Abstract
The self-medication hypothesis has been proposed to explain comorbidity between PTSD and drinking, whereupon problem drinking develops as an attempt to modulate negative affect and ameliorate PTSD symptoms. Studies have begun utilizing daily monitoring methodologies to refine our understanding of proximal relations between PTSD, affect, and alcohol use. 136 female college drinkers with a past history of sexual victimization and 38 female college drinkers with no past trauma history, completed electronic monitoring of PTSD symptoms, affect, alcohol use, and alcohol cravings, daily for 4 weeks. A two-part mixed hurdle model was used to examine likelihood of drinking and amount of alcohol consumed on drinking days. We did find significant relationships between daily PTSD symptoms, affect, and drinking. On days women experienced more intrusive and behavioral avoidance symptoms of PTSD they experienced stronger urges to drink and were more likely to drink on that day. On days where women experienced more negative affect than their average, they experienced stronger urges to drink whereas on days where women experienced more of the dysphoric symptoms associated with PTSD than their average, they drank less. On days with higher positive affect women reported stronger urges to drink and were more likely to drink. Results suggest the need to examine both aspects of affect and specific PTSD symptoms as they may differentially predict drinking behavior. Differences in the ways in which PTSD symptoms and affect influence drinking suggest that interventions more specifically address the function of drinking behaviors in reducing alcohol use among college women.
Keywords: posttraumatic stress disorder, PTSD, college students, victimization, alcohol use
College women drink more heavily than the general population and their same-age non-college attending peers (Slutske et al., 2004; Slutske, 2005). Approximately 40-45% of students endorse heavy episodic drinking (4 or more drinks per occasion for women, 5 or more for men) over the past month (Dawson, Grant, Stinson, & Chou, 2004; Grucza, Norberg, & Bierut, 2009). This drinking pattern is associated with higher negative consequences of use including increased risk of sexual assault and revictimization (McCauley et al., 2010; Mohler-Kuo et al., 2004).
Exposure to childhood sexual assault or adult sexual victimization are also relatively common among college women (Lauterbach & Vrana, 2002; Purves & Erwin, 2002; Read, Ouimette, White, Colder, & Farrow, 2011). Approximately one quarter of college students (20-32%) report a history of childhood sexual abuse (Messman-Moore, Long, & Siegfried, 2000; Walsh, Blaustein, Knight, Spinazzola, & van der Kolk, 2007). Twenty-five percent of college women report having experienced rape or attempted rape (Fisher, Cullen, & Turner, 2000; Ross, Kolars, Krahn, Gomberg, Clark, & Niehaus, 2011). Approximately 10-15% of college students meet diagnostic criteria for posttraumatic stress disorder (PTSD; Marx & Sloan, 2003; McDevitt-Murphy, Weathers, Flood, Eakin, & Benson, 2007; Twamley, Hami, & Stein, 2004).
Research has found an association between trauma exposure, especially sexual assault, and alcohol use in college students (Abbey, 2002; Goldstein, Flett, & Wekerle, 2010). Sexual assault has been associated with higher rates of binge drinking (Marx, Nichols-Anderson, Messman-Moore, Miranda, & Porter, 2000; Ross et al., 2011). Moreover, sexual assault can result in additional negative outcomes including PTSD (Messman-Moore et al., 2000), which in turn is associated with increased drinking and alcohol-related problems (Hruska & Delahanty, 2012; Messman-Moore, Ward, & Brown, 2009). Indeed, PTSD following trauma is associated with higher drinking problems, higher alcohol consumption, more drinking to intoxication, and higher rates of alcohol abuse/dependence than trauma exposure without PTSD (McDevitt-Murphy et al., 2007; Schuck & Widom, 2001; Stewart, Conrod, Samoluk, Pihl, & Dongier, 2000).
The self-medication hypothesis is the most commonly accepted theory to explain relationships between PTSD and alcohol misuse (Khantzian, 2003; McFarlane, 1998; Stewart, 1996). It postulates that when alcohol is used to alleviate or attenuate psychological distress it functions as a negative reinforcer which over time leads to alcohol problems (Stewart et al., 2000). The self-medication hypothesis does not discriminate between types of psychological distress and has been used to explain multiple psychiatric disorders (PTSD, depression, social anxiety) in relation to problem drinking (Carrigan & Randall, 2003; Robinson, Sareen, Cox, & Bolton, 2009; Swendson et al., 2000).
Given this proposed mechanism of negative reinforcement, research evaluating relationships between alcohol use and psychological distress may seek to capture the distal, long-term nature of the relationship (e.g., does onset of problematic alcohol use follow onset of PTSD?) or identify the more proximal day-to-day relationship between alcohol use and distress or symptoms (e.g., is greater distress associated with greater alcohol consumption that day?). Both types of research are important to evaluating validity of the self-medication hypothesis and both may suggest important refinements to the theory. However, research to date on PTSD and drinking has predominantly utilized cross-sectional and longitudinal methodologies to examine distal associations, and has not examined proximal relationships between negative affect, PTSD symptoms, and drinking. Proximal data collection research designs that incorporate frequent assessment of key constructs such as PTSD symptoms, negative affect, and drinking behavior allow for more nuanced evaluations of the ways in which these constructs may be associated with one another. Rather than simply evaluating whether greater PTSD symptoms or negative affect are associated with increased (or decreased) drinking, such data may be used to determine whether day-to-day symptom variability has an influence on drinking behavior.
Drinking to manage psychological distress (i.e., anxiety or depression) has been associated with higher alcohol use or consequences in college students and community samples (Baer, 2002; Ham & Hope, 2003; Geisner, Larimer, & Neighbors, 2004; Park & Levenson, 2002; Rice & Van Arsdale, 2010). In daily diary or ecological momentary assessment studies negative affect has generally been associated with alcohol consumption (Armeli, Conner, Cullum, & Tennen, 2010; Armeli, Tennen, Affleck, & Kranzler, 2000; Mohr et al., 2001; Rankin & Maggs, 2006; Simons et al., 2005; Simons et al., 2010; Swendsen et al., 2000) and daily reports of stress and negative affect have been associated with increased cravings to drink (Cleveland & Harris, 2010; Oslin, Cary, Slaymaker, Colleran, & Blow, 2009). A few studies have found no main effect of negative affect on alcohol use but have found those relationships when examining specific at risk subgroups of drinkers such as those who drink to cope (Grant, Stewart, & Mohr, 2009; Hussong, Hicks, Levy, & Curran, 2001; Swendson et al., 2000).
In longitudinal studies results have been mixed regarding relationships between PTSD and drinking. While some studies have found a relationship between trauma exposure itself and drinking problems (Read et al., 2012; Ross et al., 2011; Sartor et al., 2010), others have concluded PTSD preceded the onset of drinking problems (Danielson et al., 2009; Wolitzky-Taylor, Bobova, Zinbarg, Mineka, & Craske, 2012), whereas some studies have failed to find relationships between trauma exposure or PTSD and drinking outcomes (Najdowski & Ulllman, 2009; Testa, Livingston, & Hoffman, 2007; Walsh et al., 2012). Despite the robust literature using daily diary or event-level methodologies to examine affect in relation to drinking (Armeli et al., 2010; Grant, Stewart, & Mohr, 2009; Simons et al., 2005), there is a dearth of research using this methodology to examine PTSD and alcohol relationships (Possemato et al., 2012; Simpson, Stappenbeck, Varra, Moore, & Kaysen, 2012). One study to date has used prospective daily monitoring to test relationships between PTSD symptoms and craving for alcohol in a small, predominantly male, sample of individuals initiating treatment for alcohol abuse/dependence (Simpson et al., 2012). Days with greater PTSD severity were associated with greater alcohol craving. The study did not examine drinking behavior itself, thus we cannot tell to what extent PTSD might lead to increased consumption. Moreover, it is unknown to what extent these findings apply to young women or to individuals not seeking substance treatment.
Research attempting to untangle relationships between PTSD and problematic alcohol use has found differences in relationships between specific symptom clusters of PTSD and their relationships with drinking. Re-experiencing and hyperarousal symptoms predict drinking in some studies (Maguen, Stalnaker, McCaslin, & Litz, 2009; McFall, Mackay, & Donovan, 1992; Read, Brown, & Kahler, 2004; Simpson et al., 2012) whereas other studies have found avoidance and emotional numbing are more strongly associated with alcohol misuse (Jakupcak et al., 2010; Kehle et al., 2012). The three symptom clusters proposed by the DSM-IV criteria (American Psychiatric Association, 1994) may not be optimal for describing the disorder's underlying dimensionality (reviewed in Asmundson, Stapleton, & Taylor, 2004) and therefore may contribute to these mixed findings. One empirically supported model of PTSD isolates symptoms that are less PTSD specific, conceptualized as dysphoric, from those which are more conceptually related to the PTSD construct such as hyperarousal, effortful avoidance, and intrusive symptoms (Simms, Watson, & Doebbeling, 2002). In order to more clearly understand which aspects of PTSD may contribute to daily-level relationships with drinking, it may be useful to examine symptoms seen as hallmark features of PTSD such as re-experiencing, avoidance, and hyperarousal, separate from dysphoric symptoms. It also is important to determine whether or not the dysphoric symptoms associated with PTSD are related to drinking in a similar manner to negative affect or are more similar to other symptoms of PTSD.
The present study is an investigation of proximal relationships between trauma-specific symptoms (i.e., intrusion, effortful avoidance, arousal), dysphoria symptoms, and affect in relation to alcohol use and craving among college women engaging in heavy episodic drinking with and without sexual victimization histories. We focused on women engaging in heavy episodic drinking to be able to determine to what extent PTSD symptoms constitute a predictable risk for drinking in a sample of college women known to engage in high risk drinking. Data are from women randomly assigned to a daily monitoring condition as part of a study evaluating feasibility of utilizing Personalized Digital Assistant (PDA) devices to monitor alcohol use, cravings, affect, and PTSD symptoms for 30 days (masked reference). Studies conducted to date have not included individuals who have not experienced traumatic events as a point of comparison. Given that many college women engage in heavy episodic drinking, it is critical to include women who have not been trauma exposed in order to discriminate the observed relationships between psychological distress and drinking from typical college student drinking.
Our first set of questions related to more distal relationships regarding whether sexual victimization history per se or PTSD diagnostic status were associated with overall differences in daily alcohol use and cravings. We hypothesized that women with a history of sexual victimization would report more alcohol use and greater craving for alcohol than those without a history of trauma, and further that women with PTSD would report more alcohol use and greater craving than women with a history of sexual victimization who did not meet criteria for PTSD.
Our second set of questions focused on proximal relationships between daily PTSD symptoms including those considered trauma specific (intrusive symptoms, behavioral avoidance, and hyperarousal) and non-specific (dysphoric symptoms), as well as negative affect and alcohol use. Based on self-medication and negative reinforcement models, we predicted that on days when PTSD symptoms were higher women would experience more cravings, be more likely to drink and when they do, consume more alcohol. We predicted negative affect would also be associated with higher alcohol use and cravings. Exploratory analyses examined the role of positive affect in predicting alcohol use and cravings within this sample.
Method
Participants and Procedures
The sample included 174 undergraduate women over age 18 who completed a 4-week electronic diary monitoring period. A total of 11,544 randomly selected undergraduate women at a large northwest university were mailed and e-mailed an invitation to participate in a 20-minute web screening survey for a study on trauma in college women. Invitations contained a brief study description and instructions to log on to the URL and enter their personal identification number.
Of those invited, 4,342 (37.6%) completed screening and 860 (20%) met study criteria of 1) consuming 4 or more drinks on one occasion at least twice in the past month, and 2) reporting either no history of trauma exposure OR reporting sexual victimization (at least one incident of childhood sexual abuse OR adult sexual assault prior to the past three months). Of these, 834 completed the pre-monitoring survey (97%) in which PTSD severity was determined. Participants were invited to participate in the daily dairy monitoring (n=318, 38%) if they had no prior trauma history or if they had a history of sexual victimization and at least one intrusive and one hyperarousal PTSD symptom in the past month. Eligible participants were asked to schedule a time to come to study offices to receive a PDA and training in study protocols. Of those invited, 174 (55%) participated in the daily monitoring study. The daily monitoring study consisted of 38 no trauma participants, 77 with sexual assault and PTSD, and 59 with sexual assault and no PTSD diagnosis. The no trauma participants were less likely to come in for the daily monitoring study (39%) than participants with sexual assault (60%) or sexual assault and PTSD (66%), χ2(2, n=318) = 16.65, p = .001. Women who enrolled in the daily monitoring study had significantly higher PTSD symptoms at baseline than those who did not, F(1, 316) = 6.35, p = .01. There were no significant differences in alcohol use between women who participated in daily monitoring and those who did not, F(1, 317) = .05, p = .82.
The mean age for the final sample was 20.04 years old (SD = 1.35). Ethnicity included 71.5% White, 14.0% Asian, 7.6% Hispanic/Latino, and 9.3% multi-ethnic. A majority of the trauma-exposed sample had experienced some type of adult sexual victimization (93.4%). These included forcible rapes (21.3%), alcohol involved rapes (53.7%), alcohol involved assaults that did not involve penetration (64.7%), and coercive sexual assaults (61.0%). A sizable minority of the trauma-exposed sample had experienced child sexual abuse (44.9%).
The monitoring study consisted of two assessments daily, one before noon and one after seven p.m., for 30 days. In the training session, participants selected a two-hour block in both the morning and evening to complete assessments. An alarm was set for the start of their assessment window to alert them to complete their surveys. PDA assessments took on average 4 minutes to complete and included questions on location (e.g., home, school), affect (e.g., happy, frustrated), PTSD symptoms (e.g., jumpy/easily startled, irritable), and substance use (e.g., marijuana use, alcohol). Participants were paid $45 for screening and pre-monitoring assessments, $1 for each daily assessment completed, a $2 bonus for completing both assessments in one day, and a $10 bonus for completing 14 assessments (or 7 days) in a row. Participants could earn a total of $215 for completing all assessments. A Federal Certificate of Confidentiality was obtained and all procedures were approved by the university's Institutional Review Board.
Measures
The study was comprised of two phases, a pre-monitoring assessment and a four week monitoring period. Pre-monitoring assessments contained self-report measures on demographics, trauma exposure, PTSD, and alcohol consumption. Daily monitoring assessments contained measures of PTSD, alcohol consumption, and affect.
Pre-monitoring Assessments and Screening Criteria
The Quantity Frequency Questionnaire
(QF; Dimeff, Baer, Kivilhan, & Marlatt 1999) was used as a measure of peak drinking over the past month. Participants were included who endorsed drinking four or more drinks at least twice over the past month. A drink was defined as 12 oz. of beer, 10 oz. of microbrew or wine cooler, 4 oz. of wine, or 1 cocktail with 1 oz. of 100-proof liquor or 1.25 oz. of 80-proof liquor.
Trauma exposure
A modified version of the Traumatic Life Experiences Questionnaire (TLEQ; Kubany et al., 2000) was used. Participants were presented seventeen Criterion A events (i.e., the stressor criterion required for a diagnosis of PTSD according to the DSM-IV [APA, 1994]) and asked how many times they had experienced each event. Response options ranged from 0= no, never to 5= more than 5 times. For participants who reported an event one or more times, follow-up questions regarding the experience of fear, horror, helplessness, or physical injury were asked for each event to establish whether Criterion A of the PTSD DSM-IV diagnosis was met. Response options for follow-up questions were 1= yes and 0= no.
Sexual assault
Sexual assault in adulthood was assessed by the Sexual Experiences Survey (SES; Koss & Gidycz, 1985; Koss & Oros, 1982). Adult sexual assault was defined as “unwanted oral-genital contact, vaginal/anal intercourse, and/or penetration by objects since the age of 14.” Sexual victimization included attempted and completed unwanted oral, vaginal, and anal sexual intercourse. Response options for each of 18 experiences were 1= yes and 0= no.
Childhood sexual abuse
The Childhood Victimization Questionnaire (CVQ; Finkelhor, 1979) assessed sexual victimization prior to age 14. Childhood sexual abuse was defined as “any sexual activity that seemed coercive or forced and occurred before the age of 14 with someone 5 or more years older.” Participants were asked which, if any, of eleven unwanted sexual experiences, ranging from a sexual invitation to intercourse, had happened to them. Response options were 1= yes and 0= no.
PTSD symptomatology
The Posttraumatic Diagnostic Scale (PDS;;Foa, Cashman, Jaycox, & Perry, 1997) was used to assess PTSD symptoms for purposes of study inclusion. Participants were asked how much each PTSD symptom presented had bothered them in the last month. Women with histories of sexual victimization were asked to focus on their worst unwanted sexual experience while women with no past trauma histories were asked to focus on a stressful life event. Response options were based on a Likert scale of 0= not at all to 3= very much. PTSD diagnostic status was assigned based on meeting criteria B (1 intrusive symptom), C (3 avoidance symptoms), and D (2 hyperarousal symptoms) of the DSM-IV (APA, 1994). PTSD symptoms were highest in the group meeting diagnostic criteria for PTSD (No trauma: M = 6.1, SD = 7.2; Trauma no PTSD: M = 7.25, SD = 3.0; PTSD: M = 17.8, SD = 7.6).
Daily Monitoring Assessments
Alcohol consumption
Questions regarding alcohol focused on the participants’ alcohol use for the prior 24 hours. Participants were asked, “How many standard drinks have you had in the past 24 hours?” The same definition of a standard drink used in screening was provided. Standard drinks could be typed into the PDA. If the participant did not consume alcohol, they could either type in 0 or click the response “I did not drink.”
Alcohol craving
Participants were asked the following questions to determine their urge to drink since the last assessment: 1) I really haven't felt like drinking; 2) I felt like I could really use a drink; 3) The idea of drinking has been appealing. Response options were based on a Likert scale of 0= definitely false to 8= definitely true. These items were then summed to create a total scale of daily urges to drink, with the first item being reverse scored. Items demonstrated good internal consistency in the current sample (α = .89).
PTSD symptom checklist
The PTSD Checklist Specific version (PCL-S;;Weathers et al., 1993) was modified to be appropriate for daily assessments (Naragon-Gainey et al., 2012). Monitoring participants were presented 17 PTSD symptoms and were asked how much each symptom bothered them in the past 24 hours. Women with histories of sexual victimization were asked to focus on their worst unwanted sexual experience while women with no past trauma histories were asked to focus on a stressful life event. Response options for each question were based on a Likert scale of 1= not at all to 5= extremely.
The dimensionality of the PCL was examined using exploratory multilevel factor analysis in which between-person and within-person covariance matrices are estimated and then used as inputs to standard factor analysis software (see Reise, Ventura, Nuechterlein, & Kim, 2005). Results using promax, oblique rotation suggested three (similar) factors at both between-person and within-person levels, based on number of item loadings of 0.40 or greater and minimizing cross-loadings. The three factors included an explicit focus on trauma (items 1-8: intrusive memories, nightmares, flashbacks, distress at reminders, physiological arousal at reminders, avoidance of thoughts/feelings, avoidance of activities and situations, and psychogenic amnesia), dysphoric symptoms (items 9-15: loss of interest, emotional isolation, emotional numbing, foreshortened future, sleep disturbance, irritability, concentration problems), and hyperarousal (items 16-17: hypervigilance and excessive startle). Given these results, the PCL was scored in three separate subscales for person means (i.e., between-person subscales) and within-person deviations (i.e., within-person subscales): a) trauma subscale (items 1-8; between-person α = .90, within-person α = .79), b) dysphoria subscale (items 9-15; between-person α = .93, within-person α = .78), and hyperarousal (items 16-17; between-person α = .95, within-person α = .65).
Affect
Affect was assessed by a modified version of the Positive and Negative Affect Scale (PANAS; Watson, Clark, & Tellegen, 1988). Participants were presented with emotions and were asked to report how they were feeling at the time of the assessment. Affect items were selected from the circumplex model of affect including positive and negative valenced words, as well as words reflecting arousal (Russell, 1980; Remington, Fabrigar, & Visser, 2000). Response options included 1= no!!, 2= no??, 3= yes??, and 4= yes!!. A similar multilevel factor analysis procedure to that described for the PCL was used to examine the dimensionality of the PANAS. Multilevel factor analyses supported three (similar) factors at between-person and within-person levels. The three factors included: positive (happy, delighted: between-person α = .61, within-person α = .60), negative (angry, bored, miserable, sad: between-person α = .85, within-person α = .64), and arousal (tired, calm, tense: between-person α = .74, within-person α = .49). Measures of internal consistency are relatively low which may reflect the small number of items. As with the PCL, subscales were scored for both person means and within-person deviations. Analyses were conducted using affect assessed during the previous evening.
Data Analyses
In examining the research questions of the present study, the data analyses had to incorporate two critical aspects of the data. First, there were up to 30 repeated, daily assessments that were correlated within person. Second, the distribution of drinking (i.e., one of the primary outcomes) was strongly skewed with a notable stack of zeroes representing non-drinking days. To incorporate these two qualities of the data, a Bayesian hurdle mixed model was used for drinking, including an over-dispersed Poisson regression for the non-zero counts (Atkins, Baldwin, Zheng, Gallop, & Neighbors, 2012; Hilbe, 2011; Neighbors et al., 2011). Hurdle models are closely related to zero-inflated models, in which an outcome is modeled with two submodels: a logistic model related to zero or not zero (i.e., no drinking vs. any drinking) and a count regression model for non-zero counts (i.e., amount of drinking when there is any drinking). Hurdle models cleanly divide the data at zero, such that all zeroes are modeled in the logistic regression, and a truncated count model is used for non-zero counts (i.e., truncated because zero is not included). Random intercept terms were included in both portions of the model, allowing participants to have different likelihood of drinking at all (i.e., random intercept in logit model) and different average drinking when drinking (i.e., random intercept in count model) and random slopes for within person covariates were assessed using the Deviance Information Criterion (DIC). Intensity of urges to drink was reasonably normally distributed and hence a linear mixed model was used in these analyses (i.e., hierarchical linear or multilevel model).
Our first set of hypotheses related to differences in daily alcohol use and cravings based on trauma exposure and PTSD diagnostic status. To determine whether women meeting PTSD diagnostic criteria would experience stronger urges to drink and would drink more than women who were trauma exposed but did not meet criteria for PTSD or than women with no previous history of trauma exposure, two dummy variables were included in the models: Trauma status (0 = no trauma, 1 = trauma) and PTSD status (0 = no PTSD, 1 = PTSD diagnosis).
Our second set of hypotheses involved daily deviations in three subscales of PTSD symptoms and three subscales of affect. These time-varying covariates include information about both the overall level of the covariate (i.e., average level), as well as the daily deviations from each individual's overall average (i.e., the difference between each day's observation and the overall mean for that individual). To separate between- and within-person components of time-varying covariates, trauma and dysphoria factors of the PCL as well as negative affect from the PANAS were modeled with two predictors: an individual mean (i.e., between-person), and person-centered deviations (i.e., within-person; Curran & Bauer, 2011). Joint tests were also conducted to examine the combined within and between person effects of each covariate. All analyses were conducted in R v2.13.0 (R Development Core Team, 2010) and made extensive use of the MCMCglmm package for Bayesian generalized linear mixed models (Hadfield, 2010).
Results
Descriptive Results
There were 5,220 possible morning and evening assessments, of which participants completed 3,597 (68.9%) morning assessments and 3,382 (64.8%) evening assessments. There was notable variability across individuals in responding. The median number of completed assessments was 23 (out of 30) with interquartile range of 10. At the pre-monitoring assessment participants with trauma exposure but without PTSD reported a mean PCL score of 29.4 (SD = 8.1), and those with PTSD had a mean PCL score of 42.1 (SD = 13.6). Although our sample was recruited to engage in at least some heavy episodic drinking, participants reported no drinking on 69.8% of the days throughout the daily monitoring assessment period. Participants consumed alcohol on average 1.5 (SD = 1.5) days per week, and drank an average of 4.1 (SD = 3.1) drinks per drinking day and 6.3 (SD = 7.4) drinks per week. Table 1 has descriptive statistics and correlations for the primary variables including both the between and within person subscales where appropriate. Drinking urges and alcohol use were correlated, as were subscales of PCL and PANAS at both between and within person levels.
Table 1.
Means, Standard Deviations, and Zero Order Correlations
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Total drinks | 1.25 | 2.56 | - | |||||||||||||
| 2. Urges to drink | 3.61 | 1.12 | 0.23 | - | ||||||||||||
| 3. Trauma M | 1.41 | 0.50 | 0.05 | 0.09 | - | |||||||||||
| 4. Dysphoric M | 1.75 | 0.75 | 0.03 | 0.07 | 0.69 | - | ||||||||||
| 5. Hyperarousal M | 1.67 | 1.00 | 0.02 | 0.05 | 0.72 | 0.72 | - | |||||||||
| 6. Positive M | 2.68 | 0.43 | 0.06 | -0.05 | -0.15 | -0.27 | -0.12 | - | ||||||||
| 7. Negative M | 1.94 | 0.46 | -0.02 | 0.15 | 0.34 | 0.51 | 0.31 | -0.54 | - | |||||||
| 8. Arousal M | 2.46 | 0.36 | -0.05 | 0.15 | 0.25 | 0.32 | 0.25 | -0.51 | 0.60 | - | ||||||
| 9. Trauma D | 0 | 0.39 | 0.03 | 0.05 | 0.01 | 0.00 | 0.01 | -0.01 | 0.01 | 0.01 | - | |||||
| 10. Dysphoric D | 0 | 0.47 | -0.07 | 0.03 | -0.01 | 0.00 | -0.01 | 0.00 | 0.01 | 0.00 | 0.46 | - | ||||
| 11. Hyperarousal D | 0 | 0.53 | -0.02 | 0.00 | 0.00 | 0.01 | 0.00 | 0.00 | 0.00 | 0.01 | 0.30 | 0.39 | - | |||
| 12. Positive D | 0 | 0.65 | 0.18 | 0.00 | 0.00 | 0.01 | 0.01 | -0.01 | -0.01 | 0.00 | -0.02 | -0.15 | -0.03 | - | ||
| 13. Negative D | 0 | 0.50 | -0.11 | 0.04 | 0.01 | 0.01 | 0.00 | 0.00 | -0.02 | -0.01 | 0.06 | 0.17 | 0.07 | -0.63 | - | |
| 14. Arousal D | 0 | 0.52 | -0.11 | 0.05 | 0.01 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | -0.01 | 0.10 | 0.02 | -0.49 | 0.48 | - |
Note. SD = standard deviation; M = person mean (between person) variables; D = deviation from person mean (within person) variables.
Daily Drinking Urge Intensity and Drinking Behavior by Trauma Status and PTSD Diagnosis
A linear mixed model examining the intensity of drinking urges showed no association with trauma status (B = -0.02, 95% CI: -0.24, 0.21), and PTSD diagnosis also failed to reach significance in relationship to urges (B = 0.18, 95% CI: -0.03, 0.40). Taken as a whole, trauma status and PTSD diagnosis did not predict significant differences in drinking or drinking urges.
To examine the effect of trauma status and PTSD diagnosis on daily drinking, the Bayesian hurdle mixed model described earlier was fit. In examining covariates in the logit model (i.e., likelihood of any drinking on a given day), trauma status showed no relationship to the likelihood of drinking (odds ratio [OR] = 0.90, 95% confidence interval [CI]: 0.60, 1.42). PTSD diagnosis was also not significantly related to any drinking (OR = 0.67, 95% CI: 0.43, 1.03). In examining covariates in the count model (i.e., amount of drinking on drinking days), there was similarly no relationship for trauma status (rate ratio [RR] = 1.00, 95% CI: 0.81, 1.25)1. PTSD diagnosis also did not show a significant relationship to amount consumed on drinking days (RR = 1.17, 95% CI: 0.92, 1.40).
Between-Within Associations of Daily PTSD Symptoms and Affect with Drinking Urges and Drinking Behavior
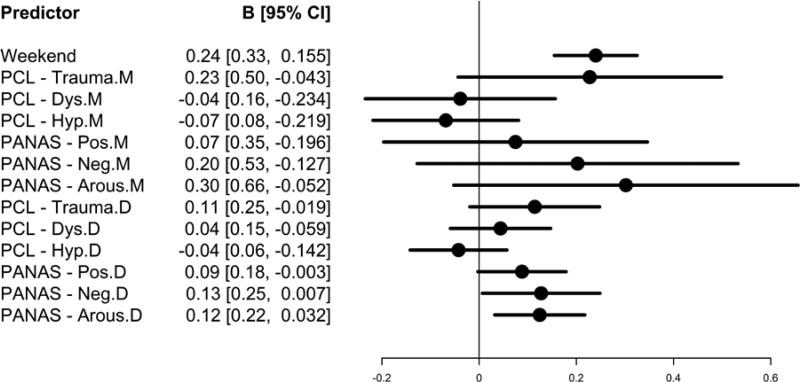
Whereas the previous results examined to what extent individuals’ trauma exposure or PTSD diagnostic status related to daily drinking, the next set of analyses examined to what extent daily PTSD symptoms (trauma-specific, dysphoric, hyperarousal) and affect (negative, positive, arousal) relate to drinking and drinking urges intensity on that same day. Results from fitting a linear mixed model predicting drinking urges from the combined between (i.e., person mean) and within (i.e., deviations from person means) person effects revealed that trauma specific symptoms (b = 0.17, p < .05) and affective arousal (b = 0.21, p < .05) were positively associated with drinking urges. Dysphoric symptoms (b = 0.003, p > .05), hyperarousal symptoms (b = -0.06, p > .05), and both positive (b = 0.08, p > .05) and negative (b = 0.17, p > .05) affect were not significantly associated with drinking urges when the between and within effects were considered jointly. As noted earlier, all covariates were also modeled using both between person and within person components separately. Results are shown in Figure 1, which reports the regression results as well as a dotplot of regression coefficients and 95% confidence intervals (CI; Gelman, Pasarica, & Dodhia, 2002). The CIs for between-person covariates are notably wider than within-person covariates, reflecting in part that there are many more repeated measures than people. Greater drinking urges were observed on weekends compared to weekdays. There were no significant between-person effects of the covariates on urges to drink. Within-person covariates revealed several significant associations with drinking urges, including each of the three PANAS subscales all positively related to drinking urges (p = .052 for the deviation from person means on positive affect).
Figure 1.
Between (M) and within (D) person effects of daily PTSD symptoms and affect on drinking urges. Regression coefficients as well as 95% confidence intervals (CI) are presented in the dotplot. Predictors with CIs that include zero are nonsignificant.
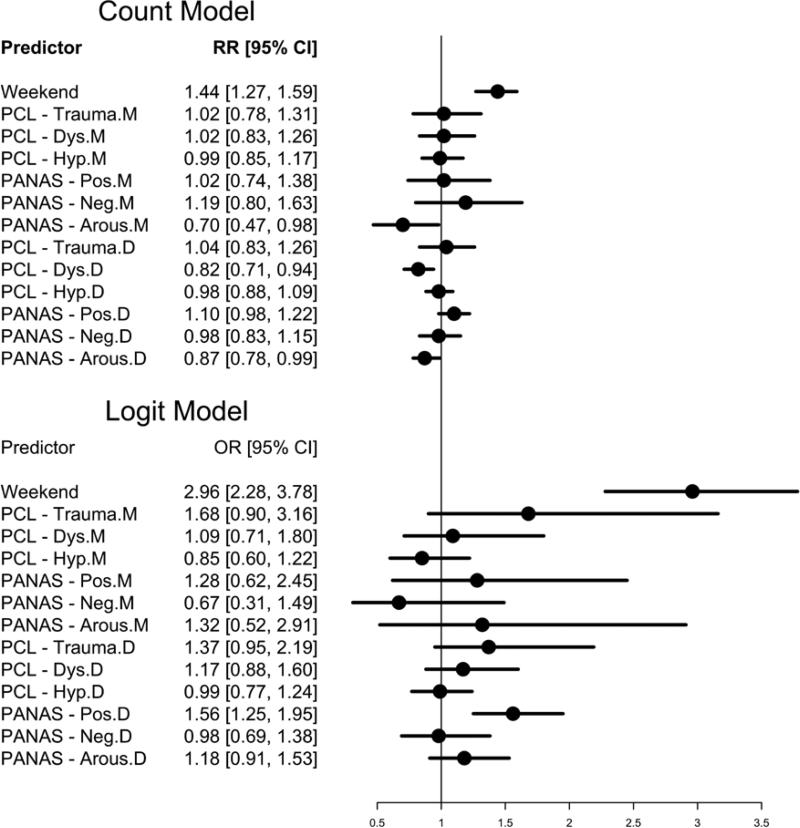
Next, we conducted a Bayesian hurdle mixed model predicting drinking, with the combined between person and within person covariates in both the count (i.e., amount of drinking on drinking days) and logit (i.e., likelihood of any drinking on a given day) models. In the count submodel, greater drinking occurred on weekends relative to weekdays. In the joint test of the between and within person effects, PANAS arousal was negatively associated with greater drinking (b = -0.25, p < .05) whereas trauma (b = 0.03, p > .05), dysphoric (b = -0.09, p > .05), and hyperarousal (b = -0.02, p > .05) symptoms, and positive (b = 0.06, p > .05) and negative affect (b = 0.08, p > .05) were not significant predictors of amount of drinking. Figure 2 reports results for the between and within effects separately in both the count (top half of Figure 2) and logit (bottom half of Figure 2) models. Individuals who reported higher mean arousal on the PANAS reported lower mean drinking (when they did drink). Days with higher dysphoric symptoms and higher arousal were associated with lower mean drinking, whereas there was a nonsignificant trend for days with more positive mood to be associated with higher mean drinking (p = .06).
Figure 2.
The effects of daily PTSD symptoms and affect on drinking behavior. The count and logit models each contain both between (M) and within (D) person effects. Rate ratios (RR) or odds ratios (OR) as well as 95% confidence intervals (CI) are presented in the dotplot. Predictors with CIs that include zero are nonsignificant.
In the logit submodel, drinking was more likely to occur on weekends compared to weekdays. The joint test of the between and within person effects suggested that trauma symptoms were positively associated with likelihood of any drinking (b = 0.42, p < .05). Additionally, the joint test revealed a positive association between positive affect and any drinking (b = 0.34, p < .05). Dysphoric (b = 0.12, p > .05) and hyperarousal (b = -0.09, p > .05) symptoms and negative (b = -0.21, p > .05) and arousal (b = 0.22, p > .05) affect were not related to any drinking when the between and within effects were considered together. The separate tests of between and within effects suggested that there were no significant between person effects of the covariates on any drinking. Days with higher positive affect were significantly related to the likelihood of any drinking, however, neither the within nor the between person effects of trauma symptoms were significantly associated with any drinking when considered separately despite a significant joint test.
Finally, several exploratory moderation analyses were examined, considering weekday vs. weekend effects or PTSD status (i.e., no trauma, trauma but no PTSD, trauma with PTSD) as potential moderators of between-within associations on drinking urges and actual drinking behavior. In both cases the larger, moderation models fit significantly worse using the DIC criterion.
Discussion
The present study is an investigation of the day-to-day relationships between PTSD symptoms, affect, and alcohol use and cravings among heavier drinking college women. We examined both more distal relationships such as the relationship between trauma exposure or PTSD diagnosis on daily drinking, and then examined more proximal relationships between symptoms, affect, and drinking behavior. Contrary to our hypotheses, we did not find significant differences between these groups of women on actual drinking behavior or urges to drink alcohol. Moreover, trauma exposure and PTSD diagnoses did not moderate daily level relationships between daily experiences of PTSD symptoms, affect, and drinking.
However, when we looked at proximal aspects of those relationships we found more complex and nuanced relationships between various aspects of PTSD symptoms and affect in relation to drinking behavior that were generally supportive of the self-medication hypothesis. On days when women experienced higher trauma specific symptoms (i.e., intrusive and behavioral avoidance symptoms of PTSD) they experienced stronger urges to drink and were more likely to drink on that day. Similarly, on days when women had a greater positive deviation from their average level of affective arousal or negative affect they also experienced stronger urges to drink. These results support the idea that individuals avoid the distressing symptoms of PTSD and negative affect through drinking or experiencing urges to drink alcohol, although it does not appear to influence how much they drink. These results are somewhat in contrast with other research on the influence of PTSD symptoms on alcohol cravings in which only the hyperarousal symptoms of PTSD were associated with increased cravings (Simpson et al., 2012). Some of this may reflect measurement issues as the prior research only included a subset of PTSD symptoms compared to the full range of symptoms included in the present study, or may reflect sample differences. It is possible that for heavier drinking women who are not treatment-seeking chronic problem drinkers, the increased desire to drink to manage distress may be driven by the intrusive symptoms. However, in response to chronic problem drinking, it may be the psychophysiological arousal that becomes associated with greater urges to drink. This latter explanation is consistent with our findings regarding the positive association between affective arousal and urges to drink.
Contrary to our hypotheses, on days where women experienced more of the dysphoric symptoms associated with PTSD than their average, they drank less. This pattern of results appears contrary to what would be expected based on a self-medication explanation. The negative association observed between dysphoric symptoms and alcohol consumption may be explained in part by the type of symptoms the women experienced. Daily monitoring studies that have examined the relation between specific negative emotions and drinking have found different patterns of results for different negative emotions (Hussong et al., 2001; Hussong, Galloway, & Feagans, 2005). For example, Hussong and colleagues (2005) found that among individuals who used alcohol to cope, greater sadness was associated with decreased daily alcohol consumption, whereas moderate to high levels of fear and shyness were associated with a decreased likelihood to drink. Dysphoric symptoms may also be related to symptoms of depression including social isolation, decreased behavioral activation, or increased somnolence, which together may result in fewer opportunities to drink in a college setting where most alcohol access is through social provision in party settings. Trauma-specific symptoms such as nightmares and avoidance may present with different constellation of activation and more urgent desire to self-medicate. Although we did not examine the relationships between specific negative emotions and drinking, our finding that days when trauma-specific symptoms were more severe were associated with greater likelihood of drinking while days with greater dysphoric symptoms were associated with drinking fewer drinks does lend credence to the idea that drinking behavior may vary as a function of the specific types of affect or symptoms experienced.
In contrast, weekend drinking was a strong predictor of all drinking outcomes, with women reporting being more likely to drink, drinking more, and experiencing more urges to drink on weekends compared to weekdays. On days when women experienced less affective arousal than normal (i.e., they were more calm, less tired, and less tense) they consumed more drinks if they drank. Additionally, days where women reported a greater positive affect than they typically report they were more likely to drink that same day, and to a lesser extent had stronger urges to drink and drank more overall. This is consistent with other daily level studies that have found positive within-persons relationships between higher positive affect being associated with more frequent and heavier drinking (Armeli et al., 2000; Rankin & Maggs, 2006; Simons et al., 2005). This may reflect more normative, yet still risky, college student drinking patterns (Kuntsche & Cooper, 2010) and may reflect the use of alcohol to have fun, to seek excitement, and influence positive mood and experiences (Mohr et al., 2001; Molnar, Busseri, Perrier, & Sadava, 2009). However, these findings are also consistent with other studies that found that women with histories of sexual victimization also drink to enhance positive affect (Grayson & Nolen-Hoeksema, 2005). PTSD is associated with emotional numbing, trouble with interpersonal connections, and difficulty with enjoyment of activities. Although women may not be explicitly self-medicating those symptoms, they may use alcohol as a means of enhancing pleasant emotional experiences that are harder for them to experience.
There are several important clinical implications resulting from these findings. First, it may be important to identify day-to-day fluctuations in specific symptoms of PTSD as possible triggers for problematic drinking rather than simply PTSD symptoms more generally. Clinicians should pay particular attention to changes in symptoms of re-experiencing and avoidance of trauma cues as increases in these symptoms could indicate a greater likelihood of drinking. For women in PTSD treatments this has particular import as increases in these symptoms could lead to increased alcohol cravings. Thus, among young women who engage in heavier drinking patterns it may be useful to identify alternative ways of coping particularly with intrusive and avoidance symptoms, as well as with negative affect. Targeting these symptoms has the potential to support women who may be reducing their drinking and may thereby mitigate the risk of developing alcohol use disorders over time (Stewart et al., 2000). Skills such as cognitive correction, relaxation, mindfulness, or seeking social support might be useful alternatives to alcohol use to help these women cope with periodic increases in memories about the event, nightmares, or attempts to avoid trauma-related cues and affect (Back, Killeen, Foa, Santa Ana, Gros, & Brady 2012; Daley & Marlatt, 2006; Donovan, Padin-Rivera, & Kowaliw, 2001; Marlatt & Donovan, 2005). Increasing women's ability to identify days of higher trauma-specific symptoms as high-risk situations for increased drinking urges and likelihood of drinking as well as the potential harmful consequences of this pattern of drinking for maintaining trauma symptoms may also be useful. Although positive deviations in dysphoric symptoms were related to drinking less on drinking days in this sample, this may still lead to other maladaptive coping strategies to deal with distress rather than drinking alcohol. Thus, understanding the full range of symptoms women experience and how they cope with these symptoms remains a priority.
Although our findings regarding the role of positive affect and drinking may not be surprising in the context of the general college drinking literature, these findings do highlight some particular risks for this population. As stated earlier, women with prior sexual victimization histories are at elevated risk for sexual revictimization and, in particular, alcohol-related sexual revictimization. Drinking in celebratory settings such as bars and parties is associated with higher victimization risk. If these women are drinking to enhance positive emotions or to increase their feelings of affective arousal this may place them at risk. Moreover, interventions associated with coping motivated drinking may not address these behaviors. These results highlight the importance of considering the function of drinking behavior within the context of that student's symptoms and experiences in reducing higher risk drinking patterns
There were several limitations of the current investigation. First, because our daily data on PTSD and drinking was collected once per day, we cannot determine whether PTSD symptoms preceded drinking behavior. This also increased the possibility that the restrospective nature of recalling PTSD and drinking at the same time influenced people's responses. Although these measurement timing issues cannot be ruled out as factors explaining our results we feel more confident about the findings given similarities between our findings on affect and PTSD in relation to drinking, as affect was measured during the preceding time point.
Another limitation is that our sample was comprised of women attending a competitive college which means we may have excluded women with a greater difficulty related to their trauma history or drinking, who would have been unable to function well enough to attend school or fulfill other role obligations. Women were also selected for this study who were already engaging in higher risk drinking. Although heavy episodic drinking is common among college women, the study design does mean we cannot address whether our results would differ for women who drink in less risky ways nor can we address broader issues regarding PTSD and affect among nondrinkers. We also did not assess negative consequences of drinking, which would be an important area to consider for future research (Simons et al., 2005). In some longitudinal and cross-sectional studies negative affect and PTSD symptoms are associated with higher negative consequences associated with drinking, rather than increases in consumption per se (Geisner et al. 2004; Simons et al., 2005; Read et al., 2012). It may be that women are drinking similar amounts but are having more consequences. Similarly, we also did not assess whether ratings of affect or dysphoria reflect hangover symptoms.
We had a response rate to the initial survey that was low, although it was within the range of other large college student surveys. Our conclusions should be considered in light of findings that students who are extremely heavy drinkers are less likely to participate in alcohol studies (Neighbors, Palmer, & Larimer, 2004). This may also have affected our compliance rate (i.e., just under 70%) with the daily monitoring procedures. It is possible this could have biased results if women differentially complied with the monitoring protocol based on PTSD levels or drinking behavior. Although a possibility, there was significant variability in both PTSD symptom levels and drinking behavior observed throughout the monitoring period suggesting women were in fact responding even when symptoms were greater or they had consumed alcohol the previous day.
In sum, these findings indicate that exposure to trauma or a diagnosis of PTSD did not significantly predict drinking behavior among heavy drinking college women more generally. However, daily fluctuations in PTSD symptoms and affect do influence drinking behaviors. Consistent with self-medication theory increased trauma specific symptoms (i.e., intrusive and behavioral avoidance symptoms) of PTSD influence both desire to drink and likelihood to drink on that same day. However, other symptoms of PTSD may be associated with reduced drinking in the short-term. Moreover, the role of positive affect and celebratory drinking among college women cannot be dismissed even among women who may be distressed and who have experienced sexual victimization. Although neither PTSD nor trauma exposure moderated these daily findings, continued research on other potential moderators, including drinking motives and expectancies, may help shed light on these associations. These findings reinforce the need for mental health practitioners and other treatment providers to pay particularly close attention to the day-to-day changes in symptoms to help clients identify patterns that may contribute to drinking or other behavioral risks.
Acknowledgments
Preparation of this article was supported in part by National Institute on Alcohol Abuse and Alcoholism Grants R01AA020252 (PI: Kaysen), R21AA016211 (PI: Kaysen) and T32AA007455 (PI: Larimer). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health, the University of Washington, or the Veterans Affairs Puget Sound Health Care System.
Footnotes
Count regression models such as Poisson regression use a log link function that guarantees that predictions from the model are within the allowable range of the outcome (i.e., never negative). Similar to logistic regression, coefficients are typically exponentiated (i.e., raised to base e) and are interpreted as rate ratios. Rate ratios reflect percentage increases / decreases in the outcome per unit change in the covariate, and 95% CI that exclude one are significant at the p < .05 level.
References
- Abbey A. Alcohol-related sexual assault: A common problem among college students. Journal of Studies on Alcohol. 2002;(SUPPL 14):118–128. doi: 10.15288/jsas.2002.s14.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Armeli S, Conner TS, Cullum J, Tennen H. A longitudinal analysis of drinking motives moderating the negative affect-drinking association among college students. Psychology of Addictive Behavior. 2010;24:38–47. doi: 10.1037/a0017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armeli S, Tennen H, Affleck G, Kranzler HR. Does affect mediate the association between daily events and alcohol use? Journal of Studies on Alcohol. 2000;61:862–871. doi: 10.15288/jsa.2000.61.862. [DOI] [PubMed] [Google Scholar]
- Asmundson GG, Stapleton JA, Taylor S. Are avoidance and numbing distinct PTSD symptom clusters?. Journal of Traumatic Stress. 2004;17:467–475. doi: 10.1007/s10960-004-5795-7. doi:10.1007/s10960-004-5795-7. [DOI] [PubMed] [Google Scholar]
- Atkins DC, Baldwin S, Zheng C, Gallop RJ, Neighbors C. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychology of Addictive Behaviors. 2012 Aug 20; doi: 10.1037/a0029508. Advance online publication. doi: 10.1037/a0029508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back SE, Killeen T, Foa EB, Santa Ana EJ, Gros DF, Brady KT. Use of an integrated therapy with prolonged exposure to treat PTSD and comorbid alcohol dependence in an Iraq Veteran. American Journal of Psychiatry. 2012;169:688–691. doi: 10.1176/appi.ajp.2011.11091433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS. Student factors: Understanding individual variation in college drinking. Journal of Studies on Alcohol. 2002;(SUPPL 14):40–53. doi: 10.15288/jsas.2002.s14.40. [DOI] [PubMed] [Google Scholar]
- Carrigan MH, Randall CL. Self-medication in social phobia: A review of the alcohol literature. Addictive Behaviors. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Cleveland HH, Harris KS. The role of coping in moderating within-day associations between negative triggers and substance use cravings: A daily diary investigation. Addictive behaviors. 2010;35(1):60–63. doi: 10.1016/j.addbeh.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models for change. Annual Review of Psychology. 2011;62:583–619. doi: 10.1146/annurev.psych.093008.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley DC, Marlatt GA. Overcoming your alcohol and drug problem: Effective recovery strategies (2nd ed.): Therapist guide. Oxford University Press; New York: 2006. [Google Scholar]
- Danielson CK, Amstadter AB, Dangelmaier RE, Resnick HS, Saunders BE, Kilpatrick DG. Trauma-related risk factors for substance abuse among male versus female young adults. Addictive Behaviors. 2009;34:395–399. doi: 10.1016/j.addbeh.2008.11.009. doi;10.1016/j.addbeh.2008.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. Journal of Studies on Alcohol and Drugs. 2004;65(4):477. doi: 10.15288/jsa.2004.65.477. [DOI] [PubMed] [Google Scholar]
- Dimeff L, Baer J, Kvilahan D, Marlatt AG. Brief alcohol screening and intervention for college students: A harm reduction approach (BASICS) Guilford; NY: 1999. [Google Scholar]
- Donovan B, Padin-Rivera E, Kowaliw S. ‘Transcend’: Initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. Journal of Traumatic Stress. 2001;14(4):757–772. doi: 10.1023/A:1013094206154. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. What's wrong with sex between adults and children? Ethics and the problem of sexual abuse. American Journal of Orthopsychiatry. 1979;49:692–697. doi: 10.1111/j.1939-0025.1979.tb02654.x. [DOI] [PubMed] [Google Scholar]
- Fisher BS, Cullen FT, Turner MG. The sexual victimization of college women (NCJ 182369). Bureau of Justice Statistics, National Institute of Justice; Washington, DC US: 2000. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. doi:10.1037/1040-3590.9.4.445. [Google Scholar]
- Geisner I, Larimer ME, Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. doi:10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Gelman A, Pasarica C, Dodhia R. Let's practice what we preach: using graphs instead of tables. American Statistician. 2002;56:121–130. [Google Scholar]
- Goldstein AL, Flett GL, Wekerle C. Child maltreatment, alcohol use and drinking consequences among male and female college students: An examination of drinking motives as mediators. Addictive Behaviors. 2010;35:636–639. doi: 10.1016/j.addbeh.2010.02.002. doi:10.1016/j.addbeh.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Grant VV, Stewart SH, Mohr CD. Coping-anxiety and coping-depression motives predict different daily mood-drinking relationships. Psychology of Addictive Behaviors. 2009;23:226–237. doi: 10.1037/a0015006. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Norberg KE, Bierut LJ. Binge drinking among youth and young adults in the United States: 1979–2006. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(7):692. doi: 10.1097/CHI.0b013e3181a2b32f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadfield JD. MCMC methods for multi-response generalized linear mixed models: The MCMCglmm R package. Journal of Statistical Software. 2010;33:1–22. [Google Scholar]
- Ham LS, Hope DA. College students and problematic drinking: A review of the literature. Clinical Psychology Review. 2003;23:719–759. doi: 10.1016/s0272-7358(03)00071-0. doi:10.1016/S0272-7358(03)00071-0. [DOI] [PubMed] [Google Scholar]
- Hilbe J. Negative binomial regression. 2nd ed Cambridge; New York: 2011. [Google Scholar]
- Hruska B, Delahanty DL. Application of the stressor vulnerability model to understanding posttraumatic stress disorder (PTSD) and alcohol-related problems in an undergraduate population. Psychology of Addictive Behaviors. 2012 doi: 10.1037/a0027584. Advance online publication. doi: 10.037/a0027584. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Galloway CA, Feagans LA. Coping motives as a moderator of daily mood-drinking covariation. Journal of Studies on Alcohol. 2005;66:344–353. doi: 10.15288/jsa.2005.66.344. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology. 2001;110:449–461. doi: 10.1037//0021-843x.110.3.449. [DOI] [PubMed] [Google Scholar]
- Jahng S, Solhan MB, Tomko RL, Wood PK, Piasecki TM, Trull TJ. Affect and alcohol use: An ecological momentary assessment study of outpatients with borderline personality disorder. Journal of Abnormal Psychology. 2011;120(3):572–584. doi: 10.1037/a0024686. doi:10.1037/a0024686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Tull MT, McDermott MJ, Kaysen D, Hunt S, Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors. 2010;35:840–843. doi: 10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Kehle SM, Ferrier-Auerbach AG, Meis LA, Arbisi PA, Erbes CR, Polusny MA. Predictors of postdeployment alcohol use disorders in National Guard soldiers deployed to Operation Iraqi Freedom. Psychology of Addictive Behaviors. 2012;26:42–50. doi: 10.1037/a0024663. doi:10.1037/a0024663. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The Self-Medication Hypothesis Revisited: The Dually Diagnosed Patient. Primary Psychiatry. 2003;10:47–48. 53–54. [Google Scholar]
- King G, Tomz M, Wittenberg J. Making the most of statistical analyses: Improving interpretation and presentation. American Journal of Political Science. 2000;44:341–355. [Google Scholar]
- Koss MP, Gidycz CA. Sexual Experiences Survey: Reliability and validity. Journal of Consulting and Clinical Psychology. 1985;53:422–423. doi: 10.1037//0022-006x.53.3.422. doi:10.1037/0022-006X.53.3.422. [DOI] [PubMed] [Google Scholar]
- Koss MP, Oros CJ. Sexual Experiences Survey: A research instrument investigating sexual aggression and victimization. Journal of Consulting and Clinical Psychology. 1982;50:455–457. doi: 10.1037//0022-006x.50.3.455. doi:10.1037/0022-006X.50.3.455. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen M, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. doi:10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lauterbach D, Vrana S. Relationship Between Trauma Exposure and Substance Use in a Sample of College Students. Journal of Trauma Practice. 2002;1:77–94. [Google Scholar]
- Maguen S, Stalnaker M, McCaslin S, Litz BT. PTSD subclusters and functional impairment in Kosovo peacekeepers. Military Medicine. 2009;174:779–785. doi: 10.7205/milmed-d-03-2808. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Donovan DM. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. 2nd ed Guilford Press; New York: 2005. [Google Scholar]
- Marx BP, Nichols-Anderson C, Messman-Moore T, Miranda J, Porter C. Alcohol consumption, outcome expectancies, and victimization status among female college students. Journal of Applied Social Psychology. 2000;30:1056–1070. doi:10.1111/j.1559-1816.2000.tb02510.x. [Google Scholar]
- Marx BP, Sloan DM. The effects of trauma history, gender, and race on alcohol use and posttraumatic stress symptoms in a college student sample. Addictive Behaviors. 2003;28:1631–1647. doi: 10.1016/j.addbeh.2003.08.039. doi:10.1016/j.addbeh.2003.08.039. [DOI] [PubMed] [Google Scholar]
- McCauley JL, Calhoun KS, Gidycz CA. Binge drinking and rape: A prospective examination of college women with a history of previous sexual victimization. Journal of interpersonal violence. 2010;25(9):1655–1668. doi: 10.1177/0886260509354580. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Weathers FW, Flood AM, Eakin DE, Benson TA. The utility of the PAI and the MMPI-2 for discriminating PTSD, depression, and social phobia in trauma-exposed college students. Assessment. 2007;14:181–195. doi: 10.1177/1073191106295914. doi:10.1177/1073191106295914. [DOI] [PubMed] [Google Scholar]
- McFall ME, Mackay PW, Donovan DM. Combat-related posttraumatic stress disorder and severity of substance abuse in Vietnam veterans. Journal of Studies on Alcohol. 1992;53:357–363. doi: 10.15288/jsa.1992.53.357. [DOI] [PubMed] [Google Scholar]
- McFarlane AC. Epidemiological evidence about the relationship between PTSD and alcohol abuse: The nature of the association. Addictive Behaviors. 1998;23:813–826. doi: 10.1016/s0306-4603(98)00098-7. doi:10.1016/S0306-4603(98)00098-7. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ, Siegfried NJ. The revictimization of child sexual abuse survivors: An examination of the adjustment of college women with child sexual abuse, adult sexual assault, and adult physical abuse. Child Maltreatment. 2000;5:18–27. doi: 10.1177/1077559500005001003. doi:10.1177/1077559500005001003. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Ward RM, Brown AL. Substance use and PTSD symptoms impact the likelihood of rape and revictimization in college women. Journal of Interpersonal Violence. 2009;24:499–521. doi: 10.1177/0886260508317199. doi:10.1177/0886260508317199. [DOI] [PubMed] [Google Scholar]
- Mohler-Kuo M, Dowdall GW, Koss MP, Wechsler H. Correlates of rape while intoxicated in a national sample of college women. Journal of Studies on Alcohol and Drugs. 2004;65(1):37. doi: 10.15288/jsa.2004.65.37. [DOI] [PubMed] [Google Scholar]
- Mohr CD, Armeli S, Tennen H, Carney MA, Aflleck G, Hromi A. Daily interpersonal experiences, context, and alcohol consumption: Crying in your beer and toasting good times. Journal of Personality and Social Psychology. 2001;80:489–500. doi: 10.1037/0022-3514.80.3.489. [DOI] [PubMed] [Google Scholar]
- Molnar DS, Busseri MA, Perrier CP, Sadava SW. A longitudinal examination of alcohol use and subjective well-being in an undergraduate sample. Journal of studies on alcohol and drugs. 2009;70(5):704. doi: 10.15288/jsad.2009.70.704. [DOI] [PubMed] [Google Scholar]
- Najdowski CJ, Ullman SE. Prospective effects of sexual victimization on PTSD and problem drinking. Addictive Behavior. 2009;34:965–968. doi: 10.1016/j.addbeh.2009.05.004. doi:10.1016/j.addbeh.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Atkins DC, Lewis MA, Lee CM, Kaysen D, Mittmann A, Rodriguez LM. Event-specific drinking among college students. Psychology of Addictive Behaviors. 2011;25:702–707. doi: 10.1037/a0024051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Palmer RS, Larimer ME. Interest and participation in a college student intervention study as a function of typical drinking. Journal of Studies on Alcohol. 2004;65:736–740. doi: 10.15288/jsa.2004.65.736. [DOI] [PubMed] [Google Scholar]
- Oslin DW, Cary M, Slaymaker V, Colleran C, Blow FC. Daily ratings measures of alcohol craving during an inpatient stay define subtypes of alcohol addiction that predict subsequent risk for resumption of drinking. Drug and alcohol dependence. 2009;103(3):131–136. doi: 10.1016/j.drugalcdep.2009.03.009. [DOI] [PubMed] [Google Scholar]
- Park CL, Levenson MR. Drinking to cope among college students: Prevalence, problems and coping processes. Journal of Studies on Alcohol. 2002;63:486–497. doi: 10.15288/jsa.2002.63.486. [DOI] [PubMed] [Google Scholar]
- Possemato K, Kaier E, Wade M, Lantinga LJ, Maisto SA, Ouimette P. Assessing daily fluctuations in posttraumatic stress disorder symptoms and substance use with interactive voice response technology: Protocol compliance and reactions. Psychological Services. 2012;9:185–196. doi: 10.1037/a0027144. doi:10.1037/a0027144. [DOI] [PubMed] [Google Scholar]
- Purves DG, Erwin PG. A study of posttraumatic stress in a student population. Journal of Genetic Psychology. 2002;163:89–96. doi: 10.1080/00221320209597970. doi:10.1080/00221320209597970. [DOI] [PubMed] [Google Scholar]
- R Development Core Team . R: A language and environment for statistical computing [Software] R Foundation for Statistical Computing; Vienna, Austria: 2010. [Google Scholar]
- Rankin LA, Maggs JL. First-year college student affect and alcohol use: Paradoxical within-and between-person associations. Journal of youth and adolescence. 2006;35(6):925–937. [Google Scholar]
- Read JP, Brown PJ, Kahler CW. Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors. 2004;29:1665–1672. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM–IV–TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3:148–156. doi: 10.1037/a0021260. doi:10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, Swartout A. Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. 2012 doi: 10.1037/a0028210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remington NA, Fabrigar LR, Visser PS. Reexamining the circumplex model of affect. Journal of Personality and Social Psychology; Journal of Personality and Social Psychology. 2000;79(2):286. doi: 10.1037//0022-3514.79.2.286. [DOI] [PubMed] [Google Scholar]
- Rice KG, Van Arsdale AC. perceived stress, drinking to cope, and alcohol-related problems among college students. Perfectionism. Journal of Counseling Psychology. 2010;57(4):439. [Google Scholar]
- Reise SP, Ventura J, Nuechterlein KH, Kim KH. An illustration of multilevel factor analysis. Journal of personality assessment. 2005;84(2):126–136. doi: 10.1207/s15327752jpa8402_02. [DOI] [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox BJ, Bolton J. Self-medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. Journal of Anxiety Disorders. 2009;23:38–45. doi: 10.1016/j.janxdis.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Ross LT, Kolars CLK, Krahn DD, Gomberg ESL, Clark G, Niehaus A. Nonconsensual sexual experiences and alcohol consumption among women entering college. Journal of Interpersonal Violence. 2011;26:399–413. doi: 10.1177/0886260510363418. [DOI] [PubMed] [Google Scholar]
- Russell JA. A circumplex model of affect. Journal of Personality and Social Psychology. 1980;39:1161–1178. [Google Scholar]
- Sartor CE, McCutcheon VV, Pommer NE, Nelson EC, Duncan AE, Waldron M, Heath AC. Posttraumatic stress disorder and alcohol dependence in young women. Journal of Studies on Alcohol and Drugs. 2010;71:810–818. doi: 10.15288/jsad.2010.71.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuck AM, Widom C. Childhood victimization and alcohol symptoms in females: Causal inferences nd hypothesized mediators. Child Abuse and Neglect. 2001;25:1069–1092. doi: 10.1016/s0145-2134(01)00257-5. doi:10.1016/S0145-2134(01)00257-5. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbelling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843x.111.4.637. doi:10.1037/0021-843X.111.4.637. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Oliver MN, Bush JA, Palmer MA. An experience sampling study of associations between affect and alcohol use and problems among college students. Journal of Studies on Alcohol and Drugs. 2005;66(4):459. doi: 10.15288/jsa.2005.66.459. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Batien BD, Wray TB. Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive behaviors. 2010;35(12):1045–1053. doi: 10.1016/j.addbeh.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Varra AA, Moore SA, Kaysen D. Symptoms of posstraumatic stress predict craving among alcohol treatment seekers: Results of a daily monitoring study. Psychology of Addictive Behaviors. 2012 Feb 2; doi: 10.1037/a0027169. Advance online publication. doi:10.1037/a0027169. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Conrod PJ, Samoluk S, Pihl RO, Dongier M. Posttraumatic stress disorder symptoms and situation-specific drinking in women substance abusers. Alcoholism Treatment Quarterly. 2000;18:31–47. doi:10.1300/J020v18n03_04. [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. doi:10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: An experience sampling test of the self-medication hypothesis. Journal of Abnormal Psychology. 2000;109:198–204. [PubMed] [Google Scholar]
- Testa M, Livingston JA, Hoffman JH. Does sexual victimization predict subsequent alcohol consumption? A prospective study among a community sample of women. Addictive Behaviors. 2007;32:2926–2939. doi: 10.1016/j.addbeh.2007.05.017. doi:10.1016/j.addbeh.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twamley EW, Hami S, Stein MB. Neuropsychological function in college students with and without posttraumatic stress disorder. Psychiatry Research. 2004;126:265–274. doi: 10.1016/j.psychres.2004.01.008. doi:10.1016/j.psychres.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Walsh K, Blaustein M, Knight WG, Spinazzola J, van der Kolk BA. Resiliency factors in the relation between childhood sexual abuse and adulthood sexual assault in college-age women. Journal of Child Sexual Abuse. 2007;16:1–17. doi: 10.1300/J070v16n01_01. doi:10.1300/J070v16n01_01. [DOI] [PubMed] [Google Scholar]
- Walsh K, Danielson CK, McCauley J, Hanson RF, Smith DW, Resnick HS, Saunders BE, Kilpatrick DG. Longitudinal trajectories of posttraumatic stress disorder symptoms and binge drinking among adolescent girls: The role of sexual victimization. Journal of Adolescent Health. 2012;50:54–59. doi: 10.1016/j.jadohealth.2011.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal Of Personality And Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi:10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility.. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. October 1993. [Google Scholar]
- Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors. 2012;37:982–985. doi: 10.1016/j.addbeh.2012.03.026. doi:10.1016/j.addbeh.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]