Abstract
Background
Damage to the hip can occur due to impingement or instability caused by anatomic factors such as femoral and acetabular version, neck-shaft angle, alpha angle, and lateral center-edge angle (CEA). The associations between these anatomic factors and how often they occur in a painful hip are unclear but if unaddressed might explain failed hip preservation surgery.
Questions/purposes
We determined (1) the influence of sex on the expression of impingement-related or instability-related factors, (2) the associations among these factors, and (3) how often both impingement and/or instability factors occur in the same hip.
Methods
We retrospectively reviewed a cohort of 170 hips (145 patients) undergoing MR arthrography of the hip for any reason. We excluded 58 hips with high-grade dysplasia, Perthes’ sequelae, previous surgery, or incomplete radiographic information, leaving 112 hips (96 patients). We measured femoral version and alpha angles on MR arthrograms. Acetabular anteversion, lateral CEA, and neck-shaft angle were measured on pelvic radiographs.
Results
We observed a correlation between sex and alpha angle. Weak or no correlations were observed between the other five parameters. In 66% of hips, two or more (of five) impingement parameters, and in 51% of hips, two or more (of five) instability parameters were found.
Conclusions
Patients with hip pain frequently have several anatomic factors potentially contributing to chondrolabral damage. To address pathologic hip loading due to impingement and/or instability, all of the anatomic influences should be known. As we found no associations between anatomic factors, we recommend an individualized assessment of each painful hip.
Level of Evidence
Level III, prognostic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Hip preservation surgery, and, in particular, less invasive nonosteotomy techniques such as hip arthroscopy are increasingly being used to treat femoroacetabular impingement (FAI). The aims of FAI surgery are to normalize bony morphology to restore impingement-free motion, alleviate symptoms, and prevent or delay the progression of degenerative changes in the hip [16]. Long-term outcome studies are required to determine whether the latter goal is achievable; however, one of the main reasons patients seek treatment is for pain that limits their function. Thus, symptom relief and return to full function are also important and constitute more immediate goals of surgery. A recent systematic review [38] reported mean improvements in pain of between 25% and 100% after surgery for FAI, with 68% to 100% of patients being satisfied with the procedure or reporting improvement in symptoms. Another systematic review [51] reported, in 10 of 12 case series (“fair” or “poor-quality” evidence according to the authors), 75% of patients believed the outcome successful.
The authors of several studies of open and arthroscopic revisions for failed hip preservation surgery have suggested underlying hip dysplasia not addressed during index surgery [26, 44] and insufficiently addressed structural abnormalities such as residual cam impingement [21, 45] are the leading reasons for failure and subsequent revision. In the absence of arthrosis, subtle, unrecognized anatomic factors causing impingement or instability might also represent a major underlying reason for these failures. Some anatomic factors might not necessarily cause impingement or instability but in combination with a mild femoral neck offset deformity or acetabular over- or undercoverage could exacerbate either problem. These predisposing factors include a high or low neck-shaft angle (coxa valga or vara), femoral version, and acetabular version. Furthermore, there is evidence that anatomy predisposing to impingement and anatomy predisposing to instability can coexist in the same hip. About 20% of patients with dysplasia, an instability factor, have acetabular retroversion [15] and more than 70% have decreased head-neck offset [12], both of which are impingement factors [16, 36]. Sex may also influence both the kind and magnitude of pathoanatomy. For example, symptomatic dysplasia and excessive femoral anteversion are more common in females [18, 20, 35, 49, 54]. In several series of patients with FAI, women with symptomatic impingement had smaller cam deformities [17, 20, 24, 37] but could present with worse preoperative scores for pain and function than men [23]. The associations between these various anatomic factors and how often they occur in a painful hip are unclear but if unaddressed at the time of surgery might explain failed hip preservation surgery.
We therefore determined (1) the influence of sex on the expression of impingement-related or instability-related factors, (2) associations among these factors, and (3) how often both impingement and instability factors occur in the same hip in a consecutive series of patients undergoing evaluation for hip pain.
Patients and Methods
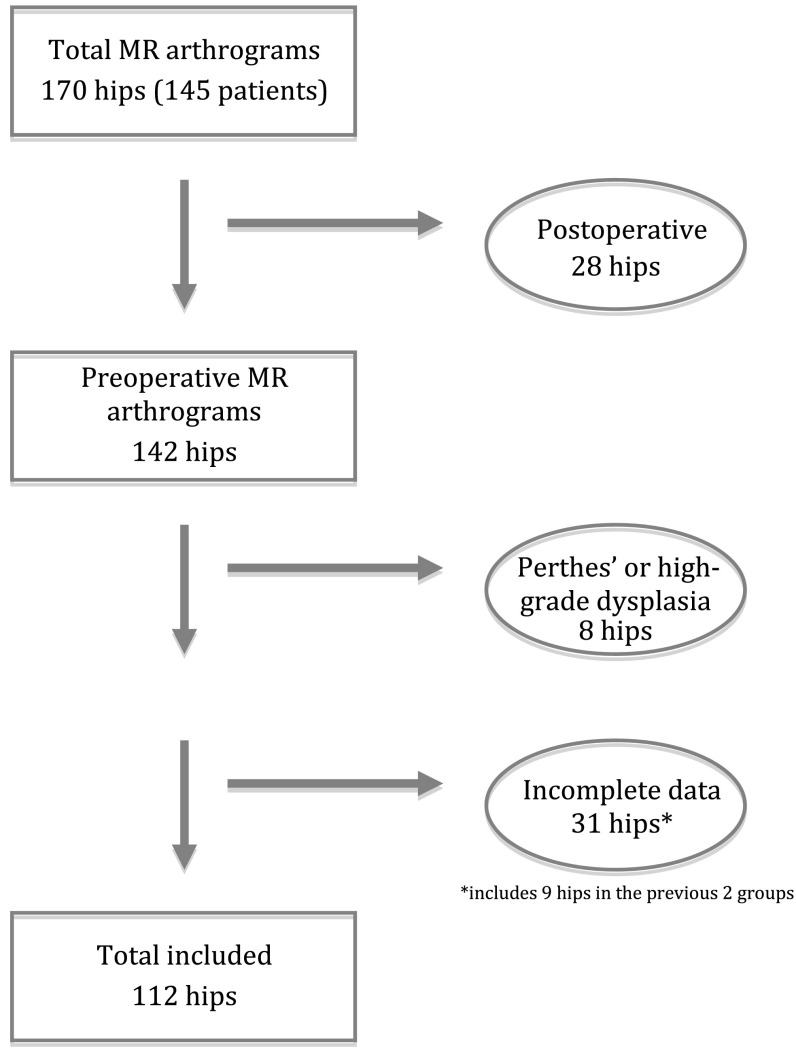
All patients between ages 20 and 40 years who underwent MR arthrography of the hip at the authors’ institution for any reason between May 2010 and April 2011 (a 1-year period) were selected from the institutional billing database for initial inclusion and imaging review. Both hips were included if bilateral MR arthrograms had been obtained for a single patient. The initial series consisted of 170 hips in 145 patients (Fig. 1). MR arthrography was used as an inclusion criterion because at the authors’ institution the standard MR arthrography protocol includes measurement of femoral neck version, which was one of the anatomic parameters of interest. In this consecutive series, the most common indications given for MR arthrography were cam FAI (59 hips), mixed FAI (31 hips), pincer FAI (10 hips), dysplasia or borderline dysplasia (21 hips), and unclear (10 hips). The series included patients whose studies were ordered by primary care sports practitioners, rheumatologists, and orthopaedic surgeons who did not specialize in hip preservation, thus not all patients were known to the authors. Patients were excluded if the MR arthrography was performed for pain after impingement or dysplasia surgery (28 hips) or for evaluation of high-grade dysplasia (defined as patients with subluxation) or Legg-Calvé-Perthes disease (eight hips) or if radiographic information was incomplete (31 hips); nine hips were excluded for combinations of exclusion criteria (eg, MR arthrography for pain after a periacetabular osteotomy for high-grade dysplasia). These exclusions left 112 hips (96 patients) in the final cohort (Fig. 1). There were 47 female hips, 65 male hips, and 16 patients with bilateral MR arthrograms, four of whom were female and 12 of whom were male. The average patient age was 29 years (SD, 6 years).
Fig. 1.
A flow diagram shows the method for inclusion of patients in the final data analysis.
MR arthrography was performed according to the institutional protocols for evaluation of patients with hip pain and suspected FAI or labral pathology. This protocol has been previously described [52]. Briefly, patients undergo a fluoroscopic-guided intraarticular injection of local anesthetic (1 mL 2% lidocaine hydrochloride; Sintetica, Mendrisio, Switzerland), iodinated contrast (1 mL iopamidol [200 mg/mL]; Bracco, Milan, Italy), and dilute MR contrast (8–10 mL gadopentetate dimeglumine at 2 mmol/L; Bayer Healthcare, Berlin, Germany) by an experienced radiologist. The interval between the intraarticular injection and MRI was less than 15 minutes.
MRI was performed with a 1.5-T system (Magnetom® Avanto; Siemens Medical Solutions, Erlangen, Germany), using a body matrix phased-array surface coil placed over the hip and a spine matrix coil integrated in the patient table. Patients were positioned supine on the MR examination table with the knees in full extension and attention to symmetric positioning of the pelvis and lower extremities. The feet were held in position with MR cushions and tape to minimize unintentional movement between series acquisition. Transverse T2-weighted fast spin-echo sequences were obtained over the femoral head and neck and separately over the femoral condyles at the knee for evaluation of femoral version (repetition time, 700 milliseconds; echo time, 42 milliseconds; 12 sections at the femoral head and neck, nine sections at the femoral condyles; section thickness, 5 mm; intersection gap, 0.5 mm; flip angle, 40°; field of view, 22 cm; matrix, 384 × 192; two signals acquired; echo train length, 14; duration of acquisition, 19 seconds at the femoral neck, 15 seconds at the femoral condyles). A three-dimensional (3-D) water excitation true fast imaging with steady-state precession (true FISP) gradient-echo sequence was acquired in a transverse oblique orientation parallel to the femoral neck axis (repetition time, 12.3 milliseconds; echo time, 5.45 milliseconds; section thickness, 1.25 mm; no intersection gap; flip angle, 28°; field of view, 17 cm; matrix, 384 × 384; one signal acquired). The 3-D true FISP data were then reformatted using the long axis of the femoral neck to obtain radial images for the evaluation of the femoral head-neck junction. The routine MR arthrography protocol additionally included a coronal T1-weighted spin-echo sequence, a coronal intermediate-balanced fast spin-echo sequence with fat saturation, and a sagittal water excitation 3-D double-echo steady-state sequence.
The lateral center-edge angle (CEA), neck-shaft angle, and central acetabular version were measured for each patient on supine AP pelvis radiographs; femoral version and alpha angles at the anterosuperior position were measured on the MR arthrogram. AP pelvis radiographs were performed at the authors’ institution, standardized for rotation and flexion, with the legs internally rotated 15°. All measurements were performed on the digital imaging systems available at the authors’ institutions (for radiographs: JiveX, Version 4.4.2.6.PC + build; Visus Technology, Bochum, Germany; for MR arthrograms: ProVision Release 5.0; Cerner, Kansas City, MO, USA). Measurements were performed by a hip preservation fellow (LMT), a senior orthopaedic resident (GL), and a radiology attending (RS), according to previously described and validated parameters [33, 52].
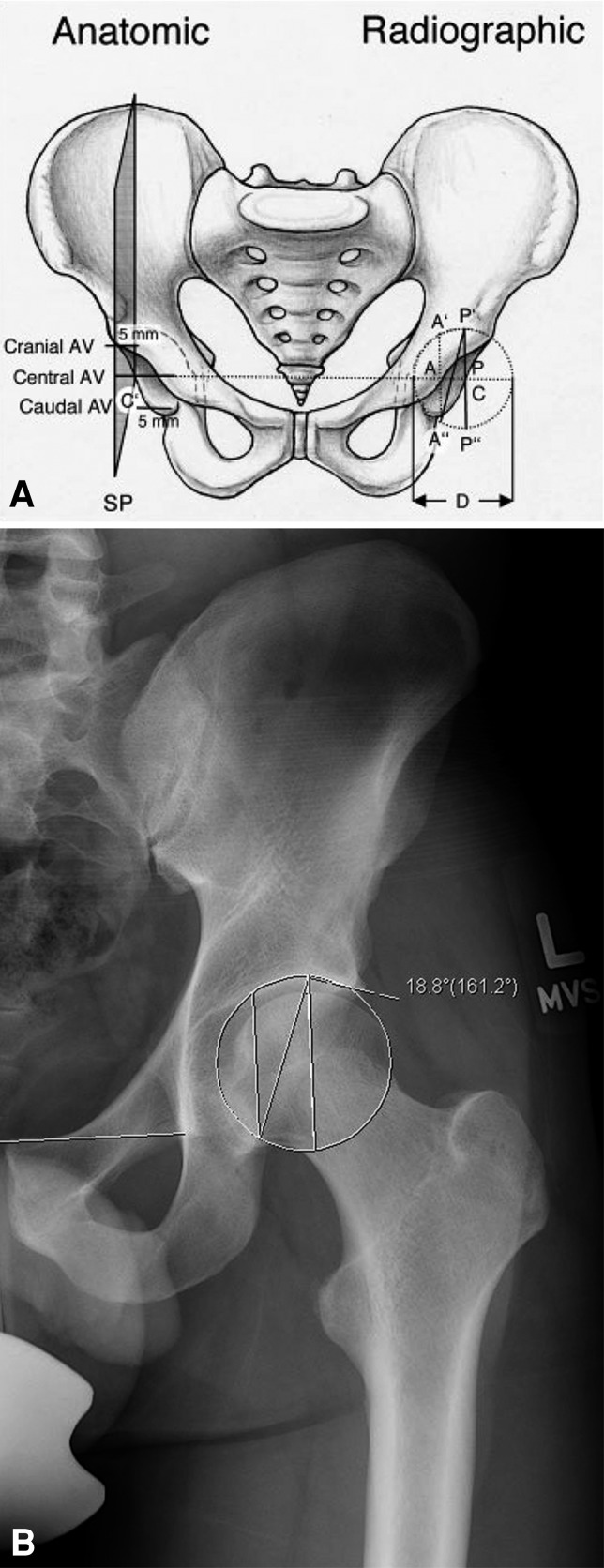
For the lateral CEA and neck-shaft angles, a best-fit (Mose) circle was used to determine the center of the femoral head. To measure the lateral CEA (Fig. 2), a line was drawn through the center of the femoral head perpendicular to the transverse pelvic axis (interteardrop line). Another line was drawn from the center of rotation through the most superolateral point of the acetabular roof. The angle formed by these two lines is the lateral CEA. The interrater reproducibility intraclass correlation coefficient (ICC) for lateral CEA has previously been determined and is 0.73 (95% CI: 0.53–0.85), with a minimal detectable change of 8.3° [34]. The neck-shaft angle is defined by the angle between the axis of the femoral neck and the femoral shaft. The femoral neck axis is defined by a line connecting the center of the femoral head and the midpoint of the femoral neck at the isthmus (Fig. 2). The femoral shaft axis is defined by a line connecting the midpoint of the proximal femoral shaft and the midpoint of the most distal portion of the femur visible on the radiograph. The interrater reproducibility ICC for neck-shaft angle is reportedly 0.95 (95% CI: 0.90–0.97) [33], with a minimal detectable change of 4.8°. Central acetabular version was measured on the AP pelvis radiograph according to the method described by Jamali et al. [25] (Fig. 3). A best-fit circle to the acetabular roof was drawn to determine the center of the acetabulum. Lines perpendicular to the interteardrop line at the center of the acetabulum were drawn at the anterior and posterior walls. The angle A″-P′-P″ was recorded as the central acetabular version. The interrater reliability ICC for measuring central acetabular version according to this method has been reported to range between 0.885 and 0.95 [25].
Fig. 2.
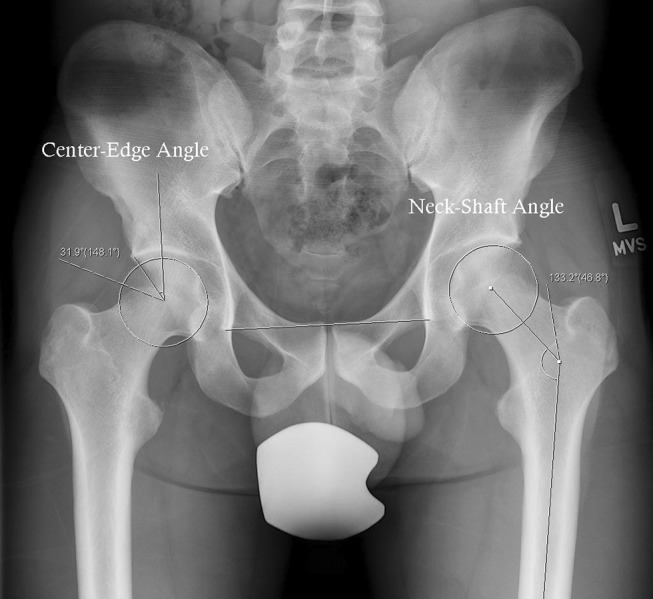
An AP pelvis radiograph demonstrates measurement of lateral CEA on the right hip and neck-shaft angle on the left hip.
Fig. 3A–B.
(A) A line drawing demonstrates measurement of acetabular version from an AP pelvis radiograph. AV = acetabular version; SP = sagittal plane; D = diameter of circle of best fit; Line CC′ = line between acetabular centers of rotation; Line AA′A″ = line drawn perpendicular to Line CC′ at the intersection of the anterior acetabular wall; Line PP′P″ = line drawn perpendicular to Line CC′ at the intersection of the posterior acetabular wall. Acetabular version was recorded as the angle A″-P′-P″. Reprinted with permission by John Wiley & Sons, Inc, from Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign.” J Orthop Res. 2007;25:758–765. (B) Measurement of acetabular version on a representative radiograph is shown.
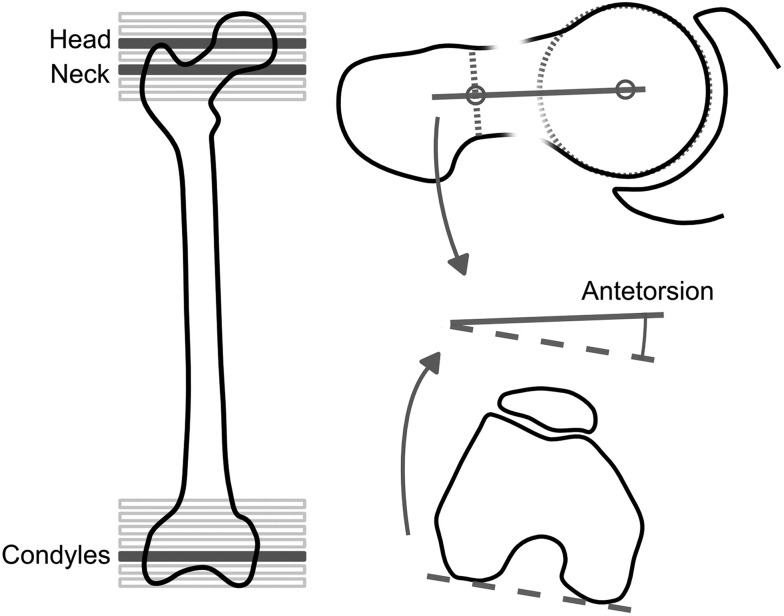
Alpha angles were measured in the anterosuperior position on radial images of the MR arthrogram. The radial slice between 12:00 (directly superior) and 3:00 (directly anterior) with the least amount of head-neck offset was selected for measurement. The alpha angle was measured according to the method described by Nötzli et al. [41] and is the angle between the axis of the femoral neck and a line connecting the center of the femoral head and the point where the contour of the femoral head exits a best-fit circle drawn around the femoral head. Femoral version was measured as has been described previously [52, 53] (Fig. 4). Briefly, the proximal femoral reference line is a line connecting the center of the femoral head and the center of the femoral neck at the narrowest point. In the distal femur, the reference line is the line connecting the posterior border of the femoral condyles. The femoral version is defined as the angle between the two femoral reference lines. The interrater reliability for femoral version using these methods and MR arthrography protocol is high, with an ICC of 0.967 (95% CI: 0.95–0.98) [52]. We considered an alpha angle of greater than 55° as abnormal [41].
Fig. 4.
A line drawing demonstrates measurement of femoral version from the MR arthrogram. Reprinted with permission by the Radiological Society of North America from Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CWA. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology. 2012;263:475–483.
Each radiographic parameter was categorized as normal or abnormal based on previous literature [25, 41, 47, 54, 57] and, if abnormal, whether it was more characteristic of impingement or instability [7].
Unless otherwise stated, all data are presented as the mean and SD. After checking for uniformity and normality of the residuals, the associations between all five radiographic parameters were examined using the Pearson product moment correlation and linear regression for a total of 10 associations. To examine whether acetabular version and femoral version predicted the alpha angle, we used a stepwise multiple regression. Frequency of deformities was presented with crosstabulation. The aforementioned analyses were carried out using SPSS® (Version 17; SPSS Inc, Chicago, IL, USA).
Results
We found associations between sex and femoral and acetabular version (p = 0.008, p = 0.04, respectively), lateral CEA (p = 0.04), and alpha angle (p < 0.001) (Table 1). The only parameter that did not have an association with sex was neck-shaft angle (p = 0.125). The associations between sex and femoral anteversion, acetabular anteversion, and lateral CEA were weak and explained only 7%, 4%, and 4%, respectively, of the variance of these parameters. Sex explained 23% of the variance in alpha angle, with women having smaller alpha angles than men.
Table 1.
Radiographic parameters, with stratification for sex
| Parameter | Overall (n = 112) | Female (n = 47) | Male (n = 65) | p value |
|---|---|---|---|---|
| Lateral center-edge angle | 30° ± 6° | 27° ± 7° | 31° ± 5° | 0.039 |
| Neck-shaft angle | 130° ± 6° | 131° ± 6° | 129° ± 5° | 0.125 |
| Acetabular version | 16° ± 6° | 17° ± 5° | 14° ± 6° | 0.037 |
| Femoral version | 16° ± 10° | 20° ± 8° | 15° ± 10° | 0.008 |
| Alpha angle | 65° ± 12° | 58° ± 8° | 70° ± 12° | 0.000 |
Values are expressed as mean ± SD.
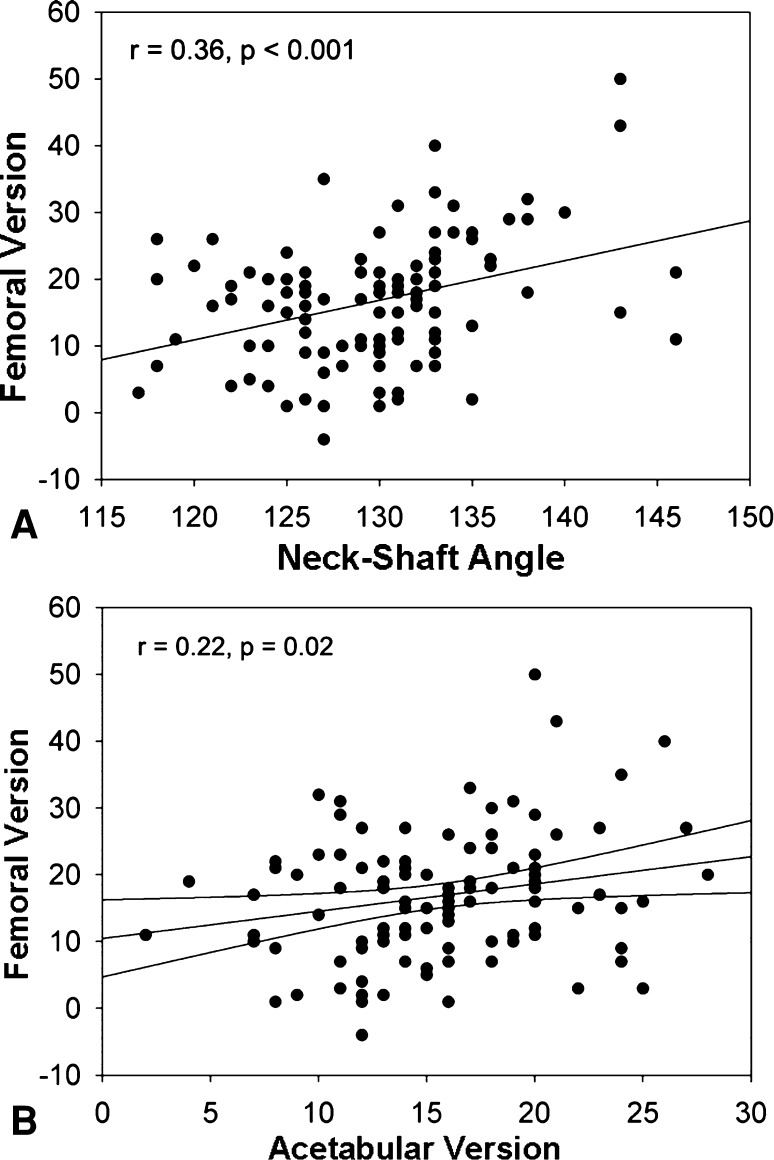
The average lateral CEA was 30° ± 6° (range, 11°–48°) (Table 1). There was no association between lateral CEA and neck-shaft angle, femoral version, or anterosuperior alpha angle (Table 2). The average neck-shaft angle was 130° ± 6° (range 117° to 146°) (Table 1). There was an association between femoral version and neck-shaft angle (Fig. 5A). Neck-shaft angle was a predictor of femoral version and explained 13% of the variance. The average femoral version was 16° ± 10° (range, −4° to 50°) (Table 1). There was an association between femoral version and acetabular version (Fig. 5B). Femoral version was a weak predictor of acetabular version and explained 5% of the variance. There was no association between femoral version and anterosuperior alpha angle (Table 2). The average central acetabular version was 16° ± 6° (range, −9° to 29°) (Table 1). There was a correlation between acetabular version and anterosuperior alpha angle (Table 2). Multiple regression showed acetabular version but not femoral version was a predictor of alpha angle (p = 0.02) but only explained 5% (4% adjusted) of the variance. The average anterosuperior alpha angle in the series was 65° ± 12° (range, 37° − 106°) (Table 1).
Table 2.
Associations between the measured radiographic parameters
| Parameter | Statistic | Lateral center-edge angle | Neck-shaft angle | Acetabular version | Femoral version | Alpha angle |
|---|---|---|---|---|---|---|
| Lateral center-edge angle | Pearson correlation | 1 | −0.108 | −0.126 | −0.011 | 0.094 |
| p value (2-tailed) | 0.255 | 0.188 | 0.908 | 0.326 | ||
| Neck-shaft angle | Pearson correlation | −0.108 | 1 | 0.168 | 0.359 | −0.190 |
| p value (2-tailed) | 0.255 | 0.077 | < 0.001 | 0.045 | ||
| Acetabular version | Pearson correlation | −0.126 | 0.168 | 1 | 0.224 | −0.191 |
| p value (2-tailed) | 0.188 | 0.077 | 0.020 | 0.045 | ||
| Femoral version | Pearson correlation | −0.011 | 0.359 | 0.224 | 1 | −0.156 |
| p value (2-tailed) | 0.908 | < 0.001 | 0.020 | 0.107 | ||
| Alpha angle | Pearson correlation | 0.094 | −0.190 | −0.191 | −0.156 | 1 |
| p value (2-tailed) | 0.326 | 0.045 | 0.045 | 0.107 |
Fig. 5A–B.
(A) A scatterplot shows the association between femoral version and neck-shaft angle (r = 0.36, p < 0.001). Neck-shaft angle is a predictor of femoral version and explains 13% of the variance. (B) A scatterplot shows the weak association between femoral version and acetabular version (r = 0.22, p = 0.02). Femoral version explains 5% of the variance of acetabular version.
The majority of hips (79%) had a normal lateral CEA [57] and normal neck-shaft angle [54]. A similar percentage (80%) had an abnormal alpha angle (Table 3). No patient had entirely normal hip anatomy (no instability or impingement factors) (Table 4). When the radiographic parameters were categorized as impingement-associated, normal, or instability-associated, 49% of hips had one or more impingement factors but no instability factors (Table 4); overall 62% of hips in this cohort had at least one or two impingement factors. In contrast, only 9% of hips had instability factors but no impingement factors.
Table 3.
Distribution of impingement, normal, and instability anatomy
| Parameter | Number of hips | ||
|---|---|---|---|
| Impingement | Normal | Instability | |
| Lateral center-edge angle (n = 112) | > 35° | 20°–35° | < 20° |
| 19 (17%) | 88 (78%) | 5 (5%) | |
| Neck-shaft angle (n = 112) | < 125° | 125°–140° | > 140° |
| 18 (16%) | 89 (79%) | 5 (5%) | |
| Acetabular version (n = 112) | < 15° | 15°–20° | > 20° |
| 51 (46%) | 45 (40%) | 16 (14%) | |
| Femoral version (n = 108) | < 15° | 15°–20° | > 20° |
| 43 (40%) | 30 (28%) | 35 (32%) | |
| Alpha angle (n = 112) | > 55° | < 55° | |
| 90 (80%) | 22 (20%) | ||
Table 4.
Distribution of impingement and/or instability factors
| Impingement factors | Number of hips | ||||||
|---|---|---|---|---|---|---|---|
| Instability factors | |||||||
| 0 | 1 | 2 | 3 | 4 | 5 | Total | |
| 0 | 0 | 3 | 3 | 2 | 2 | 0 | 10 (8.9%) |
| 1 | 13 | 10 | 6 | 0 | 0 | 0 | 29 (25.9%) |
| 2 | 13 | 21 | 6 | 0 | 0 | 0 | 40 (35.7%) |
| 3 | 18 | 4 | 0 | 0 | 0 | 0 | 22 (19.7%) |
| 4 | 10 | 0 | 0 | 0 | 0 | 0 | 10 (8.9%) |
| 5 | 1 | 0 | 0 | 0 | 0 | 0 | 1 (0.9%) |
| Total | 55 (49.1%) | 38 (33.9%) | 15 (13.4%) | 2 (1.8%) | 2 (1.8%) | 0 (0%) | 112 (100%) |
Discussion
Reports of revision hip preservation surgery provide clinical evidence that if the anatomic factors causing abnormal forces on the hip are not addressed, joint damage and symptoms are likely to progress [21, 26, 44, 45]. Similarly, correcting only impingement or instability in a patient who has subtle combinations of both types of anatomy may be a cause of continued symptoms or poor outcomes [22, 30, 34, 36]. However, even though instability and FAI are common causes of hip pain, not all patients with radiographic evidence of impingement or instability become symptomatic [6, 11, 19]. Thus, identifying anatomic factors that compensate for or exacerbate FAI or instability is important when treating young patients with hip pain. Femoral and acetabular retroversion are known to exacerbate or contribute to impingement [16, 25, 28, 43, 48], while femoral and acetabular anteversion may exacerbate mild underlying instability due to dysplasia [7]. Although the effect of the native neck-shaft angle on the hip has only been suggested [7, 8], variations in neck-shaft angle affect the lever arm of the abductors [4] and change the spatial relationship between the head and the neck. Recognizing that patients can have combinations of both impingement and instability has implications for treatment. For example, patients undergoing a periacetabular osteotomy for dysplasia may also need a femoral neck osteoplasty to restore normal ROM after surgery, particularly if acetabular coverage has been increased by the osteotomy [36]. If associations exist between sex and hip anatomy, as well as between certain types of pathoanatomy, this could help the surgeon recognize what anatomy will need correction. To further investigate this, we determined whether certain combinations of anatomic factors occur in patients with hip pain. In particular, we determined the influence of sex on the expression of impingement-related or instability-related factors, the associations between these factors, and how often both impingement and instability factors are present in the same hip.
There are limitations to this study. First, this is a population of young people with hip and groin pain seen at a specialty orthopaedic hospital. Thus, our findings may not be applicable to an asymptomatic population or to the general population of patients presenting with hip pain. Nonetheless, because multiple anatomic factors that potentially cause or exacerbate hip pain were observed in our population, it is likely important to look for these factors when planning treatment. Secondly, although the indications for the MR arthrograms were known, we do not have additional clinical data for these patients. Specifically, we make inferences about the native hip based on the radiographic parameters but do not know the associated ROM or treatment outcomes. The third limitation of the study is that acetabular version and femoral neck-shaft angle were both measured on supine AP pelvis radiographs, which may introduce bias into the study. Supine acetabular version may not be the same as functional version in stance because of the tilt of the pelvis. As such, the true forces around the hip may be different from what is inferred from the supine measurement. Standing AP pelvis radiographs would provide a more functional measurement of acetabular version; however, supine radiographs are the current standard of care [10]. The apparent neck-shaft angle measured on a radiograph is also related to the amount of internal rotation and femoral version [27, 32], which could also introduce bias or inaccuracy of the measurement. All of the AP pelvis radiographs in this series were performed with the femur in 15° of internal rotation, however. This reportedly produces accurate values for neck-shaft angle, regardless of femoral anteversion [27].
Of the associations we observed, the strongest was that between sex and alpha angle, with sex explaining 23% of the variation in alpha angle. Many studies have investigated the associations between sex and hip anatomy (Table 5) [5, 9, 17, 29, 37, 46, 52] and between the femoral and acetabular parameters measured in this study (Table 6) [1–3, 9, 14, 24, 31, 39, 46, 50, 52, 54]. Our findings agree with most of this literature but do conflict with two studies [2, 54] that found no association between femoral and acetabular version (Table 6). Although there may be some associations between anatomic parameters, for example the stereotypical coxa valga anteverted hip, the weakness of the observed effect means, in the absence of any strong developmental factor, the associations for an individual are unpredictable.
Table 5.
Previously published associations between sex and hip anatomy
| Study | Study population | Modality | Association between sex and | ||||
|---|---|---|---|---|---|---|---|
| Alpha angle | Femoral version | Acetabular version | Lateral CEA | Neck-shaft angle | |||
| Atkinson et al. [5] | Australian patients undergoing hip resurfacing | CT scan | None Avg F: 9° Avg M: 8° p = 0.387 |
Sex difference Avg F: 23° Avg M: 18° p = 0.02 |
None Avg F: 128° Avg M: 129° p = 0.85 |
||
| Buller et al. [9] | Asymptomatic US patients (29–75 years old) | CT scans originally obtained for vascular angiography | Positive correlation for F sex: 2.6° to 1° p = 0.018 |
Positive correlation for F sex: 2.79° to 1° p = 0.018 |
|||
| Gerhardt et al. [17] | Asymptomatic US professional soccer players | Pelvic radiographs | Avg F: 52.9° Avg M: 65.6° |
||||
| Laborie et al. [29] | General population of 17- to 20-year-olds in Norway | Pelvic radiographs | 10% of F with one or more cam-type findings, 35% of M with one or more cam-type findings p < 0.001 | ||||
| Nakahara et al. [37] | Asymptomatic elderly Japanese | CT scan | F had smaller alpha angles 7% of F and 25% of M with alpha angle > 55° | Sex difference Avg F: 25.2° Avg M: 20.3° p = 0.021 |
Sex difference Avg F: 21.3° Avg M: 17.5° p = 0.023 |
Sex difference Avg F: 34.7° Avg M: 37.9° p = 0.043 |
None Avg F: 125.5° Avg M: 124.3° p = 0.347 |
| Reikeras et al. [46] | Cadaveric study in Norway | Direct bone measurement and radiographs | No difference between M and F | ||||
| Sutter et al. [52] | Swiss patients with FAI compared to asymptomatic volunteers | MRI | Avg F: 16° Avg M: 10° p < 0.001 |
||||
| Current study | Swiss patients undergoing hip MR arthrography for any reason | MR arthrography and pelvic radiographs | Stronger association; explains 23% of variance Avg F: 58° Avg M: 70° p < 0.001 |
Weak association; explains 7% of variance Avg F: 20° Avg M: 15° p = 0.008 |
Weak association; explains 4% of variance Avg F: 17° Avg M: 14° p = 0.038 |
Weak association; explains 4% of variance Avg F: 27° Avg M: 31° p = 0.039 |
None Avg F: 131° Avg M: 129° p = 0.125 |
CEA = center-edge angle; FAI = femoroacetabular impingement; avg = average; F = female; M = male.
Table 6.
Previously published associations between radiographic parameters
| Study | Study population | Modality | Association between lateral CEA and | Association between | |||||
|---|---|---|---|---|---|---|---|---|---|
| Femoral version | Acetabular version | Alpha angle | Neck-shaft angle | Neck-shaft angle and femoral version | Femoral and acetabular version | Femoral version, acetabular version, and alpha angle | |||
| Akiyama et al. [1] | Japanese females with dysplasia compared with controls | CT scan and pelvic radiographs | Higher version in DDH (avg 22°) compared to controls (14°) p < 0.001 | Higher anteversion in DDH (avg 24°) compared with controls (avg 21°) p = 0.006 | Correlation in anterior and global deficiency subgroups of hips with DDH No correlation in controls | ||||
| Anda et al. [2] | Norwegian patients with symptomatic dysplasia | CT scan | Increased version in DDH compared to controls, but no correlation | None | None | ||||
| Argenson et al. [3] | French patients with DDH and arthrosis compared to controls | CT scan and pelvic radiographs | Increased anteversion for DDH compared to controls | 46.5% incidence of coxa valga in hips with DDH | None | ||||
| Buller et al. [9] | Asymptomatic US patients (29–75 years old) | CT scans originally obtained for vascular angiography | None | None | Positive correlation: 0.38° to 1° p < 0.05 | ||||
| Ellis et al. [14] | Cadaveric femora | CT scan | No difference in femoral version between cam morphology femurs (9°) and normal femurs (9°) p = 0.816 | ||||||
| Ito et al. [24] | Swiss patients with hip pain compared to controls | MRI | Decreased anteversion for patients with hip pain/impingement (10°) compared to controls (16°) | ||||||
| Leunig et al. [31] | Swiss patients with OA secondary to protrusio compared to patients with OA but no protrusio | Pelvic radiographs | Lower neck-shaft angle (121°) in protrusio group (CEA = 60°) compared to controls (CEA = 36°, neck-shaft angle 130°’) | ||||||
| Noble et al. [39] | Japanese women with DDH compared to controls | CT scan | Higher avg anteversion in DDH (42°) compared to controls (36°) p = 0.007 | No difference in neck-shaft angle between DDH and controls (avg 124° for both) p = 0.897 | |||||
| Reikeras et al. [46] | Cadaveric study in Norway | Direct bone measurement and radiographs | Weak correlation between version and neck-shaft angle | ||||||
| Steppacher et al. [50] | Swiss patients with DDH compared to patients with a deep acetabulum | MR arthrography | Hips with DDH (CEA < 25°) had more oval femoral heads Overcovered hips (CEA > 39°) had rounder femoral heads Avg alpha angle < 41° in all positions for both groups | Avg DDH: 137° Avg overcovered: 129° p < 0.001 | |||||
| Sutter et al. [52] | Swiss patients with FAI compared to asymptomatic volunteers | MRI | Femoral version similar for both cohorts (avg 12° for both) and not different for cam FAI (11°) compared to normal (13°) | ||||||
| Tönnis and Heinecke [54] | German patients with hip pain | CT scan and pelvic radiograph | No association between femoral version and DDH | No association between acetabular version and DDH | Significant numbers of patients with all combinations of femoral and acetabular version, some with compensatory relationships No correlation coefficient given |
||||
| Current study | Swiss patients undergoing hip MR arthrography for any reason | MR arthrography and pelvic radiographs | None | None | None | None | Association between neck-shaft angle and version; explains 13% of variance of version | Weak association; femoral version explains 5% of variance in acetabular version | Acetabular version is a weak predictor of alpha angle; explains 5% of variance |
CEA = center-edge angle; DDH = developmental dysplasia of the hip; OA = osteoarthritis; FAI = femoroacetabular impingement; avg = average.
The number of patients with abnormal osseous anatomy in this study is similar to three other recent surgical cohorts of patients with labral tears [13, 40, 56]. The majority of patients in this study underwent MR arthrography for a potential diagnosis of FAI. As we observed in this series, FAI is particularly common in patients with hip or groin pain, with the prevalence of impingement in similar series ranging from 87% to 94% [42, 55]. As might be expected, the majority of our patients had abnormal alpha angles, and all patients had at least one instability or impingement factor. Nearly ½ (49%) had one or more impingement factors but no instability factors, whereas few patients had instability factors but no impingement factors.
Given the weak effects of the association between sex and most of the anatomic parameters, as well as among the anatomic parameters, the effect of these associations for an individual is unpredictable. We recommend ascertaining alpha angle, femoral and acetabular version, acetabular coverage, and neck-shaft angle when determining an individual’s treatment plan. Because patients with hip pain often have a combination of pathologic bony abnormalities that may contribute to chondrolabral damage, all of the anatomic influences should be assessed to completely address the causes of hip pain and symptomatic impingement or instability.
Acknowledgments
We thank Professor Reinhold Ganz, University of Bern, Bern, Switzerland, for his contributions to the study design and helpful insights about our results.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery, Schulthess Clinic and Department of Radiology, Orthopaedic University Hospital Balgrist, Zürich, Switzerland.
References
- 1.Akiyama M, Nakashima Y, Fujii M, Sato T, Yamamoto T, Mawatari T, Motomura G, Matsuda S, Iwamoto Y. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol. 2012;41:1411–1418. doi: 10.1007/s00256-012-1368-7. [DOI] [PubMed] [Google Scholar]
- 2.Anda S, Terjesen T, Kvistad KA, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comp Assist Tomogr. 1991;15:115–120. doi: 10.1097/00004728-199101000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Argenson JN, Ryembault E, Flecher X, Brassart N, Parratte S, Aubaniac JM. Three-dimensional anatomy of the hip in osteoarthritis after developmental dysplasia. J Bone Joint Surg Br. 2005;87:1192–1196. doi: 10.1302/0301-620X.87B9.15928. [DOI] [PubMed] [Google Scholar]
- 4.Arnold AS, Komatta AV, Delp SL. Internal rotation gait: a compensatory mechanism to restore abduction capacity decreased by bone deformity? Dev Med Child Neurol. 1997;39:40–44. doi: 10.1111/j.1469-8749.1997.tb08202.x. [DOI] [PubMed] [Google Scholar]
- 5.Atkinson HD, Johal KS, Willis-Owen C, Zadow S, Oakeshott RD. Differences in hip morphology between the sexes in patients undergoing hip resurfacing. J Orthop Surg Res. 2010;5:76. doi: 10.1186/1749-799X-5-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91:162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 7.Bedi A, Dolan M, Leunig M, Kelly BT. Static and dynamic mechanical causes of hip pain. Arthroscopy. 2011;27:235–251. doi: 10.1016/j.arthro.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 8.Birnbaum K, Pandorf T. Finite element model of the proximal femur under consideration of the hip centralizing forces of the iliotibial tract. Clin Biomech(Bristol, Avon). 2011;26:58–64. [DOI] [PubMed]
- 9.Buller LT, Rosneck J, Monaco FM, Butler R, Smith T, Barsoum WK. Relationship between proximal femoral and acetabular alignment in normal hip joints using 3-dimensional computed tomography. Am J Sports Med. 2012;40:367–375. doi: 10.1177/0363546511424390. [DOI] [PubMed] [Google Scholar]
- 10.Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clohisy JC, Dobson MA, Robison JF, Warth LC, Zheng J, Liu SS, Yehyawi TM, Callaghan JJ. Radiographic structural abnormalities associated with premature, natural hip-joint failure. J Bone Joint Surg Am. 2011;93(suppl 2):3–9. doi: 10.2106/JBJS.J.01734. [DOI] [PubMed] [Google Scholar]
- 12.Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467:128–134. doi: 10.1007/s11999-008-0481-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dolan MM, Heyworth BE, Bedi A, Duke G, Kelly BT. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res. 2011;469:831–838. doi: 10.1007/s11999-010-1539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellis AR, Noble PC, Schroder SJ, Thompson MT, Stocks GW. The cam impinging femur has multiple morphologic abnormalities. J Arthroplasty. 2011;26(suppl 1):59–65. doi: 10.1016/j.arth.2011.04.028. [DOI] [PubMed] [Google Scholar]
- 15.Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895–903. doi: 10.2106/JBJS.I.00046. [DOI] [PubMed] [Google Scholar]
- 16.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 17.Gerhardt MB, Romero AA, Silvers HJ, Harris DJ, Watanabe D, Mandelbaum B. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40:584–588. doi: 10.1177/0363546511432711. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 19.Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93:580–586. doi: 10.2106/JBJS.J.00875. [DOI] [PubMed] [Google Scholar]
- 20.Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy. 2013;29:54–63. doi: 10.1016/j.arthro.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 22.Hussell JG, Rodriguez JA, Ganz R. Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:81–92. [PubMed] [Google Scholar]
- 23.Impellizzeri FM, Mannion AF, Naal FD, Hersche O, Leunig M. The early outcome of surgical treatment for femoroacetabular impingement: success depends on how you measure it. Osteoarthritis Cartilage. 2012;20:638–645. doi: 10.1016/j.joca.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 24.Ito K, Minka MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 25.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 26.Kain MSH, Novais EN, Vallim C, Millis MB, Kim YJ. Periacetabular osteotomy after failed hip arthroscopy for labral tears in patients with acetabular dysplasia. J Bone Joint Surg Am. 2011;93(suppl 2):57–61. doi: 10.2106/JBJS.J.01770. [DOI] [PubMed] [Google Scholar]
- 27.Kay RM, Jaki KA, Skaggs DL. The effect of femoral rotation on the projected femoral neck-shaft angle. J Pediatr Orthop. 2000;20:736–739. doi: 10.1097/01241398-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Kelly BT, Bedi A, Robertson CM, Dela Torre K, Giveans MR, Larson CM. Alterations in internal rotation and alpha angles are associated with arthroscopic cam decompression in the hip. Am J Sports Med. 2012;40:1107–1112. doi: 10.1177/0363546512437731. [DOI] [PubMed] [Google Scholar]
- 29.Laborie LB, Lehmann TG, Engesæter IØ, Eastwood DM, Engesæter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 30.Leunig M, Ganz R. [Bernese periacetabular osteotomy] [in German] Orthopäde. 1998;27:743–750. doi: 10.1007/pl00003460. [DOI] [PubMed] [Google Scholar]
- 31.Leunig M, Nho SJ, Turchetto L, Ganz R. Protrusio acetabuli: new insights and experience with joint preservation. Clin Orthop Relat Res. 2009;467:2241–2250. doi: 10.1007/s11999-009-0853-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu RW, Toogood P, Hart DE, Davy DT, Cooperman DR. The effect of varus and valgus osteotomies on femoral version. J Pediatr Orthop. 2009;29:666–675. doi: 10.1097/BPO.0b013e3181b769b5. [DOI] [PubMed] [Google Scholar]
- 33.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 35.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810–824. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 36.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 37.Nakahara I, Takao M, Sakai T, Nishii T, Yoshikawa H, Sugano N. Gender differences in 3D morphology and bony impingement of human hips. J Orthop Res. 2011;29:333–339. doi: 10.1002/jor.21265. [DOI] [PubMed] [Google Scholar]
- 38.Ng VY, Arora N, Best TM, Pan X, Ellis TJ. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med. 2010;38:2337–2345. doi: 10.1177/0363546510365530. [DOI] [PubMed] [Google Scholar]
- 39.Noble PC, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. The three-dimensional shape of the dysplastic femur. Implications for THR. Clin Orthop Relat Res. 2003;417:27–40. [PubMed] [Google Scholar]
- 40.Nogier A, Bonin N, May O, Gedouin JE, Bellaiche L, Boyer T, Lequesne M; French Arthroscopy Society. Descriptive epidemiology of mechanical hip pathology in adults under 50 years of age. Prospective series of 292 cases: clinical and radiological aspects and physiopathological review. Orthop Trauma Surg Res. 2010;96(8 suppl):S53–S58. [DOI] [PubMed]
- 41.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 42.Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res. 2010;468:2710–2714. doi: 10.1007/s11999-010-1233-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paliobeis CP, Villar RN. The prevalence of dysplasia in femoroacetabular impingement. Hip Int. 2011;21:141–145. doi: 10.5301/HIP.2011.7422. [DOI] [PubMed] [Google Scholar]
- 44.Parvizi J, Bican O, Bender B, Mortazavi SMJ, Purtill JJ, Erickson J, Peters C. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24(suppl 1):110–113. doi: 10.1016/j.arth.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 45.Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 46.Reikeras O, Høiseth A, Reigstad A, Fönstelien E. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand. 1982;53:775–779. doi: 10.3109/17453678208992291. [DOI] [PubMed] [Google Scholar]
- 47.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 48.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 49.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 50.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stevens MS, LeGay DA, Glazebrook MA, Amirault D. The evidence for hip arthroscopy: Grading the current indications. Arthroscopy. 2010;26:1370–1383. doi: 10.1016/j.arthro.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 52.Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology. 2012;263:475–483. doi: 10.1148/radiol.12111903. [DOI] [PubMed] [Google Scholar]
- 53.Tomczak RJ, Guenther KP, Rieber A, Mergo P, Ros PR, Brambs HJ. MR imaging measurement of the femoral antetorsional angle as a new technique: comparison with CT in children and adults. AJR Am J Roentgenol. 1997;168:791–794. doi: 10.2214/ajr.168.3.9057536. [DOI] [PubMed] [Google Scholar]
- 54.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 55.Weir A, de Vos RJ, Moen M, Hölmich P, Tol JL. Prevalence of radiological signs of femoroacetabular impingement in patients presenting with long-standing adductor-related groin pain. Br J Sports Med. 2011;45:6–9. doi: 10.1136/bjsm.2009.060434. [DOI] [PubMed] [Google Scholar]
- 56.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 57.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chirurg Scand. 1939;83(suppl 58):7–38. [Google Scholar]