Abstract
Background
Low-velocity gunshots are often associated with extremity fractures. There is no consensus, however, on the use of antibiotics for these injuries.
Questions/purposes
We performed a literature review to answer the following questions: (1) Are antibiotics needed for the treatment of these fractures? (2) Is gram-negative coverage necessary? (3) How long should antibiotics be administered? And (4) which is the optimal administration route?
Methods
We conducted a MEDLINE® search and found only two relevant prospective, randomized studies. Further searches identified all case series with information on the use of antibiotics in gunshot fractures. In total, 33 studies provided enough data to answer the study questions. An assessment of the quality of the identified studies was performed. Twenty-three studies met at least ½ of the quality items of the assessment tool.
Results
Antibiotics did not significantly reduce the infection rate for fractures treated nonoperatively (1.7% with antibiotics versus 5.1% without) with the numbers available. There was no significant difference in infection rates when gram-negative coverage was added, either in nonoperatively treated fractures (1.7% versus 2.8%) or in operatively treated fractures (0% versus 2.5%). Duration of antibiotic administration did not significantly affect the infection rate. No difference was found between intravenous and oral antibiotic administration for nonoperatively treated fractures.
Conclusions
This literature review could not demonstrate a significant benefit with the use of antibiotics for low-velocity gunshot fractures treated nonoperatively; however, the statistical power for these comparisons was low in the available literature, which is insufficiently strong to recommend a treatment. Gram-negative coverage did not alter the infection rates in gunshot fractures, nor did longer duration of antibiotic administration. For fractures treated nonoperatively, oral antibiotics are as efficacious as intravenous antibiotics.
Introduction
Gunshot trauma remains a considerable cause of morbidity and socioeconomic cost globally [37]. In the United States, around 30,000 fatal and 65,000 to 75,000 nonfatal firearm injuries were reported annually during the last decade [8].
Despite extensive experience with civilian low-velocity gunshot wounds, no consensus exists on use of antibiotics for treatment of these injuries. Minor soft tissue wounds can successfully be treated in an outpatient basis, as was shown by Ordog et al. [31], who reported an infection rate of 1.8% in 16,892 low-velocity gunshot wounds (with associated minor fractures in only 4%). In the presence of fractures, however, a controversy still exists. The study of Howland and Ritchey [21] showed a low infection rate in low-velocity gunshot-induced fractures treated with superficial débridement. They reported no advantage in patients treated with antibiotics, and these results made them advocate against the use of antibiotics in the treatment of such injuries. Dickey et al. [10], in a prospective, randomized study, treated gunshot fractures nonoperatively with and without antibiotics and found similar infection rates between the two groups. However, many investigators advocate the use of antibiotics after gunshot trauma of the extremities [6, 15, 17, 41] since it has been shown, both in vitro [36, 40] and in the clinical setting [33], that most gunshot wounds are contaminated.
There is also no consensus regarding the type, duration, and route of antibiotics that should be administered. Shorter [1, 7, 10, 15, 17, 28, 30, 42] versus longer [11, 12, 16, 23, 24, 29, 33, 41] courses of antibiotics have been used. Some authors [1, 6, 22, 24, 39] advocate additional gram-negative coverage, while others [7, 11, 17, 19, 20, 23, 26, 30, 32, 38, 41, 42] regard it as unnecessary. For fractures treated nonoperatively, oral antibiotic administration has been proposed as equally effective as intravenous administration [13, 22, 41].
The controversy on the use of antibiotics does not apply for fractures necessitating fixation. Typically, treatment of fractures secondary to gunshots follows the accepted protocols for each area of injury [1, 3, 6, 7, 13, 16, 19, 20, 24–26, 28–30, 38, 39, 41, 42]. It is widely accepted that perioperative intravenous antibiotics are necessary when an implant is inserted; however, the optimal type and duration of antibiotics in these clinical scenarios are not known.
No meta-analysis or systematic overview of the role of antibiotics in fractures caused by gunshots has been published during the past 5 years. We therefore performed a systematic literature review to answer the following questions: (1) Are antibiotics needed for the treatment of these fractures? (2) Is gram-negative coverage necessary? (3) How long should antibiotics be administered? And (4) which is the optimal administration route?
Search Strategy and Criteria
We performed a search of the MEDLINE® database, restricted to the English language and human subjects. The keywords applied were “gunshot” or “shotgun” or “gun shot” AND “antibiotic” or “antibiotics” or “antimicrobial” or “antimicrobials,” which were included in the “Title” or “Abstract” fields (Fig. 1). This search identified 220 articles. The following criteria had to be fulfilled for a study to be included in our systematic analysis: gunshot fractures of the extremities, low-velocity gunshots, the inclusion of a total of at least 10 fractures in the study, and adequate information on the infection rate after the treatment of these patients, with or without antibiotics. We excluded studies focusing on soft tissue injuries; fractures of the head, spine, hand, or foot; isolated joint injuries; associated injuries of the abdomen or chest; injuries inflicted by shotguns; and combat or high-velocity injuries. This resulted in 14 articles [3, 5, 10, 11, 15, 17, 22, 24, 27, 32, 34, 38, 39, 41] fulfilling the inclusion criteria, and only four of them [10, 15, 17, 22] were comparative studies. Of these four comparative studies, only two were prospective, randomized controlled trials, and they actually addressed different issues on the use of antibiotics in gunshot-induced fractures treated nonoperatively. Dickey et al. [10] compared antibiotics versus no antibiotics, while Knapp et al. [22] compared intravenous versus oral antibiotics.
Fig. 1.
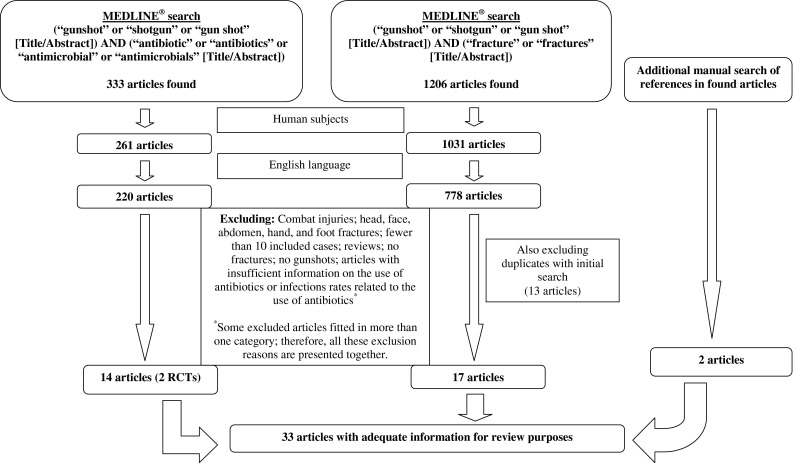
The flowchart illustrates the methodology for identifying relevant articles. RCT = randomized controlled trial.
We also evaluated the various Level IV clinical studies reporting on extremity fractures caused by low-velocity gunshots. Although these are considered lower-quality studies for the purpose of a literature review, these were the only data available that could be used to address some of the study questions. Most of these additional studies were case series focusing on the fracture treatments rather than the antibiotic therapies. We included all these studies, provided there was enough information on the use of antibiotics and the infection rates. To include as many of these studies as possible, we performed an additional MEDLINE® search restricted to the English language and human subjects. The keywords applied this time were “gunshot” or “shotgun” or “gun shot” AND “fracture” or “fractures” in the “Title” or “Abstract” fields. This search identified 778 articles; many of these were included in our initial search. These articles were examined according to the aforementioned inclusion and exclusion criteria, resulting in 17 additional studies [1, 6, 7, 12, 13, 16, 19–21, 23, 25, 26, 28–30, 35, 42] regarded as appropriate for inclusion in the review.
We also manually searched the references in the identified articles to find possible relevant articles not included in our MEDLINE® searches. This way we were able to identify two additional studies [14, 33] with information on the use of antibiotics for the treatment of gunshot fractures of the extremities.
In total, we identified 33 studies considered as providing enough data to answer one or more of the study questions. Some of these articles [5, 10, 11, 14, 15, 17, 21, 22, 28, 32–34, 41] did not provide information on the location of the extremity fracture, while others [10, 11, 14, 15, 17, 21, 32, 33, 41] included hand and feet fractures. Similarly, some studies [3, 6, 13, 19, 21, 27, 29, 32, 34] did not provide enough data on the type of gun used and others [3, 6, 13, 19, 21, 23, 26, 29, 33, 34, 38] reported mixed results; in many cases, the type of gun used could not be identified [3, 13, 26]. Whenever there was adequate data in the article, we excluded patients with hand or foot fractures and patients with injuries from high-velocity guns or shotguns. Whenever this was not possible, we included these patients, as reported.
Some studies [1, 3, 5, 7, 10–12, 16, 20, 24, 29, 32, 33, 38, 41] reported separately on superficial and deep infections; others [6, 13–15, 17, 22, 23, 26, 28, 30, 35, 39, 42] reported only on deep infections or superficial infections; and others [19, 21, 27, 34] did not differentiate between the two. To present uniform results, we considered the total number of infections reported from each study as the outcome variable. Pin tract infection was not considered an infection.
In terms of the antibiotic type used, we accepted that additional gram-negative coverage is provided by third-generation cephalosporins, ciprofloxacin, and aminoglycosides. First- and second-generation cephalosporins have narrow gram-negative coverage when administered alone and are considered to mainly provide gram-positive coverage.
Assessment of the quality of all studies included in the review was performed by means of a methodologic quality assessment list (Table 1), which consisted of 14 domains in six different categories as proposed by Hayden et al. [18]. Every item on the list was scored either positively if adequate information regarding the specific item was provided or negatively if there was inadequate information. A study scoring positively in at least ½ of the items (seven of 14) was considered a higher-quality study (n = 23; [1, 3, 5–7, 10–12, 16, 17, 19, 20, 22, 24–26, 29, 30, 33, 38, 39, 41, 42]), whereas the remaining were considered of lower quality (n = 10; [13–15, 21, 23, 27, 28, 32, 34, 35]). In an attempt to limit potential bias in some of the lower-quality studies, a separate analysis including only the higher-quality ones was performed along with the analysis of all 33 studies.
Table 1.
Assessment list used for measuring the quality of the 33 studies meeting the inclusion/exclusion criteria consisting of 14 domains in six different categories as proposed by Hayden et al. [18]
| Category | Category description | Domain | Domain description |
|---|---|---|---|
| A | Study participation/population of interest | 1 | Source population clearly defined |
| 2 | Study population described (demographics) | ||
| 3 | Study population represents population of interest (low-velocity extremity fractures, associated injuries, hand/feet fractures excluded) | ||
| B | Study attrition/followup | 4 | Completeness of followup described |
| 5 | Completeness of followup adequate (> 75% of study population for at least 6 months) | ||
| C | Factor of interest measurement | 6 | Factor of interest defined in study participants to sufficiently limit potential bias (information on whether antibiotics were given) |
| 7 | Factor of interest measured appropriately (adequate information on type, duration, and route of antibiotics administration) | ||
| D | Confounding factors measurement and account | 8 | Confounding factors described (type of gun used, type of treatment, comorbidities) |
| 9 | Confounding factors accounted for (type of gun used, type of treatment, comorbidities) | ||
| E | Outcome measurement | 10 | Outcome measure defined |
| 11 | Outcome measured appropriately (infection rate provided) | ||
| F | Results analysis | 12 | Analysis described |
| 13 | Analysis appropriate (information on superficial and deep infection provided separately) | ||
| 14 | Analysis provides sufficient presentation of data |
The data extracted from the studies included for analysis were (1) the total number of fractures that met the inclusion and exclusion criteria, (2) the use of antibiotics, (3) the type of antibiotics, (4) the duration of antibiotic use, (5) the use of fracture fixation, (6) and the number of total infections reported.
We performed a statistical analysis of categorical variables using the two-tailed Fisher’s exact test or the chi-square test, as appropriate. A p value of less than 0.05 was considered statistically significant.
Results
In an analysis of higher-quality studies about fractures treated nonoperatively (no fixation, no surgical irrigation and débridement [I&D]), with the numbers available, there were no significant differences detected in terms of infection rate between patients treated with antibiotics and those not treated. Nine higher-quality articles [1, 5, 10–12, 17, 22, 24, 41] that included 574 fractures had sufficient relevant data. The total percentage of infections in fractures treated with antibiotics was 1.7%, while the infection rate for fractures treated without antibiotic treatment was 5.1% (Table 2). The difference was not significant with the numbers available (p = 0.17). Inclusion of all studies, including 937 fractures, showed an infection rate of 2.4% when antibiotics were used versus 6.7% without antibiotics. With these numbers, the difference was significant (p = 0.031).
Table 2.
Infection rate with the use of antibiotics or not in gunshot-induced fractures treated nonoperatively
| Studies included in analysis | Infection rate (%) (number of infections/number of fractures treated) | p value | |
|---|---|---|---|
| Antibiotics | No antibiotics | ||
| Higher-quality studies (9 of 23) | 1.7 (9/535) | 5.1 (2/39) | 0.17 |
| All studies (17 of 33) | 2.4 (20/847) | 6.7 (6/90) | 0.031 |
The overall infection rate in all 1156 fractures in 23 articles [1, 3, 5–7, 10–12, 16, 17, 19, 20, 22, 24–26, 29, 30, 33, 38, 39, 41, 42] was 1.9%. Analysis of the need for antibiotics in fixation-treated fractures was not performed, as we found no such fractures treated without antibiotics in the literature [1, 3, 6, 7, 13, 16, 19, 20, 24–26, 28–30, 38, 39, 41, 42].
With the numbers available, the difference in infection rate with the addition of gram-negative coverage for the treatment of fractures treated nonoperatively (no fixation, no surgical I&D) was not significant (1.7% with both gram-positive and gram-negative coverage versus 2.8 % with only gram-positive coverage) (p = 0.22). Seven higher-quality studies [1, 10, 11, 17, 22, 24, 41] provided relevant data for a total of 404 fractures (Table 3). Similar results were found with the inclusion of all studies (Table 3). For fixation-treated gunshot-induced fractures, there were available data in 11 higher-quality studies [1, 6, 7, 19, 20, 24, 26, 30, 38, 39, 42] that included 334 fractures (Table 4). Similarly, there was no significant difference in infection rate with the addition of gram-negative coverage with the numbers available (0% with both gram-positive and gram-negative coverage versus 2.5 % with only gram-positive coverage) (p = 0.19). Similar results were found with the inclusion of all studies (Table 4).
Table 3.
Infection rates with gram-positive antibiotic coverage alone or combined gram-positive and gram-negative antibiotic coverage for gunshot-induced fractures treated nonoperatively
| Studies included in analysis | Infection rate (%) (number of infections/number of fractures treated) | p value | |
|---|---|---|---|
| Gram-positive coverage | Gram-positive and gram-negative coverage | ||
| Higher-quality studies (7 of 23) | 2.8 (3/108) | 1.7 (5/296) | 0.22 |
| All studies (10 of 33) | 3.4 (7/204) | 1.7 (5/296) | 0.24 |
Table 4.
Infection rates with gram-positive antibiotic coverage alone or combined gram-positive and gram-negative antibiotic coverage for gunshot-induced fractures treated with fracture fixation
| Studies included in analysis | Infection rate (%) (number of infections/number of fractures treated) | p value | |
|---|---|---|---|
| Gram-positive coverage | Gram-positive and gram-negative coverage | ||
| Higher-quality studies (11 of 23) | 2.5 (6/238) | 0.0 (0/96) | 0.19 |
| All studies (12 of 33) | 2.9 (7/241) | 0.0 (0/96) | 0.20 |
For fractures treated without surgery, there was no obvious benefit to longer antibiotic administration. Data from seven higher-quality studies [1, 10, 11, 17, 22, 24, 41], including 404 fractures (Table 5), showed no significant differences in infection rate among groups treated with antibiotics for 1 to 2 days (2.1%), 3 days (1.6%), and more than 3 days (3.3%) with the numbers available (p = 0.7). Similar results were found with the inclusion of all studies (Table 5). In gunshot-induced fractures treated with fixation data from 11 higher-quality studies [1, 6, 7, 16, 19, 20, 24, 29, 38, 39, 42], including 240 fractures (Table 6), no significant difference was found among the various durations of antibiotic administration (1.7% for 1–2 days, 2.7% for 3 days, 6.3% for more than 3 days) (p = 0.45). Similar results were found with the inclusion of all studies (Table 6). Isolated analysis of the optimal duration of a specific antibiotic coverage could not be performed because not enough studies that used the same antibiotic for different time intervals were available.
Table 5.
Infection rates with different durations of antibiotic administration for gunshot-induced fractures treated nonoperatively
| Studies included in analysis | Infection rate (%) (number of infections/number of fractures treated) | p value | ||
|---|---|---|---|---|
| 1–2 days of coverage | 3 days of coverage | > 3 days of coverage | ||
| Higher-quality studies (7 of 23) | 2.1 (2/95) | 1.6 (4/248) | 3.3 (2/61) | 0.70 |
| All studies (10 of 33) | 2.8 (3/108) | 1.6 (4/248) | 3.8 (5/133) | 0.42 |
Table 6.
Infection rates with different durations of antibiotic administration for gunshot-induced fractures treated with fracture fixation
| Studies included in analysis | Infection rate (%) (number of infections/number of fractures treated) | p value | ||
|---|---|---|---|---|
| 1–2 days of coverage | 3 days of coverage | > 3 days of coverage | ||
| Higher-quality studies (11 of 23) | 1.7 (1/60) | 2.7 (4/148) | 6.3 (2/32) | 0.45 |
| All studies (13 of 33) | 1.7 (1/60) | 2.8 (5/180) | 8.6 (3/35) | 0.15 |
For patients treated nonoperatively, with the numbers available, there was no difference in infection rates whether antibiotics were administered intravenously or orally. Overall, seven higher-quality studies [1, 5, 10, 17, 22, 24, 41], including 485 fractures, provided adequate data on this question (Table 7). Studies in which patients were treated with intravenous antibiotics followed by oral administration were not included in this analysis [11, 12]. Similar results were found with the inclusion of all studies (Table 7). Patients treated surgically were given intravenous antibiotics in the studies we found; therefore, this question does not apply to them.
Table 7.
Infections rate with the use of intravenous or oral antibiotics for gunshot-induced fractures treated nonoperatively
| Studies included in analysis | Infection rate (%) (number of infections/number of fractures treated) | p value | |
|---|---|---|---|
| Intravenous antibiotics | Oral antibiotics | ||
| Higher-quality studies (7 of 23) | 1.4 (5/349) | 2.2 (3/136) | 0.69 |
| All studies (10 of 33) | 2.0 (8/392) | 1.6 (3/185) | 1 |
Discussion
Although civilian gunshot trauma that causes extremity fractures is common [8, 37], there are still controversies on the optimal treatment protocol. We therefore performed a systematic literature review to answer the following questions: (1) Are antibiotics needed for the treatment of these fractures? (2) Is gram-negative coverage necessary? (3) How long should antibiotics be administered? And (4) which is the optimal administration route?
There were limitations to our systematic review. Only two prospective randomized studies [10, 22] were identified, each addressing different aspects of the problem. One of them [10] compared antibiotics versus no antibiotics, while the other one compared intravenous versus oral antibiotic administration [22]. To extract as much information from the literature as possible, we included Level IV studies, which had multiple limitations. Some studies had poor documentation or mixed patient populations in regard to our inclusion and exclusion criteria. We aimed to include only low-velocity gunshot injuries; however, information on the type of gun used was not always available, while in many cases the type of gun used could not be identified [3, 13, 26]. Moreover, the weapon’s velocity is not the only factor correlating with the injury inflicted [2, 9, 26]. We also attempted to exclude patients with hand or foot fractures, associated abdominal injuries, and high-velocity injuries. This was not always feasible, and inevitably some of these patients were included. The followup periods were not properly documented in all studies. Deep and superficial infections were not separately investigated, as neither their definitions nor their documentation was always sufficient.
An analysis of the quality of the Level IV studies was performed in an attempt to limit potential bias in some of them [4]. Twenty-three of the initially identified 33 studies met at least ½ of the 14 criteria under consideration in the assessment tool used. Analysis was performed both for all studies and for the higher-quality ones separately. Inclusion of the lower-quality studies did not differentiate the results in any direction, suggesting they were not biased. This is the reason we chose to present the results of both analyses.
The first question addressed in this review was the controversial issue of the need for antibiotic coverage in gunshot-induced fractures of the extremities. This does not apply to patients with fractures treated with fixation who receive antibiotics prophylactically; therefore, no such fractures treated without antibiotics were found in the literature [1, 3, 6, 7, 13, 16, 19, 20, 24–26, 28–30, 38, 39, 41, 42]. In the subgroup of patients treated without surgery, analysis of the higher-quality studies with adequate information on the specific question found no significant difference in the infection rate without antibiotic coverage, with the numbers available. In the only study that directly compared antibiotics versus no antibiotics in gunshot-induced fractures, Dickey et al. [10] prospectively randomized patients to receive local wound care and nonoperative fracture treatment together with either cefazolin for 1 day or no antibiotics. No difference was found, as there was one infection in 36 fractures in the antibiotic group versus one infection in 37 fractures in the nonantibiotics group. However, given the fact that infection after gunshot injuries is an uncommon complication (1.9% of 1156 fractures in the 23 studies included in our review), large numbers of patients would have to be enrolled for a study to show a significant benefit with any intervention in terms of reducing infections in gunshot fractures. Therefore, the above comparisons may have been prone to Type II error. A post hoc power analysis of the results based on the higher-quality studies demonstrated a power of only 41%. Interestingly, inclusion of all studies found a similar increase in infection rate when antibiotics were not used, but with the higher numbers included, this time the difference was significant (Table 2). It therefore appears that the literature is insufficiently strong for a definite conclusion to be drawn on this question; still these data could be used for hypothesis generation for future studies.
The second question addressed was the type of antibiotic coverage, which is also controversial. Hansraj et al. [17] performed a comparative study on the need for gram-negative coverage for these injuries when treated nonoperatively, but no information on randomization was provided. They compared a third-generation cephalosporin (ceftriaxone) to a first-generation cephalosporin (cefazolin), both administered for 2 days, and found no difference in the infection rate. Analysis of six more studies with relevant data [1, 10, 11, 22, 24, 41] showed no significant difference in infection rate with the use of gram-negative coverage (Table 3). Similar results were found for fractures that needed fixation (Table 4).
The duration of coverage was the third study question analyzed. No evidence was found that longer antibiotic coverage is of benefit for gunshot-induced fractures treated either nonoperatively (Table 5) or with fixation (Table 6). This issue is not adequately addressed in the literature. There was only one comparative study regarding duration of antibiotic administration. Geissler et al. [15] compared a single intramuscular dose of 1 g cefonicid administered to 25 consecutive patients with a nonoperatively treated gunshot fracture versus a 2-day intravenous course of unspecified antibiotics in a reportedly comparable group of 25 patients. Excluding hand and foot fractures, there was no infection in 11 extremity fractures treated with the single intramuscular dose and one infection in 13 patients treated with intravenous antibiotics.
The optimal route of antibiotic administration was the fourth question reviewed. Data regarding this issue were available only for fractures treated nonoperatively. The only prospective randomized study by Knapp et al. [22] found no difference in the infection rate between the administration of intravenous cephapirin and gentamicin for 3 days (118 fractures) versus oral ciprofloxacin for 3 days (100 fractures), with two infections in each group. From the seven studies identified with data on this issue, the conclusion was the same (Table 7); gunshot-induced fractures treated nonoperatively can successfully be treated either orally or intravenously.
Most gunshot fractures of the extremities are treated operatively. These patients always receive intravenous antibiotics prophylactically. The findings of this literature review could not find a significant benefit in the inclusion of gram-negative coverage for these injuries or for administering antibiotics for more than 48 hours. For fractures treated nonoperatively, no definite conclusion on the need for antibiotic coverage could be reached. When antibiotics are used for these fractures, adding gram-negative coverage or extending administration beyond 48 hours did not significantly reduce the infection rate, while oral antibiotics were as efficacious as intravenous antibiotics. Despite the extensive experience with these injuries, well-designed, randomized, controlled studies are still needed to address these issues.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
References
- 1.Bartkiw MJ, Sethi A, Coniglione F, Holland D, Hoard D, Colen R, Tyburski JG, Vaidya R. Civilian gunshot wounds of the hip and pelvis. J Orthop Trauma. 2010;24:645–652. doi: 10.1097/BOT.0b013e3181cf03ea. [DOI] [PubMed] [Google Scholar]
- 2.Bartlett CS, Helfet DL, Hausman MR, Strauss E. Ballistics and gunshot wounds: effects on musculoskeletal tissues. J Am Acad Orthop Surg. 2000;8:21–36. doi: 10.5435/00124635-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Bergman M, Tornetta P, Kerina M, Sandhu H, Simon G, Deysine G, Alcindor F. Femur fractures caused by gunshots: treatment by immediate reamed intramedullary nailing. J Trauma. 1993;34:783–785. doi: 10.1097/00005373-199306000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Brand R. Editorial: CORR® criteria for reporting meta-analyses. Clin Orthop Relat Res. 2012;470:3261–3262. doi: 10.1007/s11999-012-2624-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brettler D, Sedlin ED, Mendes DG. Conservative treatment of low velocity gunshot wounds. Clin Orthop Relat Res. 1979;140:26–31. [PubMed] [Google Scholar]
- 6.Brien WW, Kuschner SH, Brien EW, Wiss DA. The management of gunshot wounds to the femur. Orthop Clin North Am. 1995;26:133–138. [PubMed] [Google Scholar]
- 7.Cannada LK, Jones TR, Guerrero-Bejarano M, Viehe T, Levy M, Farrell ED, Ostrum RF. Retrograde intramedullary nailing of femoral diaphyseal fractures caused by low-velocity gunshots. Orthopedics. 2009;32:162. doi: 10.3928/01477447-20090301-05. [DOI] [PubMed] [Google Scholar]
- 8.CDC. Injury Prevention & Control: Data & Statistics (WISQARS™). Available at: http://www.cdc.gov/injury/wisqars/index.html. Accessed August 12, 2012.
- 9.Cooper GJ, Ryan JM. Interaction of penetrating missiles with tissues: some common misapprehensions and implications for wound management. Br J Surg. 1990;77:606–610. doi: 10.1002/bjs.1800770604. [DOI] [PubMed] [Google Scholar]
- 10.Dickey RL, Barnes BC, Kearns RJ, Tullos HS. Efficacy of antibiotics in low-velocity gunshot fractures. J Orthop Trauma. 1989;3:6–10. doi: 10.1097/00005131-198903010-00002. [DOI] [PubMed] [Google Scholar]
- 11.Dickson K, Watson TS, Haddad C, Jenne J, Harris M. Outpatient management of low-velocity gunshot-induced fractures. Orthopedics. 2001;24:951–954. doi: 10.3928/0147-7447-20011001-14. [DOI] [PubMed] [Google Scholar]
- 12.Elstrom JA, Pankovich AM, Egwele R. Extra-articular low-velocity gunshot fractures of the radius and ulna. J Bone Joint Surg Am. 1978;60:335–341. [PubMed] [Google Scholar]
- 13.Ferraro SP, Zinar DM. Management of gunshot fractures of the tibia. Orthop Clin North Am. 1995;26:181–189. [PubMed] [Google Scholar]
- 14.Freeark RJ, Graivier L, Briney W, Ott R. Gunshot fractures. Q Bull Northwest Univ Med Sch. 1961;35:305–310. [PMC free article] [PubMed] [Google Scholar]
- 15.Geissler WB, Teasedall RD, Tomasin JD, Hughes JL. Management of low velocity gunshot-induced fractures. J Orthop Trauma. 1990;4:39–41. doi: 10.1097/00005131-199003000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Hall RF, Pankovich AM. Ender nailing of acute fractures of the humerus: a study of closed fixation by intramedullary nails without reaming. J Bone Joint Surg Am. 1987;69:558–567. [PubMed] [Google Scholar]
- 17.Hansraj KK, Weaver LD, Todd AO, Taylor SM, Griffin MD, Dukhram KM, Judd TP, Hansraj MS. Efficacy of ceftriaxone versus cefazolin in the prophylactic management of extra-articular cortical violation of bone due to low-velocity gunshot wounds. Orthop Clin North Am. 1995;26:9–17. [PubMed] [Google Scholar]
- 18.Hayden J, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144:427–437. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- 19.Hohmann E, Tetsworth K, Radziejowski MJ, Wiesniewski TF. Comparison of delayed and primary wound closure in the treatment of open tibial fractures. Arch Orthop Trauma Surg. 2007;127:131–136. doi: 10.1007/s00402-006-0222-6. [DOI] [PubMed] [Google Scholar]
- 20.Hollmann MW, Horowitz M. Femoral fractures secondary to low velocity missiles: treatment with delayed intramedullary fixation. J Orthop Trauma. 1990;4:64–69. doi: 10.1097/00005131-199003000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Howland WS, Jr, Ritchey SJ. Gunshot fractures in civilian practice: an evaluation of the results of limited surgical treatment. J Bone Joint Surg Am. 1971;53:47–55. [PubMed] [Google Scholar]
- 22.Knapp TP, Patzakis MJ, Lee J, Seipel PR, Abdollahi K, Reisch RB. Comparison of intravenous and oral antibiotic therapy in the treatment of fractures caused by low-velocity gunshots: a prospective, randomized study of infection rates. J Bone Joint Surg Am. 1996;78:1167–1171. doi: 10.2106/00004623-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Leffers D, Chandler RW. Tibial fractures associated with civilian gunshot injuries. J Trauma. 1985;25:1059–1064. [PubMed] [Google Scholar]
- 24.Lenihan MR, Brien WW, Gellman H, Itamura J, Kuschner SH. Fractures of the forearm resulting from low-velocity gunshot wounds. J Orthop Trauma. 1992;6:32–35. [PubMed] [Google Scholar]
- 25.Levy AS, Wetzler MJ, Guttman G, Covall DJ, Fink B, Whitelaw GP, Kozin S. Treating gunshot femoral shaft fractures with immediate reamed intramedullary nailing. Orthop Rev. 1993;22:805–809. [PubMed] [Google Scholar]
- 26.Long WT, Chang W, Brien EW. Grading system for gunshot injuries to the femoral diaphysis in civilians. Clin Orthop Relat Res. 2003;408:92–100. doi: 10.1097/00003086-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 27.McCormick P, McCarthy M, Broadie T, Yaw P, Glover J. Role of antibiotics in the treatment of extremity gunshot wounds. Indiana Med. 1987;80:470–472. [PubMed] [Google Scholar]
- 28.Molinari RW, Yang EC, Strauss E, Einhorn TA. Timing of internal fixation in low-velocity extremity gunshot fractures. Contemp Orthop. 1994;29:335–339. [PubMed] [Google Scholar]
- 29.Nicholas RM, McCoy GF. Immediate intramedullary nailing of femoral shaft fractures due to gunshots. Injury. 1995;26:257–259. doi: 10.1016/0020-1383(95)00012-X. [DOI] [PubMed] [Google Scholar]
- 30.Nowotarski P, Brumback RJ. Immediate interlocking nailing of fractures of the femur caused by low- to mid-velocity gunshots. J Orthop Trauma. 1994;8:134–141. doi: 10.1097/00005131-199404000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Ordog GJ, Wasserberger J, Balasubramanium S, Shoemaker W. Civilian gunshot wounds—outpatient management. J Trauma. 1994;36:106–111. doi: 10.1097/00005373-199401000-00017. [DOI] [PubMed] [Google Scholar]
- 32.Parisien JS. The management of gunshot fractures of the extremities. Bull Hosp Jt Dis Orthop Inst. 1981;41:28–36. [PubMed] [Google Scholar]
- 33.Patzakis MJ, Harvey JP, Ivler D. The role of antibiotics in the management of open fractures. J Bone Joint Surg Am. 1974;56:532–541. [PubMed] [Google Scholar]
- 34.Roth AI, Fry DE, Polk HC. Infectious morbidity in extremity fractures. J Trauma. 1986;26:757–761. doi: 10.1097/00005373-198608000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Ryan JR, Hensel RT, Salciccioli GG, Pedersen HE. Fractures of the femur secondary to low-velocity gunshot wounds. J Trauma. 1981;21:160–162. doi: 10.1097/00005373-198102000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Thoresby FP, Darlow HM. The mechanisms of primary infection of bullet wounds. Br J Surg. 1967;54:359–361. doi: 10.1002/bjs.1800540509. [DOI] [PubMed] [Google Scholar]
- 37.WHO. Chapter 2: Youth violence. Available at: http://www.who.int/violence_injury_prevention/violence/global_campaign/en/chap2.pdf. Accessed August 12, 2012.
- 38.Wisniewski TF, Radziejowski MJ. Gunshot fractures of the humeral shaft treated with external fixation. J Orthop Trauma. 1996;10:273–278. doi: 10.1097/00005131-199605000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Wiss DA, Brien WW, Becker V. Interlocking nailing for the treatment of femoral fractures due to gunshot wounds. J Bone Joint Surg Am. 1991;73:598–606. [PubMed] [Google Scholar]
- 40.Wolf AW, Benson DR, Shoji H, Hoeprich P, Gilmore A. Autosterilization in low-velocity bullets. J Trauma. 1978;18:63. doi: 10.1097/00005373-197801000-00012. [DOI] [PubMed] [Google Scholar]
- 41.Woloszyn JT, Uitvlugt GM, Castle ME. Management of civilian gunshot fractures of the extremities. Clin Orthop Relat Res. 1988;226:247–251. [PubMed] [Google Scholar]
- 42.Wright DG, Levin JS, Esterhai JL, Heppenstall RB. Immediate internal fixation of low-velocity gunshot-related femoral fractures. J Trauma. 1993;35:678–681. doi: 10.1097/00005373-199311000-00004. [DOI] [PubMed] [Google Scholar]


