Abstract
Background
Surgical hip dislocation allows for a 360° view of the acetabulum and may facilitate a reduction in selected acetabular fractures. To our knowledge there is no description in the literature of the different techniques used to reduce acetabular fractures through this approach. The aims of this study are to describe a technique of hip surgical dislocation to treat a variety of acetabular fracture patterns and to ascertain the early results with this technique, including the quality of fracture reductions achieved, clinical results, operative time, and complications such as avascular necrosis and heterotopic ossification.
Description of Technique
The procedure involves digastric trochanteric flip osteotomy and safe dislocation of the femoral head, preserving its vessels. T-type, transverse fractures alone or associated with posterior wall could be reduced with specific clamps and reduction adequacy can be judged by direct view. Anterior column fixation could be performed with one or two screws; the posterior column could be fixed with a single posterior plate or with two plates if a transverse fracture is associated with a posterior wall fracture.
Methods
Between 2005 and 2011, we used this approach selectively to manage those types of fractures; during the period in question, we treated 312 acetabular fractures surgically, of which 31 (10%) were treated using this approach. Patient demographic, injury, and surgical variables as well as complications were recorded. Outcomes were evaluated with the Merle d’Aubigné and Postel system. Radiographic outcome was scored according to Matta’s criteria on postoperative radiographs (AP and Judet views). Minimum followup was 24 months (mean, 43 months; range, 24–87 months).
Results
Fracture reduction was defined as anatomic in 65% cases, imperfect in 16%, and poor in 19%. Mean Merle d’Aubigné score was 15 points (out of 18, with higher scores being better). Two patients developed symptomatic femoral head avascular necrosis.
Conclusions
In complex cases, surgical dislocation presents several advantages; a single approach may reduce surgical time, permit direct intraarticular assessment, and facilitate screw placement closer to the articular surface. It also presents several limitations; some difficulties with bone-reduction clamp positioning, limited fixation of the anterior column, and a small risk of greater trochanter malunion.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-013-3228-8) contains supplementary material, which is available to authorized users.
Introduction
Open reduction and internal fixation remains the treatment of choice for most displaced acetabular fractures, and long-term results are largely related to the quality of the reduction of the fracture, particularly at the level of the weightbearing articular surface [15, 16, 22, 27, 28]. Even a small (1-mm) articular incongruence has been reported to lead to deterioration of the fractured articulation in a short time [26].
The goal of the treatment of a displaced acetabular fracture is to achieve anatomical reduction. The majority of fractures can be treated through a single standard exposure, but each approach allows only a partial view of the acetabulum. For example, through a standard approach like Kocher-Langenbeck, intraarticular control of the fracture reduction is poor, even if capsulotomy is performed to better visualize the dome [39]; furthermore, direct intraarticular reduction control is nearly absent with the ilioinguinal and the Smith-Petersen approach [22].
For complex fractures, extensile modifications or combined approaches are proposed to make reduction easier [21, 22], but the use of combined or extensile approaches has been criticized because they are associated in some reports with a high rate of complications, including infection, heterotopic ossification, and muscle weakness [1, 7, 12–14, 18–20, 37, 43, 44, 46].
The surgical dislocation technique popularized by Ganz et al. [8] for the treatment of femoroacetabular impingement (FAI) allows a 360° view of the acetabulum and may be helpful to achieve an anatomic reduction of the anterior and posterior column while avoiding combined or extensile approaches. This technique is based on the anatomical description of the course of the ascending branch of the medial circumflex artery and allows for complete visualization of the inner acetabulum with a low risk of avascular necrosis of the femoral head [10]. In 2002, Siebenrock et al. [38] reported the first 12 cases of surgical hip dislocation, concluding that this approach allows better assessment of the reduction in cases of transverse fractures alone and transverse fractures associated with posterior wall fractures. However, to our knowledge, there is no description in the literature of the different reduction techniques for different types of fractures.
The aims of this study are to describe a technique of hip surgical dislocation to treat a variety of acetabular fracture patterns and to ascertain the early results with this technique, including the quality of fracture reductions achieved, clinical results, operative time, and complications such as avascular necrosis and heterotopic ossification.
Surgical Technique
The surgical approach has been previously described by Siebenrock et al. [39]. In this article, we offer an abbreviated description of the approach, a description of reduction techniques, and a surgical video (Video 1). Either Gibson or the Kocher-Langenbeck approach could be used: in this case series, the Kocher-Langenbeck approach was used because it allows more space for the positioning of posterior clamps; however, the developers of this technique prefer the Gibson approach because it preserves the gluteus maximus muscle.
Trochanteric flip osteotomy is executed to obtain a fragment containing the insertion of the gluteus medius, vastus lateralis, and long tendon of the gluteus minimus muscles. To ensure that the major part of the piriformis tendon remains on the stable part of the greater trochanter, a small part of the most posterior portion of the gluteus medius tendon should be initially kept attached to the trochanter and sharply cut after osteotomy. Only then is the superior border of the piriformis tendon dissected near the trochanteric insertion and the interval between the gluteus minimus and the piriformis muscles is isolated. This interval is safe regarding the risk of damage to the deep branch of the medial circumflex artery. The osteotomized trochanteric fragment is then flipped and slid anteriorly after releasing the origin of the gluteus minimus; débridement of the gluteus minimus could be performed at this stage if necessary (gluteus minimus injuries are very common in acetabular fractures). An anterosuperior capsulotomy (Z-shaped) is performed when the capsule is intact or completed if there is a partial capsular rupture. The femoral head is dislocated anteriorly through adduction and external rotation of the leg. With manipulations of the leg, the acetabulum is visualized and the surfaces of the fragments are cleaned of debris. After relocation of the femoral head, destroyed muscle tissue is débrided and the external fracture lines are visualized. Thereafter, it must be decided whether fracture manipulation and fixation can be executed without myotenotomy of the external rotators. If the tendons have to be cut, this should be done at a minimal distance of 2 cm from the posterior trochanteric crest. The obturator externus tendon should be preserved in all events so as not to damage the deep branch of the medial femoral circumflex artery. The posterior wall and column are now exposed and posterior lines of the fracture could be easily visualized. Next, a direct reduction maneuver is performed based on the fracture type. For a transverse fracture/transverse plus posterior wall fracture, fracture reduction can be achieved with several techniques; the easiest method is obtained using two 3.5-mm Jungbluth clamps (Matta Pelvic System–Stryker Trauma AG, Selzach, Switzerland) with the first one placed in the anterior column and the second in the posterior column (Fig. 1). In juxtatectal and transtectal transverse fractures, the anterior column clamp could be easily placed above the anterior rim of the fracture, whereas infratectal fractures do not allow for easy placement of the anterior clamp; therefore, a posterior Jungbluth clamp and a 3-mm Schanz screw (Matta Pelvic System–Stryker Trauma AG), drilled into the anterior column, could be used.
Fig. 1.

Placement of the two Jungbluth clamps for transverse fracture reduction is shown on the sawbone model.
The second posterior clamp could be placed between the area of bone above the roof and the posterior border of the greater sciatic notch or the angle thereof (depending on the site of deattachment). If a Gibson approach is used, the posterior clamp (Fig. 2) is often placed closer to the posterior wall to avoid excessive tension of the fascia. Reduction of a transverse fracture with two Jungbluth clamps is commonly obtained by pushing the inferior part of the pelvic brim outward and downward (Video 2). Occasionally, a supplementary Schanz screw in the ischial tuberosity could be useful to increase the derotation of the fragment. Interfragmentary compression of the transtectal fractures was sometimes achieved with a Matta clamp inserted in the greater sciatic notch. After reduction, fixation is achieved with one or two 3.5-mm cortical screws inserted along the axis of the anterior column. The entry point is situated at least 3 to 4 cm above the roof of the acetabulum along the anterior pillar of the iliac wing. The area of a possible point of entry is a circle approximately 2 cm in diameter; a guide could be used to avoid muscle injuries. The direction of the screw could be checked by touching the medial aspect of the iliopectineal eminence from behind the posterior column and by direct vision of the articular surface. In obese patients or those with big muscles, correct screw direction could be hard to find: the drill tends to go medially and anteriorly; therefore, the fracture could sometimes only be fixed with a few millimeters of screw engagement medial to the fracture line. Then, the head is relocated, and posterior plating for the posterior column is performed with the commonly used technique described by Letournel and Judet [22]. If necessary, the posterior wall is reduced before the posterior column fixation, as commonly performed during the Kocher-Langenbeck approach. In those cases, a second more lateral plate for fixation of the posterior wall could be used to fix the fragment after the posterior column fixation. The femoral head is dislocated again to check the reduction (sometimes, although the extraarticular surface looks reduced, imperfect reduction of the articular surface is found) and to be sure that no intraarticular screws are placed.
Fig. 2.
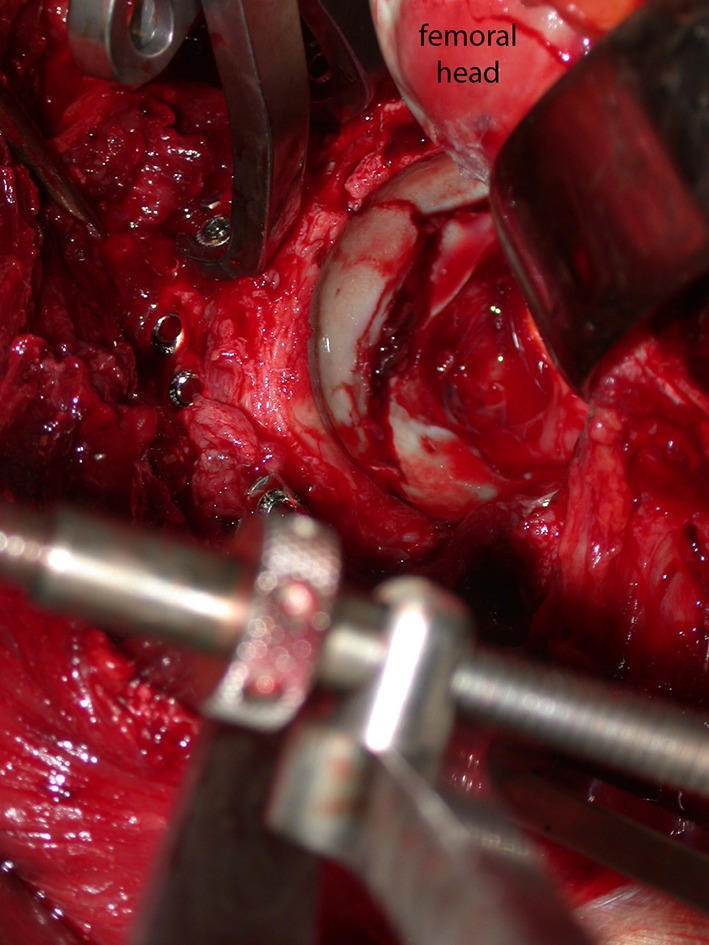
The Jungbluth clamp should be placed according to the direction of the fracture rim; in this case, the anterior column Jungbluth clamp was in the standard location, whereas the posterior Jungbluth clamp was placed closer to the posterior wall to obtain better control of the fragments (in this surgical image of a right acetabular fracture, the head is dislocated anteriorly then moved medially and inferiorly to achieve a better view of the reduction).
In T-shaped fractures, the reduction could be performed by transforming the T fracture into a simple transverse fracture: the two columns can be reduced distally to the transverse fracture with Schanz screws inserted in the ischial tuberosity and in the anterior column; temporary fixation of the columns distal to the fracture is then achieved by inserting one or two Kirschner wires from posterior to anterior. Final reduction and fixation can then be achieved as previously described for transverse fractures. We used this reduction step only in a few cases (three of 10 patients). In the other cases, the reduction of the anterior column had been challenging when the reduction of the columns was attempted separately; its reduction to the upper healthy part of the acetabulum can be facilitated either by a Schanz screw used as a joystick inserted into the anterior column through the articular cartilage of the inner lower part of the acetabulum (Fig. 3) or by using a collinear clamp (Synthes, Paoli, PA, USA) inserted through the vertical branch of the T (Fig. 4). In our experience, the collinear clamp could be very helpful for achieving good reduction without limiting the working space (Fig. 5). Fixation is achieved by one or two 3.5-mm screws inserted into the anterior column, as described before. Reduction and fixation of the posterior column are achieved according to the standard technique, then the femoral head is dislocated again to check the reduction and to ensure that no intraarticular screws are placed.
Fig. 3.

Placement of the posterior Jungbluth clamp and the Schanz screw is shown in a T-shaped fracture sawbone model.
Fig. 4.

Placement of the posterior Jungbluth clamp and the collinear clamp is shown in a T-shaped fracture sawbone model.
Fig. 5.
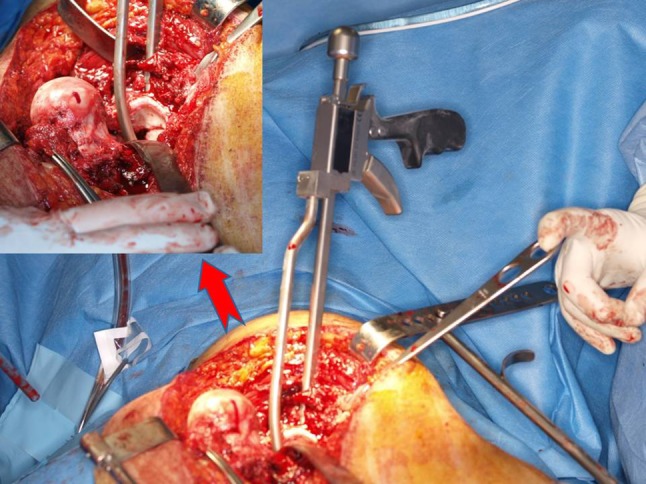
Placement of the posterior Jungbluth clamp and the collinear clamp screw is shown in a surgical image of T-shaped fracture.
The head is relocated in the acetabulum, positioning sutures are applied to the retinaculum and capsule without any tension, and then the trochanteric fragment is fixed with two or three screws [38].
Materials and Methods
Between 2005 and 2011, we used this approach selectively to manage T-type fractures, isolated transverse fractures, or those associated with posterior wall fractures; during the period in question, we surgically treated 312 acetabular fractures, of which 31 (10%) were treated using this approach (Table 1). Before that, the surgeon involved had experience with this approach for other indications, including 40 cases of FAI and 21 cases of slipped capital epiphysis [25]. At the beginning of our learning curve (the first 3 years of this study), indications for surgical dislocation included only complex cases. Inclusion criteria were T-type fractures or transverse fractures isolated or associated with posterior wall fractures with at least of one of the following criteria: (1) comminuted roof area stated as not sufficiently reconstructable through either the Kocher-Langenbeck or ilioinguinal approach alone (roof areas with multiple fracture lines or obvious impaction presenting as comminution zones in the CT scans); and (2) delayed treatment (more than 3 weeks from trauma). From the fourth year of the study, our indication for surgical dislocation included all T-type fractures, isolated transverse fractures, and those associated with posterior wall fractures if displaced by more than 3 mm. All fractures were treated by a single surgeon (first author). During the period in question, only 35% of patients with those fracture patterns (34 of 96 patients) were treated using this approach. One patient was lost to followup, and two were excluded from this study for a concomitant fracture of the ipsilateral lower limb. We performed a surgical dislocation in nine other patients who were excluded for a concomitant femoral head fracture. Another exclusion criterion was a followup shorter than 2 years (12 patients were excluded).
Table 1.
Population data
| Patient number | Sex | Age (years) | Side | Fracture type | Followup (months) |
|---|---|---|---|---|---|
| 11 | M | 47 | Right | T type (transverse transtectal) | 56 |
| 17 | M | 32 | Left | T type (transverse transtectal) | 29 |
| 28 | M | 36 | Left | T type (transverse transtectal) | 26 |
| 29 | M | 44 | Right | T type (transverse transtectal) | 24 |
| 19 | M | 43 | Left | T type (transverse transtectal) | 26 |
| 12 | M | 23 | Left | T-type (transverse infratectal) | 55 |
| 24 | M | 22 | Right | T-type (transverse infratectal) | 24 |
| 26 | M | 55 | Left | T-type (transverse infratectal) | 25 |
| 27 | M | 25 | Right | T-type (transverse infratectal) | 24 |
| 20 | F | 47 | Right | T-type (transverse juxtatectal) | 24 |
| 18 | M | 39 | Left | T-type (transverse juxtatectal) | 27 |
| 1 | F | 19 | Left | T-type (transverse juxtatectal) | 87 |
| 3 | M | 27 | Left | T-type (transverse juxtatectal) | 82 |
| 6 | F | 26 | Right | T-type (transverse juxtatectal) | 65 |
| 25 | M | 29 | Left | Transverse (infratectal) | 25 |
| 4 | M | 36 | Right | Transverse (infratectal) | 68 |
| 2 | M | 40 | Right | Transverse (infratectal) | 83 |
| 14 | M | 37 | Right | Transverse (juxtatectal) | 43 |
| 16 | M | 24 | Right | Transverse (juxtatectal) | 37 |
| 21 | F | 51 | Left | Transverse (juxtatectal) | 24 |
| 23 | M | 44 | Left | Transverse (juxtatectal) | 24 |
| 5 | F | 40 | Left | Transverse (transtectal) | 66 |
| 10 | F | 45 | Right | Transverse (transtectal) | 47 |
| 8 | F | 30 | Left | Transverse + posterior wall | 53 |
| 9 | M | 23 | Left | Transverse + posterior wall | 47 |
| 22 | M | 27 | Left | Transverse + posterior wall | 27 |
| 30 | M | 21 | Right | Transverse + posterior wall | 24 |
| 31 | M | 39 | Right | Transverse + posterior wall (femoral head posterior dislocation) | 41 |
| 7 | M | 48 | Right | Transverse + posterior wall (femoral head posterior dislocation) | 62 |
| 13 | M | 48 | Right | Transverse + posterior wall (femoral head posterior dislocation) | 45 |
| 15 | M | 26 | Left | Transverse + posterior wall (femoral head posterior dislocation) | 38 |
M = male; F = female.
The study was approved by the local ethical committee. Patients were asked to give their informed consent to the use of an unconventional approach when eligible according to the selection criteria.
Patient age at surgery, sex, side of injury, blood loss, operative time, and postoperative complications were recorded in a custom-made database. All patients postoperatively received prophylactic indomethacin therapy. The presence of heterotopic ossification was recorded and graded according to the Brooker classification [2]. Patients were retrospectively reviewed for the purpose of this study and outcome was evaluated with the Merle d’Aubigné-Postel scoring system [6].
The reduction of the fracture was evaluated according to Matta et al.’s criteria [26] by measuring the residual postoperative displacements on the three plain radiographs (AP and Judet views). For each of these radiographs, the maximum displacement seen at any of the normal radiographic lines of the acetabulum or the innominate bone was recorded in millimeters, and the highest of the three values was used to grade the reduction according to one of three categories: anatomical (0–1 mm of displacement), imperfect (2–3 mm), or poor (more than 3 mm). Three surgeons reviewed the postoperative radiographs. In case of disagreement among reviewers, the worst category was used for the final classification. An analysis of interobserver reliability was performed by calculating kappa coefficients with 95% confidence intervals [4]. A kappa value of 1.0 indicates that there is perfect agreement among the reviewers, whereas a value of 0 suggests that the level of agreement is no better than chance alone. A value of less than 0 suggests that there is disagreement among the reviewers, which is the result of more than just chance alone [4]. Minimum followup was 24 months (mean, 43 months; range, 24–87 months).
Results
Fracture reduction was defined as anatomic in 65% of the cases, imperfect in 16%, and poor in 19%. The reviewers showed substantial agreement for the reduction classification; the kappa value was 0.73 (SE 0.12).
The mean surgical time was 203 minutes (SD 69) including anesthetic time; the mean incision to suture time was 150 minutes (SD 54), whereas the mean estimated blood loss was 1334 mL (SD 623). Five patients required homologous blood in the operating room.
The mean Merle d’Aubigné and Postel score was 15 (SD 1.8) points; six patients had an excellent result (21%), and 14 patients had a good result (48%), whereas the clinical score was fair in five cases (17%) and poor in four cases (14%).
Two patients developed symptomatic avascular necrosis of the femoral head and presented a transverse plus posterior wall fracture; closed reduction of the traumatic posterior dislocation was performed before arrival to our hospital.
Four patients developed early osteoarthritis and underwent hip arthroplasty after a mean of 20 months (SD 17). Heterotopic ossification was recorded in seven cases; four patients were classified as Stage II and three patients were classified as Stage III according to the Brooker classification. Two patients presented preoperative sciatic nerve palsy and did not recover complete nerve function after surgery; no iatrogenic nerve palsy occurred.
Discussion
Surgical dislocation of the hip has been previously used to treat a variety of nontraumatic hip pathologies, including FAI, slipped capital femoral epiphysis, and Perthes’ disease. Several papers show the safety of this technique for nontraumatic pathology [8–10, 25, 32, 35, 40, 41]. Ganz et al. [8] reported their experience using this approach for nontraumatic hip conditions in 213 hips in which trochanteric fixation failed in only three patients, and no clinical or radiological evidence of avascular necrosis was found, demonstrating the safety of this approach. However, to our knowledge, only four [30, 38, 39, 45] case series of surgical dislocation for traumatic injuries appear in the literature; three manuscripts were published by the center where this technique was initially described [38, 39, 45]. We believe that this study is interesting because the safety and efficacy of this technique are yet to be demonstrated when performed by other centers; our results support the reproducibility shown in the only published study [30] performed outside the developers’ center.
This study had a number of limitations. First, selection bias and the learning curve could have strongly influenced our results. Although this technique was initially indicated only for complex or multifragmentary cases, not all of the patients with a transverse or T-type fracture were enrolled in the first third of the study (ie, patients older than 55 years were excluded) and indications for this technique were modified during the study period. Second, we also acknowledge that this study comprised a single center and was single surgeon-based. Thus, there is concern about the reproducibility of this technique; the surgeon who performed all surgeries has been trained to perform the technique and has experience either in acetabular fracture treatment through standard approaches or nontraumatic hip disease treatment through surgical dislocation. Our results may not be reproduced by centers without high volumes of acetabular fractures and/or with less experience in this technique for nontraumatic diseases.
Other limitations are the small number of enrolled patients, the absence of a control group, and a short followup. Other patients could develop posttraumatic arthritis over time. One patient has been lost to followup and even a single patient could negatively influence the rate of avascular necrosis. Postoperative reductions were evaluated with radiographs and not with CT scans [29], which is a major limitation for our conclusions regarding the quality of reduction. Three reviewers with experience in hip surgery but work in the study’s institution have evaluated the fractures’ reductions; thus, they might have undergraded the postoperative displacements. Avascular necrosis could also be present in more patients, which were not identified because postoperative MRI was not always performed.
The technique itself also has some limitations, and these deserve comment. Importantly, surgical dislocation presents an optimal view of the anterior column but fracture reduction may be challenging when the anterior rim of the fracture is medial to the iliopubic eminence. The lower extraarticular part of the anterior column is often difficult to visualize and the placement of a reduction clamp may be difficult. New reduction clamps may be useful to avoid this problem, because they may be expressly designed for reduction of the anterior column using surgical dislocation.
Another major limitation of this approach is the lateral decubitus position. The prone position, commonly used during the standard Kocher-Langenbeck approach, could neutralize the gravitational deforming forces and may deskill the reduction [5]; however, in the literature, there is no consensus on this topic [31].
Another important limitation is the limited ability to achieve fixation of the anterior column. Early stability and good compression of the anterior column can be a challenge with one or two screws.
We briefly describe a comparison between our results and either published papers describing standard approaches or the other four papers’ results with this technique. Our rate (65%) of anatomical reduction is comparable to other published studies using standard or extensive approaches; the anatomical reduction rate is reported in the range from 62% to 84% of patients [3, 12, 23, 24, 33, 34, 44] for the easiest patterns of transverse and T-type fractures, whereas in complex cases, it is reported between 14.4% and 68% [20, 33, 36, 42, 46]. A comparison between published results describing surgical dislocation [30, 38, 39, 45] and our study is complicated; for example, in all of the other similar studies, 20% to 33% of patients underwent a second surgical approach (Table 2). This could perhaps justify the slightly inferior rate of anatomical reduction that we achieved, but also our learning curve could have affected the presented results.
Table 2.
Literature reports on surgical dislocation for acetabular fracture
| Study | Number of patients | Fracture type | Surgical approach | Additional surgical approach | Followup (months) | Number of anatomical reductions | Mean Merle d’Aubigne’ scores | Avascular necrosis | Heterotopic ossification |
|---|---|---|---|---|---|---|---|---|---|
| Siebenrock et al. [38] | 12 | 5 Transverse + PW; 3 PW; 1 T-type + PW; 1 T-type; 1 transverse; 1 post column + PW | 12 Kocher-Langembeck | 2 Smith-Petersen 1 Ileoinguinal second win | 35 | 10 | Mean 16.8 (4 patients = 18; 2 patients = 15) | 0 | 4 |
| Siebenrock et al. [39] | 10 | 6 Transverse + PW; 3 PW; 1 T-type + PW | 10 Kocher-Langembeck | 1 Smith-Petersen 1 Ileoinguinal second win | 20 | 8 | 5 18 points; 4 16–17 points; 1 14 points | 0 | 6 |
| Tannast et al. [45] | 60 | 17 Transverse + PW; 24 PW; 3 T-type; 9 transverse; 3 post column + PW; 1 anterior column + post hemitransverse; 3 both columns | 60 Kocher-Langembeck | ? | 53 | 50 | Using Matta Clinical Score 22 excellent; 14 very good; 8 good; 4 fair; 6 poor | 0 | 20 |
| Naranje et al. [30] | 18 | 6 Transverse + PW; 6 PW; 3 T-type; 3 T-type + PW | 18 Kocher-Langembeck | 6 Ileoinguinal | At least 26 | 14 | Mean 17.6 (9 patients = 18; 1 patient = 15) | 1 | 15 |
| Current study | 32 | 8 Transverse + PW; 10 T-type; 9 transverse; 4 post column + anterior hemitransverse | 31 Kocher-Langembeck | 43 | 20 | 6 excellent; 14 good; 6 fair; 4 poor | 2 | 7 |
PW = posterior wall.
Our clinical results are also similar to other case series using standard or extensive approaches; Giannoudis et al. [12], when analyzing 3670 published fractures, showed excellent rates and good results of 86% for transverse fractures, 83% for transverse and posterior wall fractures, and 71% for T-shaped fractures according to the Merle d’Aubigné and Postel grading system. Our results are also comparable with those achieved with the same technique (Table 2).
The mean surgical time reported in this case series seems inferior to the operative time reported for extensile approaches and similar or slightly superior to the Kocher-Langenbeck approach; for example, Kinik and Armangil [20] reported a mean surgical time for the extensile triradiate approach of 280 minutes, and Iselin et al. [17] showed a mean surgical time of 202 minutes when performing a Kocher-Langenbeck approach for posterior wall fractures. Further studies are needed to confirm or disprove these results.
Regarding osteonecrosis of the femoral head, a recent meta-analysis of 3670 surgically treated displaced acetabular fractures reported an incidence of 9.2% for patients with a posterior dislocation, whereas for patients who did not have a posterior dislocation, this figure was 5% [12]. Our rate (6%) could be favorably compared with those data.
Heterotopic ossification rates described in the literature span a wide range from 7% receiving prophylactic indomethacin therapy [11] to 40% with the extensile iliofemoral approach [12, 46]. Our heterotopic ossification rate (23%) seems to be in line with those results.
Surgical dislocation and fracture reduction through this approach could be challenging. Independent from the surgical technique, acetabular fracture treatment itself is often challenging and, we believe, should be performed in specialized referral centers. However, after a period of appropriate training, surgeons working in a center with a high volume of acetabular fractures could, in our opinion, easily add this technique to their portfolio.
The risk of trochanteric malunion or nonunion after surgical dislocation has been described for elective cases but, so far, not in trauma cases [8]. This is likely a function of there not being very many cases of this approach reported for traumatic indications; there is no reason to believe that the risk would be lower in surgical dislocations performed for trauma. Patients should be informed preoperatively about the possible postoperative risks of trochanteric osteotomy.
In contrast, this approach also presents several advantages; the acetabulum and femoral head may be completely visualized and proper evaluation may be made through a single approach, perhaps reducing surgical time. Direct intraarticular assessment helps to achieve proper reduction, even when free and impacted fragments are present. Furthermore, small intraarticular fragments can be directly visualized and removed. Although traction in a standard Kocher-Langenbeck approach can help the surgeon remove small fracture fragments from within the joint, a direct view using a surgical dislocation allows him or her to perform this step with ease. Fixation of the fracture can be performed under direct vision and the screw placement is monitored to avoid intraarticular penetration; therefore, safe screw placement closer to the articular surface may be achieved. This step could be a challenge in the standard posterior approach in which image intensifier pictures and experience guide the procedure.
In our opinion, surgical dislocation is a safe technique and presents several advantages with respect to the standard approaches for complex cases; however, further studies are needed to confirm our results. We remain interested in learning more about this approach and look forward to larger, multicenter trials to see if our promising initial experience can be replicated.
Electronic supplementary material
Video 1 The different techniques for the reduction of fractures through the surgical dislocation technique are shown. (WMV 339487 kb)
Video 2 Reduction of a transverse fracture is commonly performed by pushing the inferior part of the pelvic brim outward and downward. (AVI 39548 kb)
Acknowledgments
We acknowledge the important assistance of Gianluca Amadore, IT administrator, for radiographic information technology support. We would like to thank Dr. Marco M. Favuto for his help with the revision of the discussion session.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed in the Orthopaedic Department, San Luigi Hospital of Orbassano, University of Turin, Turin, Italy.
References
- 1.Alonso JE, Davila R, Bradley E. Extended iliofemoral versus triradiate approaches in management of associated acetabular fractures. Clin Orthop Relat Res. 1994;305:81–87. doi: 10.1097/00003086-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Brooker A, Bowerman J, Robinson R, Riley LH. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1955;55:1629–1632. [PubMed] [Google Scholar]
- 3.Chiu FY, Chen CM, Lo WH. Surgical treatment of displaced acetabular fractures in 72 cases followed for 10 (6 ± 14) years. Injury. 2000;31:181–185. doi: 10.1016/S0020-1383(99)00277-6. [DOI] [PubMed] [Google Scholar]
- 4.Cohen JA. A coefficient of agreement of nominal scales. Educ Psychol Measure. 1960;20:37–46. doi: 10.1177/001316446002000104. [DOI] [Google Scholar]
- 5.Collinge C, Archdeacon M, Sagi HC. Quality of radiographic reduction and perioperative complications for transverse acetabular fractures treated by the Kocher-Langenbeck approach: prone versus lateral position. J Orthop Trauma. 2011;25:538–542. doi: 10.1097/BOT.0b013e31820b913d. [DOI] [PubMed] [Google Scholar]
- 6.d’Aubigné RM, Postel M. The Classic: Functional results of hip arthroplasty with acrylic prosthesis. 1954. Clin Orthop Relat Res. 2009;467:7–27. doi: 10.1007/s11999-008-0572-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daum WJ, Scarborough MT, Gordon W, Jr, Uchida T. Heterotopic ossification and other perioperative complications of acetabular fractures. J Orthop Trauma. 1992;6:427–432. doi: 10.1097/00005131-199212000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 9.Gardner MJ, Suk, Pearle A, Buly RL, Helfet DL, Lorich DG. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma. 2005;19:334–342. [PubMed] [Google Scholar]
- 10.Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679–683. doi: 10.1302/0301-620X.82B5.10426. [DOI] [PubMed] [Google Scholar]
- 11.Ghalambor N, Matta JM, Bernstein L. Heterotopic ossification following operative treatment of acetabular fracture. An analysis of risk factors. Clin Orthop Relat Res. 1994;305:96–105. doi: 10.1097/00003086-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Giannoudis PV, Grotz MRW, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 13.Griffin DB, Beaulé PE, Matta JM. Safety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulum. J Bone Joint Surg Br. 2005;87:1391–1396. doi: 10.1302/0301-620X.87B10.16538. [DOI] [PubMed] [Google Scholar]
- 14.Harris AM, Althausen P, Kellam JF, Bosse MJ. Simultaneous anterior and posterior approaches for complex acetabular fractures. J Orthop Trauma. 2008;22:494–497. doi: 10.1097/BOT.0b013e3181830d2a. [DOI] [PubMed] [Google Scholar]
- 15.Heeg M, Klasen HJ, Visser JD. Operative treatment for acetabular fractures. J Bone Joint Surg Br. 1990;72:383–386. doi: 10.1302/0301-620X.72B3.2341432. [DOI] [PubMed] [Google Scholar]
- 16.Heeg M, Oostvogel HJ, Klasen HJ. Conservative treatment of acetabular fractures: the role of the weight-bearing dome and anatomic reduction in the ultimate results. J Trauma. 1987;27:555–559. doi: 10.1097/00005373-198705000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Iselin LD, Wahl P, Studer P, Munro JT, Gautier E. Associated lesions in posterior wall acetabular fractures: not a valid predictor of failure. J Orthop Traumatol. 2013 June 4 [Epub ahead of print]. DOI: 10.1007/s10195-013-0247-x. [DOI] [PMC free article] [PubMed]
- 18.Johnson EE, Matta JM, Mast JW, Letournel E. Delayed reconstruction of acetabular fractures 21–120 days following injury. Clin Orthop Relat Res. 1994;305:20–30. [PubMed] [Google Scholar]
- 19.Kaempffe FA, Bone LB, Border JR. Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;5:439–445. doi: 10.1097/00005131-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Kinik H, Armangil M. Extensile triradiate approach in the management of combined acetabular fractures. Arch Orthop Trauma Surg. 2004;124:476–482. doi: 10.1007/s00402-004-0694-1. [DOI] [PubMed] [Google Scholar]
- 21.Kumar A, Shah NA, Kershaw SA, Clayson AD. Operative management of acetabular fractures. A review of 73 fractures. Injury. 2005;36:605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 22.Letournel E, Judet R. Fractures of the Acetabulum. 2. Berlin, Germany: Springer-Verlag; 1993. pp. 521–588. [Google Scholar]
- 23.Li XG, Tang TS, Sun JY. Results after surgical treatment of transtectal transverse acetabular fractures. Orthop Surg. 2010;2:7–13. doi: 10.1111/j.1757-7861.2009.00056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Q, Wu D, Li P, Han SF. Surgical treatment for complex acetabular fractures. Chin J Traumatol. 2006;9:325–328. [PubMed] [Google Scholar]
- 25.Massè A, Aprato A, Grappiolo G, Turchetto L, Campacci A, Ganz R. Surgical hip dislocation for anatomic reorientation of slipped capital femoral epiphysis: preliminary results. Hip Int. 2012;22:137–144. doi: 10.5301/HIP.2012.9208. [DOI] [PubMed] [Google Scholar]
- 26.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 27.Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986;205:230–240. [PubMed] [Google Scholar]
- 28.Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;407:173–186. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 29.Moed BR, Carr SE, Gruson KI, Watson JT, Craig JG. Computed tomographic assessment of fractures of the posterior wall of the acetabulum after operative treatment. J Bone Joint Surg Am. 2003;85:512–522. doi: 10.2106/00004623-200303000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Naranje S, Shamshery P, Yadav CS, Gupta V, Nag HL. Digastric trochanteric flip osteotomy and surgical dislocation of hip in the management of acetabular fractures. Arch Orthop Trauma Surg. 2010;130:93–101. doi: 10.1007/s00402-009-0873-1. [DOI] [PubMed] [Google Scholar]
- 31.Negrin LL, Benson CD, Seligson D. Prone or lateral? Use of the Kocher-Langenbeck approach to treat acetabular fractures. J Trauma. 2010;69:137–141. doi: 10.1097/TA.0b013e3181b28ba6. [DOI] [PubMed] [Google Scholar]
- 32.Nötzli HP, Siebenrock KA, Hempfing A, Ramseier LE, Ganz R. Perfusion of the femoral head during surgical dislocation of the hip. Monitoring by laser Doppler flowmetry. J Bone Joint Surg Br. 2002;84:300–304. doi: 10.1302/0301-620X.84B2.12146. [DOI] [PubMed] [Google Scholar]
- 33.Oh CW, Kim PT, Park BC, Kim SY, Kyung HS, Jeon IH, Cheon SH, Min WK. Results after operative treatment of transverse acetabular fractures. J Orthop Sci. 2006;11:478–484. doi: 10.1007/s00776-006-1045-6. [DOI] [PubMed] [Google Scholar]
- 34.Onche II, Obiano SK, Udoh MK. A prospective evaluation of the management and outcome of traumatic posterior dislocation of the hip: a preliminary report. Niger J Med. 2008;17:163–167. doi: 10.4314/njm.v17i2.37376. [DOI] [PubMed] [Google Scholar]
- 35.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 36.Porter SE, Graves ML, Allan Maples R, Woodall JJ, Wallace JG, Russell ML. Acetabular fracture reductions in the obese patient. J Orthop Trauma. 2011;25:371–377. doi: 10.1097/BOT.0b013e3181f974f4. [DOI] [PubMed] [Google Scholar]
- 37.Reinert CM, Bosse MJ, Poka A, Schacherer T, Brumback RJ, Burgess AR. A modified extensile exposure for the treatment of complex or malunited acetabular fractures. J Bone Joint Surg Am. 1988;70:329–337. [PubMed] [Google Scholar]
- 38.Siebenrock KA, Gautier E, Woo AK, Ganz R. Surgical dislocation of the femoral head for joint débridement and accurate reduction of fractures of the acetabulum. J Orthop Trauma. 2002;16:543–552. doi: 10.1097/00005131-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Siebenrock KA, Gautier E, Ziran BH, Ganz R. Trochanteric flip osteotomy for cranial extension and muscle protection in acetabular fracture fixation using a Kocher-Langenbeck approach. J Orthop Trauma. 1998;12:387–391. doi: 10.1097/00005131-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Sink EL, Beaulé PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicentre study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132–1136. doi: 10.2106/JBJS.J.00794. [DOI] [PubMed] [Google Scholar]
- 41.Spencer S, Millis MB, Kim YJ. Early results of treatment for hip impingement syndrome in slipped capital femoral epiphysis and pistol grip deformity of femoral head-neck junction using the surgical dislocation technique. J Pediatr Orthop. 2006;26:281–285. doi: 10.1097/01.bpo.0000217726.16417.74. [DOI] [PubMed] [Google Scholar]
- 42.Stannard JP, Harris HW, Volgas DA, Alonso JE. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;377:44–56. doi: 10.1097/00003086-200008000-00008. [DOI] [PubMed] [Google Scholar]
- 43.Starr AJ, Watson JT, Reinert CM, Jones AL, Whitlock S, Griffin DR, Borer DS. Complications following the ‘T extensile’ approach: a modified extensile approach for acetabular fracture surgery—report of forty-three patients. J Orthop Trauma. 2002;16:535–542. doi: 10.1097/00005131-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Stöckle U, Hoffmann R, Südkamp NP, Reindl R, Haas NP. Treatment of complex acetabular fractures through a modified extended iliofemoral approach. J Orthop Trauma. 2002;16:220–230. doi: 10.1097/00005131-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Tannast M, Krüger A, Mack PW, Powell JN, Hosalkar HS, Siebenrock KA. Surgical dislocation of the hip for the fixation of acetabular fractures. J Bone Joint Surg Br. 2010;92:842–852. doi: 10.1302/0301-620X.92B6.22994. [DOI] [PubMed] [Google Scholar]
- 46.Triantaphillopoulos PG, Panagiotopoulos EC, Mousafiris C, Tyllianakis M, Dimacopoulos P, Lambiris EE. Long-term results in surgically treated acetabular fractures through the posterior approaches. J Trauma. 2007;62:378–382. doi: 10.1097/01.ta.0000196540.81630.4e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1 The different techniques for the reduction of fractures through the surgical dislocation technique are shown. (WMV 339487 kb)
Video 2 Reduction of a transverse fracture is commonly performed by pushing the inferior part of the pelvic brim outward and downward. (AVI 39548 kb)


