Abstract
Background
Revision hip surgery of the femur for patients with substantial bone loss is challenging. We previously reported 41 patients (44 hips) treated with femoral impaction grafting followed for a minimum of 2 years. The survivorship, using femoral reoperation for symptomatic aseptic loosening as the end point, was 97% at 8 years. However, data on longer term survival are crucial to adequately compare this surgical technique with other types of revision hip arthroplasty procedures.
Questions/purposes
We therefore asked what the survivorship of impaction bone grafting was at longer followup, if the severity of bone loss was associated with failure, and finally, if longer length stems had improved survival compared with shorter stems.
Methods
Between 1993 and 2002, 78 femoral revisions were performed in 71 patients using impaction grafting. The average age of the patients was 67 years (range, 33–84 years). Sixty-nine of the 71 patients were available for followup evaluation. We obtained Harris hip scores preoperatively and postoperatively. Radiographs were measured for radiolucent lines. Patients were followed a minimum of 2 years (average, 10.6 years; range, 2–19 years).
Results
Survival of the femoral component without revision for any cause was 93% (confidence interval [CI], 83%–97%) and for aseptic loosening was 98% (CI, 87%–100%) at 19 years. Neither severity of bone loss nor the length of the stem predicted failure.
Conclusions
Impaction bone grafting has a high survival of 93% at the 19-year followup for patients with severe bone loss of their femur.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Revision hip surgery of the femur for patients with substantial bone loss can pose a major challenge. The treatment has been described using extensively coated femoral stems [3, 13, 26], modular stems with distal tapers [10, 12, 14, 15, 17, 19, 22], and impaction bone grafting with cemented polished stems [4, 7, 16, 21, 23, 25, 27]. Femoral impaction grafting, first reported by Gie et al. in 1993 [5], has the advantage of adding bone to the deficient femur, but it is a time-consuming procedure with reported risks of fracture ranging from 5% to 12% [1, 5, 7, 9].
We previously reported our results of 41 patients (44 hips) with impaction bone grafting followed a minimum of 2 years (average, 4.7 years; range, 2–8 years) [11]. Survivorship using femoral reoperation for symptomatic aseptic loosening as the end point was 95% (confidence interval [CI], 72%–99%) at 8 years. Four fractures (three intraoperative and one postoperative stress fracture) occurred but none of the patients required revision surgery. Additionally, one patient had a trochanteric nonunion and one patient sustained a dislocation. Several authors have reported high survival (77%–100%) at 5 to 19 years for femoral bone impaction grafting [4, 7, 16, 21, 23, 25, 27]. Halliday et al. [7], reporting findings of the developers of the technique, found a survivorship of 90.5% at 11 years for femoral reoperation and 99.1% at 11 years for femoral revision for aseptic loosening as the end point. In a retrospective study of 79 patients (81 hips) followed 5 to 17 years, Garcia-Cimbrelo et al. [4] found a survival rate for reoperation for any cause of 98.6%. The largest study included 1305 revisions from the Swedish National Arthroplasty Registry [16]. Survival for all causes of failure was 94% for women and 94.7% for men at 15 years. The authors concluded the technique of impaction bone grafting was reliable, learned rapidly by the Swedish surgeons, and produced a predictably low incidence of aseptic loosening.
Sporer and Paprosky [24] reported the use of a modular cementless femoral stem as an alternative technique to impaction grafting for femoral revision of hips with greater loss of bone (using the classifications of Paprosky Type III, IV [18] and Endo-Klinik Grade 3, 4 [2]). Additionally, the relative ease of insertion of the more recently available modular tapered stems [10, 12, 14, 15, 17, 22] resulted in our performing fewer impaction bone grafting procedures in patients needing femoral revision. However, if we are to compare impaction bone grafting survival with modular tapered stems, then it is crucial to study longer followup to either confirm or refute the results of others.
We therefore determined (1) the survival of our femoral impaction grafting at 2 to 19 years; (2) if the severity of bone loss based on the Paprosky and Endo-Klinik classifications predicted revision; and (3) if longer stems had a higher survival than shorter stems.
Patients and Methods
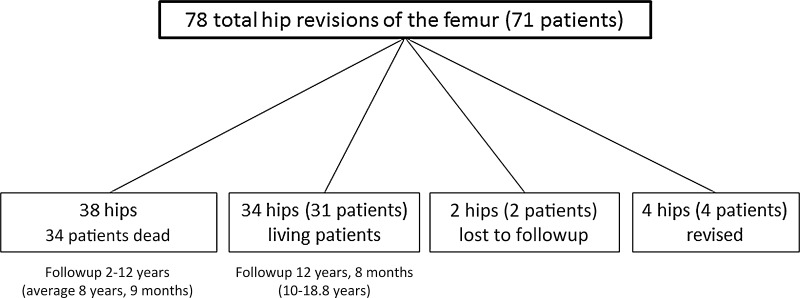
In 1993, we began using impaction bone grafting for femoral revision hip surgery. Professor Robin Ling, who developed the technique, participated in the preoperative planning and surgery for the first two patients. Between 1993 and 2002, we performed 78 femoral revisions using impaction grafting in 71 patients (Fig. 1). The indications for femoral impaction allografting were mechanical loosening of the femoral component and lack of femoral cancellous bone with either an intact cortical shell or a proximal femur that could be reconstructed with mesh or strut allograft, or both. Patients were primarily younger patients with bone loss for whom we could add bone to rebuild their femur or elderly patients with femoral canals greater than 18 mm. The bone loss was best categorized by the Paprosky or Endo-Klinik classification as Paprosky Type II, III, or IV or Endo-Klinik Grade 2, 3, or 4.
Fig. 1.
The schematic represents the outcome of the 78 revisions in 71 patients who had femoral impaction grafting. The last followup interval (range and average) for the dead and living patients is also noted in the figure.
The contraindications for femoral impaction allografting were (1) patients with healthy bone (Paprosky Type I or II or Endo-Klinik Grade 1 or 2); (2) patients whose proximal femur could not be reconstructed into a tube that would accept the impaction technique; and (3) the presence of infection. The group accounted for 18% of all the femoral revisions during that interval. The remaining 82% of patients were treated with uncemented techniques using extensively coated stems or cemented stems. The impaction bone grafting group included 39 males and 32 females. The average age of the patients was 67 years with a range from 33 to 84 years. The most common primary diagnosis was osteoarthritis and the indication for revision arthroplasty in the patients was mechanical failure (Table 1). Thirty-four patients (38 hips) had died and information before death was available on these patients. Four (four hips) of the 71 patients (78 hips) had revision surgery, and two patients (2 hips) were lost to followup leaving 31 patients (34 hips) living with impaction grafted hips still intact. The followup on the living patients was 12 years 8 months (range, 10–19 years) and the followup on the entire cohort was 10 years 6 months (range, 2–19 years) (Fig. 1).
Table 1.
Patient data
| Original diagnosis, number of hips (number of patients) | Number of hips | Number of previous revisions | Preoperative HHS | Postoperative HHS |
|---|---|---|---|---|
| Osteonecrosis 45 (43) |
39 | 0 | 45 (SD 16) |
88 (SD 11) |
| Traumatic arthritis 11 (11) |
20 | 1 | ||
| Inflammatory arthritis 8 (8) |
17 | 2 | ||
| Avascular necrosis 6 (4) |
2 | 3 | ||
| Developmental dysplasia of the hip 5 (3) |
||||
| Other childhood hip disease 3 (2) |
HHS = Harris hip score.
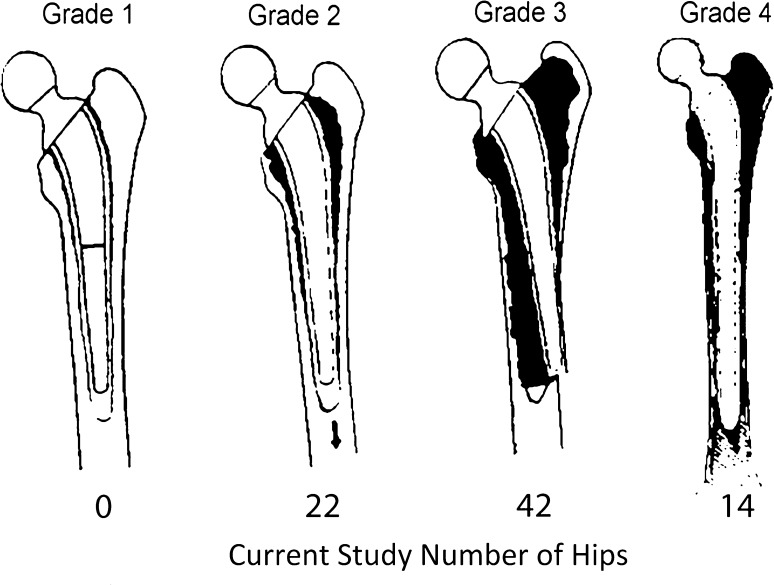
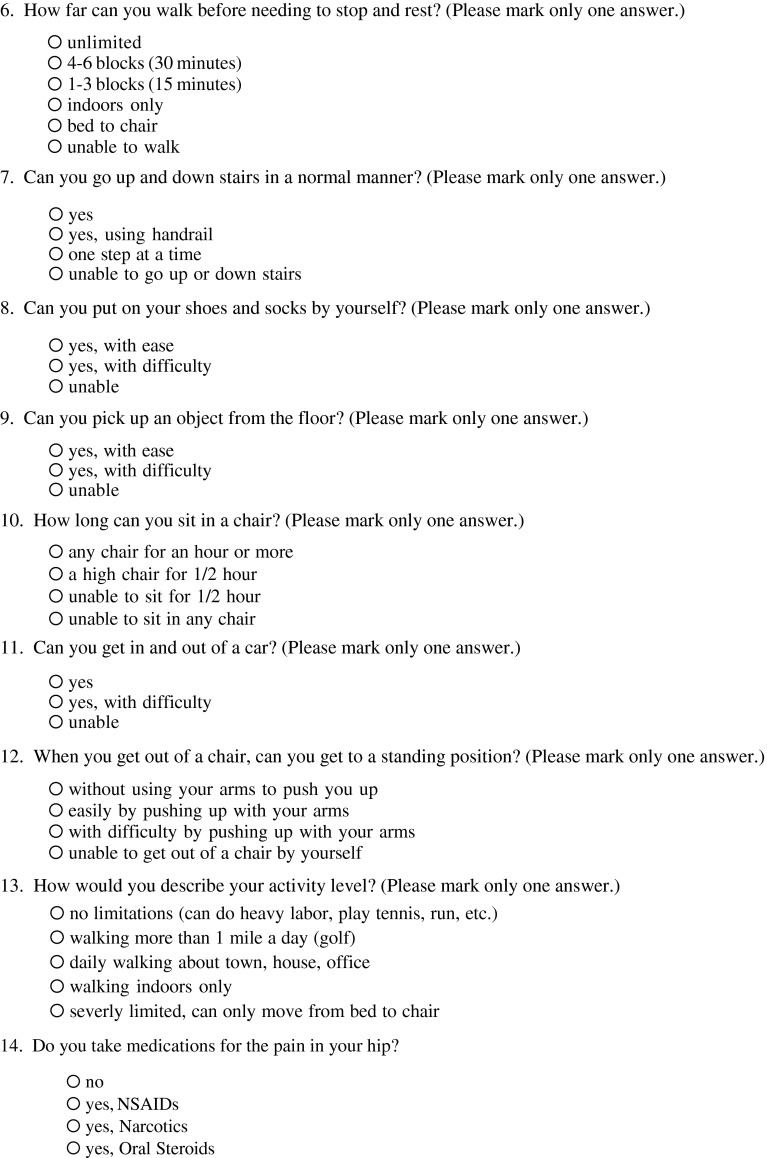
Preoperatively the bone was classified using the Endo-Klinik classification [2] (Fig. 2) and the classification of Paprosky [18] (Fig. 3). We found severe bone loss (Endo-Klinik Grade 3 and Grade 4) in 72% of our patients (Fig. 2).
Fig. 2.
A schematic of the Endo-Klinik classification for femoral bone loss is represented in this figure. The number below each respective grade represents the number of hips in the study that had bone loss described by the grade shown. (Reproduced and adapted with permission and copyright of the British Editorial Society of Bone and Joint Surgery [Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;1:14–21.]).
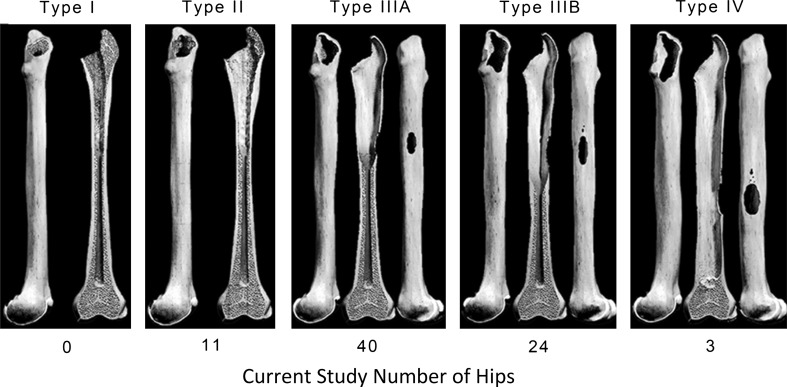
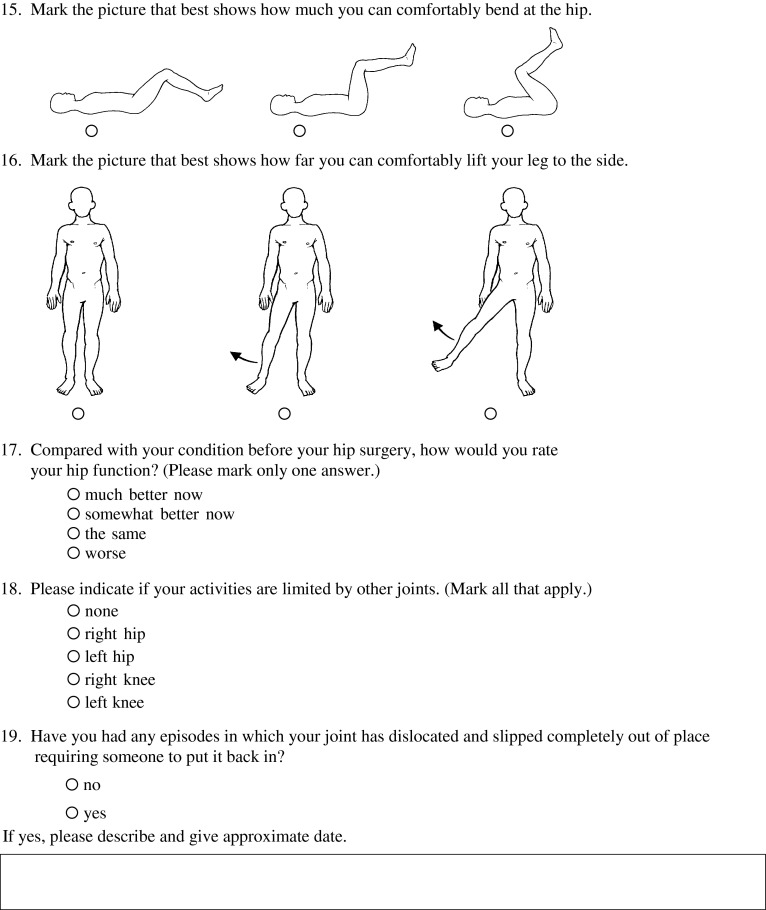
Fig. 3.
A schematic of the Paprosky classification representing bone loss is represented in this figure. The number of hips below each type represents the number of hips in the study with bone loss reflecting the type above the number.
We previously described the surgical technique [11] and it has not changed. One surgeon (KLG) performed all of the procedures. After the previous stem, bone cement, and other intramedullary foreign material had been removed, a cement plug was placed 2 cm distal to the most distal area of osteolysis. The canal was then filled with unwashed cancellous bone chips prepared with a bone mill from fresh-frozen allograft femoral heads (two to three femoral heads were used for the impaction grafting technique). The bone chips were packed firmly on the previously placed plug. A series of cannulated, cylindrical, and conical tamps were used to impact the bone chips. The cannulated instruments were then removed and a trial component was placed. A trial reduction was performed to assess for stability of the hip. The stem types were also as previously reported, and within this group, 33 patients received a collarless polished taper (Zimmer, Warsaw, IN, USA) and 45 received a Spectron (Smith & Nephew, Memphis, TN, USA) with 18 of the Spectron stems of a standard length (120–140 mm) and 27 of a longer length (ranging from 175 to 225 mm). In general, the stems were selected based on bone defect location and our concern about the risk of femur fracture if a shorter stem was selected.
The patients were mobilized on postoperative Day 1 with protected weightbearing using a walker or crutches for 6 weeks and then allowed to weightbear as tolerated. Physical therapy was performed under the supervision of a physical therapist while the patients were hospitalized. Over the ensuing 6 weeks, the patients were weaned from their walking aid to a cane. At approximately 6 months, the patients were independent of walking aids.
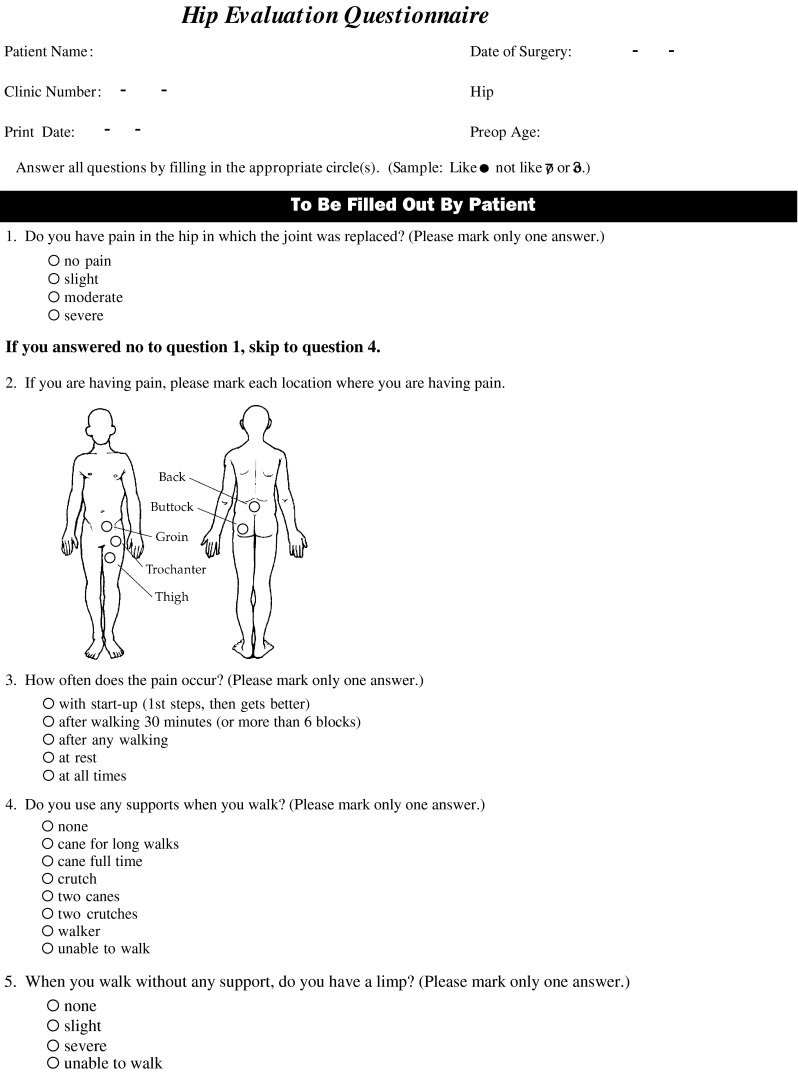
Patients were followed postoperatively at 6 weeks, 3 months, 1 year, 2 years, and every year thereafter. The patients were evaluated clinically using the Harris hip score [8] preoperatively and postoperatively. If patients had not returned for followup evaluation, they were contacted and asked to return for followup. Six patients were unable to return at periods between 10 and 13 years; they were asked to complete a questionnaire (Appendix A) and to have radiographs taken by their local physician. All of the patients provided the completed questionnaire and all provided radiographs. The immediate postoperative radiograph and the most recent radiographs were compared to assess for changes of component position.
Two of us (KLG, NDO) simultaneously evaluated all radiographs [6]. The immediate postoperative radiographs and the most recent radiographs were compared to assess a change in stem position. Measurements were made comparing the stem positions with respect to a fixed point on the radiographs for each respective patient (for example, trochanteric wires, tip of the greater trochanter, proximal aspect of the lesser trochanter). Because subsidence is a normal feature in impaction grafting, we were unable to use the change in stem position as definitive evidence of loosening. Serial radiographs were therefore used to identify progressive radiolucent lines that were circumferential and greater than 2 mm as a definition for stem loosening [8].
Survival of the femoral component was estimated using the method of Kaplan and Meier and comparisons of survival made using the log-rank test. Fisher’s exact test was used to associate bone loss to component survival. Fisher’s exact test was also used to compare failure (yes/no) with short versus long stems.
Results
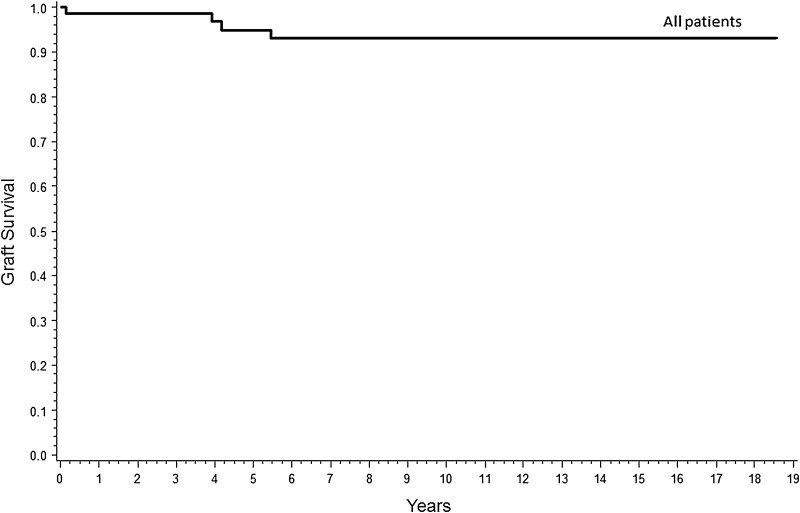
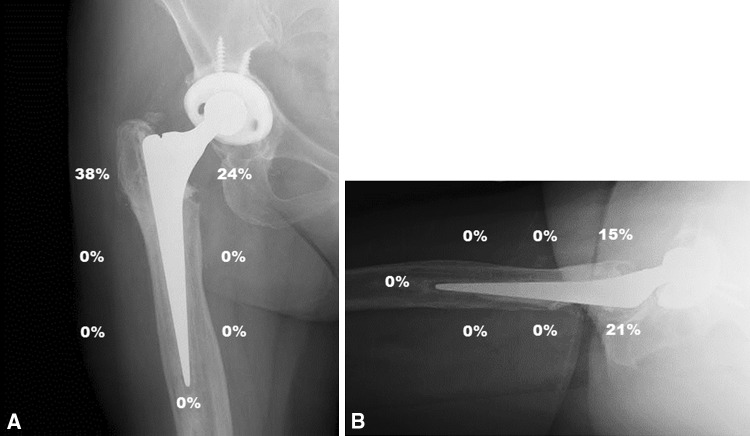
Survival of the femoral component without revision for any cause was 93% (95% CI, 83%–97%) at 19 years (Fig. 4). Survival of the femoral component without revision for aseptic loosening was 98% (95% CI, 87%–100%) at 19 years. Twenty-five of the hips were pain-free or caused mild pain, four hips caused moderate or severe pain, and five patients were unable to give an accurate history because of dementia. Eighteen patients were able to ambulate without walking aids, seven used a cane, and four patients used a walker. Overall, 27 of the hips had Harris hip scores above 80 points. Radiolucent lines were common in the proximal zones of the stem (Fig 5A–B). None of the stems had evidence of loosening with circumferential radiolucent lines.
Fig. 4.
The graph shows the survival of the femoral component without revision for any cause was 93% (95% CI, 83%–97%) at 19 years.
Fig. 5A–B.
(A) The AP radiograph (a study patient) shows the Gruen zones with the percent of patients who had radiolucent lines visible on their radiograph at their most recent followup. (B) The lateral radiograph shows the Gruen zones with the percent of patients who had radiolucent lines visible on their radiograph at their most recent followup.
Femoral bone loss at the time of revision was not associated with stem survivorship using either the Endo-Klinik or the Paprosky classifications (Endo-Klinik p = 1.0, Paprosky p = 0.65). One of 22 Endo-Klinik Grade 2 hips failed and three of 56 Endo-Klinik Grades 3 or 4 failed. Similarly, one of 11 Paprosky Type II hips failed and three of 67 Paprosky Type III or IV failed. The length of the stem was also not associated with implant survival. Three failures occurred in 51 hips with a short stem and one failure occurred in 27 long stems (p = 1.00).
Of the 71 patients, complications occurred in 10 (14%). Six patients sustained a fracture and three of these were diagnosed intraoperatively. The intraoperative fractures occurred during stem extraction or cement removal and not during the impaction of the bone graft. One of the intraoperative fractures occurred through the metaphysis and was treated with a long stem prosthesis. One fracture was also in the proximal metaphysis of a 33-year-old patient with rheumatoid arthritis. The fracture was stabilized with a mesh and wires and the impaction bone grafting technique performed. This particular patient developed aseptic loosening and the hip was revised 6 years postoperatively. The third intraoperative fracture was also proximal and fixed intraoperatively. Three fractures occurred postoperatively, one was treated with a plate and screws, one required revision with a long-stemmed prosthesis, and one was a stress fracture below the tip of the stem that resolved with protected weightbearing. Two patients sustained a dislocation but neither has required further surgery. Two patients developed periprosthetic infections that were successfully treated with a two-stage exchange. Four of the hips were revised.
Discussion
Impaction bone grafting of the femur for revision surgery has been a successful option for patients with major bone loss requiring surgery. A number of studies have reported followups ranging from means of 7.5 to 12.6 years for this technique (Table 2). These studies suggest survivorship ranging from 70.8 to 92% at 7.5 to 18 years. The most common complications reported in the studies were fracture (5%–12% of patients), dislocation (3%–4% of patients), and infection (0%–2.5% of patients) (Table 2). Long-term survival results are critical to assess this technique. We therefore determined the survival of the femoral component at this long-term followup, whether femoral bone loss at the time of revision correlated with stem survival, and whether stem length was associated with implant survival.
Table 2.
Impaction bone grafting results
| Study | Number of patients/hips | Demographics | Defects/classifications | Implant selection | Length of followup (years) (range) | Complications | Survivorship |
|---|---|---|---|---|---|---|---|
| Ornstein et al. [16] | 1188/1305 | 650 F 538 M 71 years |
NS | 108 standard stems 145 long stems |
8.1 (5–18) | 33 fracture/infection 11 loosening NS dislocation |
99% for aseptic loosening 74% for any reason |
| Halliday et al. [7] | 207/226 | NS | 12 Grade 1 106 Grade 2 62 Grade 3 6 Grade 4 |
Standard stems | 10.4 (5–11) | 5% fracture 2.2% infection 1% loosening NS dislocation |
99% for aseptic loosening 90.5% for any reason |
| Garcia-Cimbrelo et al. [4] | 79/81 | 48 F 33 M 64 years |
20 Grade 2 40 Grade 3 21 Grade 4 |
69 standard stem 12 long stems |
10.4 (5–17) | 7.5% fracture 1% infection 1% loosening |
100% Grade 2 81% Grade 3 at 10 years 70.8% Grade 4 |
| Schreurs et al. [20] | 33/33 | 24 F 9 M 63 years |
3 Grade 1 14 Grade 2 13 Grade 3 4 Grade 4 |
Standard stems | 10.4 (8–13) | 11% fracture 0% infection 0% loosening 0% dislocation |
100% for aseptic loosening 85% for any reason |
| Wraighte and Howard [27] | 75/75 | 35 F 40 M 68 years |
2 Grade 1 19 Grade 2 50 Grade 3 4 Grade 4 |
Standard stems | 10.5 (6.3–14.1) | 6.7% fracture 2.5% infection 0% loosening 4% dislocation |
92% |
| Ten Have et al. [25] | 29/31 | 23 F 6 M 65 years |
1 Grade 1 11 Grade 2 9 Grade 3 11 Grade 4 |
Standard stems | 12.6 (10–14.7) | 12% fracture NS infection NS loosening 3% dislocation |
77.4% |
| Sierra et al. [23] | 40/42 | 26 F 14 M 73.8 years |
2 Grade 1 4 Grade 2 25 Grade 3 9 Grade 4 |
All long stems | 7.5 | 29% complications | 90% |
| Current study | 71/78 | 32 F 39 M 67 years |
0 Grade 1 22 Grade 2 42 Grade 3 14 Grade 4 |
51 standard stems 27 long stems |
12.8 (10–18.8) | 6% fracture 2.5% infection 1% loosening 2.5% dislocation |
98% for aseptic loosening 93% for any reason |
F = female; M = male; NS = not stated.
We note four limitations of this study. First, this is a retrospective study without a control group. Patients were selected for this surgical procedure based on the amount of bone loss. This selection bias accounts for only 18% of all revision hips having this surgical technique. Additionally, patients were not randomized to alternative treatments. Second is that the data collected were from a single surgeon’s experience and may not be applicable to all practices. Third, the radiographs were measured by the authors manually and by the treating surgeon with the potential for observer bias. However, objective measurements were taken to evaluate a change in the component position and/or the presence of circumferential radiolucent lines greater than 2 mm. Additionally, osteolysis was quantified by measuring in millimeters to lessen the risk of observer bias. The manual measurement is less accurate than roentgen stereophotogrammetric analysis that has been used to measure implant position change and is more accurate but was not used in this study.
We found impaction grafting provided a survival rate of 93% at 19 years. The results are consistent with previously reported studies of comparable followup. Schreurs et al. reported 33 patients with 33 hips followed for an average of 10.4 years with a 100% survival for aseptic loosening and 85% for any reason [20]. Wraighte and Howard reported 75 patients with 75 hips also followed for over 10 years with 92% survival at 10.5 years [27]. Sierra et al. reported 40 patients all treated with longer stems with a 90% survival at 10 years [23] (Table 2).
We found implant survival did not correlate with the amount of bone loss by either the Endo-Klinik or Paprosky classifications. In contrast, Garcia-Cimbrelo et al. [4] found implant survival was associated with bone loss; patients with Endo-Klinik Grade II defects had a survival rate of 100% at 10 years, Endo-Klinik Grade III 81% at 10 years, and Endo-Klinik Grade IV 70.8% at 10 years. We have no explanation for the discrepancy in findings.
We also found the length of the stem did not affect implant survival but we purposely selected the long stems for the more difficult reconstructions and, thus, there was selection bias for the prostheses. Three of the long-term studies [4, 16, 23] also selected long stems for their patients who had more complicated revisions and their results are consistent with our results (Table 2).
Impaction bone grafting has a high survival of 77% to 100% at 19 years and, in our opinion, continues to have a role for challenging femoral revisions. The use of modern, modular tapered stems has been reported since 2003 as a cementless option with reported good survival (with results as high as 97% at 40 months) [10]. The reported followup of modular tapered stems is less than 10 years in all of these studies. We believe the technique of impaction bone grafting should remain as a treatment option for those patients with severe femoral bone loss. The role of impaction bone grafting will be better defined as the long-term studies of modular femoral stems are available for comparison.
Acknowledgments
We thank Dana M. Schwarz RN, for her assistance with the manuscript.
Appendix
Footnotes
None of the authors nor has their institution received funding related to the content of this study. One or more of the authors (KLG) has received funding that is not related to the content of this manuscript. The funding source includes Biomet (Warsaw, IN, USA) (KLG) in the amount of USD 100,000 to USD 1,000,000. The institution of the authors has received funding from TRAK Surgical Inc (Omaha, NE, USA), Smith & Nephew (Memphis, TN, USA), Biomet, Vanguard (Valley Forge, PA, USA), Exponent (Menlo Park, CA, USA), Gruppo Bioimplanti (St Paul, MN, USA), and Renovis (Redlands, CA, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that the institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
This work was performed at the University of Nebraska Medical Center, Omaha, NE, USA.
References
- 1.Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID. Massive early subsidence following femoral impaction grafting. J Arthroplasty. 1997;5:535–540. doi: 10.1016/S0883-5403(97)90176-5. [DOI] [PubMed] [Google Scholar]
- 2.Engelbrecht E, Heinert K. Klassifikation und behandlungsrichtlinien von knochensubstanzverlusten bei revisionsoperationen am hüftgelenk. In: Arcq M, ed. Primär- Und Revisions-Alloarthroplastik Hüft- Und Kniegelenk. 1987:189–201.
- 3.Engh CA, Griffin WL, Marx CL. Cementless acetabular components. J Bone Joint Surg Br. 1990;1:53–59. doi: 10.1302/0301-620X.72B1.2298795. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Cimbrelo E, Garcia-Rey E, Cruz-Pardos A. The extent of the bone defect affects the outcome of femoral reconstruction in revision surgery with impacted bone grafting: a five- to 17-year follow-up study. J Bone Joint Surg Br. 2011;11:1457–1464. doi: 10.1302/0301-620X.93B11.27321. [DOI] [PubMed] [Google Scholar]
- 5.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;1:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 6.Gruen TA, McNeice GM, Amstutz HC. ‘Modes of failure’ of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 7.Halliday BR, English HW, Timperley AJ, Gie GA, Ling RS. Femoral impaction grafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg Br. 2003;6:809–817. [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;4:737–755. [PubMed] [Google Scholar]
- 9.Hostner J, Hultmark P, Karrholm J, Malchau H, Tveit M. Impaction technique and graft treatment in revisions of the femoral component: laboratory studies and clinical validation. J Arthroplasty. 2001;1:76–82. doi: 10.1054/arth.2001.9830. [DOI] [PubMed] [Google Scholar]
- 10.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;3(Suppl 1):94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 11.Mahoney CR, Fehringer EV, Kopjar B, Garvin KL. Femoral revision with impaction grafting and a collarless, polished, tapered stem. Clin Orthop Relat Res. 2005;432:181–187. doi: 10.1097/01.blo.0000150320.73465.82. [DOI] [PubMed] [Google Scholar]
- 12.McInnis DP, Horne G, Devane PA. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty. 2006;3:372–380. doi: 10.1016/j.arth.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Moreland JR, Moreno MA. Cementless femoral revision arthroplasty of the hip: minimum 5 years followup. Clin Orthop Relat Res. 2001;393:194–201. doi: 10.1097/00003086-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Mumme T, Muller-Rath R, Weisskopf M, Andereya S, Neuss M, Wirtz DC. The cement-free modular revision prosthesis MRP-hip revision stem prosthesis in clinical follow-up. Z Orthop Ihre Grenzgeb. 2004;3:314–321. doi: 10.1055/s-2004-822795. [DOI] [PubMed] [Google Scholar]
- 15.Murphy SB, Rodriguez J. Revision total hip arthroplasty with proximal bone loss. J Arthroplasty. 2004;4(Suppl 1):115–119. doi: 10.1016/j.arth.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Ornstein E, Linder L, Ranstam J, Lewold S, Eisler T, Torper M. Femoral impaction bone grafting with the Exeter stem—the Swedish experience: survivorship analysis of 1305 revisions performed between 1989 and 2002. J Bone Joint Surg Br. 2009;4:441–446. doi: 10.1302/0301-620X.91B4.21319. [DOI] [PubMed] [Google Scholar]
- 17.Ovesen O, Emmeluth C, Hofbauer C, Overgaard S. Revision total hip arthroplasty using a modular tapered stem with distal fixation: good short-term results in 125 revisions. J Arthroplasty. 2010;3:348–354. doi: 10.1016/j.arth.2008.11.106. [DOI] [PubMed] [Google Scholar]
- 18.Paprosky WG, Aribindi R. Hip replacement: treatment of femoral bone loss using distal bypass fixation. Instr Course Lect. 2000;49:119–130. [PubMed] [Google Scholar]
- 19.Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty. 2007;7:993–999. doi: 10.1016/j.arth.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Schreurs BW, Arts JJ, Verdonschot N, Buma P, Slooff TJ, Gardeniers JW. Femoral component revision with use of impaction bone-grafting and a cemented polished stem. J Bone Joint Surg Am. 2005;11:2499–2507. doi: 10.2106/JBJS.D.02547. [DOI] [PubMed] [Google Scholar]
- 21.Schreurs BW, Luttjeboer J, Thien TM, de Waal Malefijt MC, Buma P, Veth RP, Slooff TJ. Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis. A concise follow-up, at eight to nineteen years, of a previous report. J Bone Joint Surg Am. 2009;3:646–651. doi: 10.2106/JBJS.G.01701. [DOI] [PubMed] [Google Scholar]
- 22.Schuh A, Werber S, Holzwarth U, Zeiler G. Cementless modular hip revision arthroplasty using the MRP titan revision stem: outcome of 79 hips after an average of 4 years’ follow-up. Arch Orthop Trauma Surg. 2004;5:306–309. doi: 10.1007/s00402-004-0656-7. [DOI] [PubMed] [Google Scholar]
- 23.Sierra RJ, Charity J, Tsiridis E, Timperley JA, Gie GA. The use of long cemented stems for femoral impaction grafting in revision total hip arthroplasty. J Bone Joint Surg Am. 2008;6:1330–1336. doi: 10.2106/JBJS.G.00055. [DOI] [PubMed] [Google Scholar]
- 24.Sporer SM, Paprosky WG. Femoral fixation in the face of considerable bone loss: the use of modular stems. Clin Orthop Relat Res. 2004;429:227–231. doi: 10.1097/01.blo.0000150120.80409.0d. [DOI] [PubMed] [Google Scholar]
- 25.Ten Have BL, Brouwer RW, van Biezen FC, Verhaar JA. Femoral revision surgery with impaction bone grafting: 31 hips followed prospectively for ten to 15 years. J Bone Joint Surg Br. 2012;5:615–618. doi: 10.1302/0301-620X.94B5.27909. [DOI] [PubMed] [Google Scholar]
- 26.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;4(Suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 27.Wraighte PJ, Howard PW. Femoral impaction bone allografting with an Exeter cemented collarless, polished, tapered stem in revision hip replacement: a mean follow-up of 10.5 years. J Bone Joint Surg Br. 2008;8:1000–1004. doi: 10.1302/0301-620X.90B8.20390. [DOI] [PubMed] [Google Scholar]