Abstract
Aim
The objective of this study was to evaluate the effect of instituting the 2010 Basic Life Support Guidelines on in-hospital pediatric and adolescent cardiopulmonary resuscitation (CPR) quality. We hypothesized that quality would improve, but that targets for chest compression (CC) depth would be difficult to achieve.
Methods
Prospective in-hospital observational study comparing CPR quality 24 months before and after release of the 2010 Guidelines. CPR recording/feedback-enabled defibrillators collected CPR data (rate (CC/min), depth (mm), CC fraction (CCF, %), leaning (% > 2.5 kg.)). Audiovisual feedback for depth was: 2005 ≥ 38mm; 2010 ≥ 50mm; for rate: 2005 ≥ 90 and ≤ 120 CC/min; 2010 ≥ 100 and ≤ 120 CC/min. The primary outcome was average event depth compared with Student’s t-test.
Results
45 CPR events (25 before; 20 after) occurred, resulting in 1336 thirty-second epochs (909 before; 427 after). Compared to 2005, average event depth (50 ± 13 vs. 43 ± 9 mm; p=0.047), rate (113 ± 11 vs. 104 ± 8 CC/min; p<0.01), and CCF (0.94 [0.93, 0.96] vs. 0.9 [0.85, 0.94]; p=0.013) increased during 2010. CPR epochs during the 2010 period more likely to meet Guidelines for CCF (OR 1.7; CI 95: 1.2–2.4; p<0.01), but less likely for rate (OR 0.23; CI 95: 0.12–0.44; p<0.01), and depth (OR 0.31; CI 95: 0.12–0.86; p=0.024).
Conclusions
Institution of the 2010 Guidelines was associated with increased CC depth, rate, and CC fraction; yet, achieving 2010 targets for rate and depth was difficult.
Keywords: pediatric, cardiopulmonary resuscitation, quality appraisal
Introduction
Thousands of children require in-hospital cardiopulmonary resuscitation (CPR) each year for sudden cardiac arrest.1,2 While resuscitation outcomes are improving, far too many children will suffer a neurological injury after their event.3,4 As resuscitation quality is associated with cardiac arrest outcome,5–9 recent science has focused on improving CPR quality, which unfortunately frequently does not meet American Heart Association (AHA) standards during resuscitation attempts.10,11
The 2010 Basic Life Support Guidelines12,13 shifted the focus of resuscitation from airway management towards providing high quality minimally interrupted chest compressions (CCs). This paradigm shift was exemplified in the acronym change from Airway-Breathing-Circulation (ABC) to Circulation-Airway-Breathing (CAB), and summarized in the Guidelines catchphrase “Push Hard, Push Fast.” By providing a simple message that was consistent across age groups – and only delaying ventilation by ~ 9–18 seconds when starting with CCs – the hope was that more cardiac arrest victims would receive high quality CPR, particularly from bystanders, and that outcomes would be improved.14
To date, no publication has evaluated if the Guideline’s change in focus has led to the desired effects (i.e., faster and deeper minimally interrupted CCs). Therefore, the objective of this study was to evaluate the quality of CPR performed at our institution compared to the targets established by the 2010 Basic Life Support Guidelines.12,13 We hypothesized that CPR quality would improve with institution of the 2010 Guidelines, but that the recommended targets for CC depth would be difficult to achieve even when CPR recording/feedback-enabled defibrillators, a post-cardiac arrest debriefing program,15 and daily CPR refresher trainings16–18 are utilized.
Methods
Design
This investigation is a prospective in-hospital observational study with the primary objective to compare the quality of CPR performed before and after publication of the Basic Life Support Guidelines in October 2010. Events occurring between October 2008 and September 2010 (24 months) were in the 2005 “before” period, while those occurring from October 2010 to September 2012 were in the 2010 “after” period. A censor period to allow dissemination of the Guidelines at our institution was not utilized or necessary. This conservative design was chosen because the infrastructure at our institution allows rapid dissemination of new national CPR training recommendations, particularly to those who are designated to perform chest compressions (resident/fellow trainees and registered nurses). Immediately in October 2010, our daily bedside CPR training program16–18 instituted 2010 Guidelines for nurse training, and all residents and fellows were individually trained to these targets at the start of their rotations. Additionally, the CPR recording/feedback-enabled defibrillator was also immediately “adapted” to 2010 Guidelines by using our intensive bedside training to focus providers on the use of its numeric visual feedback for CC rate and depth. Of note, audio feedback in accordance with 2010 Guidelines required a software upgrade that was not installed until January 2012.
The study protocol including consent procedures was approved by the Institutional Review Board at The Children’s Hospital of Philadelphia. Data collection procedures were completed in compliance with the guidelines of the Health Insurance Portability and Accountability Act (HIPAA) to ensure subject confidentiality. Written consent was obtained from all health care providers who participated in the resuscitation attempts.
Study Population
Consecutive chest compression events in the pediatric intensive care unit (PICU) or emergency department (ED) were considered in the analysis. These locations were chosen as they are the only care areas where the CPR recording/feedback-enabled defibrillators are deployed. All events – both pulseless arrest and bradycardia with poor perfusion – were considered.
Institutional Resuscitation Care Practices
At our institution, the Heartstart MRx defibrillator with Q-CPR option, jointly designed by Philips Health Care (Andover, MA) and the Laerdal Medical Corporation (Stavanger, Norway) was used to collect quantitative CPR data and to provide real-time feedback if the CPR was not meeting Guidelines in place at the time. The primary differences being: 1) the CC depth target: 2005 - ≥ 38mm; 2010 - ≥ 50mm (absolute measurement-based depth targets were based upon CT and external anthropometric measurement studies19–21 to coincide with the Guidelines recommendation of “at least 1/3 the Anterior-Posterior diameter” of the chest); and 2) the CC rate targets (in 2010, rate target was increased from “approximately” 100 CC/min to “at least” 100 CC/min). In both periods, CPR recording feedback-enabled defibrillators were deployed and there were ongoing daily CPR refresher trainings.16–18 Of note, in the 2010 period, a post-cardiac arrest debriefing program was instituted.15
Outcome Variables
Quantitative CPR was downloaded from the MRx defibrillators within 24 hours of each event. A Microsoft Windows based software program, Q-CPR Review (Version 2.1.0.0, Laerdal Medical, Stavanger, Norway), was used for initial examination and extraction of the quantitative CPR quality data. CPR quality parameters included chest compression rate (CC/min) and depth (mm), CC Fraction (i.e., the percentage of time during pulseless arrest that compressions are provided) and percentage of CC with significant leaning (> 2.5 kg22). In accordance with previous publications on CPR quality, an average of each parameter was calculated using Q-CPR Review for each event and for each 30-second epoch of resuscitation. Compliance with 2005 Guidelines was defined as: depth ≥ 38mm; rate ≥ 90 and ≤ 120/min; CC Fraction > 90%; leaning ≤ 10% of compressions. Targets for 2010 were: depth ≥ 50mm; rate ≥ 100 and ≤ 120/min; CC fraction > 90%; leaning ≤ 10% of compressions.
Statistical Analysis
Standard descriptive summaries, appropriate for the underlying distribution of the variable, were calculated. The primary outcome of interest was CC depth, treated as a continuous variable at the event level. CC depth was chosen as the primary outcome because it was the parameter most changed between 2005 and 2010 and also it has been most associated with survival outcome in human studies compared to other quality targets.8,23,24 Using a local quality improvement database, we estimated it would take at least 24 months to enroll 25 events in each period, which would give us over 80% power to show an improvement in depth from 38mm (2005 targets) to 50mm (2010 targets), assuming a standard deviation of 14mm10 (two-sided alpha equal to 0.05). At the event level, normally distributed continuous variables were compared with Student’s t-test while Wilcoxon Rank Sum was used for non-parametric variables. Compliance with Guidelines at the event level was compared via Chi-square test. In the secondary regression analysis to evaluate compliance of CPR epochs with Guidelines, generalized estimating equations were used to appropriately adjust the standard errors for within-event correlation of epochs. P values less than 0.05 were considered statistically significant. Statistical analysis was completed using Stata (Version 12.0, StataCorp, College Station, TX).
Results
During the study, a total of 45 CPR events occurred, which resulted in 25 events in the 2005 “before” period and 20 events in the 2010 “after” period. These events resulted in 1336 thirty-second epochs of CPR (909 before; 427 after). The average age of arrest victim was 13.9 ± 5 years (range 3.75–28 yrs.); average mass was 48.8 ± 22 kilograms (range 15.3–100.7 kg). All subjects were receiving invasive mechanical ventilation during CPR quality assessment. There were no significant differences between patient demographics or cardiac arrest event data between the two periods (Table 1).
Table 1.
Patient demographic and cardiac arrest event data.
| 2005 | 2010 | p | |
|---|---|---|---|
|
| |||
| Subject Demographic Data | n=25 | n=20 | |
| Age: years mean ± SD | 15 ± 5 | 12 ± 4 | 0.062 |
| Mass: years mean ± SD | 47.5 ± 19 | 51 ± 28 | 0.64 |
| Sex: male n (%) | 11 (44) | 15 (75) | 0.07 |
|
| |||
| Cardiac Arrest Event Data | |||
| Location PICU n (%) | 19 (76) | 13 (65) | 0.42 |
| Time of Arrest n (%) | 0.54 | ||
| Day/Evening (7AM–10:59PM) | 9 (36) | 9 (45) | |
| Night/Weekends* (11PM–6:59AM) | 16 (64) | 11 (55) | |
| Arterial line n (%) | 5 (20) | 3 (15) | 0.72 |
| Duration of CPR: minutes median (IQR) | 16.5 (4.5–22.5) | 7 (2.5–16) | 0.053 |
| Initial Rhythm n (%) | 0.84 | ||
| Bradycardia | 8 (32) | 8 (40) | |
| Asystole/PEA | 13 (52) | 10 (50) | |
| Ventricular Fibrillation Pulseless Ventricular Tachycardia | 4 (16) | 2 (10) | |
| Survival n (%) | |||
| Return of Spontaneous Circulation | 11 (44) | 11 (55) | 0.46 |
| Survival to Hospital Discharge | 3 (12) | 2 (10) | 0.99 |
Weekend indicates time between Friday 11PM and Monday 6:59AM. PEA indicates pulseless electrical activity.
Event-level Analysis
In the primary analysis at the event level, in 2010 CC rate improved (113 ± 11 vs. 104 ± 8 CC/min; p<0.01), depth improved (50 ± 13 vs. 43 ± 9 mm; p=0.047), and CC Fraction increased (0.94 [0.93–0.96] vs. 0.9 [0.85–0.94]; p=0.013) compared to 2005 (Table 2). Compliance at the event level improved for CC Fraction (2010: 16/20 (80%) vs. 2005: 11/25 (44%); p=0.018), but there was a trend towards worsening compliance for rate (2010 13/20 (65%) vs. 23/25 (92%); p=0.057) and depth (9/20 (45%) vs. 18/25 (72%); p=0.066, Table 3). However, when 38mm (2005 Guidelines) was used as an alternative depth compliance target for the 2010 period, there was a non-significant increase in event compliance (17/20 (85%) vs. 18/25 (72%); p=0.47, Table 3), suggesting that depth did improve, but not to 2010 targets.
Table 2.
CPR quality variables. Primary analysis at the event level evaluated as continuous variables.
| 2005 | 2010 | p | |
|---|---|---|---|
|
| |||
| CPR Quality Targets | n = 25 | n = 20 | |
| Rate (CC/min) | 104 ± 8 | 113 ± 11 | < 0.01 |
| Depth (mm) | 43 ± 9 | 50 ± 13 | 0.047 |
| CC Fraction | 0.9 [0.85–0.94] | 0.94 [0.93–0.96] | 0.013 |
| Leaning (%) | 8 [7–13] | 6 [2–13] | 0.24 |
Table 3.
Number (%) of events compliant with CPR guidelines. Targets for 2005 were: depth ≥ 38mm; rate ≥ 90 and ≤ 120/min; CC Fraction > 90%; leaning ≤10% of compressions. Targets for 2010 were: rate ≥ 100/min and ≤ 120/min; CC Fraction > 90%; leaning ≤ 10% of compressions. Depth for 2010 reported both as ≥ 50mm (2010 guidelines) and ≥ 38mm (2005 guidelines)
| 2005 | 2010 | p | |
|---|---|---|---|
|
| |||
| CPR Compliance n (%) | n = 25 | n = 20 | |
| Rate | 23 (92) | 13 (65) | 0.057 |
| Depth (2010 ≥ 50mm) | 18 (72) | 9 (45) | 0.066 |
| Depth (2010 ≥ 38mm) | 18 (72) | 17 (85) | 0.47 |
| CC Fraction | 11 (44) | 16 (80) | 0.018 |
| Leaning | 15 (60) | 14 (70) | 0.49 |
CPR Epoch-level Analysis
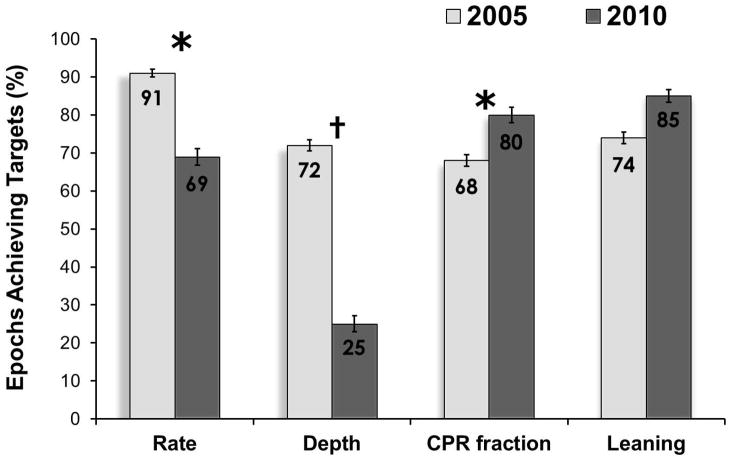
The percentage of epochs meeting Guidelines in 2010 improved (mean (SE)) for CC Fraction (68 (2) vs. 80 (2)) and leaning (74 (2) vs. 85 (2)), but decreased for rate (91 (1) vs. 69 (2)) and depth (72 (2) vs. 25 (2)); p<0.01 for all comparisons. After controlling for within event correlation and the duration of CPR, CPR during the 2010 “after” period was more likely to meet Guidelines for CC Fraction (OR 1.7; CI 95: 1.2–2.4; p<0.01), but less likely for rate (OR 0.23; CI 95: 0.12–0.44; p<0.01), and depth (OR 0.31; CI 95: 0.11–0.86; p=0.024).
In a sensitivity analysis, with the intent to reduce the possibility that rescuers were targeting CPR quality to a patient physiological outcome instead of quantitative depth and rate measurements, findings at the event level of improved rate, depth, and CC Fraction in 2010 were robust when the analysis was limited to those events without arterial lines. This was true also for compliance at the event level which continued to show improved CC Fraction, and a trend towards worse compliance for rate and depth in 2010.
Discussion
To our knowledge, this is the first study to investigate the quality of actual in-hospital pediatric and adolescent CPR performed in acute care areas and its compliance with the 2010 Guidelines. We found that at our institution, CC rate, depth, and CC Fraction improved, but that the targets established in 2010 were difficult to achieve, particularly for CC depth and rate. It is also important to note that these findings were robust when limited to events without invasive arterial lines – a possible alternative target for quality CPR.25,26
In 2010, there was a dramatic shift in the Guidelines from a sequence that emphasized airway management first (A-B-C) to one that focused on providing early high quality chest compressions (C-A-B).12,13 This was best exemplified in the Guidelines’ catchphrase, “Push Hard. Push Fast. Minimize Interruptions.” The notion that deeper, faster minimally interrupted compressions save lives is supported by vast evidence taken from animal27–29 and adult studies.5–7,9,24 This study fills an important gap in knowledge by evaluating whether the Guidelines had the intended effect of improving delivered CC depths, rates, and limiting interruptions.
While the Guidelines are developed using a rigorous evidence evaluation process,30 it is important to note that when compared to adults, relatively little data has been collected from actual children in cardiac arrest. In fact, the decision to increase the CC depth recommendation in 2010 to ~5cm in children was based upon CT19,20 and anthropometric studies21 of healthy children, not those in actual cardiac arrest. However, as injuries from pediatric CPR are rare,31 expert consensus suggested that the real “risk” to the child is for providers to not push hard enough, so the depth for children was increased, even though there was little evidence to suggest that we could achieve such depths in actual practice.
In terms of compression rate, prior to 2010, the focus of quality improvement was to avoid excessively slow rates with less emphasis on the possibility of pushing too fast. This recommendation was driven by animal and adult data that demonstrated either improved CPR physiology32–35 or short term survival9 when inadequate chest compression rates were avoided. Data supporting an upper rate threshold was less robust.33 Ultimately, the recommendation to change from “approximately” to “at least” 100 CC/min was instituted in 2010. Interestingly, in a large recent 2012 out-of-hospital adult cardiac arrest investigation, the Resuscitation Outcomes Consortium demonstrated that odds of short term survival peaked at approximately 125 CC/min and then declined.7 This study supported the concern of some that there may be a risk of increasing recommended CC rates without providing an upper limit, as providers may push at a frequency above a high threshold more commonly, as they did in our study.
Incomplete release between compressions gained more attention in the Guidelines over the last decade. Not only have human studies established this as a particularly problematic CPR error,36,37 animal data has demonstrated worsened CPR physiology and survival when the chest does not fully recoil during compressions.22,38 It is important to note that in this investigation, although providers did provide CC of increased depth and rate, this was not associated with increased leaning between compressions.
In this study, while CPR quality improved, the targets established by the 2010 Guidelines were difficult to achieve, despite an intensive quality improvement (QI) program. Our particular QI initiative focuses on: 1) identifying children at risk for arrest; 2) retraining bedside care providers of these children to perform quality CPR;16–18 3) using CPR recording/feedback-enabled defibrillators to guide CPR quality during resuscitation; and 4) solidifying improved performance through an intensive post-cardiac arrest debriefing program.15 And while we were unable to achieve 2010 Guidelines consistently, the authors do not intend to suggest that these targets are unattainable, as we have deployed and studied only one particular QI program. In short, more work is needed. As an example, the timing, intensity, and content of frequent CPR bedside re-trainings and post-cardiac arrest debriefings, both promising targets that we utilized, should be investigated further in an attempt to improve Guideline compliance and overall resuscitation quality in the future.
This study has several limitations. First, this study was completed in a clinical environment with a long history of CPR quality research, with an active interest and infrastructure to evaluate and improve resuscitation care. How the 2010 Guideline implementation may have affected CPR quality more globally – in hospitals without feedback-enabled defibrillators, daily CPR refresher trainings, and post-cardiac arrest debriefings – remains an unanswered question. Second, due to the size limitations of the existing technology, we were unable to accurately report ventilation quality39 and had limited data on pediatric patients <8 years of age, which importantly comprise the majority of patients receiving CPR in the emergency department. Third, as the software upgrade for audio feedback in accordance with 2010 Guidelines was not available and installed until January 2012, the effect of audio feedback to achieve these new targets was not fully evaluated. Fourth, the effect of mattress deflection was not accounted for in our reporting of CC depth. Our group of investigators has demonstrated that the technology used in this study can overestimate the actual thorax compression by as much as 1.3 cm on soft beds due to mattress compression.40 Therefore, the actual Guideline compliance for CC depth is much worse than reported in this investigation. Finally, due to the small number of arrests studied, attributing changes in survival to implementation of the 2010 Guidelines could not be determined and is an important unanswered question.
Conclusions
At our institution during actual pediatric and adolescent resuscitation attempts, implementation of the 2010 Basic Life Support Guidelines for cardiopulmonary resuscitation resulted in the provision of deeper chest compressions that were performed at higher rates and with less interruption. However, when events were evaluated strictly regarding compliance, the targets established in 2010 were difficult to achieve, particularly for CC depth and rate. Larger studies evaluating improved patient outcomes with implementation of the Guidelines are warranted in pediatrics.
Figure 1.
Percentage of CPR epochs achieving targets (mean (SE)). Targets for 2005 (n=909) were: depth ≥ 38mm; rate ≥ 90 and ≤ 120/min; CC Fraction > 90%; leaning ≤ 10% of compressions. Targets for 2010 (n=427) were: depth ≥ 50mm; rate ≥ 100/min and ≤120/min; CC Fraction > 90%; leaning ≤10% of compressions. Odds of achieving targets calculated using generalized estimating equations to adjust standard errors for within event correlation of CPR epochs. *p<0.01. †p=0.024.
Acknowledgments
This study was supported by a Laerdal Medical Foundation Center of Excellence Grant and the Endowed Chair of Pediatric Critical Care Medicine at the Children’s Hospital of Philadelphia. We would like to thank all members of the Pediatric Intensive Care Unit and Emergency Department multidisciplinary team for supporting resuscitation research at our institution.
Abbreviations
- AHA
American Heart Association
- CPR
cardiopulmonary resuscitation
- CC
chest compression
Footnotes
Conflicts of Interest: The authors acknowledge the following potential conflicts of interest. Vinay Nadkarni, Dana Niles, Akira Nishisaki, and Matt Maltese receive unrestricted research grant support from the Laerdal Foundation for Acute Care Medicine. Robert Sutton is supported through a career development award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (K23HD062629).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Parra DA, Totapally BR, Zahn E, et al. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med. 2000;28(9):3296–3300. doi: 10.1097/00003246-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 2.Slonim AD, Patel KM, Ruttimann UE, Pollack MM. Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. 1997;25(12):1951–1955. doi: 10.1097/00003246-199712000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295(1):50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 4.Girotra S, Spertus JA, Li Y, et al. Survival trends in pediatric in-hospital cardiac arrests: An analysis from get with the guidelines-resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6(1):42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheskes S, Schmicker RH, Christenson J, et al. Perishock pause: An independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation. 2011;124 (1):58–66. doi: 10.1161/CIRCULATIONAHA.110.010736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120(13):1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Idris AH, Guffey D, Aufderheide TP, et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125(24):3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stiell IG, Brown SP, Christenson J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40(4):1192–1198. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: A prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 10.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293(3):305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 11.Sutton RM, Niles D, Nysaether J, et al. Quantitative analysis of CPR quality during inhospital resuscitation of older children and adolescents. Pediatrics. 2009;124(2):494–499. doi: 10.1542/peds.2008-1930. [DOI] [PubMed] [Google Scholar]
- 12.Berg MD, Schexnayder SM, Chameides L, et al. Pediatric basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126(5):e1345–60. doi: 10.1542/peds.2010-2972C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berg RA, Hemphill R, Abella BS, et al. Part 5: Adult basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S685–705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 14.Holmberg M, Holmberg S, Herlitz J. Effect of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients in sweden. Resuscitation. 2000;47(1):59–70. doi: 10.1016/s0300-9572(00)00199-4. [DOI] [PubMed] [Google Scholar]
- 15.Zebuhr C, Sutton RM, Morrison W, et al. Evaluation of quantitative debriefing after pediatric cardiac arrest. Resuscitation. 2012;83(9):1124–1128. doi: 10.1016/j.resuscitation.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niles D, Donoghue A, Kalsi MS, et al. “Rolling refreshers”: A novel approach to maintain CPR psychomotor skill competence. Resuscitation. 2009;80(8):909–912. doi: 10.1016/j.resuscitation.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 17.Sutton RM, Niles D, Meaney PA, et al. “Booster” training: Evaluation of instructor-led bedside cardiopulmonary resuscitation skill training and automated corrective feedback to improve cardiopulmonary resuscitation compliance of pediatric basic life support providers during simulated cardiac arrest. Pediatr Crit Care Med. 2011;12(3):e116–21. doi: 10.1097/PCC.0b013e3181e91271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutton RM, Niles D, Meaney PA, et al. Low-dose, high-frequency CPR training improves skill retention of in-hospital pediatric providers. Pediatrics. 2011;128(1):e145–51. doi: 10.1542/peds.2010-2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kao PC, Chiang WC, Yang CW, et al. What is the correct depth of chest compression for infants and children? A radiological study. Pediatrics. 2009;124(1):49–55. doi: 10.1542/peds.2008-2536. [DOI] [PubMed] [Google Scholar]
- 20.Braga MS, Dominguez TE, Pollock AN, et al. Estimation of optimal CPR chest compression depth in children by using computer tomography. Pediatrics. 2009;124(1):e69–74. doi: 10.1542/peds.2009-0153. [DOI] [PubMed] [Google Scholar]
- 21.Sutton RM, Niles D, Nysaether J, et al. Pediatric CPR quality monitoring: Analysis of thoracic anthropometric data. Resuscitation. 2009;80(10):1137–1141. doi: 10.1016/j.resuscitation.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 22.Zuercher M, Hilwig RW, Ranger-Moore J, et al. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Crit Care Med. 2010;38(4):1141–1146. doi: 10.1097/CCM.0b013e3181ce1fe2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: A prospective interventional study. Resuscitation. 2006;71(3):283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 24.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71(2):137–145. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Sutton RM, Friess SH, Bhalala U, et al. Hemodynamic directed CPR improves short-term survival from asphyxia-associated cardiac arrest. Resuscitation. 2012 doi: 10.1016/j.resuscitation.2012.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friess SH, Bhalala U, Maltese MR, et al. Hemodynamic directed CPR improves short-term survival from asphyxia-associated cardiac arrest. Resuscitation. 2012 doi: 10.1016/j.resuscitation.2012.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ewy GA, Zuercher M, Hilwig RW, et al. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation. 2007;116(22):2525–2530. doi: 10.1161/CIRCULATIONAHA.107.711820. [DOI] [PubMed] [Google Scholar]
- 28.Berg RA, Sanders AB, Kern KB, et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104(20):2465–2470. doi: 10.1161/hc4501.098926. [DOI] [PubMed] [Google Scholar]
- 29.Kern KB, Carter AB, Showen RL, et al. Twenty-four hour survival in a canine model of cardiac arrest comparing three methods of manual cardiopulmonary resuscitation. J Am Coll Cardiol. 1986;7(4):859–867. doi: 10.1016/s0735-1097(86)80348-5. [DOI] [PubMed] [Google Scholar]
- 30.International Liaison Committee on R. The international liaison committee on resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: Neonatal resuscitation. Pediatrics. 2006;117(5):e978–88. doi: 10.1542/peds.2006-0350. [DOI] [PubMed] [Google Scholar]
- 31.Maguire S, Mann M, John N, et al. Does cardiopulmonary resuscitation cause rib fractures in children? A systematic review. Child Abuse Negl. 2006;30(7):739–751. doi: 10.1016/j.chiabu.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Feneley MP, Maier GW, Kern KB, et al. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988;77(1):240–250. doi: 10.1161/01.cir.77.1.240. [DOI] [PubMed] [Google Scholar]
- 33.Fitzgerald KR, Babbs CF, Frissora HA, Davis RW, Silver DI. Cardiac output during cardiopulmonary resuscitation at various compression rates and durations. Am J Physiol. 1981;241(3):H442–8. doi: 10.1152/ajpheart.1981.241.3.H442. [DOI] [PubMed] [Google Scholar]
- 34.Maier GW, Newton JR, Jr, Wolfe JA, et al. The influence of manual chest compression rate on hemodynamic support during cardiac arrest: High-impulse cardiopulmonary resuscitation. Circulation. 1986;74(6 Pt 2):IV51–9. [PubMed] [Google Scholar]
- 35.Wolfe JA, Maier GW, Newton JR, Jr, et al. Physiologic determinants of coronary blood flow during external cardiac massage. J Thorac Cardiovasc Surg. 1988;95(3):523–532. [PubMed] [Google Scholar]
- 36.Niles D, Nysaether J, Nishisaki A, et al. Leaning is common during in-hospital pediatric CPR, and decreased with automated corrective feedback. Resuscitation. 2009;80(5):553–557. doi: 10.1016/j.resuscitation.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 37.Fried DA, Leary M, Smith DA, et al. The prevalence of chest compression leaning during inhospital cardiopulmonary resuscitation. Resuscitation. 2011;82(8):1019–1024. doi: 10.1016/j.resuscitation.2011.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yannopoulos D, McKnite S, Aufderheide TP, et al. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 2005;64(3):363–372. doi: 10.1016/j.resuscitation.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 39.Roberts K, Srinivasan V, Niles DE, et al. Does change in thoracic impedance measured via defibrillator electrode pads accurately detect ventilation breaths in children? Resuscitation. 2010;81(11):1544–1549. doi: 10.1016/j.resuscitation.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 40.Nishisaki A, Nysaether J, Maltese M, et al. Effect of mattress deflection on CPR quality assessment for older children and adolescents. Resuscitation. 2009;80(5):540–545. doi: 10.1016/j.resuscitation.2009.02.006. [DOI] [PubMed] [Google Scholar]