Abstract
Background
Dislocation continues to commonly cause failure after primary and revision total hip arthroplasty (THA). Fully constrained liners intended to prevent dislocation are nonetheless associated with a substantial incidence of failure by redislocation, mechanical failure, aseptic loosening, or a combination. Constrained liners with cutouts of the elevated rims can theoretically increase range of movement and therefore decrease the risk dislocation, but it is unclear if they do so in practice and whether they are associated with early wear or loosening.
Questions/purposes
We therefore determined (1) occurrence or recurrence of dislocation and (2) rate of complications associated with constrained implants with cutouts; and (3) assessed for early cup loosening.
Methods
We retrospectively reviewed the records of 81 patients at high risk for dislocation who had 82 constrained liners inserted for primary (n = 10) or revision (n = 72) THA between 2008 and 2010. From the records we extracted demographic and implant data and instances of recurrent dislocation, implant failure, osteolysis, loosening, or construct failure. The minimum followup was 24 months (mean, 34 months; range, 24–49 months).
Results
Three liners failed as a result of further dislocation (3%). Three deep infections occurred. One patient had progressive loosening at the shell-bone interface.
Conclusions
Our observations suggest this liner is associated with a relatively low risk of dislocation in patients at high risk for dislocation and those with recurrent dislocation.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Postoperative dislocation is one of the most common reasons for revision after primary and revision THA. Dislocation was reported as the reason for revision in 33% of cases in the New Zealand Joint Registry [28], 27.6% in the Australian Orthopaedic Association Joint Registry [4], and from 23% to 34% in the Scandinavian registries [20]. Annual incidence of dislocation after primary THA has been reported at 1.9% [27] with higher risk in older patients and those with neck or femur fracture. Neurologic conditions and impaired abductor function are also risk factors [1, 9, 33]. Dislocation remains one of the most common complications after revision THA with dislocation rates ranging from 6.6% to 21.2% [1, 10, 11, 22, 35].
Several surgical options are available to treat or prevent instability. Larger femoral heads increase the head-neck ratio and the “jump-distance” or head displacement distance thereby reportedly reducing the dislocation rate [2]. Lachiewicz and Soileau [24] reported a 4% early dislocation rate and no dislocation at 5 to 10 years followup when using 36- or 40-mm heads in patients at high risk for dislocation. Garbuz et al. [16] reported a reduction in dislocation rate to 1.1% when using 36- and 40-mm heads in revision arthroplasty. They do require a large cup or a thin liner, and this may not be ideal or possible in all patients. Bipolar and tripolar articulations combine a large head with constraint, increasing the force required to dissociate the head from the cup but commonly with the price of reducing ROM before neck impingement [32]. These systems are associated with dislocation rates of 4% to 29% after primary and revision arthroplasty [3, 7, 17, 31]. However, bipolar and tripolar systems have several articulations that can fail by disengagement [8, 12] and they may cause increased polyethylene (PE) wear [18]. Constrained cups typically incorporate a liner that is greater than a 180° hemisphere [29]. Thus, when the head is engaged in the liner, it is gripped by the enveloping PE. These systems transmit considerable stress to the various interfaces of the construct. Constrained cups reportedly have dislocation rates at short followup of 1% to 3% after primary THA performed in patients at risk of dislocation [6, 8, 21] and 6% to 16% after revision THA [8, 12, 14, 21, 23, 36]. A variety of mechanical failure modes have been defined [29, 37, 38] including loss of fixation to the acetabulum, disengagement of the liner from the cup, and dislocation of the head from the liner. Over the medium term, damage can occur as the neck repeatedly impinges on the edge of the liner creating PE debris [29, 30]. If a dislocation or implant dissociation occurs, then open management with simple relocation or full revision is required.
As an alternative, constrained liners with cutouts in the PE that can be positioned in regions of potential neck impingement have been developed (Fig. 1). Retaining fingers on each side of the cutouts grip the head to provide focal constraint. A metal reinforcing ring is positioned over the PE liner to buttress the external surface of the fingers and discourage elastic or plastic deformation of the fingers. When properly aligned, the cutout region theoretically allows a greater ROM to be maintained, theoretically reduces liner impingement and damage, and theoretically lowers the risk of the head levering out as the neck contacts the edge of the cup. However, it is unclear whether these theoretical advantages translate into reduced rates of dislocation, wear, or loosening compared with other constrained designs.
Fig. 1.

The TLC liner. Note the cutouts on either side of the retaining fingers that accommodate the neck during internal and external rotation, both in flexion and extension, if properly aligned. Adjacent fingers or prongs supported by a metal ring prevent the fingers from spreading and allowing the head to escape.
Therefore, we determined (1) the occurrence or recurrence of dislocation and (2) the rate and types of complications associated with this implant. We also (3) radiographically assessed for early cup loosening in patients who had constrained liners designed with cutouts.
Patients and Methods
We retrospectively reviewed the records of all 81 patients who were implanted with 82 Trilogy® Longevity® Constrained (TLC) liners (Zimmer, Warsaw, IN, USA) between June 2008 and February 2010. The indications for the TLC liner were: (1) patients at high risk of dislocation undergoing primary THA (ie, neurological conditions: cerebral palsy, spina bifida, poliomyelitis; deficient abductor muscles such as arthrodesis takedown); (2) patients having revision THA for recurrent instability; and (3) patients having their femoral component revised to a proximal femoral replacement. There were no specific contraindications defined for this study over and above the standard contraindications for hip arthroplasty such as unresolved local infection. During this period, we treated 1586 patients with primary THA and 452 patients with revision THA. Ten of the 82 liners were inserted in patients having primary THA and 72 in patients undergoing revision arthroplasty (Table 1). Thirty-seven patients were treated with the constrained liner after episodes of recurrent instability. Forty-five patients were treated with the constrained liner because they were considered at high risk of dislocation. Of these, 15 were undergoing revision to a proximal femoral replacement. The mean age of the patients at the time of surgery was 68 years (range, 14–94 years). Fifty patients were female and 31 male (including the bilateral case). Six patients died at a mean of 22 months after surgery (range, 7–42 months). None had complications related to their THA. The remaining 75 patients (75 liners) were followed up at a minimum of 24 months (mean, 34 months; range, 24–49 months). All 75 patients were contacted by telephone to confirm ongoing stability of their THA and invited to attend the followup clinic; 52 patients attended for followup specifically for this study.
Table 1.
Indications for the use of the Trilogy® Longevity® Constrained liner
| Clinical scenario | Diagnosis | Number of hips |
|---|---|---|
| Primary THA (n = 10) |
Cerebral palsy with spasticity | 4 |
| Polio | 1 | |
| Spina bifida | 1 | |
| Spondyloepiphyseal dysplasia | 1 | |
| Multiple sclerosis | 1 | |
| Fusion takedown | 1 | |
| Avascular necrosis with soft tissue disruption | 1 | |
| Revision THA (n = 72) |
Recurrent instability | 37 |
| Abductor deficiency | 17 | |
| Proximal femoral replacement | 15 | |
| Other | 3 |
The internal diameter of the TLC liner and thus head size are determined by the size of the acetabular shell. Up to a 52-mm shell, the head size is 28 mm; for 54- and 56-mm shells, the head size is 32 mm; and for 58-mm and larger, the head size is 36 mm. A cemented liner option is available for fixation to well-fixed and properly aligned shells that do not have a compatible locking mechanism. In 23 cases, isolated liner and head exchange was performed. In 14 cases, the shell was also revised and in one of these cases, the femoral component was also revised.
We prefer a posterolateral approach to the acetabulum because of its versatility coupled with whatever is indicated to complete the femoral reconstruction as well such as an extended trochanteric osteotomy. If the preexisting shell is to be retained, its interface stability and acceptable alignment are confirmed. The appropriate outside diameter of the liner insert is chosen (and thereby its obligatory inside diameter). The inner surface of the shell is prepared to maximize the grouting qualities of acrylic cement, the chosen liner next inserted, and the fixation fingers properly aligned until the acrylic has cured. A system of liner trials is available to fine-tune the alignment decision before the final liner is inserted. As a general rule, using the “acetabular clock” as a guide, the superior focal fixation finger is placed at noon or 1 o’clock for the left hip (therefore the inferior finger at 6 or 7 o’clock) and at noon or 11 o’clock for the right hip (therefore the inferior finger at 6 or 5 o’clock). Care is taken to clear the periphery of bone and soft tissue so as not to impede the placement of the locking ring after the femoral head is reduced. If the preexisting shell is to be revised, it is removed, the new acetabular bed prepared, bone deficiency characterized and replenished with morselized bone, the new shell implanted, orientated in 40° to 45° abduction and 15° to 20° of anteversion and then fixed with multiple screws, and the liner inserted. The locking fingers are aligned as described earlier and the liner locked with the mechanism inherent to the shells compatible with the TLC system. If the shell chosen is not compatible, acrylic polymer fixation can be used as outlined earlier. A system of trials is available to assist in finalizing the ideal locking finger alignment. The femoral reconstruction is completed, the femoral head reduced, the absence of impingement confirmed (especially in flexion combined with internal rotation and extension combined with external rotation), and the securing ring locked in place. Regions of extraarticular impingement arising from bone or excess soft tissue on the greater trochanter, femoral neck, or intertrochanteric region should be assessed and resected as possible. Femoral implants should establish adequate length and offset based on the anatomy of the patient. If in a revision setting this is not possible, the femoral component may need to be revised. Likewise, abductor tension should be established by restoring length and offset. Implant position is established by preoperative templating and can be assisted by intraoperative use of leg length devices. Adequate soft tissue tension is assessed by gauging joint laxity during axial traction and hip ROM before subluxation occurs. In some cases it may be necessary to perform a trochanteric osteotomy to tension the abductors and shift the greater trochanter away from an area of impingement.
Twenty patients had revision with a conventional long stem implant, 17 of these had deficiency of the abductor mechanism with the remaining three considered unstable in the operating room. Ten patients had primary THA with a TLC liner inserted for neurologic impairment or prior soft tissue injury (Table 1). In six patients, liners were cemented into the acetabular shell. Head sizes were 28 mm in 18 cases, 32 mm in 28 cases, and 36 mm in 36 cases. Thirty-eight patients had a TLC placed into an existing ingrown cup and 44 into a newly implanted device. Screws were used to augment fixation in all but one of the new acetabular components with more than one screw (range, two to four) used in 33 patients (86%).
Early mobilization is emphasized in all cases under supervision of specialized orthopaedic nursing and physiotherapy teams. The extent of weightbearing is determined by the security of implant interface fixation determined at the time of operation and the complexity of the reconstruction. By and large, this follows a program of 50% protected weightbearing or less for 6 weeks advanced according to the clinical progress and radiographic findings at followup, which is at 6 and 12 weeks. Active abduction is encouraged unless the abductors are absent or greater trochanteric fixation is flimsy. Flexion to 90° is permitted in most cases and greater after 12 weeks.
Patients were routinely seen in the clinic at 6 and 12 weeks, 1 year, and 2 years postoperatively. At each visit, AP and lateral radiographs were obtained with clinical examination focused on gait, muscle function, and comfort with ROM. Fifty-two of the 75 patients had complete followup records. Fifteen were unable to attend because they did not wish to travel for reasons of distance or medical comorbidity. Eight patients had followup at 2 years but not at 1 year. Complications related to the implant were obtained from the clinical notes. These were classified using the failure modes identified by Guyen et al. [18] for the Osteonics cup being: failure at the implant bone interface (Type I), disengagement of the liner from the cup (Type II), locking ring failure (Type III), dislocation of the femoral head (Type IV), and infection (Type V).
One of us (JTM), not a treating surgeon, assessed AP pelvis and lateral views of the hip. Followup and postoperative radiographs were compared. Loosening of the cup was defined as continuous progressive lucencies around the acetabulum from DeLee and Charnley [13] zones 1 to 3 or migration greater than 2 mm. Films were classified as no evidence of osteolysis or loosening, borderline evidence of loosening, or clear evidence of loosening. Osteolysis rates have been reported to be more reliable when determined by a single reviewer comparing a series of radiographs, although the interobserver correlation is poor (kappa 0.28 to 0.44) [15]. Liners were assessed for evidence of dissociation or asymmetry of the locking ring. Sixty-six of the 75 patients had complete sets of radiographs available for review. Six were missing followup films at 2 years and three did not have suitable postoperative lateral films.
Results
Three of 82 patients had a dislocation. All three had a history of dislocation before insertion of the TLC liner. Two were noncompliant patients (ie, both had a history of substance or opioid abuse) and both dislocated early after revision to the TLC liner (3 and 5 months, respectively). The third patient was an active 73-year-old man who dislocated his TLC liner while gardening. The acetabular component and TLC liner had been intentionally aligned in retroversion to compensate for a markedly anteverted stem (Fig. 2). He eventually had his femoral component revised to a more anteverted position along with a dual-mobility construct on the acetabular side to prevent further instability.
Fig. 2A–B.
Radiographs of a 73-year-old man revised to a cemented TLC liner for instability: (A) lateral and (B) AP pelvic views. Note the cup is retroverted and the stem anteverted. Despite initially functioning well, the hip dislocated 47 months after implantation of the liner.
Five complications in addition to the dislocations were observed (Table 2) according to the classification of Guyen et al. [18]. One implant failed as a result of pullout of the cementless cup (Type I failure). This occurred in a 71-year-old woman who had three previous revisions initially for aseptic loosening and then for pelvic dissociation. She eventually underwent revision to a cemented TLC liner for instability. Thirty-seven months later she presented with increasing groin pain with radiology confirming pullout of the cup. One Type III failure occurred after unseating of the locking ring in an 81-year-old woman. She underwent revision with a TLC liner for recurrent instability. On postoperative radiography, it was noted that the locking ring was not properly seated (Fig. 3). She was revised to a dual-mobility construct. Three deep infections occurred (Type V failure) with subsequent exchange of the TLC liner during management. No Type II failures were observed. Six other reoperations were performed not involving failure of the acetabular construct (Table 2).
Table 2.
Complications associated directly with the TLC liners in this series
| Complication | Number of hips | Mean months to failure |
|---|---|---|
| Type I (cup pullout) | 1 (1%) | 37 |
| Type II (liner disengaged) | 0 | |
| Type III (locking ring failure) | 1 (1%) | 0 |
| Type IV (dislocation) | 3 (4%) | 19 (range, 3–47) |
| Type V (deep infection) | 3 (4%) | 11 (range, 1–30) |
| Other reoperations | ||
| Loosening stem | 1(1%) | 33 |
| Periprosthetic fracture femur | 2 (2%) | 6 (range, 0–12) |
| Superficial infection washout | 2 (2%) | 0.5 (range, 0–1) |
| Deep infection washout | 1 (1%) | 1 |
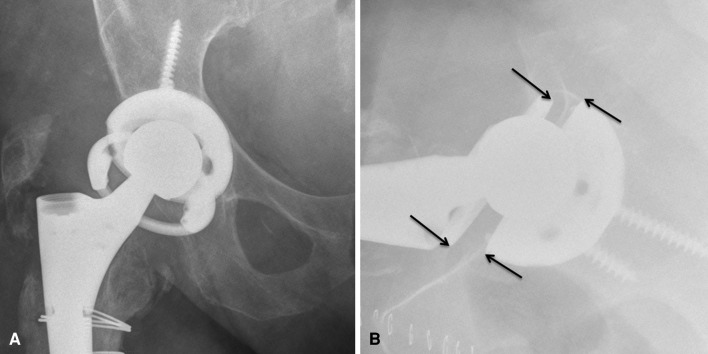
Fig. 3A–B.
Radiographs after revision THA in a patient with a deficient abductor mechanism: (A) AP pelvic and (B) lateral views. The liner appears malaligned in (A) and this is confirmed in (B) where the arrows show the noncemented TLC should be aligned with the edges of the acetabular component.
No loosening of the acetabular components was seen in the surviving patients other than the case with late cup pullout.
Discussion
Recurrent instability after THA is still a challenge to the arthroplasty surgeon. Rates of dislocation after revision or primary hip arthroplasty for patients at risk of instability are still ranging from 6% to 20% despite various surgical solutions proposed and reported in the literature [9, 10]. The downside of the more constrained devices includes limitations of ROM and an increased risk of impingement between the femoral neck and the constrained liner, potentially transferring high stresses at the bone-implant interface. This may simply change the mechanism of failure from dislocation to loosening and wear [29]. In view of these concerns, we reviewed the rate of redislocation, the early complications associated with focal constrained liners, and early radiographic cup loosening.
We acknowledge the limitations of the presented study. First, our retrospective study lacked a comparison group using alternative implants (ie, tripolar articulations or dual-mobility articulations) for patients at high risk for dislocation. It is difficult to compare dislocation rates with other such devices from the literature owing to varying indications, surgical techniques, or patient populations. During the study period we did not have a defined list of indications and contraindications for using the focal constrained liners. Therefore, the indications were broad and included patients with complex femoral and acetabular reconstruction and multiple medical comorbidities. This may have had an impact on our complication rate, because most of the general complications (ie, infection) were not related to the use of the constrained liners. Second, the followup is short and further evaluation of the potential for wear and loosening at the bone-implant interface is required. Third, we did not include an assessment of function and quality of life, because this was not routinely recorded at subsequent followup visits. The broad range of indication and underlying functional status make comparison difficult. We were however able to identify the outcome for the entire cohort, all of whom have known risk factors for instability.
The primary indication for the TLC liner is prevention of instability. Ideally, this should be achieved without reducing the long-term survival of the implant. We report a relatively low dislocation rate (three of 82 liners) with the use of the TLC liner in a group of complex patients. Failure resulting from dislocation occurred in three patients, all with a history of instability. Two of those who dislocated had psychosocial and substance abuse issues. The other occurred in a patient with malpositioned components. The TLC liner is unlikely to provide long-term stability in the setting of severe implant malposition, especially excessive abduction, retroversion, or anteversion of the acetabular component. This position allows repeated impingement and damage to the liner. Optimal implant position and tissue tensioning remain paramount. In the setting of malpositioned components, consideration should be given to revision and correct orientation of the implants. Our dislocation rate at 2 years compares favorably with other reported series in the literature (Table 3). Berend et al. [5] reported overall survival in 667 cases using the S-ROM®. They report a 17.5% redislocation rate at 5 years followup. The same group published early followup of the Freedom® constrained liner (Biomet, Warsaw, IN, USA) [6]. At 9-month followup, one dislocation (1.2%) occurred. The S-ROM® system had a 6.1% dislocation rate at 3 months and 10.2% at 1 year followup. Our experience with this design was similar in terms of early failure. Their conclusion was that design improvements reducing impingement would reduce recurrent dislocation and liner damage. We had no dislocation in the small group (10 patients) of high-risk primary cases when a TLC liner was used. Hernigou et al. [21] compared THA performed on patients with neuromuscular disease with a constrained device used in 164 hips and conventional heads used in 132 hips. At minimum followup of 5 years (mean, 7 years; range, 5–10 years), the dislocation rate in the constrained group was 2% and 25% in the conventional group. Dual-mobility acetabular components are an alternative to constraint. Short- and medium-term results of this type of implant used in primary and revision THA have been published mainly by European centers [25, 26]. Vasukutty et al. [34] reported the outcome for 155 double-mobility components used in revision THA cases; 29 of these were for instability. Three subsequently dislocated (2%). Two occurred in cases initially revised for instability and all three had abductor deficiency. All were reduced closed and none required further revision surgery. Hamadouche et al. [19] reported a 4% dislocation rate at 4-year followup using a similar cemented dual-mobility device. The results of a dual-mobility construct used to prevent instability are encouraging and we have started to use this new implant in revision cases at high risk of instability where other options have failed. Large femoral heads (≥ 36 mm) have been associated with low (< 2%) dislocation rates in the revision setting [16]. These have the advantage of greater ROM before intraarticular impingement occurs with favorable wear characteristics. They do require a suitable cup size to accommodate the liner and although this is not usually an issue during revision, primary cases may not reach that threshold.
Table 3.
Revision rates of constrained liners and dual-mobility liners used in treating instability reported in the literature
| Study | Device | Number of hips | Mean followup (months) | Overall rerevision rate | Failure by dislocation | Acetabular component failure* |
|---|---|---|---|---|---|---|
| Berend et al. [5] | Constrained | 667 | 127 | 42.1% | 17.5% | 1.1% |
| Berend et al. [6] | Constrained (increased ROM) | 81 | 9 | 1.2% | 1.2% | 0% |
| Bremner et al. [8] | Tripolar constrained | 101 | 124 | 17% | 1% | 5% |
| Cooke et al. [12] | Tripolar constrained | 58 | Minimum 24 (range, 24–42) | 13.8% | 5.2% | 8.6% |
| Goetz et al. [17] | Tripolar constrained | 55 | 64 | 13% | 4% | 2% |
| Hamadouche et al. [19] | Cemented dual mobility | 47 | 51 | 4% | 4% | 0% |
| Hernigou et al. [21] | Constrained | 164 | 84 | 3% | 2% | 1% |
| Shapiro et al. [31] | Tripolar constrained | 85 | 58 | 8.2% | 2.4% | 4.8% |
| Shrader et al. [32] | Constrained | 109 | 38 | 7% | 0% | 1.8% |
| Vasukutty et al. [34] | Dual mobility | 148 | 42 | 2% | 2% | 0% |
| Current study | Constrained | 82 | 34 | 13.4% | 3.7% | 2.4% |
* Note that acetabular component failure includes loosening of the acetabular component and the liner breaking.
Other complications associated with the TLC liner were one additional failure as a result of an improperly seated locking ring (1%) and one as a result of pullout of the cementless cup (1%). Six other TLC liners (7%) were revised for other reasons unrelated to the constrained liner, adding to an overall revision rate of 13% (11 of 82 liners) at minimum 2 years followup. In their series of 667 cases using the S-ROM®, Berend et al. [5] reported an overall survival rate of 68.5% at 5 years falling to 51.7% at 10 years. In that series, 17.5% failed by dislocation, 0.7% by the locking ring breaking, and 10% by acetabular loosening.
No evidence of loosening of the acetabular components was seen in the surviving patients other than the case with late cup pullout. The failed case was a cemented liner placed into an apparently well ingrown cup. Guyen et al. [18] reported failure modes for 43 Omnifit constrained liners (Stryker Orthopaedics, Mahwah, NJ, USA) and Cooke et al. [12] reported similar problems with pullout associated with three of eight failures in a series of 58 Omnifit liners. In the study by Guyen et al. [18], 11 (26%) failed at the bone-implant interface in newly implanted cups despite the use of multiple screws (range, three to eight). They recommended the use of large heads in newly implanted cups with poor fixation and, if dislocation occurs, to use a constrained device as a salvage option once the cup is ingrown. We have not found this necessary with the TLC liner. It has been our practice to use multiple screws with a new acetabular shell.
Our study suggests this focal constrained acetabular liner is associated with a relatively low risk of early dislocation in patients at high risk for dislocation. Further monitoring is necessary to establish the durability of the implant.
Acknowledgments
We thank Donald Garbuz MD, and Nelson Greidanus MD, for contributing patients to the study; and Daphné Savoy, Research Coordinator, for her assistance in the preparation of the manuscript.
Footnotes
One of the authors certifies that he (JTM) has or may receive payments or benefits, during the study period, an amount of less than USD 10,000, from Zimmer, Inc (Warsaw, IN, USA).
One of the authors certifies that he (BAM) has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Zimmer, Inc. One of the authors certifies that he (CDP) has or may receive payments or benefits, during the study period, an amount of USD 10,000–USD 100,000 from Zimmer, Inc and USD 10,000–USD 100,000 from DePuy Synthes Canada Ltd (Markham, Ontario, Canada). The remaining author (MHV) certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article. The institution of the authors (JTM, MHV, BAM, CPD) has received funding from Zimmer, Inc, DePuy Synthes Canada Ltd, Johnson & Johnson (Canada) Inc (Markham, Ontario, Canada), Stryker Canada (Hamilton, Ontario, Canada), and Bayer Inc (Toronto, Ontario, Canada).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792. [PubMed] [Google Scholar]
- 2.Amstutz HC, Le Duff MJ, Beaulé PE. Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res. 2004;429:108–116. doi: 10.1097/01.blo.0000150310.25603.26. [DOI] [PubMed] [Google Scholar]
- 3.Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17–23. doi: 10.1016/0883-5403(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 4.Annual Report. AOA: Adelaide; 2010. [Google Scholar]
- 5.Berend KR, Lombardi AV, Mallory TH, Adams JB, Russell JH, Groseth KL. The long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failures. J Arthroplasty. 2005;20:93–102. doi: 10.1016/j.arth.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Berend KR, Lombardi AV, Welch M, Adams JB. A constrained device with increased range of motion prevents early dislocation. Clin Orthop Relat Res. 2006;447:70–75. doi: 10.1097/01.blo.0000218745.07366.60. [DOI] [PubMed] [Google Scholar]
- 7.Bigsby E, Whitehouse MR, Bannister GC, Blom AW. The medium term outcome of the Omnifit constrained acetabular cup. Hip Int. 2012;22:505–510. doi: 10.5301/HIP.2012.9746. [DOI] [PubMed] [Google Scholar]
- 8.Bremner BRB, Goetz DD, Callaghan JJ, Capello WN, Johnston RC. Use of constrained acetabular components for hip instability: an average 10-year follow-up study. J Arthroplasty. 2003;18:131–137. doi: 10.1016/S0883-5403(03)00295-X. [DOI] [PubMed] [Google Scholar]
- 9.Callaghan JJ, Heithoff BE, Goetz DD, Sullivan PM, Pedersen DR, Johnston RC. Prevention of dislocation after hip arthroplasty: lessons from long-term followup. Clin Orthop Relat Res. 2001;393:157–162. doi: 10.1097/00003086-200112000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Carter AH, Sheehan EC, Mortazavi SM, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;26(Suppl):46–52. doi: 10.1016/j.arth.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 11.Cogan A, Klouche S, Mamoudy P, Sariali E. Total hip arthroplasty dislocation rate following isolated cup revision using Hueter’s direct anterior approach on a fracture table. Orthop Traumatol Surg Res. 2011;97:501–505. doi: 10.1016/j.otsr.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Cooke CC, Hozack W, Lavernia C, Sharkey P, Shastri S, Rothman RH. Early failure mechanisms of constrained tripolar acetabular sockets used in revision total hip arthroplasty. J Arthroplasty. 2003;18:827–833. doi: 10.1016/S0883-5403(03)00325-5. [DOI] [PubMed] [Google Scholar]
- 13.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 14.Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty. 2005;20(Suppl 3):103–107. [DOI] [PubMed]
- 15.Engh CA, Jr, Sychterz CJ, Young AM, Pollock DC, Toomey SD, Engh CA., Sr Interobserver and intraobserver variability in radiographic assessment of osteolysis. J Arthroplasty. 2002;17:752–759. doi: 10.1054/arth.2002.33554. [DOI] [PubMed] [Google Scholar]
- 16.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Valle Della CJ, Gross AE. The Frank Stinchfield Award: dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356. doi: 10.1007/s11999-011-2146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goetz DD, Capello WN, Callaghan JJ, Brown TD, Johnston RC. Salvage of a recurrently dislocating total hip prosthesis with use of a constrained acetabular component. A retrospective analysis of fifty-six cases. J Bone Joint Surg Am. 1998;80:502–509. doi: 10.2106/00004623-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Guyen O, Lewallen DG, Cabanela ME. Modes of failure of Osteonics constrained tripolar implants: a retrospective analysis of forty-three failed implants. J Bone Joint Surg Am. 2008;90:1553–1560. doi: 10.2106/JBJS.G.00317. [DOI] [PubMed] [Google Scholar]
- 19.Hamadouche M, Biau DJ, Huten D, Musset T, Gaucher F. The use of a cemented dual mobility socket to treat recurrent dislocation. Clin Orthop Relat Res. 2010;468:3248–3254. doi: 10.1007/s11999-010-1404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Havelin LI, Robertsson O, Fenstad AM, Overgaard S, Garellick G, Furnes O. A Scandinavian experience of register collaboration: the Nordic Arthroplasty Register Association (NARA) J Bone Joint Surg Am. 2011;93(Suppl 3):13–19. doi: 10.2106/JBJS.K.00951. [DOI] [PubMed] [Google Scholar]
- 21.Hernigou P, Filippini P, Flouzat-Lachaniette C-H, Batista SU, Poignard A. Constrained liner in neurologic or cognitively impaired patients undergoing primary THA. Clin Orthop Relat Res. 2010;468:3255–3262. doi: 10.1007/s11999-010-1340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 23.Knudsen R, Ovesen O, Kjaersgaard-Andersen P, Overgaard S. Constrained liners for recurrent dislocations in total hip arthroplasty. Hip Int. 2007;17:78–81. doi: 10.1177/112070000701700204. [DOI] [PubMed] [Google Scholar]
- 24.Lachiewicz PF, Soileau ES. Low early and late dislocation rates with 36- and 40-mm heads in patients at high risk for dislocation. Clin Orthop Relat Res. 2012 May 11 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 25.Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res. 2008;466:389–395. doi: 10.1007/s11999-007-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lautridou C, Lebel B, Burdin G, Vielpeau C. [Survival of the cementless Bousquet dual mobility cup: minimum 15-year follow-up of 437 total hip arthroplasties] [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:731–739. doi: 10.1016/j.rco.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Meek RMD, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 28.Eleven Year Report. Christchurch, New Zealand: NZOA; 2010. [Google Scholar]
- 29.Noble PC, Durrani SK, Usrey MM, Mathis KB, Bardakos NV. Constrained cups appear incapable of meeting the demands of revision THA. Clin Orthop Relat Res. 2012;470:1907–1916. doi: 10.1007/s11999-011-2212-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah SN, Kaye RJ, Kelly NH, Su EP, Padgett DE, Wright TM. Retrieval analysis of failed constrained acetabular liners. J Arthroplasty. 2009;24:54–57. doi: 10.1016/j.arth.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 31.Shapiro GS, Weiland DE, Markel DC, Padgett DE, Sculco TP, Pellicci PM. The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty. 2003;18:250–258. doi: 10.1054/arth.2003.50090. [DOI] [PubMed] [Google Scholar]
- 32.Shrader MW, Parvizi J, Lewallen DG. The use of a constrained acetabular component to treat instability after total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2179–2183. doi: 10.2106/00004623-200311000-00019. [DOI] [PubMed] [Google Scholar]
- 33.Turner RS. Postoperative total hip prosthetic femoral head dislocations. Incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994;301:196–204. [PubMed] [Google Scholar]
- 34.Vasukutty NL, Middleton RG, Matthews EC, Young PS, Uzoigwe CE, Minhas THA. The double-mobility acetabular component in revision total hip replacement: the United Kingdom experience. J Bone Joint Surg Br. 2012;94:603–608. doi: 10.1302/0301-620X.94B5.27876. [DOI] [PubMed] [Google Scholar]
- 35.Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;26:16–23. doi: 10.1016/j.arth.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 36.Williams JT, Jr, Ragland PS, Clarke S. Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop. 2007;31:273–277. doi: 10.1007/s00264-006-0191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang C, Goodman SB. Outcome and complications of constrained acetabular components. Orthopedics. 2009;32:115. [PubMed] [Google Scholar]
- 38.Yun AG, Padgett D, Pellicci P, Dorr LD. Constrained acetabular liners: mechanisms of failure. J Arthroplasty. 2005;20:536–541. doi: 10.1016/j.arth.2004.12.054. [DOI] [PubMed] [Google Scholar]