Abstract
Background
Hand surgeons treat trapeziometacarpal arthrosis as if everyone with the disease presents for treatment despite evidence that suggests that trapeziometacarpal arthrosis is a normal part of human aging for which—it seems safe to assume—most people never seek medical attention.
Questions/purposes
The aims of our study were (1) to confirm the prevalence of radiographic trapeziometacarpal arthrosis in a very large sample and to determine if age and sex are associated with (2) any radiographic evidence of trapeziometacarpal arthrosis; and (3) radiographic evidence of severe trapeziometacarpal arthrosis.
Methods
A total of 2321 patients 31 years or older with radiographs obtained during treatment of a distal radius fracture at a tertiary care medical center emergency department between 2002 and 2012 were analyzed. Trapeziometacarpal arthrosis was graded using the 3-point scale of Sodha et al. (none, definite, destroyed trapeziometacarpal joint); we used regression analyses to determine the association of age (in 10-year age groups) and sex with the presence of trapeziometacarpal arthrosis.
Results
The prevalence of trapeziometacarpal arthrosis steadily increased to 85% between the ages of 71 and 80 years and reached 100% in women (with 50% of them being classified as severe) aged 91 years or older and 93% in men of 81 years or older. Severe arthrosis was more prevalent at earlier ages among women and reached 35% in women and 34% in men who were 81 years or older. Logistic regression identified higher age as the strongest factor associated with trapeziometacarpal arthrosis, but sex was also a factor.
Conclusions
Radiographic trapeziometacarpal arthrosis is an expected part of human aging. Given that only three patients in this large cohort had evidence of prior surgery, it seems that most people adapt to trapeziometacarpal arthrosis. Treatments that optimize adaptation in patients who present with trapeziometacarpal arthrosis-related symptoms and disability merit additional study.
Level of Evidence
Level IV, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Despite evidence suggesting that trapeziometacarpal arthrosis is a normal part of the human aging process (whose prevalence increases steadily from age 40 years onward with a 91% prevalence in patients older than 80 years of age, according to one study [7]), to which most people presumably adapt, hand surgeons and their patients often conceive of it as a condition that requires treatment to depend on the hand. The realization that trapeziometacarpal arthrosis is so prevalent that one can safely assume that it is generally well tolerated provides patients with the relatively counterintuitive option of adapting to the changes.
Given that this concept is either inadequately proved or inadequately disseminated, we felt it important to perform a prevalence study similar to the one noted earlier [7] but with a larger cohort of adult patients aged 31 years and older.
The aims of our study were (1) to determine the prevalence of radiographic trapeziometacarpal arthrosis and to determine if age and sex are associated with (2) any radiographic evidence of trapeziometacarpal arthrosis; and (3) radiographic evidence of severe trapeziometacarpal arthrosis.
Patients and Methods
This study was approved by our human research committee. Two thousand eight hundred sixty patients who were seen at the emergency department with 2955 distal radius fractures from April 2002 through May 2012 were identified using a database of musculoskeletal injuries. Patients who were 31 years or older at the time of their visit and who had posteroanterior, oblique, and lateral radiographs of the wrist were included for analysis. Patients were excluded based on (1) prior visible surgery for trapeziometacarpal arthrosis on the side of the radiograph; and (2) pregnancy during the visit as required by our human research committee. Only one series of radiographs (the most recent) was included of patients who had visited more than once and/or for bilateral distal radius fractures. Six hundred thirty-four sets of radiographs were excluded: 95 sets were duplicates in patients with multiple distal radius fractures within the study period; 423 sets were in patients younger than 31 years of age; there were no radiographs in 24 patients; 89 sets were incomplete or poor quality; and three hands (0.1% of all hands; three of 1175 [0.26%] of all patients diagnosed with radiographic arthrosis) had already had radiographic evidence of operative treatment for trapeziometacarpal arthrosis. This left 2321 radiographs for the analysis (Fig. 1). The average age of all 2321 patients was 60 ± 16 years (range, 31–101 years), and 67% were women.
Fig. 1.
Flow diagram is shown detailing subject selection for study.
The radiographs were evaluated for trapeziometacarpal arthrosis based on a grading system developed by Sodha et al. [7]. This grading system has been proven to be reliable (substantial intraobserver agreement and moderate interobserver agreement according to criteria of Landis and Koch [5]) [7]. The simple three-grade scale system is as follows: Grade 1, no or nearly no trapeziometacarpal arthrosis; Grade 2, definite trapeziometacarpal arthrosis but not severe; and Grade 3, severe trapeziometacarpal arthrosis (Fig. 2).
Fig. 2A–D.
Examples of trapeziometacarpal arthrosis according to each Sodha Grade. (A) Sodha Grade 1, no or nearly no trapeziometacarpal arthrosis. (B) Sodha Grade 2, definite trapeziometacarpal arthrosis but not severe. (C) Sodha Grade 2 or 3, definite trapeziometacarpal arthrosis which might be graded as severe. (D) Sodha Grade 3, severe trapeziometacarpal arthrosis.
Three research assistants (SJEB, JPB, MGJSH) graded 90 radiographs to evaluate interobserver agreement. According to Landis and Koch [5], the Fleiss multirater kappa (κ) [3] among the three observers showed a substantial overall agreement, κ = 0.62 (95% confidence interval [CI], 0.52–0.71; p < 0.001). The agreement for the individual Grades was as follows: Grade 1, κ = 0.75 (substantial agreement; 95% CI, 0.63–0.87; p < 0.001); Grade 2, κ = 0.49 (moderate agreement; 95% CI, 0.37–0.61; p < 0.001); and Grade 3, κ = 0.55 (moderate agreement; 95% CI, 0.43–0.67; p < 0.001). After the interobserver agreement was established, the research assistants (who all had an MD degree) each reviewed one-third of all radiographs, unaware of the patients’ sex and age.
Statistical Analysis
An a priori sample size analysis showed that to be able to detect a prevalence of 50% with a 95% CI within 2.5% of the true prevalence (5% width of CIs), we needed 1537 subjects.
Prevalence rates are reported with 95% CIs. In bivariable analysis, the Pearson chi-square test was used to assess the relationship between the grade of trapeziometacarpal arthrosis and age and sex. Ordinal logistic regression analysis was performed to evaluate the effect of age in 10-year groups and sex on the grade of trapeziometacarpal arthrosis (1, 2, or 3). Binary logistic regression analyses were performed to assess the predictive value of age group and sex on the presence of trapeziometacarpal arthrosis Grades 2 and 3 combined and separately for Grade 3. A two-tailed p value of < 0.05 was considered significant.
Results
Prevalence of Trapeziometacarpal Arthrosis
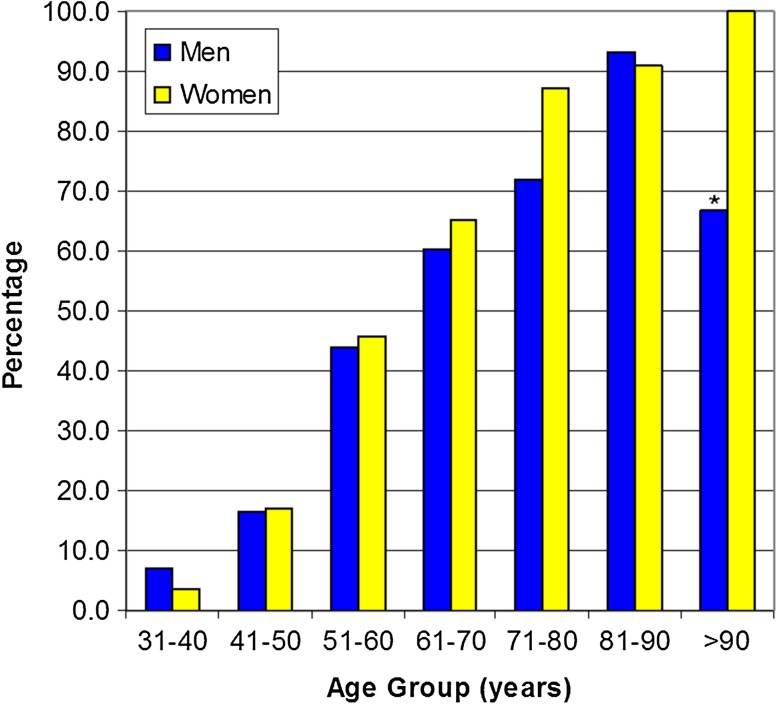
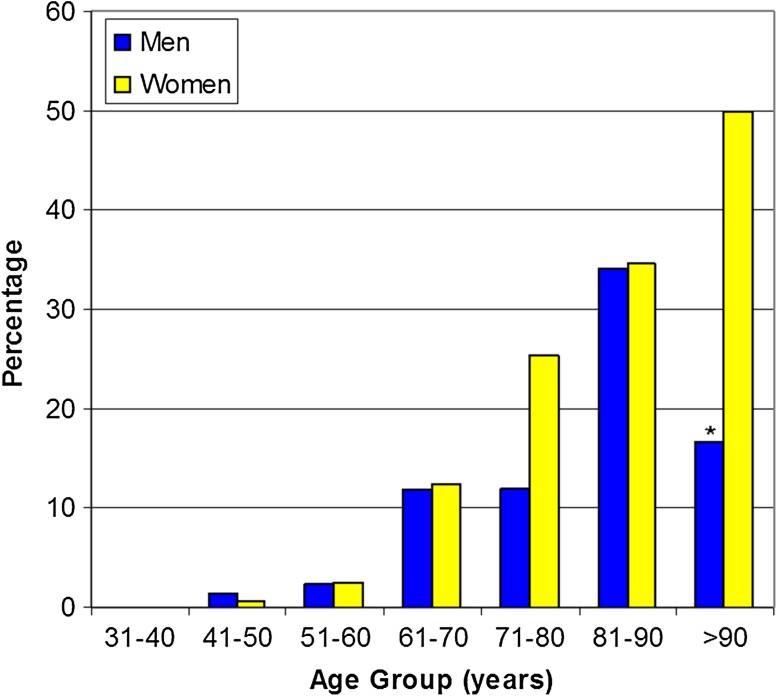
The prevalence of radiographic trapeziometacarpal arthrosis increased steadily with age after age 31 years, reaching a prevalence of 100% in women older than age 90 years and 93% in men 81 years or older (there were only six men older than 90 years in our cohort so the 67% prevalence in that age group is not reliable) (Fig. 3). Severe trapeziometacarpal arthrosis (Grade 3) was more prevalent among women and reached 35% in women and 34% in men who were 81 years or older and 50% in women older than 90 years (Fig. 4). Prevalence rates of the presence of trapeziometacarpal arthrosis and severe trapeziometacarpal arthrosis are shown (Table 1) with 95% CIs for each 10-year age group.
Fig. 3.
The prevalence of trapeziometacarpal arthrosis increases with age in both men and women. *Note that there were only six men older than 90 years in our cohort; therefore, the prevalence among men in this age group is not reliable.
Fig. 4.
The prevalence of severe trapeziometacarpal arthrosis increases with age in both men and women. *Note that there were only six men older than 90 years in our cohort; therefore, the prevalence among men in this age group is not reliable.
Table 1.
Age-related prevalence of trapeziometacarpal arthrosis (n = 2321)
| Age group (years) | Patients per Sodha grade | |||||||
|---|---|---|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | Grades 2 and 3 | |||||
| Number | Prevalence (95% CI) | Number | Prevalence (95% CI) | Number | Prevalence (95% CI) | Number | Prevalence (95% CI) | |
| 31–40 | 251 | 94 (92–97) | 15 | 6 (3–8) | 0 | 0 (0–0) | 15 | 6 (3–8) |
| 41–50 | 356 | 83 (80–87) | 68 | 16 (12–19) | 4 | 1 (0.02–1.8) | 72 | 17 (13–20) |
| 51–60 | 311 | 55 (51–59) | 244 | 43 (39–47) | 14 | 2 (1.2–3.7) | 258 | 45 (41–49) |
| 61–70 | 156 | 36 (32–41) | 223 | 52 (47–56) | 53 | 12 (9–15) | 276 | 64 (59–68) |
| 71–80 | 51 | 15 (11–19) | 205 | 61 (56–67) | 78 | 23 (19–28) | 283 | 85 (81–89) |
| 81–90 | 22 | 9 (5–12) | 143 | 57 (51–63) | 87 | 35 (29–40) | 230 | 91 (88–95) |
| > 90 | 2 | 5 (−2–12) | 20 | 50 (34–66) | 18 | 45 (29–61) | 38 | 95 (88–102) |
CI = confidence interval.
Factors Associated With the Presence of Trapeziometacarpal Arthrosis
Increasing age and female sex are associated with radiographic trapeziometacarpal arthrosis. In bivariable analysis, women had a significantly higher prevalence of Grades 2 and 3 combined or Grade 3 trapeziometacarpal arthrosis compared with men (p < 0.001). Evidence of Grade 2 or 3 arthrosis was seen in 56% of women compared with 36% of men, and Grade 3 arthrosis was found in 14% of women compared with 5.5% of men. The prevalence of the presence of trapeziometacarpal arthrosis (Grades 2 and 3 combined) significantly increased with age (p < 0.001) (Table 2). The prevalence of severe trapeziometacarpal arthrosis also significantly increased with age (p < 0.001) (Table 3).
Table 2.
Bivariable analysis: all Sodha grades (n = 2321)
| Parameter | Patients per Sodha grade | p value | |||||
|---|---|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | |||||
| Number | Percent | Number | Percent | Number | Percent | ||
| Sex | < 0.001 | ||||||
| Female | 659 | 42 | 688 | 44 | 212 | 14 | |
| Male | 490 | 64 | 230 | 30 | 42 | 6 | |
| Age group (years) | < 0.001 | ||||||
| 31–40 | 251 | 94 | 15 | 6 | 0 | 0 | |
| 41–50 | 356 | 83 | 68 | 16 | 4 | 1 | |
| 51–60 | 311 | 55 | 244 | 43 | 14 | 2 | |
| 61–70 | 156 | 36 | 223 | 52 | 53 | 12 | |
| 71–80 | 51 | 15 | 205 | 61 | 78 | 23 | |
| 81–90 | 22 | 9 | 143 | 57 | 87 | 35 | |
| > 90 | 2 | 5 | 20 | 50 | 18 | 45 | |
Table 3.
Bivariable analysis: Sodha Grades 2 and 3 (n = 2321)
| Parameter | Patients per Sodha grade | p value | |||
|---|---|---|---|---|---|
| Grade 1 | Grades 2 and 3 | ||||
| Number | Percent | Number | Percent | ||
| Sex | < 0.001 | ||||
| Female | 659 | 42 | 900 | 58 | |
| Male | 490 | 64 | 272 | 36 | |
| Age group (years) | < 0.001 | ||||
| 31–40 | 251 | 94 | 15 | 6 | |
| 41–50 | 356 | 83 | 72 | 17 | |
| 51–60 | 311 | 55 | 258 | 45 | |
| 61–70 | 156 | 36 | 276 | 64 | |
| 71–80 | 51 | 15 | 283 | 85 | |
| 81–90 | 22 | 9 | 230 | 91 | |
| > 90 | 2 | 5 | 38 | 95 | |
Sex (women) and older age significantly contributed to the ordinal logistic regression model and explained 41% of the variability in higher Sodha grade for trapeziometacarpal arthrosis (Nagelkerke R2 = 0.41). Women were 1.3 times more likely to show radiographic evidence of trapeziometacarpal arthrosis (odds ratio [OR], 1.3; 95% CI, 1.0–1.5; p = 0.025). A 10-year increase in age increased the odds of trapeziometacarpal arthrosis by 2.6 (OR, 2.6; 95% CI, 2.4–2.8; p < 0.001). The binary logistic regression model with sex (women) and higher age explained 43% of the variability in trapeziometacarpal arthrosis (Grades 2 and 3 combined; Nagelkerke R2 = 0.43), but sex did not reach statistical significance (OR, 1.2, 95% CI, 0.97–1.5; p = 0.086). A 10-year increase in age increased the odds of having trapeziometacarpal arthrosis by 2.7 (OR, 2.7; 95% CI, 2.5–3.0; p < 0.001).
Factors Associated With Severe Trapeziometacarpal Arthrosis
For severe radiographic trapeziometacarpal arthrosis, increasing age was the only risk factor. The binary logistic regression model with sex (women) and higher age explained 28% of the variability in severe trapeziometacarpal arthrosis (Grade 3; Nagelkerke R2 = 0.28). Sex did not contribute significantly to the model (OR, 1.4; 95% CI, 0.95–2.0; p = 0.089). Severe trapeziometacarpal arthrosis was 2.4 times more likely with a 10-year increase in age (OR, 2.4; 95% CI, 2.1–2.7; p < 0.001).
Discussion
Awareness that trapeziometacarpal arthrosis is a normal part of human aging for which it can be assumed only a fraction of people seek help from a doctor; it gives patients and providers perspective as they search for the best ways to ensure a dependable hand as arthrosis develops. Studies that look at the prevalence of trapeziometacarpal arthrosis dichotomously (eg, before or after menopause) or clinically (patients that report symptoms) seems misleading compared with studies that assess the radiographic prevalence of arthrosis in small age groups over a continuum of ages. We felt there was a need to repeat the latter study in a larger cohort to increase awareness of and confidence in the finding that trapeziometacarpal arthrosis is an expected part of aging. We hope that this study confirming that age is strongly associated with trapeziometacarpal arthrosis—the finding that 100% of women older than 90 years of age have it in particular—will help patients and surgeons conceive of this disease as an expected part of aging to which most people adapt, that an arthritic hand can be a dependable hand.
This study had a number of limitations. It is possible that patients who fracture their distal radius are not representative of the entire population, but that seems unlikely. The interobserver agreement was not nearly perfect so ideally all raters would have examined all radiographs. The study design did not allow for assessment of symptoms and disability; in other words, we addressed pathoanatomy alone with no sense of how many patients considered their trapeziometacarpal arthrosis a health problem. There were only six men older than 90 years, limiting the validity and reliability of that age group.
The prevalence of trapeziometacarpal arthrosis is higher than what most hand surgeons cite, although there is evidence apart from the present study that it is indeed very common [7]. Several factors might help explain the discrepancies. First, most prior studies looked at single age cutoffs rather than the spectrum over all ages. In addition, most other studies used a single posteroanterior view and used the Kellgren and Lawrence grading system, which is not specific to the trapeziometacarpal joint [2, 4, 6, 8, 9]. Finally, studies that use radiographs of patients with fracture of the distal radius most likely have better representation of older aged patients than in prior studies. Marshall et al. [6] found that 53% of 592 community-dwelling adults aged 50 years or older (mean 64 years; 62% women) had radiographic evidence of trapeziometacarpal arthrosis (which is comparable to 66% identified in our series). Dahaghin et al. [2] found a lower radiographic prevalence of 36% among 3906 inhabitants of a suburb aged 55 years and older consisting of 58% women. A study by Wilder et al. [9] found much lower rates of radiographic trapeziometacarpal arthrosis in a community-based study population for which 3327 participants with an average age of 62 years (range, 40–94 years) were recruited: 6.6% (9.0% in men versus 5.7% in women) in participants aged 40 to 49 years, which increased to 36.4% (31.5% in men versus 39.3% in women) in participants who were 80 years or older. Armstrong et al. [1] found a 33% radiographic prevalence of trapeziometacarpal arthrosis in postmenopausal women between the ages of 45 and 70 years, also lower than our results. The Copenhagen Osteoarthritis Study [8] found that significant trapeziometacarpal arthrosis (Kellgren and Lawrence Grades 3 and 4) increased from 0% to 22.7% among men between 50 and 80 + years of age and from 0.9% to 36.9% in women between 50 and 80 + years of age. The prevalence of Kellgren and Lawrence Grades 3 and 4 in women was comparable to Sodha Grade 3 among women between the ages of 81 and 90 years in our cohort.
Age is the most important factor associated with radiographic trapeziometacarpal arthrosis and more severe disease. Compared with Sodha and colleagues [7], the current study identified slightly more arthrosis in men and less severe arthrosis in women of comparable age, but our larger study confirmed their earlier findings.
The strengths of this study are the large sample size and the confirmed reliability of trapeziometacarpal arthrosis grading on standard wrist radiographs. The results of our study suggest that female sex might be less important than previously thought with older age being by far the dominant risk factor for radiographic trapeziometacarpal arthrosis, supporting earlier work that has identified age as a risk factor [1, 4, 7–9]. It appears that people who live long enough will get trapeziometacarpal arthrosis. This combined with the fact that only 0.1% of patients with a fracture of the distal radius were excluded from our analysis because of radiographic evidence of prior surgery, despite the very high observed prevalence of severe trapeziometacarpal arthrosis, suggests that most people adapt to trapeziometacarpal arthrosis. Treatments that optimize adaptation are an option for patients who experience symptoms and disability from trapeziometacarpal arthrosis and merit additional study.
Acknowledgments
We thank Associate Professor David Zurakowski at Harvard Medical School for his help with the statistical analysis of this study.
Footnotes
One of the authors (SJEB) certifies that she has or may receive payments or benefits, during the study period, greater than USD 10,000 from Anna Foundation|NOREF, Genootschap Noorthey and Stichting Vreedefonds, The Netherlands, for Scientific Research. One of the authors (MGJSH) certifies that he has or may receive payments or benefits, during the study period, greater than USD 10,000 from Anna Foundation|NOREF, and Marti-Keunig Eckhart Stichting, The Netherlands, for Scientific Research. One of the authors (DR) certifies that he has or may receive payments or benefits, during the study period, less than USD 10,000 from Skeletal Dynamics LLC (Miami, FL, USA) and Wright Medical Technology, Inc (Arlington, TN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19:340–341. doi: 10.1016/0266-7681(94)90085-X. [DOI] [PubMed] [Google Scholar]
- 2.Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, Pols HA, Hazes JM, Koes BW. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study) Ann Rheum Dis. 2005;64:682–687. doi: 10.1136/ard.2004.023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fleiss JL, Levin B, Paik MC. The measurement of interrater agreement. In: Balding DJ, Cressie NAC, Fisher NI, Johnstone IM, Kadane JB, Ryan LM, Scott DW, Smith AFM, Teugels JL, editors. Statistical Methods for Rates and Proportions. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2003. pp. 598–626. [Google Scholar]
- 4.Haara MM, Heliovaara M, Kroger H, Arokoski JP, Manninen P, Karkkainen A, Knekt P, Impivaara O, Aromaa A. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86:1452–1457. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 6.Marshall M, van der Windt D, Nicholls E, Myers H, Dziedzic K. Radiographic thumb osteoarthritis: frequency, patterns and associations with pain and clinical assessment findings in a community-dwelling population. Rheumatology (Oxford). 2011;50:735–739. doi: 10.1093/rheumatology/keq371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sodha S, Ring D, Zurakowski D, Jupiter JB. Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am. 2005;87:2614–2618. doi: 10.2106/JBJS.E.00104. [DOI] [PubMed] [Google Scholar]
- 8.Sonne-Holm S, Jacobsen S. Osteoarthritis of the first carpometacarpal joint: a study of radiology and clinical epidemiology. Results from the Copenhagen Osteoarthritis Study. Osteoarthritis Cartilage. 2006;14:496–500. doi: 10.1016/j.joca.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Wilder FV, Barrett JP, Farina EJ. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14:953–957. doi: 10.1016/j.joca.2006.04.013. [DOI] [PubMed] [Google Scholar]