Dear Editor
Homebound older adults are an important subpopulation of the elderly who commonly experience higher rates of chronic illness, disability, cognitive impairment, and psychological distress than do general community-dwelling older adults (Qiu et al., 2010). A growing body of research has demonstrated that psychological distress such as anxiety and depression is associated with poorer cognitive functioning in later life (Beaudreau and O’Hara, 2008). Despite the high prevalence of these problems in this population, no research has examined the association between psychological distress and cognitive impairment. The purpose of this study was to investigate the association between anxiety and depression and cognitive impairment in homebound older adults.
Participants in this study were 142 older adults who were deemed eligible for in-home services by the participant’s primary care doctor and were receiving this aid through county aging services. A more detailed description of study methods can be found in another article (Gum et al., 2009). Case managers referred participants to the study following routine home visits and provided their standardized assessment of the participant. The research team completed a one-time structured research assessment.
The main outcome was presence of cognitive impairment as measured by the modified mini mental status examination (3MS; Teng and Chui, 1987). The 3MS is a measure of global cognitive functioning. The suggested cut-score of less than 80 was adopted to represent cognitive impairment. Depressive and anxiety symptoms were assessed with the Brief Symptom Inventory – 18 (BSI-18; Derogatis, 2000). Meeting criteria for a current depressive or anxiety disorder was assessed using the Structured Clinical Interview for the DSM-IV (SCID). Number of chronic medical conditions and degree of functional impairment were obtained from the case manager’s assessment.
Participants with cognitive impairment were compared to those without cognitive impairment using t-tests, Fisher exact tests, and chi-square tests. Logistic regression analyses were conducted to examine the associations between psychological distress and cognitive impairment. We ran two models; the first model examined the association between anxiety and depressive symptoms and likelihood of cognitive impairment. The second model examined the association between depressive and anxiety disorders and likelihood of cognitive impairment. In each model, the final regression model controlled for the following covariates: age (range: 60–93), gender, education, race, chronic medical conditions (range: 1–15), ADL and IADL limitations (range: 2–14), and number of non-psychotropic medications (range: 0–20).
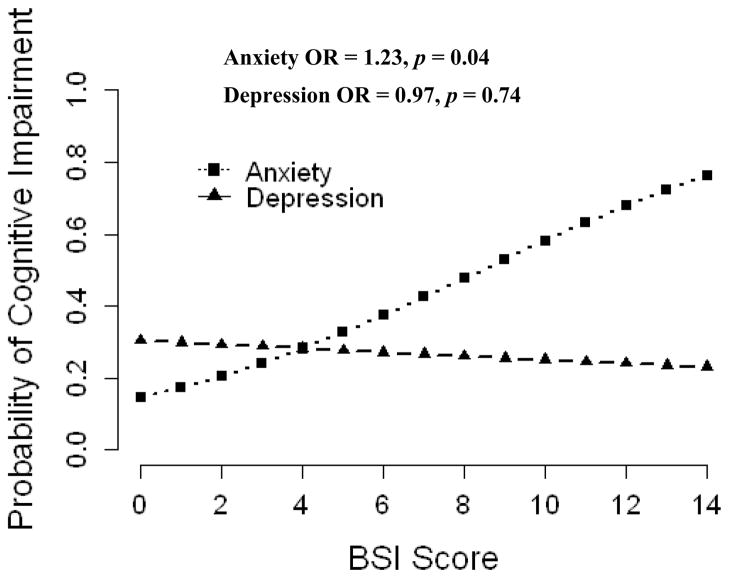
In total, 16.7% of the samples were identified as having cognitive impairment. Participants with cognitive impairment had higher levels of depressive (6.34 vs. 3.72, p = 0.03) and anxiety (5.74 vs. 3.31, p = 0.02) symptoms. A significantly greater proportion met criteria for a current anxiety disorder (26.1% vs. 9.6%, p = 0.04). Those with cognitive impairment did not differ from those without in terms of age (77.8 vs. 74.1, p = 0.06), number of medical conditions (4.87 vs. 5.08, p = 0.72), functional impairment (9.96 vs. 9.12, p = 0.47), or number of medications (7.57 vs. 7.34, p = 0.83). In the logistic regression analysis, anxiety symptoms (OR = 1.23, p = 0.04) were associated with increased likelihood of cognitive impairment, but depressive symptoms were not (OR = 0.97, p = 0.74). Figure 1 displays the predicted probabilities of having cognitive impairment by anxiety and depressive symptoms after controlling for all covariates. In the second logistic model, meeting criteria for an anxiety disorder (OR = 6.92, p = 0.01) was associated with cognitive impairment, whereas depressive disorders were not (OR = 1.14, p = 0.88).
Figure 1.
Predicted probability of cognitive impairment in relation to anxiety and depressive symptoms after controlling for demographics, health, and disability.
This cross-sectional investigation found that cognitive impairment was associated with elevated symptoms of depression and anxiety as well as higher rates of anxiety disorders. After controlling for other factors that influence cognition, anxiety disorders and symptoms remained strongly associated with cognitive impairment. Participants with an anxiety disorder were almost seven times more likely than non-anxious participants to have cognitive impairment. Depressive symptoms or disorders were no longer associated with cognitive impairment after accounting for these covariates. This study demonstrates the clinical importance of assessing for anxiety when working with this population. Longitudinal research is needed to elucidate the directionality of this relationship in order to identify targets for future interventions.
Acknowledgments
Mr. Petkus receives support from the National Institute on Aging (Fellowship: 1F31AG042218)
Footnotes
No Conflicts to Report.
Previous presentation: These findings were presented at the 2012 annual meeting of Anxiety Disorders Association of America. April 2012, Washington DC.
Contributor Information
Andrew J. Petkus, San Diego State University / University of California, San Diego Joint Doctoral Program in Clinical Psychology
Amber M. Gum, Department of Mental Health Law and Policy, Louis de la Parte Florida Mental Health Institute, University of South Florida
Julie Loebach Wetherell, VA San Diego Healthcare System, Department of Psychiatry, University of California, San Diego
References
- BEAUDREAU SA, O’HARA R. Late-life anxiety and cognitive impairment: a review. American Journal of Geriatric Psychiatry. 2008;16:790–803. doi: 10.1097/JGP.0b013e31817945c3. [DOI] [PubMed] [Google Scholar]
- DEROGATIS L. Brief Symptom Inventory (BSI) 18: Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Systems; 2000. [Google Scholar]
- GUM AM, PETKUS A, MCDOUGAL SJ, PRESENT M, KING-KALLIMANIS B, SCHONFELD L. Behavioral health needs and problem recognition by older adults receiving home-based aging services. International Journal of Geriatric Psychiatry. 2009;24:400–8. doi: 10.1002/gps.2135. [DOI] [PubMed] [Google Scholar]
- QIU WQ, DEAN M, LIU T, GEORGE L, GANN M, COHEN J, BRUCE ML. Physical and mental health of homebound older adults: an overlooked population. Journal of the American Geriatrics Society. 2010;58:2423–8. doi: 10.1111/j.1532-5415.2010.03161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TENG EL, CHUI HC. The Modified Mini-Mental State (3MS) examination. Journal of Clinical Psychiatry. 1987;48:314–8. [PubMed] [Google Scholar]