Abstract
Background
Arthroscopic approaches for the diagnosis and treatment of hip disorders are well established; however, there are limited data regarding revision hip arthroscopy. There have been several studies evaluating the findings of MR arthrography with primary hip arthroscopy, but to our knowledge, no study has evaluated the diagnostic value of MR arthrography before revision hip arthroscopy.
Questions/purposes
We obtained sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of MR arthrography to detect labral lesions, chondral lesions and loose bodies before revision hip arthroscopy.
Methods
We performed a single-surgeon, retrospective review of 70 revision hip arthroscopies (62 patients) and assessed the association between MR arthrography findings and intraoperative findings. There were 43 females and 19 males with a mean age of 36 years (range, 17–59 years). Radiographic interpretation was performed by one of four fellowship-trained musculoskeletal radiologists at three institutions, who had at least 5 years of experience. Radiographic findings were compared with surgical findings by one of the authors for calculation of sensitivity, specificity, PPV, and NPV.
Results
The sensitivity, specificity, PPV, and NPV of MR arthrography for detecting labral tears were 82%, 70%, 94%, and 39%, respectively. The sensitivity, specificity, PPV, and NPV of MR arthrography for detecting chondral damage were 65%, 90%, 94%, and 50%, respectively. The sensitivity, specificity, PPV, and NPV of MR arthrography for detecting loose bodies were 33%, 100%, 100%, and 88%, respectively.
Conclusions
Our study showed the utility of MR arthrography to assist in the diagnosis and treatment of patients with ongoing or recurrent symptoms who have had prior hip arthroscopy. Our data show that MR arthrography is superior at ruling in, rather than ruling out, labral lesions, chondral lesions, and loose bodies, as there were studies interpreted as normal which in fact showed disorders.
Level of Evidence
Level III, diagnostic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Arthroscopic surgery of the hip has gained popularity during the past decade for various hip disorders, including labral tears, chondral damage, femoroacetabular impingement (FAI), synovial chondromatosis, loose bodies, foreign body removal, and crystalline hip arthropathy [20, 30]. Although many patients do well with these procedures [1, 4, 19, 22, 23, 26], a certain cohort of patients never fully experience relief after surgery or they have recurrent symptoms of hip disorders. Multiple factors can contribute to a failed procedure, including untreated bony abnormality, soft tissue laxity, poor patient selection, inadequate surgical procedure, or a new injury [2, 29]. Further, the presence of advanced degenerative arthritis has been associated with inferior outcomes when compared with the presence of isolated labral tears and/or only mild chondral disorder [9, 18, 28].
Numerous studies associating the findings of MR arthrography with primary hip arthroscopy have shown sensitivity of 71% to 100% [3, 7, 8, 10, 27, 31] and specificity of 44% to 100% [10, 14, 21]. Byrd and Jones [5] reported improved sensitivity of MR arthrography compared with MRI using arthroscopic hip findings as the gold standard. The use of MR arthrography improved the rate of false-negative results from 42% with MRI to 8% with MR arthrography. Some studies have been performed to evaluate the utility of MR arthrography compared with surgical findings at revision knee arthroscopy (evaluating menisci and chondral damage/repair) [6, 11, 15, 17] and revision shoulder arthroscopy [16, 24] (evaluating rotator cuff and labral disorders), but to our knowledge, no study has evaluated the diagnostic value of MR arthrography before revision hip arthroscopy.
The purpose of our study was to evaluate the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of MR arthrography in detecting (1) labral lesions, (2) chondral lesions, and (3) loose bodies in patients with continued or recurrent symptoms scheduled for revision hip arthroscopy.
Patients and Methods
Institutional review board approval was obtained before the start of the study. We performed a single-surgeon, retrospective review of revision hip arthroscopies performed between August 1993 and August 2009 to determine the association between MR arthrography and intraoperative findings. All patients who underwent a revision hip arthroscopy and had a complete medical record, including MR arthrography with radiologist report, operative notes, and operative photographs, were included. In the 62 patients (70 hips), there were 43 females and 19 males, with an average age of 34 years (range, 17–59 years) (Table 1). This represented 89.7% (70 of 78) of the revision hip arthroscopy procedures performed during the period in question, with the balance of the patients not meeting inclusion criteria because repeat MR arthrography was not performed (n = 7) or records were missing (n = 1). For 11 hips in 11 patients (16%), the index procedure was not performed by the senior author. There were 28 arthroscopies of the left hip and 42 of the right hip. All patients had preoperative groin pain. Fifty-seven of 70 hips (81%) had mechanical symptoms of locking or catching. All patients had nonoperative management that failed, including rest, NSAIDs, activity modification, physical therapy, and intraarticular steroid injections (33 of 70 hips).
Table 1.
Select data collected via chart review
| Variable | Value |
|---|---|
| Sex (number of female/male patients) | 43/19 |
| Age (years)* | 36 (17–59) |
| Side (number on left/right hips) | 28/42 |
| Preoperative groin pain (%) | 100 |
| Preoperative mechanical symptoms (%) | 81 |
| Number of patients with labral tears | |
| By MR arthrography | 49 |
| At surgery | 60 |
| Number of patients with chondral injuries | |
| By MR arthrography | 32 |
| At surgery | 49 |
* Values are expressed as mean, with range in parentheses.
The radiographic interpretations were compared with the surgical findings, as hip arthroscopy is considered the gold standard for diagnosis. The imaging studies were performed and interpreted by one of four fellowship-trained musculoskeletal radiologists at three institutions, who had at least 5 years of experience. All readings were performed preoperatively, without the radiologist knowing a specific diagnosis for the patients. The reports were evaluated for the presence or absence of labral tears, cartilage injury, loose bodies, and location of the disorder.
The imaging protocol involved injecting a 15-mL mixture of 0.9% normal saline, Marcaine™ 0.5% with epinephrine (Hospira, Inc, Lake Forest, IL, USA), Isovue®-300 (Bracco Diagnostics Inc, Monroe Township, NJ, USA), and ProHance® (Bracco Diagnostics Inc) into the joint space, followed by imaging with a 1.5-Te GE MR scanner (GE Healthcare, Milwaukee, WI, USA), using the following sequences: coronal T1, coronal T1 with fat suppression, coronal T2 with fat suppression, coronal short tau inversion recovery (STIR), sagittal oblique T1 with fat suppression, axial proton density with fat suppression, and axial oblique T1 with fat suppression.
The hip arthroscopies were performed with the patient in the lateral position under general anesthesia. The patients were placed in the hip positioner and Innomed® hip distractor (Innomed, Inc, Savannah, GA, USA). Satisfactory distraction was confirmed with fluoroscopy. After preparing and draping, two 6-inch (15-cm) spinal needles were introduced through the lateral portal, directly into the joint. This was followed by creating two skin incisions and introducing our arthroscope and outflow cannula. A pressure-sensitive inflow pump was used during the course of the case. Intraarticular evaluation was performed using 30° and 70° arthroscopic cameras. The labral tears were identified based on location and the cartilage injuries based on location and Outerbridge grade. The operative reports, operative images, and MR arthrography images with reports were evaluated by a fellowship-trained hip surgeon (PJG) not directly involved in the care of the patients.
We obtained sensitivity, specificity, PPV, and NPV of MR arthrography in the detection (presence or absence) of labral lesions, chondral lesions, and loose bodies for revision hip arthroscopy.
Results
The comparison of MR arthrography and intraoperative findings showed good accuracy in detecting labral disorders, with a sensitivity of 82%, specificity of 70%, PPV of 94%, and NPV of 39% (Table 2). There were 11 patients whose MR arthrography images were read as a normal labrum but were found to have a labral tear intraoperatively. Six of these tears were anteromedial, four were anterior, and one had diffuse fraying located anterior, posterior, and lateral (Table 3). An axial oblique T1 MR arthrography image depicts an anteromedial labral tear, confirmed at the time of arthroscopy (Fig. 1).
Table 2.
Comparison of MR arthrography with intraoperative findings at revision hip arthroscopy
| Parameter | Labral tear | Chondral injury | Loose bodies |
|---|---|---|---|
| Sensitivity | 49/60 (82%) | 32/49 (65%) | 4/12 (33%) |
| Specificity | 7/10 (70%) | 17/19 (90%) | 58/58 (100%) |
| PPV | 49/52 (94%) | 32/34 (94%) | 4/4 (100%) |
| NPV | 7/18 (39%) | 17/34 (50%) | 58/66 (88%) |
PPV = positive predictive value; NPV = negative predictive value.
Table 3.
Comparison of location of labral tear location*
| Labral tear location | MR arthrography | Scope |
|---|---|---|
| Anteromedial | 1 | 33 |
| Anterior | 29 | 25 |
| Anterosuperior | 11 | 2 |
| Superior | 5 | 1 |
| Posterosuperior | 2 | 0 |
| Posterior | 0 | 1 |
| Not specified | 5 | 0 |
| Total | 53 | 62 |
* All tears, not just hips, ie, some hips with multiple tears.
Fig. 1A–B.
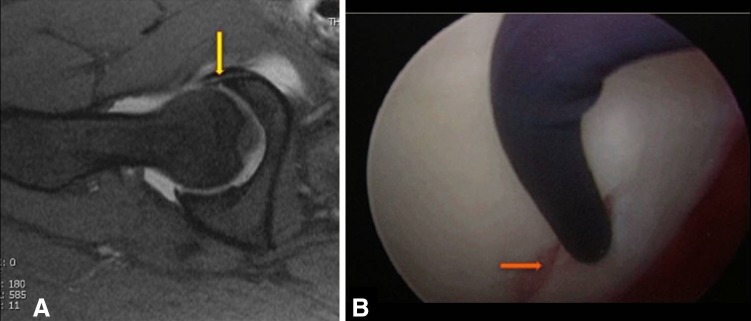
(A) An axial oblique T1-weighted MR arthrography image shows an anteromedial labral tear (arrow), (B) confirmed at the time of arthroscopy (arrow).
For detecting chondral disorders, MR arthrography revealed similar sensitivity but better specificity than with detecting labral disorders: sensitivity of 65%, specificity of 90%, PPV of 94%, and NPV of 50% (Table 2). Seventeen patients had their MR arthrography images read as showing normal articular cartilage. These patients in fact had chondral damage in at least one location at the time of arthroscopy. Overall, 32 of 49 hips with at least one chondral injury were identified by MR arthrography. However, when looking at all injuries (ie, in patients with a chondral injury in more than one location), MR arthrography appears to be more accurate for detection of chondral damage of the femoral head (20 of 21) (Table 4) than for detection of acetabular chondral damage (36 of 65) (Table 5). A coronal STIR MR arthrography image shows a superior femoral head cartilage lesion, correlating with intraoperative findings of a chondral flap lesion of the superior femoral head (Fig. 2). Further, MR arthrography appears to be superior at detecting Grades III and IV acetabular chondral injuries as compared with Grades I and II injuries (18 of 22 [82%] versus 15 of 31 [48%], respectively). Two patients had positive findings on MR arthrography but neither chondral injuries nor labral tears were identified at the time of surgery.
Table 4.
Comparison of location of femoral head chondral damage*
| Location | MR arthrography | Scope |
|---|---|---|
| Anteromedial | 2 | 3 |
| Anterior | 6 | 8 |
| Anterosuperior | 2 | 0 |
| Superior | 4 | 4 |
| Posterosuperior | 0 | 0 |
| Posterior | 2 | 6 |
| Not specified | 4 | 0 |
| Total | 20 | 21 |
* All chondral injuries, not just hips, ie, some hips with multiple chondral injuries. Seven MR arthrography images read as having isolated femoral head defect, ie, no acetabular defect; no hip scopes with isolated femoral head involvement.
Table 5.
Comparison of location of acetabular chondral damage*
| Location | MR arthrography | Scope |
|---|---|---|
| Anteromedial | 2 | 8 |
| Anterior | 11 | 33 |
| Anterosuperior | 7 | 10 |
| Superior | 10 | 5 |
| Posterosuperior | 0 | 2 |
| Posterior | 3 | 5 |
| Not specified | 3 | 2 |
| Total | 36 | 65 |
* All chondral injuries, not just hips, ie, some hips with multiple chondral injuries.
Fig. 2A–B.
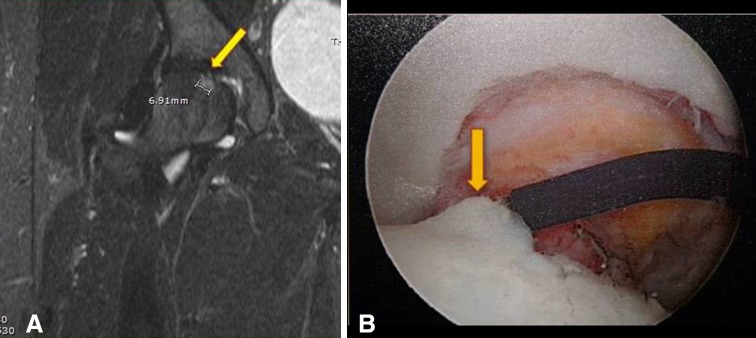
(A) A coronal STIR MR arthrography image shows a superior femoral head cartilage lesion (arrow) with underlying bone marrow edema (cursor), (B) correlating with intraoperative findings of a chondral flap lesion of the superior femoral head (arrow) with Grades II to III wear.
MR arthrography is better at ruling in loose bodies, with a specificity and PPV of 100%, while sensitivity is only 33% (Table 2). The NPV is 88%; however, the reason the NPV is good is that the prevalence of loose bodies was low (12/70 cases), as compared with the prevalence of labral tears or chondral injuries. With such a low incidence, the high NPV is misleading and does not indicate that MR arthrography is a good test for ruling out loose bodies. Of the four loose bodies detected on MR arthrography, two were in the anterior acetabulum and two were in the fovea. At the time of hip arthroscopy, two of the loose bodies were identified in the anterior acetabulum and 10 were in the fovea. The two anterior loose bodies were identified correctly, but only two of 10 foveal loose bodies were identified correctly by MR arthrography.
Discussion
Although arthroscopic hip procedures have become more common, and so revision arthroscopy is becoming an increasingly important procedure, there are limited data regarding diagnostic tools that can help guide the decision to perform revision hip arthroscopy. There have been several studies evaluating the findings of MR arthrography with primary hip arthroscopy [3, 7, 8, 10, 27, 31], but to our knowledge, no study has evaluated the diagnostic value of MR arthrography before revision hip arthroscopy. We therefore obtained sensitivity, specificity, PPV, and NPV of MR arthrography to detect labral lesions, chondral lesions, and loose bodies for revision hip arthroscopy.
Our study has some limitations. First, we recognize that the retrospective design is not as powerful as a prospective analysis. This prevented us from assessing interrater and intrarater reliabilities of the four radiologists; however, although we recognize some variability might exist in each radiologist’s interpretation of the presence or absence of labral disruption, chondral injury, or loose bodies, we believe they are representative of what would be reasonably expected in clinical practice. In addition, all MR arthrography images were reviewed by one of four fellowship-trained musculoskeletal radiologists at a major referral center for hip arthroscopy, therefore they were experienced in performing and interpreting these images to evaluate for labral tears and chondral injuries. Second, we did not include a control group, as all patients who received MR arthrography had persistent pain and underwent a revision hip arthroscopy. Third, we acknowledge the limitations associated with using MR arthrography to distinguish new lesions from old postoperative lesions; however, all patients presented with persistent pain and mechanical symptoms. Fourth, as not all the MR arthrography imaging reports contained detailed descriptions of the findings, we were able to base our comparisons only on the presence or absence of a tear, chondral injury or loose body; so it is possible that the MR arthrography findings were not concordant with the findings at arthroscopy. This information, along with the findings on MR arthrography, was used to make the decision to treat with revision arthroscopy.
Our results support the use of MR arthrography before revision hip arthroscopy, given its relatively high sensitivity and specificity in detecting labral disorders. Previous studies showed the sensitivity of MR arthrography to range between 71% to 100% [3, 7, 8, 10, 27, 31] for primary hip arthroscopy, with our study showing 82% sensitivity in detecting labral disorders before revision arthroscopy. In addition, specificity of MR arthrography ranging from 44% to 100% has been reported [10, 14, 21] for primary hip arthroscopy, as compared with 70% in our study for revision arthroscopy. NPV has consistently been low, only 13% in a study by Keeney et al. [13] and 39 % in our study. A potential reason for the low NPV in our study was likely attributable to the patient population of the study; ie, patients with a prolonged course of pain and prior hip surgery have a higher likelihood of having intraarticular disorders than the general population, making a true-negative MR arthrography result less likely. In our patient sample, a labrum tear was observed for 86% of hips at revision arthroscopy. Similarly, our PPV for labral tears of 94% is consistent with prior studies that had PPVs ranging from 93% to 100% [3, 13]. Given the high prevalence of labral lesions in repeat arthroscopy in our study and in the study by Heyworth et al. [12], a high PPV would be expected. The use of MR arthrography to detect labral lesions may be affected by location of the labral lesion. Although the majority of tears were located anteriorly (97%), we found that 53% of these tears were more specifically located anteromedial, a location that is difficult to assess with MR arthrography and difficult to access arthroscopically. We believe that the discrepancy regarding the anteromedial lesions is that currently MR arthrography cannot adequately distinguish a postsurgical change from a new injury (specifically as intraoperatively many of the labral tears at revision arthroscopy were adjacent to the tear location seen anteriorly at primary surgery).
For chondral lesions, MR arthrography is better at ruling in than in detecting disorders. Keeney et al. [13] reported sensitivity, specificity, PPV, and NPV of 47%, 89%, 84%, and 59%, respectively, when evaluating the utility of MR arthrography for detecting chondral damage before primary hip arthroscopy. Schmid et al. [25] also evaluated the diagnostic effectiveness of MR arthrography to detect chondral disorders and found some variability between two interpreting radiologists, with specificities of 79% and 50%, sensitivities of 77% and 84%, PPVs of 73% and 71%, and NPVs of 83% and 68%. These studies are consistent with our MR arthrography data, which showed sensitivity, specificity, PPV, and NPV of 65%, 90%, 94%, and 50%, respectively, for chondral damage. Keeney et al. [13] also described the difficulty of MR arthrography in detecting Grades I and II lesions, in which 22.8% of these injuries were not identified. In our study, the detection of these early lesions was even more difficult, with 52% of Grades I and II lesions missed on MR arthrography. The large variability in detecting Grades I and II lesions between our study and that of Keeney et al. is most likely the result of variability in the size and depth of detected lesions, different imaging sequences used, and/or different radiologists interpreting the reports.
For loose bodies, MR arthrography exhibited 100% specificity, but poor sensitivity. We know of no previous study which has examined the diagnostic accuracy of MR arthrography in detecting loose bodies in the hip. Every loose body identified as being present on preoperative imaging was confirmed through arthroscopy; however, eight loose bodies observed during arthroscopy were unidentified on MR arthrography.
We found MR arthrography to be useful in assisting in the diagnosis and treatment of ongoing or recurrent symptoms in patients who have had hip arthroscopy. Our data show that MR arthrography is superior at ruling in, rather than ruling out, labral lesions, cartilage lesions, and loose bodies before revision hip arthroscopy. Detecting chondral lesions, specifically early (Grade I) lesions proved to be most difficult using MR arthrography. Future studies could include the use of delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), which measures the biochemical integrity of cartilage by detecting changes in glycosaminoglycans.
Acknowledgments
We thank Jo Ann Lee MS for assistance with data collection and organization and Maureen Dwyer PhD ATC for assistance with manuscript preparation.
Footnotes
One of the authors certifies that he (JCM) has received or may receive payments or benefits, during the study period, an amount less than USD 10,000 from Innomed Inc (Savannah, GA, USA), and an amount less than USD 10,000 from Arthrex (Naples, FL, USA). One of the authors certifies that he (PJG) has received or may receive payments or benefits, during the study period, an amount less than USD 10,000 from Zimmer (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Newton-Wellesley Hospital, Newton, MA, USA.
References
- 1.Beaule PE, O’Neill M, Rakhra K. Acetabular labral tears. J Bone Joint Surg Am. 2009;91:701–710. doi: 10.2106/JBJS.H.00802. [DOI] [PubMed] [Google Scholar]
- 2.Bogunovic L, Gottlieb M, Pashos G, Baca G, Clohisy JC. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res. 2013;471:2523–2529. doi: 10.1007/s11999-013-3015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burnett SJ, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457. doi: 10.2106/JBJS.D.02806. [DOI] [PubMed] [Google Scholar]
- 4.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 5.Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668–1674. doi: 10.1177/0363546504266480. [DOI] [PubMed] [Google Scholar]
- 6.Cardello P, Gigli C, Ricci A, Chiatti L, Voglino N, Pofi E. Retears of postoperative knee meniscus: findings on magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) by using low and high field magnets. Skeletal Radiol. 2009;38:149–156. doi: 10.1007/s00256-008-0600-y. [DOI] [PubMed] [Google Scholar]
- 7.Chan YS, Lien LC, Hsu HL, Wan YL, Lee MS, Hsu KY, Shih CH. Evaluating hip labral tears using magnetic resonance arthrography: a prospective study comparing hip arthroscopy and magnetic resonance arthrography diagnosis. Arthroscopy. 2005;21:1250. doi: 10.1016/j.arthro.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Czerny C, Hofmann S, Neuhold A, Tschauner C, Engel A, Recht MP, Kramer J. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology. 1996;200:225–230. doi: 10.1148/radiology.200.1.8657916. [DOI] [PubMed] [Google Scholar]
- 9.Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for degenerative joint disease. Arthroscopy. 1998;14:435. [Google Scholar]
- 10.Freedman BA, Potter BK, Dinauer PA, Giuliani JR, Kuklo TR, Murphy KP. Prognostic value of magnetic resonance arthrography for Czerny stage II and III acetabular labral tears. Arthroscopy. 2006;22:742–747. doi: 10.1016/j.arthro.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Gobbi A, Kon E, Berruto M, Francisco R, Filardo G, Marcacci M. Patellofemoral full-thickness chondral defects treated with Hyalograft-C: a clinical, arthroscopic, and histologic review. Am J Sports Med. 2006;34:1763–1773. doi: 10.1177/0363546506288853. [DOI] [PubMed] [Google Scholar]
- 12.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Keeney JA, Peelle MW, Jackson J, Rubin D, Maloney WJ, Clohisy JC. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;429:163–169. doi: 10.1097/01.blo.0000150125.34906.7d. [DOI] [PubMed] [Google Scholar]
- 14.Leunig M, Werlen S, Ungersbock A, Ito K, Ganz R. Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br. 1997;79:230–234. doi: 10.1302/0301-620X.79B2.7288. [DOI] [PubMed] [Google Scholar]
- 15.Magee T, Shapiro M, Rodriguez J, Williams D. MR arthrography of postoperative knee: for which patients is it useful? Radiology. 2003;229:159–163. doi: 10.1148/radiol.2291020988. [DOI] [PubMed] [Google Scholar]
- 16.Magee TH, Gaenslen ES, Seitz R, Hinson GA, Wetzel LH. MR imaging of the shoulder after surgery. AJR Am J Roentgenol. 1997;168:925–928. doi: 10.2214/ajr.168.4.9124141. [DOI] [PubMed] [Google Scholar]
- 17.Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M. Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med. 2005;33:1499–1504. doi: 10.1177/0363546505274717. [DOI] [PubMed] [Google Scholar]
- 18.Margheritini F, Villar RN. The efficacy of arthroscopy in the treatment of hip osteoarthritis. Chir Organi Mov. 1999;84:257–261. [PubMed] [Google Scholar]
- 19.McCarthy JC, Barsoum W, Puri L, Lee JA, Murphy S, Cooke P. The role of hip arthroscopy in the elite athlete. Clin Orthop Relat Res. 2003;406:71–74. doi: 10.1097/00003086-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy JC, Lee JA. Arthroscopic intervention in early hip disease. Clin Orthop Relat Res. 2004;429:157–162. doi: 10.1097/01.blo.0000150118.42360.1d. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell B, McCrory P, Brukner P, O’Donnell J, Colson E, Howells R. Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sports Med. 2003;13:152–156. doi: 10.1097/00042752-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 22.O’leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy. 2001;17:181–188. doi: 10.1053/jars.2001.21481. [DOI] [PubMed] [Google Scholar]
- 23.Potter BK, Freedman BA, Andersen RC, Bojescul JA, Kuklo TR, Murphy KP. Correlation of Short Form-36 and disability status with outcomes of arthroscopic acetabular labral debridement. Am J Sports Med. 2005;33:864–870. doi: 10.1177/0363546504270567. [DOI] [PubMed] [Google Scholar]
- 24.Probyn LJ, White LM, Salonen DC, Tomlinson G, Boynton EL. Recurrent symptoms after shoulder instability repair: direct MR arthrographic assessment—correlation with second-look surgical evaluation. Radiology. 2007;245:814–823. doi: 10.1148/radiol.2453061329. [DOI] [PubMed] [Google Scholar]
- 25.Schmid MR, Notzli HP, Zanetti M, Wyss TF, Hodler J. Cartilage lesions in the hip: diagnostic effectiveness of MR arthrography. Radiology. 2003;226:382–386. doi: 10.1148/radiol.2262020019. [DOI] [PubMed] [Google Scholar]
- 26.Shindle MK, Voos JE, Nho SJ, Heyworth BE, Kelly BT. Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am. 2008;90(suppl 4):2–19. doi: 10.2106/JBJS.H.00686. [DOI] [PubMed] [Google Scholar]
- 27.Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186:449–453. doi: 10.2214/AJR.04.1809. [DOI] [PubMed] [Google Scholar]
- 28.Walton NP, Jahromi I, Lewis PL. Chondral degeneration and therapeutic hip arthroscopy. Int Orthop. 2004;28:354–356. doi: 10.1007/s00264-004-0585-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ward JP, Rogers P, Youm T. Failed hip arthroscopy: causes and treatment options. Orthopedics. 2012;35:612–617. doi: 10.3928/01477447-20120621-11. [DOI] [PubMed] [Google Scholar]
- 30.Yusaf MA, Hame SL. Arthroscopy of the hip. Curr Sports Med Rep. 2008;7:269–274. doi: 10.1249/JSR.0b013e318186d4c5. [DOI] [PubMed] [Google Scholar]
- 31.Ziegert AJ, Blankenbaker DG, De Smet AA, Keene JS, Shinki K, Fine JP. Comparison of standard hip MR arthrographic imaging planes and sequences for detection of arthroscopically proven labral tear. AJR Am J Roentgenol. 2009;192:1397–1400. doi: 10.2214/AJR.08.1609. [DOI] [PubMed] [Google Scholar]


