capacity. When additional views are required, the proper settings should be taken into account so that the best possible photograph is always obtained. Images should also be digitally formatted in order to provide a consistent and high quality product.
Acknowledgments
Disclosures: Research reported in this publication was supported by the National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases under Award Number R01 AR062066 and from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2R01 AR047328-06 and a Midcareer Investigator Award in Patient-Oriented Research under Award Number K24 AR053120 (to Dr. Kevin C. Chung.)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rogers BO. The first pre- and post-operative photographs of plastic and reconstructive surgery: contributions of Gurdon Buck (1807-1877). Aesthetic plastic surgery. 1991;15:19–33. doi: 10.1007/BF02273830. [DOI] [PubMed] [Google Scholar]
- 2.Wallace AF. The early history of clinical photography for burns, plastic and reconstructive surgery. British journal of plastic surgery. 1985;38:451–65. doi: 10.1016/0007-1226(85)90001-3. [DOI] [PubMed] [Google Scholar]
- 3.Guy C, Guy R, Zook E. Standards of photography (Discussion). Plast Reconstr Surg. 1984;74:145. doi: 10.1097/00006534-198407000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Henderson JL, Larrabee WF, Jr., Krieger BD. Photographic standards for facial plastic surgery. Archives of facial plastic surgery. 2005;7:331–3. doi: 10.1001/archfaci.7.5.331. [DOI] [PubMed] [Google Scholar]
- 5.Swamy RS, Sykes JM, Most SP. Principles of photography in rhinoplasty for the digital photographer. Clinics in plastic surgery. 2010;37:213–21. doi: 10.1016/j.cps.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Russell P, Nduka C. Digital photography for rhinoplasty. Plastic and reconstructive surgery. 2003;111:1366. doi: 10.1097/00006534-200303000-00075. [DOI] [PubMed] [Google Scholar]
- 7.Galdino GM, DaSilva, Gunter JP. Digital photography for rhinoplasty. Plastic and reconstructive surgery. 2002;109:1421–34. doi: 10.1097/00006534-200204010-00035. [DOI] [PubMed] [Google Scholar]
- 8.Galdino GM, Vogel JE, Vander Kolk CA. Standardizing digital photography: it's not all in the eye of the beholder. Plastic and reconstructive surgery. 2001;108:1334–44. doi: 10.1097/00006534-200110000-00037. [DOI] [PubMed] [Google Scholar]
- 9.Tatlidede S, Egemen O, Bas L. A useful tool for intraoperative photography: underwater camera case. Annals of plastic surgery. 2008;60:239–40. doi: 10.1097/SAP.0b013e318095a75f. [DOI] [PubMed] [Google Scholar]
- 10.Khavkin J, Ellis DA. Standardized photography for skin surface. Facial plastic surgery clinics of North America. 2011;19:241–6. doi: 10.1016/j.fsc.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Zarem HA. Standards of photography. Plastic and reconstructive surgery. 1984;74:137–46. doi: 10.1097/00006534-198407000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Hagan KF. Clinical photography for the plastic surgery practice--the basics. Plastic surgical nursing : official journal of the American Society of Plastic and Reconstructive Surgical Nurses. 2008;28:188–92. 93–4. doi: 10.1097/01.PSN.0000342822.44387.c5. [DOI] [PubMed] [Google Scholar]
- 13.Galdino GM, Chiaramonte M, Klatsky SA. The digital darkroom, part 3: digital presentations in plastic surgery. Aesthetic surgery journal / the American Society for Aesthetic Plastic surgery. 2001;21:1–9. doi: 10.1067/maj.2001.111958. [DOI] [PubMed] [Google Scholar]
- 14.Archibald DJ, Carlson ML, Friedman O. Pitfalls of nonstandardized photography. Facial plastic surgery clinics of North America. 2010;18:253–66. doi: 10.1016/j.fsc.2010.01.005. Table of Contents. [DOI] [PubMed] [Google Scholar]
- 15.Nayler JR. Clinical photography: a guide for the clinician. Journal of postgraduate medicine. 2003;49:256–62. [PubMed] [Google Scholar]
- 16.Neff LL, Humphrey CD, Kriet JD. Setting up a medical portrait studio. Facial plastic surgery clinics of North America. 2010;18:231–6. doi: 10.1016/j.fsc.2010.01.002. Table of Contents. [DOI] [PubMed] [Google Scholar]
- 17.Yavuzer R, Smirnes S, Jackson IT. Guidelines for standard photography in plastic surgery. Ann Plast Surg. 2001;46:293–300. doi: 10.1097/00000637-200103000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Humphrey CD, Kriet JD. Intraoperative photography. Facial plastic surgery clinics of North America. 2010;18:329–34. doi: 10.1016/j.fsc.2010.01.008. Table of Contents. [DOI] [PubMed] [Google Scholar]
- 19.Becker DG, Tardy ME., Jr. Standardized photography in facial plastic surgery: pearls and pitfalls. Facial plastic surgery : FPS. 1999;15:93–9. doi: 10.1055/s-2008-1064305. [DOI] [PubMed] [Google Scholar]