Abstract
Community health center providers and staff access to resources for their Latino and non-Latino patients with diabetes is unknown. We analyzed survey data from 577 community health center providers and staff who manage diabetes from 85 sites across 10 Midwestern states. Respondents were labeled as high proportion (HP) providers if >25 % of their site’s diabetes population was Latino. HP providers were more likely than non-HP providers to have access to physician’s assistants (71 vs. 58 %) and certified diabetes educators (61 vs. 51 %), but less access to endocrinologists (25 vs. 35 %) (p < 0.05). HP providers had greater access to Spanish-speaking providers (48 vs. 26 %), on-site interpreters (83 vs. 59 %), culturally tailored diabetes education programs (64 vs. 26 %), and community outreach programs (77 vs. 52 %) (p < 0.05). Providers at HP sites reported greater access to a range of personnel and culturally tailored programs. However, increased access to these services is needed across all sites.
Keywords: Diabetes, Latino, Services, Community health centers
Background
It is imperative that the healthcare system be prepared to care for the growing Latino population and its burden of diabetes [1, 2]. Many Latinos who are uninsured or live in medically underserved settings receive care in community health centers [3]. However, there has been no comprehensive assessment of the accessibility of diabetes services for patients at health centers or of specific resources for Latino patients [4]. We conducted a cross-sectional survey of providers at Midwestern community health centers to assess their access to services for their patients with diabetes and measure how these services vary by the proportion of Latinos served at the site.
Methods
This study was carried out by the MidWest Clinicians’ Network (MWCN) Research Committee comprised of investigators from MWCN, the University of Chicago, North Dakota State University, and University of Evansville. MWCN is a nonprofit organization that supports community-based primary health care across 10 Midwestern states.
Participants and Data Collection
Between August 2010 and November 2010, we mailed a survey to 1,471 eligible providers at 97 health center sites affiliated with MWCN. Eligible providers currently treated or managed patients with diabetes. Participants gave informed consent by returning the completed survey. The study received human subject approval from the University of Chicago Institutional Review Board.
Measures
A 28-item questionnaire included multiple-choice questions on participant and workplace characteristics and health center resources.
Provider Characteristics
Providers were asked their position at the health center, year of birth, gender, race/ethnicity, number of years in practice, and percent of patients with diabetes who were Latino.
Health Center Characteristics
Providers were asked their center’s location (city, suburban or rural), wait for a routine physician appointment, and health center hours. Respondents reported the percentage of the site’s diabetes patients who were Latino and the percentage of the patients who were foreign born and uninsured. Providers were labeled as working in high proportion (HP) sites if >25 % of their site’s diabetes patient population was Latino. The rest were labeled as working at low proportion (LP) sites.
Health Center Personnel
Providers reported their access to the following personnel when needed: (1) primary care physicians, (2) advanced practice nurses, (3) physician assistants, (4) endocrinologists, and (5) certified diabetes educators. Respondents who took care of Latino patients with diabetes were asked if the following personnel and services were available at their site: (1) Spanish-speaking front desk staff, (2) Spanish-speaking providers, (3) on-site interpreter services, and (4) telephone lines for off-site interpreters. Respondents chose from 5 responses: never, occasionally, sometimes, often, or usually. We classified responses as “having access” if the respondent reported accessibility to services “often” or “usually.”
Culturally Tailored Services
Providers who reported caring for Latino patients were asked if they had access to the following programs for their patients: (1) community health workers, (2) physical activity classes in Spanish, (3) culturally tailored nutrition counseling for Latinos, (4) culturally tailored diabetes education for Latinos, (5) partnership with local organizations, (6) telemedicine services to access off-site healthcare professionals, (7) diabetes group visits in Spanish, and (8) multidisciplinary teams.
Analysis
We examined descriptive statistics of participants’ individual and workplace characteristics and access to personnel and diabetes services. To analyze the relationship between participant characteristics and proportion of Latino diabetes patients served, we conducted bivariate analyses using Chi square test for categorical variables and Wilcoxon rank sum tests for continuous variables. To investigate how provider access to health center personnel and site services varied by proportion of Latino diabetes patients served at the site, we used a generalized linear mixed effect model with random effects for each site. The analyses were performed using SAS 9.2 (Cary, NC, 2009).
Results
A total of 620 of 1,471 eligible providers responded to the survey, for an adjusted response rate of 47 %. Female providers were more likely to return the survey than male providers (46 vs. 39 %, p = 0.04). The physician response rate was lower than that of advanced practice nurses and physician assistants (35, 50, and 42 %, respectively, p <0.001). We analyzed data from the 577 respondents from 85 health center sites across 10 states who reported the percent of Latino patients with diabetes seen at their site.
Provider Demographics and Health Center Characteristics: Table 1
Table 1.
Respondent characteristics by their site’s proportion of Latino patients with diabetesa
| Across all sites | By proportion of patients at site with diabetes who are Latino
|
p value | ||
|---|---|---|---|---|
| (N = 577) N (%) | > 25 % (N = 265) N (%) | ≤25 % (N = 312) N (%) | ||
| Respondent characteristics | ||||
| Types of providers | 0.09 | |||
| Physicians | 228 (40) | 96 (36) | 132 (43) | |
| Advanced practice nurses | 120 (21) | 58 (22) | 62 (20) | |
| Physician assistants | 55 (10) | 35 (13) | 20 (7) | |
| Registered nurses | 45 (8) | 21 (8) | 24 (8) | |
| Medical assistants | 39 (7) | 17 (6) | 22 (7) | |
| Licensed practical nurses | 22 (4) | 13 (5) | 9 (3) | |
| Dietitians | 4 (1) | 0 (0) | 4 (1) | |
| Case managers | 3 (1) | 1 (0.4) | 2 (1) | |
| Certified diabetes educators | 2 (0.4) | 1 (0.4) | 1 (0.3) | |
| Health educators | 1 (0.2) | 1 (0.4) | 0 (0) | |
| Otherb | 55 (10) | 21 (8) | 34 (11) | |
| Age (mean ± SD) [years] | 46.2 (12) | 45.3 (12) | 47.0 (12) | 0.09 |
| Male | 156 (27) | 0.10 | ||
| Race/ethnicity | 0.05 | |||
| Caucasian | 430 (76) | 185 (71) | 245 (80) | |
| Asian | 53 (9) | 29 (11) | 24 (8) | |
| Black or African American | 48 (8) | 24 (9) | 24 (8) | |
| Other | 38 (7) | 24 (9) | 14 (5) | |
| Latino ethnicity | 37 (7) | 27 (10) | 10 (3) | < 0.001 |
| Born outside of US | 123 (22) | 59 (22) | 64 (21) | 0.69 |
| Years practicing (mean ± SD) | 14.0 (11) | 12.9 (10) | 15.0 (11) | 0.01 |
| Workplace characteristics | ||||
| Site locale | ||||
| Urban | 363 (63) | 189 (71) | 174 (56) | < 0.001 |
| Rural | 155 (27) | 53 (20) | 102 (33) | < 0.001 |
| Suburban | 56 (10) | 23 (9) | 33 (11) | 0.4 |
| Wait for routine physician appointment | 0.15 | |||
| No wait | 165 (30) | 70 (28) | 95 (32) | |
| < 2 weeks | 246 (45) | 114 (46) | 132 (44) | |
| 2–4 weeks | 107 (20) | 56 (23) | 51 (17) | |
| 1–2 months | 19 (4) | 6 (2) | 13 (4) | |
| More than 2 months | 10 (2) | 2 (1) | 8 (3) | |
| Evening appointments available | 387 (68) | 202 (77) | 185 (60) | < 0.001 |
| Weekend appointments available | 229 (41) | 113 (43) | 116 (38) | 0.2 |
| Percent of diabetes patients at site who are Latino (%) | ||||
| 0 | 91 (16) | – | – | |
| ≤25 | 221 (38) | – | – | |
| 26–50 | 141 (24) | – | – | |
| 51–75 | 67 (12) | – | – | |
| 76–100 | 57 (10) | – | – | |
| Percent of Latino patients who are foreign born (mean ± SD) | 53.2 (29) | 58.9 (23) | 47.6 (33) | < 0.001 |
| Percent of Latino patients at site who are uninsured (mean ± SD) | < 0.001 | |||
| 25 % or less | 107 (20) | 17 (7) | 90 (31) | |
| 26–50 % | 110 (20) | 57 (22) | 53 (18) | |
| 51–75 % | 164 (30) | 102 (39) | 62 (22) | |
| 76–100 % | 168 (31) | 86 (33) | 82 (29) | |
N counts vary somewhat due to missing values. All percentages do not sum to 100 due to rounding
Other job titles include social worker, pharmacist, clinical services manager, director of pharmacy, medical director, medical technologist, Women, Infants and Children (WIC) nutritionist, and respondents with multiple titles
Providers at HP sites were more likely to be of Latino ethnicity, work at urban sites, have foreign-born Latino patients, and have higher rates of uninsured patients. Most respondents (84 %) reported caring for Latino patients.
Overall Access to Personnel and Resources: Table 2
Table 2.
Availability of personnel and resources to respondents across all sites (N = 577)a
| Respondents reporting having access N (%) | |
|---|---|
| Healthcare personnelb | |
| Primary care physician | 538 (95) |
| Advanced practices nurses | 467 (85) |
| Physician assistants | 347 (64) |
| Endocrinologists | 167 (30) |
| Certified diabetes educators | 309 (56) |
| Bilingual personnel and language servicesb,c | |
| Spanish-speaking front desk staff | 336 (70) |
| Spanish-speaking provider | 180 (38) |
| On-site interpreter services | 345 (73) |
| Telephone lines to off-site interpreters | 288 (61) |
| Diabetes services and programsc | |
| Community outreach worker program | 297 (65) |
| Physical activity classes in Spanish | 94 (20) |
| Culturally-tailored nutrition counseling for Latinos | 203 (44) |
| Culturally tailored diabetes education for Latinos | 211 (46) |
| Partnerships with local organizations | 158 (35) |
| Telemedicine | 44 (10) |
| Group visits for diabetes patients in Spanish | 122 (26) |
| Multidisciplinary teams | 246 (54) |
N counts vary somewhat due to missing values. All percentages do not sum to 100 due to rounding
Availability was defined as having access to the personnel or service >50 % of the time
Access to these services was only asked of the 486 respondents who reported managing Latino patients with diabetes
The majority of respondents reported having access to primary care physicians (95 %), advanced practice nurses (85 %), physician assistants (64 %), and certified diabetes educators (56 %) for their patients; however, few had access to an endocrinologist (30 %). Many respondents reported having access to on-site interpreter services (72 %) but access to Spanish-speaking providers (38 %) was low. More than half of the respondents noted the availability of community outreach workers (65 %) and multidisciplinary teams (54 %) but less access to other culturally tailored services.
Access to Resources by Proportion of Latino Patients at Site
Healthcare Personnel
Providers at HP sites were more likely to have access to physician assistants (71 vs. 58 %, p = 0.002) and certified diabetes educators (61 vs. 51 %, p = 0.01) compared to providers at LP sites (Fig. 1). Providers at LP sites had higher rates of access to an endocrinologist than did providers at HP sites (35 vs. 25 %, p = 0.02).
Fig. 1.
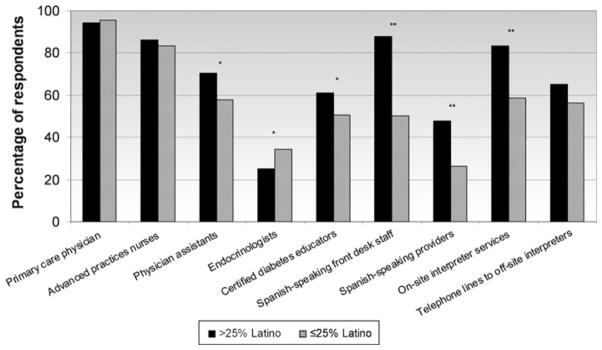
Provider and staff accessibility by site’s proportion of Latino patients [N = 577 (Spanish-speaking front desk staff, Spanish-speaking providers, on site interpreter services and telephone lines to off-site interpreters were only asked of the 486 respondents who reported seeing Latino diabeters patients)].
*Statistically significant at p < 0.05. **Statistically significant at p <0.001
Bilingual Personnel and Language Services
Providers who cared for Latino patients at HP sites had access to Spanish-speaking front desk staff (88 vs. 50 %, p <0.001), Spanish-speaking providers (48 vs. 26 %, p <0.001) and on-site interpreter services (83 vs. 59 %, p <0.001) more frequently than did LP site providers.
Diabetes Services and Programs
Providers at HP sites who cared for Latino patients were more likely to have access to community outreach workers (77 vs. 52 %, p < 0.001), physical activity classes in Spanish (35 vs. 5 %, p < 0.001), culturally tailored nutrition counseling (63 vs. 23 %, p < 0.001), culturally tailored diabetes patient education (64 vs. 26 %, p < 0.001), and partnerships with local organizations (49 vs. 20 %, p < 0.001) for their patients than did LP providers (Fig. 2). Providers at HP sites noted higher rates of group visits for diabetes patients in Spanish (40 vs. 12 %, p < 0.001) and of multidisciplinary teams compared to providers at LP sites (64 vs. 43 %, p < 0.001).
Fig. 2.
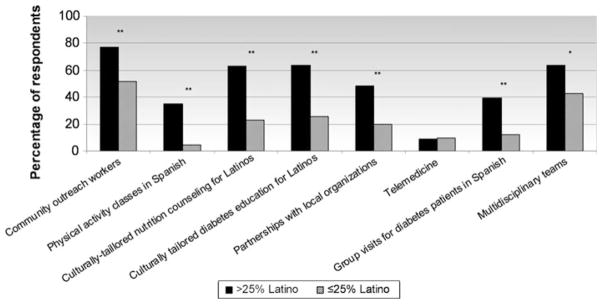
Availability of resources to providers by site’s proposition of Latino patients [N = 486 (We excluded respondents who stated they saw no Latino patients)].
*Statistically significant at p < 0.05. **Statistically significant at p <0.001
Discussion
Our study is the first to measure the availability of culturally tailored diabetes programs at health centers across a region of the US and how availability of these services differs by the proportion of Latino patients served.
Providers who worked at centers that served many Latino patients had access to many culturally tailored programs and to interpretation services. This finding dovetails with evidence that culturally tailored healthcare interventions can improve diabetes outcomes and that access to interpretation services improves patient satisfaction and patient receipt of clinical information [5–8]. However, since reimbursement for these service is not always available, it is unclear how centers are financing these programs [9]. Centers may be using grants to offer culturally tailored services, however sustaining these programs requires ongoing support and innovative, longer-term funding streams. Additionally, the quantity and quality of culturally tailored programs needed to impact diabetes outcomes is unclear [5, 6, 10]. A set of best practices that describes the personnel, programs, and systems of care needed to serve Latino patients with diabetes may be important to establish to ensure that sites are offering the right kinds of services for their patient population.
Despite the paucity of bilingual healthcare personnel in the US, we found that community health centers are able to attract personnel who are Spanish-speaking. Health centers may be uniquely positioned to hire bilingual personnel by being situated in communities with larger pools of minority job applications and by appealing to minority providers who have the inherent desire to practice in under-served areas. However, more programs are needed that mentor minority students and encourage them to pursue careers in healthcare [11].
Providers working at centers with many Latino patients reported greater access to many non-physician personnel. Training physician assistants, nurse practitioners and other non-physician providers will be especially important as they increasingly serve as primary care providers and co-manage patients with diabetes [5, 6]. However, we still need to understand the best ways of coordinating care among different types of providers.
Nevertheless, access to culturally tailored programs, interpretation services, and subspecialists needs to be strengthened across all sites. We found that some providers had no or limited access to culturally tailored programs. And despite a federal mandate that obligates the provision of interpretation services to all patients, not all the providers in our survey reported having access to interpretation services [12]. Additionally, health center providers across all sites had limited access to endocrinologists, corroborating other studies that have reported poor access to subspecialists within the safety net healthcare system [13].
Limitations
We had a lower survey response rate from physicians, although our overall response rate was high compared to other provider surveys. Additionally, we were unable to account for financial resources available to the sites that may have affected the types of services and programs available.
Conclusions
Our study provides insight into how some health centers have strengthened their services and their workforce to better meet the needs of their Latino patients. Further work needs to examine how these centers are able to offer these services, why others are not, and what the impact is of these services on diabetes disparities.
Acknowledgments
We would like to thank all the participating providers and staff from the MidWest Clinicians’ Network health center sites. We are grateful to James Jung for helping with data management and cleaning and to Amanda Giese for her help in formatting the figures. This research was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases Diabetes Research and Training Center (P60 DK20595) and Chicago Center for Diabetes Translation Research (P30 DK092949). Dr. Baig is supported by a NIDDK Mentored Patient-Oriented Career Development Award (K23 DK087903-01A1). Dr. Chin is supported by a NIDDK Midcareer Investigator Award in Patient-Oriented Research (K24 DK071933).
Footnotes
Conflict of interest The authors do not have any conflicts of interest to disclose.
Contributor Information
Arshiya A. Baig, Email: abaig@uchicago.edu, Section of General Internal Medicine, Department of Medicine, University of Chicago, 5841 S. Maryland Ave. MC 2007, Chicago, IL 60637, USA
Cara A. Locklin, College of Nursing, University of Illinois at Chicago, Chicago, IL, USA
Amanda Campbell, MidWest Clinicians’ Network, Lansing, MI, USA.
Cynthia T. Schaefer, University of Evansville, Evansville, IN, USA. MidWest Clinicians’ Network, Lansing, MI, USA
Loretta J. Heuer, MidWest Clinicians’ Network, Lansing, MI, USA. North Dakota State University, Fargo, ND, USA
Sang Mee Lee, Department of Health Studies, University of Chicago, Chicago, IL, USA.
Marla C. Solomon, Department of Pediatric Endocrinology, University of Illinois at Chicago, Chicago, IL, USA
Michael T. Quinn, Section of General Internal Medicine, Department of Medicine, University of Chicago, 5841 S. Maryland Ave. MC 2007, Chicago, IL 60637, USA
J. Martin Vargas, Community Action Partnership of Western Nebraska, Gering, NE, USA.
Deborah L. Burnet, Section of General Internal Medicine, Department of Medicine, University of Chicago, 5841 S. Maryland Ave. MC 2007, Chicago, IL 60637, USA
Marshall H. Chin, Section of General Internal Medicine, Department of Medicine, University of Chicago, 5841 S. Maryland Ave. MC 2007, Chicago, IL 60637, USA
References
- 1.Centers for Disease Control and Prevention. Diabetes Report Card 2012. Atlanta: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2012. [Google Scholar]
- 2.United States Census Bureau. The Hispanic population: 2010—census briefs. Washington: United States Census Bureau; 2011. [Google Scholar]
- 3.Forrest CB, Whelan EM. Primary care safety-net delivery sites in the United States: a comparison of community health centers, hospital outpatient departments, and physicians’ offices. JAMA. 2000;284(16):2077–83. doi: 10.1001/jama.284.16.2077. [DOI] [PubMed] [Google Scholar]
- 4.National Association of Community Health Centers. Serving patients with limited English proficiency: results of a community health center survey. Bethesda: National Association of Community Health Centers; 2008. [Google Scholar]
- 5.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5 suppl):101S–56S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baig AA, Wilkes AE, Davis AM, et al. The use of quality improvement and health information technology approaches to improve diabetes outcomes in African American and Hispanic patients. Med Care Res Rev. 2010;67(5 Suppl):163S–97S. doi: 10.1177/1077558710374621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? a systematic review of the literature. Health Serv Res. 2007;42(2):727–54. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moreno G, Tarn D, Morales L. Impact of interpreters on the receipt of new prescription medication information among Spanish-speaking Latinos. Med Care. 2009;47(12):1201–8. doi: 10.1097/MLR.0b013e3181adcc1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ku L, Flores G. Pay now or pay later: providing interpreter services in health care. Health Aff (Millwood) 2005;24(2):435–44. doi: 10.1377/hlthaff.24.2.435. [DOI] [PubMed] [Google Scholar]
- 10.Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007;64(5 Suppl):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grumbach K, Chen E. Effectiveness of University of California postbaccalaureate premedical programs in increasing medical school matriculation for minority and disadvantaged students. JAMA. 2006;296(9):1079–85. doi: 10.1001/jama.296.9.1079. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services. Office of Minority Health. National Standards for culturally and linguistically appropriate services in health care—final report. March 2001. Washington: U.S. Department of Health and Human Services; 2001. [Google Scholar]
- 13.Gusmano MK, Fairbrother G, Park H. Exploring the limits of the safety net: community health centers and care for the uninsured. Health Aff (Millwood) 2002;21(6):188–94. doi: 10.1377/hlthaff.21.6.188. [DOI] [PubMed] [Google Scholar]


