Abstract
Background
Valgus hips with increased antetorsion present with lack of external rotation and posterior hip pain that is aggravated with hip extension and external rotation. This may be the result of posterior femoroacetabular impingement (FAI).
Questions/purposes
We asked whether (1) the range of motion (ROM); (2) the location of anterior and posterior bony collision zones; and (3) the prevalence of extraarticular impingement differ between valgus hips with increased antetorsion compared with normal hips and hips with idiopathic FAI.
Methods
Surface models based on CT scan reconstructions of 13 valgus hips with increased antetorsion, 22 hips with FAI, and 27 normal hips were included. Validated three-dimensional collision detection software was used to quantify the simulated hip ROM and the location of impingement on the acetabular and the femoral sides.
Results
Hips with coxa valga and antetorsion showed decreased extension, external rotation, and adduction, whereas internal rotation in 90° of flexion was increased. Impingement zones were more anteroinferior on the femur and posteroinferior on the acetabular (pelvic) side; and the zones were more frequently extraarticular, posterior, or to a lesser degree anterior against the inferior iliac spine. We found a higher prevalence of extraarticular impingement for valgus hips with increased antetorsion.
Conclusions
Valgus hips with increased antetorsion predispose to posterior extraarticular FAI and to a lesser degree anteroinferior spine impingement.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Coxa valga is often associated with acetabular dysplasia [5, 19] and neuromuscular disorders [18] but may also occur as an isolated entity. Coxa valga can be combined with excessive femoral antetorsion [6]. Based on our clinical experience with patients with a valgus hip and high antetorsion, pain occurs in the buttock and by provocation in hip extension and external rotation (ER). Increased antetorsion of the neck is associated with an increased range of internal rotation (IR) and reciprocal decrease in ER [1, 4]. A high neck-shaft angle implies a decreased lateral femoral shaft offset, which theoretically may contribute to decreased range of hip motion, specifically adduction, IR, and ER [28]. Both an increased neck shaft angle and femoral antetorsion can result in decreased range of external rotation. Thus, the question arises whether hips with coxa valga and increased antetorsion are at risk for femoroacetabular impingement (FAI), which may be most pronounced posteriorly [9].
We therefore addressed the following questions: (1) how is ROM affected in hips with coxa valga and increased antetorsion compared with normal hips and hips with FAI; (2) how does the location of anterior and posterior FAI zones on the femur/acetabulum in hips with coxa valga and increased antetorsion differ compared with normal hips and hips with FAI; (3) does the prevalence of extraarticular impingement locations differ in hips with coxa valga and increased antetorsion compared with normal hips and hips with FAI?
Patients and Methods
We performed a retrospective comparative study of 52 patients (62 hips). Three groups were evaluated: seven patients with isolated coxa valga and antetorsion (13 hips), 26 normal subjects (27 hips), and 19 patients with FAI (22 hips; Table 1). All patients with coxa valga and increased antetorsion were recruited from our outpatient clinic between January 2005 and April 2011. Inclusion criteria for hips in the study group were a shaft-neck angle ≥ 135° [6, 27, 28] and a concomitant femoral antetorsion > 25° [27] in the presence of a nondysplastic acetabulum. Exclusion criteria were a lateral center-edge (LCE) angle of less than 25° [11] combined with an acetabular index of more than 14° [27] and osteoarthritis Grade 1 or higher according to Tönnis [26]. Normal hips and hips with FAI were available from a previous study [22]. The normal hips were selected from the contralateral hips of 146 patients undergoing CT-based computer-assisted THA. Hips with the following features were excluded: THA or TKA (n = 10), pain (n = 4), previous hip surgery (n = 3), osteoarthritis Grade 1 or higher according to Tönnis [26] (n = 40), LCE angle of less than 25° (n = 24), pistol grip deformity [20] (n = 13), coxa profunda (n = 13), coxa vara or valga (n = 1), acetabular retroversion [17, 25] (n = 4), protrusio acetabuli (n = 2), alpha angle [13] of more than 50° (n = 4), and femoral retrotorsion (n = 1). For the FAI group, the diagnosis was based on the current recommendations of a positive correlation among symptoms, findings during physical examination (pain in forced flexion, IR, and adduction), and radiographic findings [25]. There were 13 hips with a combined cam-pincer type, six hips with a pure cam type, and three hips with a pure pincer-type impingement. The study was approved by the local institutional review board.
Table 1.
Demographic and radiographic data
| Parameter | Normal | FAI | Coxa valga | p value |
|---|---|---|---|---|
| Number of hips | 27 | 22 | 13 | – |
| Age (years) | 54 ± 11 (31–74) | 36 ± 10 (17–49)* | 30 ± 13 (15–50)* | < 0.001 |
| Gender (percent male of all hips) | 56 | 68 | 0*,† | < 0.001 |
| Side (percent right of all hips) | 33 | 50 | 54 | 0.472 |
| Height (cm) | 168 ± 10 (158–195) | 175 ± 7 (163–188)* | 170 ± 7 (161–179) | 0.030 |
| Weight (kg) | 77 ± 16 (49–115) | 80 ± 20 (52–127) | 64 ± 13 (50–89)*,† | 0.033 |
| Body mass index | 27 ± 4 (20–36) | 26 ± 5 (19–37) | 22 ± 4 (17–28)*,† | 0.005 |
| Alpha angle (Nötzli) | 42 ± 5 (34–39) | 62 ± 12 (40–84)* | 52 ± 6 (42–61)*,† | < 0.001 |
| Lateral edge angle (degrees) | 32 ± 5 (25–44) | 33 ± 7 (17–42) | 31 ± 10 (25–44) | 0.279 |
| CCD angle (degrees) | 130 ± 5 (122–140) | 132 ± 7 (121–146) | 148 ± 9 (135–161)*,† | < 0.001 |
| Acetabular index (degrees) | 6 ± 4 (−6 to 13) | 4 ± 5 (−10 to 14.2) | 5 ± 5 (−3 to 12) | 0.288 |
| Extrusion index (percent) | 23 ± 5 (12–33) | 18 ± 7.5 (4–35) | 21 ± 9 (10–34) | 0.796 |
| Femoral antetorsion CT (degrees) | 21 ± 7 (7–39) | 22 ± 8 (0–35) | 58 ± 17 (33–87)*,† | < 0.001 |
Values are expressed as mean ± SD with range in parentheses; * significant difference compared with the normal group; †significant difference compared with the FAI group; FAI = femoroacetabular impingement.
With the help of a three-dimensional (3-D) model from a CT scan of the pelvis and the distal femur [15, 16, 23], we compared the computed ROM and the individual impingement zones among the three groups. Based on the primary research question (ROM, ER in extension), we performed a power analysis. Given a normal ER in neutral of 47° [22], a minimal detectable difference of 15° of ER among the three groups, and an estimated SD of 13° [22], we calculated a minimal sample size of 12 hips for each group to provide a level of alpha 0.01 and a beta of 0.10.
A CT scan of the entire pelvis and the distal part of the femur according to a previously defined protocol [7, 23] was available for all patients. We then built a 3-D polygon model of the pelvis and the femur using the Amira Visualization Toolkit (Visage Imaging Inc, Carlsbad, CA, USA). The acetabular reference coordinate system was the anterior pelvic plane, defined by both anterosuperior iliac spines and the pubic tubercles [24]. The femoral reference coordinate system was defined by the center of the femoral head, the knee center, and both femoral condyles [12]. Femoral version was calculated according to Murphy et al. [12]. Each individual hip was then virtually simulated with the help of previously described and validated software [23, 29]. This software uses automatic rim detection [15], a best-fitting sphere algorithm for identification of the femoral head center [10], and the equidistant method for motion analysis [16]. The equidistant method was specifically designed for virtual FAI analysis [16]. Based on a cadaveric investigation including cartilage, labrum, and joint capsule, an impingement collision can be detected with a mean accuracy of 2.6° ± 2.5° [16].
Using this computerized analysis, we calculated the ROM for the following motions for all three groups: flexion, extension, abduction, adduction, IR, and ER (in neutral and 90° of flexion). Furthermore, we evaluated two motion patterns, which correspond to the anterior and the posterior impingement test. For the anterior impingement test, IR was studied in 1° increments between 60° and 120° of flexion and 0° and 20° of adduction. Analogously for the posterior impingement test, ER was studied in 1° increments between −5° and 20° of extension and −20° and 20° of adduction.
The location of the impingement zones was determined by the distribution of all impingement points for every possible combination of motion for an individual patient. The impingement zones were calculated for the anterior and the posterior impingement tests separately. The distribution of the impingement zones was calculated using a clock system with 6 o’clock representing the acetabular notch on the acetabular side and the femoral axis on the femoral side. Three o’clock was consistently defined anteriorly for both right and left hips. In addition, the location of impingement was further specified as extra- or intraarticular. Intraarticular locations comprised the acetabular rim and the lunate surface on the acetabular side and the femoral head and neck on the femoral side. All other anatomical areas were defined as extraarticular. For the posterior impingement test, impingement zones were only recorded if a normal external rotation of 47° in neutral flexion could not be achieved [22].
We tested the data for normal distribution with the Kolmogorov-Smirnov test. Because not all the parameters were normally distributed, we used nonparametric tests for comparison. To compare demographic and radiographic data, ROM, or location of impingement among the three groups, we used a Kruskal-Wallis test; if significant, we used the Mann-Whitney U test to compare each of the three combinations of two groups. To compare binominal demographic data and the prevalence of extraarticular impingement among the three groups, we used a chi square test; if significant, we used the Fisher’s exact test to compare among each of the three combinations of two groups.
Results
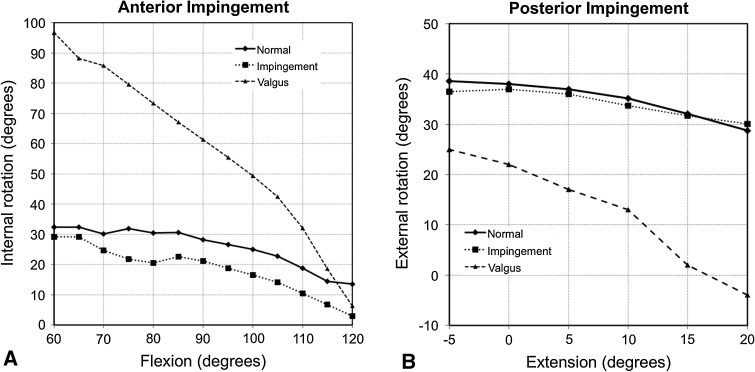
Hips with coxa valga and increased antetorsion had decreased amplitude for extension, adduction, ER in neutral, and 90° of flexion, and increased amplitude of abduction, IR in extension, and 90° of flexion (Table 2). For the anterior impingement test, an increased IR was observed for valgus hips up to a flexion of 110° (Fig. 1A). For the posterior impingement test, ER was decreased in valgus hips for the entire range of extension investigated (Fig. 1B).
Table 2.
ROM of control and study groups
| Parameter | Normal | FAI | Coxa valga et antetorta | p value |
|---|---|---|---|---|
| Flexion (degrees) | 125 ± 13 (103–146) | 117 ± 14 (86–144) | 119 ± 14 (90–140) | 0.247 |
| Extension | 41 ± 8 (28–50) | 33 ± 13 (19–44) | 26 ± 23 (−16 to 50)*,† | < 0.001 |
| Abduction (degrees) | 63 ± 12 (39–80) | 56 ± 8 (40–69)* | 76 ± 15 (56–96)*,† | < 0.001 |
| Adduction (degrees) | 38 ± 10 (13–58) | 33 ± 9 (21–50) | 24 ± 17 (−10 to 50)* | 0.010 |
| Internal rotation in extension (degrees) | 110 ± 17 (84–146) | 96 ± 20 (56–140)* | 134 ± 9 (114–140)*,† | < 0.001 |
| External rotation in extension (degrees) | 47 ± 12 (20–72) | 43 ± 13 (18–68) | 22 ± 21 (−20 to 42)*,† | < 0.001 |
| Internal rotation in 90° of flexion (degrees)‡ | 33 ± 9 (13–40) | 21 ± 15 (–8 to 40)* | 59 ± 16 (36–93)*,† | < 0.001 |
| External rotation in 90° of flexion | 103 ± 13 (74–128) | 99 ± 19 (45–125) | 84 ± 15 (50–102)*,† | 0.011 |
Values are expressed as mean ± SD with range in parentheses; * significant difference compared with the normal group; †significant difference compared with the FAI group; ‡values calculated for hips with a minimum of 90° of flexion only; FAI = femoroacetabular impingement.
Fig. 1A–B.
Two graphs showing the anterior and posterior impingement tests for the three study groups. (A) For the anterior impingement test, hips with coxa valga and antetorsion showed increased IR from 60° to 110° of flexion compared with both the normal (p < 0.001 for all flexion values in this range) and impingement groups (p < 0.001 for all flexion values in this range). (B) For the posterior impingement test, hips with coxa valga and antetorsion showed decreased ER for the evaluated range of extension compared with both the normal (p < 0.001 for all extension values) and impingement groups (p < 0.001 for all extension values).
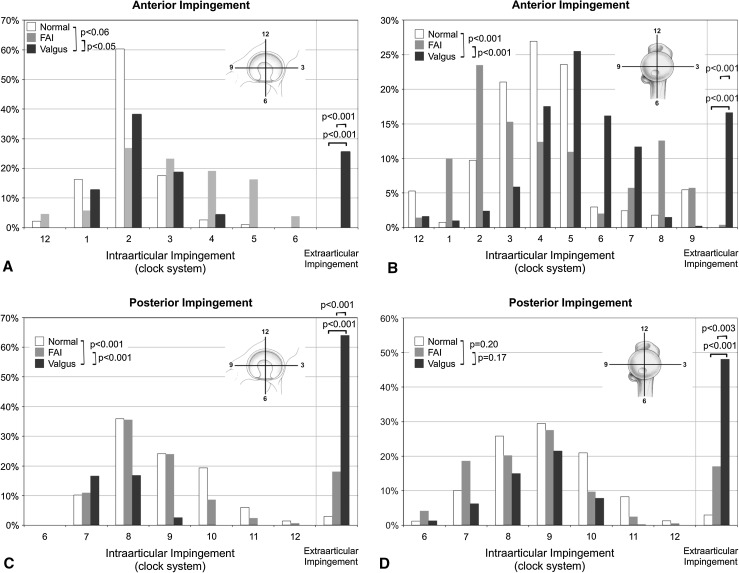
The anterior impingement zones on the acetabulum were located more anterior compared with normal (p = 0.06) and more superior compared with the FAI group (p = 0.05) (Fig. 2A). The anterior impingement zones on the femoral side were located more anteroinferiorly compared with normal and FAI hips (p < 0.001 for both comparisons) (Fig. 2B). The posterior impingement zones of the acetabulum were located more posteroinferiorly in comparison to normal and FAI hips (p < 0.001 for both comparisons) (Fig. 2C). The posterior impingement zones on the femoral side did not differ between valgus hips in comparison to normal (p = 0.20) or FAI hips (p = 0.17) (Fig. 2D).
Fig. 2A–D.
The impingement zones for the anterior (A–B) and posterior (C–D) impingement tests are shown. On the acetabulum, the impingement zones were located more anterior compared with normal (p = 0.06) and more superior compared with the FAI group (p = 0.05). On the femur, the impingement zones were located more anteroinferiorly compared with normal and FAI hips (p < 0.001 for both comparisons). We found a higher prevalence of extraarticular impingement on the acetabular (A) and the femoral sides (B) for the anterior impingement test in valgus hips when compared with normal (p < 0.001) and FAI hips (p < 0.001). The posterior impingement zones of the acetabulum (C) were located more posteroinferiorly in comparison with normal (p < 0.001) and FAI hips (p < 0.001). The posterior impingement zones on the femoral side (D) did not differ between valgus hips in comparison to normal (p = 0.20) or FAI hips (p = 0.17). A higher prevalence of extraarticular impingement was found for valgus hips compared with the normal and FAI groups on the acetabular (C; p < 0.001) and femoral sides (D; p < 0.003).
We found a higher prevalence of extraarticular impingement on the acetabular and the femoral side for the anterior impingement test for valgus hips in comparison to normal and FAI hips (p < 0.001 for all comparisons). The anterior extraarticular impingements were located on the inferior iliac spine on the acetabular side and on the greater trochanter and neck area on the femoral side (Fig. 3A–C). For the posterior impingement test, a higher prevalence of extraarticular impingement was found for valgus hips compared with the normal and FAI groups on the acetabular (p < 0.001 and p = 0.012, respectively) and femoral sides (p < 0.003 and p = 0.084, respectively). The posterior extraarticular impingements were located on the ischial tuberosity on the acetabular side (Fig. 3) and on the lesser and greater trochanter and the intertrochanteric crest (Fig. 3D–E).
Fig. 3A–E.
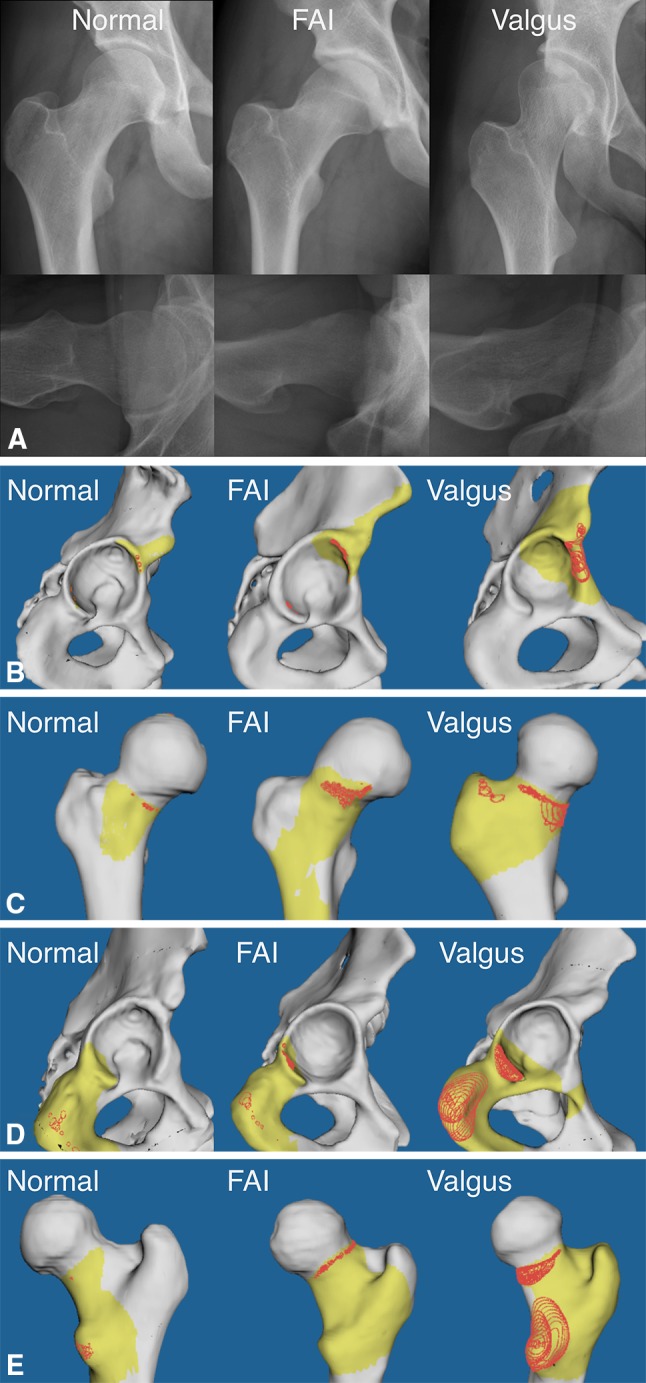
(A) This figure shows representative cases from each study group (left: normal hip, middle: femoroacetabular impingement hip, right: valgus hip with increased antetorsion). (B) The simulated anterior impingement zones of the acetabulum are located in the anterosuperior quadrant in FAI hips (middle) and more anteroinferiorly in valgus hips with increased antetorsion (right). (C) The simulated anterior impingement zones of the femur are located more inferior in the calcar area in valgus hips with increased antetorsion (right) compared with normal hips (left) and hips with FAI (middle). (D) The simulated posterior impingement zones of the acetabulum are located in the posteroinferior quadrant of the acetabulum and extraarticularly on the ischial tuberosity in valgus hips with increased antetorsion (right). (E) On the femoral side, the posterior impingement zone in valgus hips and increased antetorsion (right) are typically located in the area of the lesser trochanter.
Discussion
In our experience, patients with symptomatic valgus hips with increased antetorsion typically present with pain in the buttock and a positive posterior impingement sign. A high neck-shaft angle implies a decreased lateral femoral shaft offset, which theoretically may contribute to decreased adduction and rotation [28]. The increased antetorsion of the femoral neck is associated with an increased IR and reciprocal decreased ER [27]. Thus, the question arises whether a coxa valga with increased antetorsion puts a hip at risk for posterior FAI. We therefore asked whether there are differences between hips with coxa valga and increased antetorsion and normal and FAI hips regarding (1) ROM; (2) location of anterior and posterior impingement; and (3) prevalence of extraarticular impingement.
There are several limitations to this study. First, our study focuses on pure geometrical collision detection between two nondeformable surface models. This method neither implies information on additional instability or soft tissue structures nor includes static load transmission parameters (eg, joint contact pressure). We suspect the pathomechanism of impingement may rather be additive than competitive in regard to potential static overloading [8]. Second, the simulated 3-D CT evaluation only detects osseous collision but does not take into account soft tissue restriction to motion. Therefore, ROM may be overestimated. However, posterior intra- and extraarticular osseous impingement in the study group occurred at substantially lower degrees of extension, ER, and adduction compared with the control groups. An additional posterior soft tissue impingement would further aggravate the conflict and lead to an underestimation of the real posterior FAI conflict.
Valgus hips with increased antetorsion do have a predominant extraarticular limitation of extension, ER, and adduction when compared with normal hips or hips with idiopathic FAI. On the other hand, these hips have an increased range of IR in flexion. These findings reveal a dynamic difference in hip function that has not been well addressed in the literature. Most of the biomechanical studies [3, 8, 14] deal with static overload of the hip to explain dysfunction or potential early osteoarthritis. Our findings change the focus to a potential underlying dynamic pathomechanism that would subsequently require the surgeon to consider static and dynamic abnormalities when formulating treatment of these hips.
A valgus hip with increased antetorsion predisposes to posterior predominantly extraarticular impingement (Fig. 3). The posterior impingement pattern detected by the computed ROM analysis is consistent with the clinical symptoms and findings [9]. This is consistent with the observation of Tönnis and Heinecke [27] who showed overcorrection of a retroverted femoral neck (ie, creating iatrogenically increased antetorsion) can lead to painful restriction of ER. One may speculate that the posterior impingement could act as a fulcrum. This could lead to an anterior subluxation potentially resulting in anterior chondrolabral lesions. This matches our clinical experience with these patients who often present with an additional positive anterior FAI test and chondrolabral lesions seen intraoperatively in the anterior acetabular area. Concomitant hip dysplasia together with coxa valga and increased antetorsion would even aggravate the dynamic anterior instability. Another explanation for these changes in the anterior acetabular part could be an additional anterior impingement in deep flexion caused by the valgus neck and the decreased lateral offset.
Anterior impingement zones in valgus hips with increased antetorsion tend to be more frequently extraarticular when compared with normal hips or hips with idiopathic FAI. The predominant collision zones in patients with cam, pincer, or mixed types of FAI are at the anterosuperior acetabular rim between 12 and 3 o’clock with a maximum at the 2 o’clock position (Fig. 3B) [2, 21]. In the current study, valgus hips with increased antetorsion had predominant intraarticular collision zones within the same range but an additional 26% exhibited impingement between the inferior iliac spine and the anterior portion of the greater trochanter (Fig. 3B). On the femoral side, predominant impingement was located at 2 o’clock in patients with idiopathic FAI and at 4 o’clock in normal hips (Fig. 3C). Valgus hips with increased antetorsion exhibited a more inferiorly located collision zone at the femoral neck at 5 o’clock (Fig. 3C). Theoretically, the more inferior collision zones at the femoral neck in the study indicate a potential impingement conflict toward the far end range of flexion. Thereby the more inferior parts of the neck likely will impinge against the superior rim or inferior iliac spine. This would be consistent with the rather substantial drop of the IR capacity in the simulation during the end range of flexion. In addition, the restricted adduction in the simulation may be the result of decreased femoral shaft offset compared with the hip center. This result is consistent with the findings of Tubby [28] who described limitations of adduction as a cardinal symptom in coxa valga.
In summary, valgus hips with increased antetorsion do have a distinct aberrant ROM when evaluated by computed 3-D simulated motion analysis. Compared with normal hips and hips with an idiopathic FAI, coxa valga and antetorsion do have an increased range for IR during flexion. On the other hand, ER, extension, and adduction are restricted, which correspond to the clinical presentation [9]. The pathomechanism of posterior FAI hips should be included when evaluating treatment options for valgus hips with increased antetorsion. The logical surgical treatment option would therefore be a varus and derotation osteotomy of the proximal femur.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Audenaert EA, Peeters I, Vigneron L, Baelde N, Pattyn C. Hip morphological characteristics and range of internal rotation in femoroacetabular impingement. Am J Sports Med. 2012;40:1329–1336. doi: 10.1177/0363546512441328. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Bombelli R. [Biomechanical significance of coxa valga in relation to dysplasia of the acetabulum] [in German] Z Orthop Ihre Grenzgeb. 1985;123:452–455. [PubMed] [Google Scholar]
- 4.Botser IB, Ozoude GC, Martin DE, Siddigi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy. 2012;28:619–627. doi: 10.1016/j.arthro.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hips. Clin Orthop Relat Res. 2009;467:128–134. doi: 10.1007/s11999-008-0481-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haverkamp D, Marti RK. Bilateral varus osteotomies in hip deformities: are early interventions superior? A long-term follow-up. Int Orthop. 2007;31:185–191. doi: 10.1007/s00264-006-0147-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124. doi: 10.1097/BLO.0b013e318031c595. [DOI] [PubMed] [Google Scholar]
- 8.Kummer B. [Clinical significance of coxa valga] [in German] Z Orthop Ihre Grenzgeb. 1985;123:443–452. [PubMed] [Google Scholar]
- 9.MacDonald S, Garbuz D, Ganz R. Clinical evaluation of the symptomatic young adult hip. Semin Arthroplasty. 1997;8:3–9. [Google Scholar]
- 10.Mahaisavariya B, Sitthiseripratip K, Tongdee T, Bohez EL, Vander Sloten J, Oris P. Morphological study of the proximal femur: a new method of geometrical assessment using 3-dimensional reverse engineering. Med Eng Phys. 2002;24:617–622. doi: 10.1016/S1350-4533(02)00113-3. [DOI] [PubMed] [Google Scholar]
- 11.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT. Femoral anteversion. J Bone Joint Surg Am. 1987;69:1169–1176. [PubMed] [Google Scholar]
- 13.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 14.Pauwels F. Biomechanics of the Normal and Diseased Hip. Theoretical Foundation, Technique and Results of Treatment. New York, NY, USA: Springer; 1976. [Google Scholar]
- 15.Puls M, Ecker TM, Steppacher SD, Tannast M, Siebenrock KA, Kowal JH. Automated detection of the osseous acetabular rim using three-dimensional models of the pelvis. Comput Biol Med. 2011;41:285–291. doi: 10.1016/j.compbiomed.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Puls M, Ecker TM, Tannast M, Steppacher SD, Siebenrock KA, Kowal JH. The equidistant method—a novel hip joint simulation algorithm for detection of femoroacetabular impingement. Comput Aided Surg. 2010;15:75–82. doi: 10.3109/10929088.2010.530076. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 18.Robin J, Graham HK, Selber P, Dobson F, Smith K, Baker R. Proximal femoral geometry in cerebral palsy: a population-based cross-sectional study. J Pediatr Orthop. 2006;26:536–541. doi: 10.1302/0301-620X.90B10.20733. [DOI] [PubMed] [Google Scholar]
- 19.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 21.Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466:273–280. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tannast M, Hanke M, Ecker TM, Murphy SB, Albers CE, Puls M. LCPD: reduced range of motion resulting from extra- and intraarticular impingement. Clin Orthop Relat Res. 2012;470:2431–2440. doi: 10.1007/s11999-012-2344-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. doi: 10.1002/jor.20309. [DOI] [PubMed] [Google Scholar]
- 24.Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop Relat Res. 2005;436:144–150. doi: 10.1097/01.blo.0000157657.22894.29. [DOI] [PubMed] [Google Scholar]
- 25.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 26.Tönnis D. General Radiography of the Hip Joint. Berlin, Heidelberg, Germany: Springer; 1987. pp. 100–142. [Google Scholar]
- 27.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Tubby AH. Coxa valga (Collum valgum) Proc R Soc Med. 1908;1:107. doi: 10.1177/003591570800101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip2Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45. doi: 10.1016/j.cmpb.2007.02.010. [DOI] [PubMed] [Google Scholar]