Abstract
Background
It is unclear whether late THA dislocations are related to mechanical impingement or to a biological mechanism that decreases the stability provided by the capsule (eg, inflammation secondary to osteolysis). It is also unknown if alumina-on-alumina bearing couples decrease the risk of late dislocation as a result of the absence of wear and osteolysis.
Question/purposes
We asked (1) whether the cumulative number of dislocations differed with alumina-on-alumina (AL/AL) or alumina-on-polyethylene bearings (AL/PE); (2) whether patient factors (age, sex, and diseases) affect risk of late dislocation; (3) whether mechanical factors (component malposition, penetration resulting from creep and wear) or (4) biologic hip factors at revision (thickness of the capsule, volume of joint fluid removed at surgery, histology) differed with the two bearing couples.
Methods
One hundred twenty-six patients (252 hips) with bilateral THA (one AL/AL and the contralateral AL/PE) received the same cemented implants except for the cup PE cup or an AL cup. The cumulative risk of dislocation (first-time and recurrent dislocation) was calculated at a minimum of 27 years. We measured cup position, creep and wear, and capsular thickness in the hips that had revision.
Results
AL/PE and AL/AL hips differed by the cumulative number of dislocation (31 with AL/PE versus four with AL/AL) and by the number of late dislocations (none with AL/AL, 28 with AL/PE). Cause of osteonecrosis, age, and sex affected the number of dislocations. The frequency of component malposition did not differ between the two bearing couples. The risk of late dislocation appeared less in AL/AL hips with increased capsular thickness (mean, 4.5 mm; range, 3–7 mm) compared with the thinnest (mean, 1.2 mm; range, 0.2–2 mm) capsule of AL/PE hips.
Conclusions
AL/AL bearing couples decreased the cumulative risk of dislocation as compared with AL/PE bearing couples.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Dislocation is a common complication of THA and a leading cause of revision [12, 16, 23]. Instability resulting in dislocation impairs function, is distressing for patients, and is a disturbing complication for surgeons. Dislocation can present as a single or a recurring event [23] and consists of two related yet separate conditions occurring early or late [2, 9, 36], although definitions of what constitutes early and late vary. The occurrence of a first-time dislocation appears highest during the first few months after hip arthroplasty; however, first-time late dislocation also can occur many years after the procedure. Berry et al. [2] demonstrated that there is an indefinite, low-level risk of first-time dislocation after hip arthroplasty with polyethylene (PE) cups and 22-mm diameter heads and that the cumulative (first time, late, and recurrent) long-term number of dislocations after THA may be higher than immediately postoperative (1 year) in some patients. However, the reasons for late dislocation after hip arthroplasty likely differ: late dislocations have been associated with increased soft tissue compliance, trauma, neurological decline, and PE wear [26, 36]. Although bearing couples with aluminum (AL)-PE friction have a low wear rate [34, 35], bearing couples with hard-on-hard friction are associated with minimal or no wear and low osteolysis rates, and it is unclear whether these bearings will change the risk of late dislocation as a result of the absence of wear. In our 20-year study of patients with an AL/AL bearing in one hip and AL-on-PE (AL/PE) in the other [18], we were surprised when we identified no late dislocation in these patients and in contrast to our experience with arthroplasties with AL/PE bearings.
We therefore asked (1) whether the cumulative number of dislocations differed with AL/AL or AL/PE bearings; (2) whether patient factors (age, sex, and diseases) affecting risk of dislocation; (3) whether mechanical hip factors (component malposition, penetration resulting from creep and wear); and (4) whether biologic hip factors at revision (thickness of the capsule, volume of joint fluid, histology) affecting risk of dislocation differed with the two bearing couples.
Patients and Methods
We retrospectively reviewed 126 patients (252 hips) with bilateral THA (one ceramic-on-ceramic, AL/AL, and the contralateral ceramic-on-PE, AL/PE) who had THA performed from 1978 to 1985. Between 1978 and 1982, osteonecrosis in young patients was an indication for an AL/AL hip. Because there was concern about fixation of the AL cup with cement resulting from the observation of early loosening between cement and an AL cup [13], after 1982 the second arthroplasty of a series of patients with bilateral osteonecrosis was AL/PE. The mean age at surgery was 45 years (range, 29–60 years). The indication for surgery was late-stage osteonecrosis with a substantial amount of flattening of the articular surface. THA was a primary procedure in all hips. Of the initial cohort of 126 patients, 12 patients were lost to followup after 25 years followup, and 30 died at an average followup of 22 years (range, 13–26 years). This left 84 living patients for study. The underlying diagnosis was osteonecrosis for all patients. The cause of osteonecrosis was alcohol abuse in 28, corticosteroid treatments in 32, sickle cell disease in 26 patients, and other various causes for the other patients. There were 56 female patients and 70 male patients. The mean age at surgery was 45 years (range, 29–60 years). The minimum followup was 30 years (mean, 32 years; range, 30–34 years) after the AL/AL hips and 27 years (mean, 29 years; range, 27–30 years) after the AL/PE hips. Among the 63 patients who were 75 years of age or older at the most recent followup, occurrence of cognitive dysfunction (confusion, dementia, psychosis) or neuromuscular dysfunction (alcoholism, stroke, or Parkinson’s disease) had occurred in 21 patients. Of the 252 hips, there were 82 hips that had been revised for another cause other than dislocation (cup loosening for 38 AL/AL hips and 44 AL/PE hips) at the most recent followup.
Surgery was performed with a posterolateral approach under general anesthesia. Capsular repair was not performed and the external rotator muscles were not reattached to the femoral bone. All patients received the same implants except for the cups. The prostheses were manufactured by Ceraver (Ceraver Osteal, Roissy, France) and sterilized with ethylene oxide at this period. The stem was made of anodized titanium alloy (TiAl6V4) and was smooth and always cemented. The AL head was always 32 mm in diameter and anchored through the same Morse taper (14–16 mm; 5°–42°). Therefore, all patients had the same head-neck ratio. The acetabular components were made either of PE or AL. Both components were always fixed with cement (Palacos G; Heraeus Medical GmbH, Hanau, Germany) containing antibiotics (gentamicin). The single-part AL acetabular component had grooves on the outer surface.
Postoperatively the patients were encouraged to be upright with weightbearing after surgery. No patient was placed into a hip spica cast to minimize the possibility of hip dislocation. ROM of the hip and knees was begun immediately and ambulation progressed as tolerated according to the ability of each patient (usually after 48 hours). The physiotherapy was supervised by a medical doctor for the first 3 weeks and continued for 45 days.
The routine followup was 3, 6, and 12 months and then annually thereafter. At each visit, patients underwent clinical and radiological evaluation. From the charts, we determined whether there were any dislocations (posterior or anterior) or revisions for recurrent dislocation or loosening. We routinely evaluated patients, in person or by means of a standardized letter or telephone questionnaire, at 2 to 3 months postoperatively; at 1, 2, and 5 years; and then at each subsequent 5-year interval until revision or death. At each time point, we specifically asked patients whether they had dislocation of the hip. We did not consider a sensation of subluxation of the hip to be sufficiently specific to represent an episode of hip instability. We only considered a complete hip dislocation (the head has moved completely out of the acetabulum and required anesthesiology and surgeon intervention to relocate the hip) to be a dislocation event. For each patient, the cumulative risk of dislocation was calculated as the sum of all the dislocations. Late dislocation has been defined as occurring 2 or more years after surgery. Therefore, a first-time dislocation could be early or late and recurrent dislocation could be early or late. Analysis of dislocations was performed on all patients of the series.
Wear was considered as a risk of dislocation because of subsequent decentering in the joint. Three of us who were not treating surgeons (YH, OP, IG) made all measurements from standard frontal and lateral views. The technique used for measurement of PE wear and creep was adapted [19] from a technique previously described [14, 15, 17, 18] used both for measurement and accuracy (intraobserver and interobserver errors were less than 0.09 mm). By comparison with the initial postoperative and long-term followup films, measurement of the femoral head penetration within the cup could be made. Acetabular cup position was considered as a risk of dislocation [28]. Determining the exact three-dimensional orientation of an acetabular cup from plain radiographs is basically not possible, except when additional landmarks are available. Nevertheless, we had plain radiographs of the pelvis with both hips for each patient. Therefore, comparative inclination and anteversion cup angles could be determined for both hips. Acetabular inclination was assessed according to the acetabular abduction angle [28]. Radiographic anteversion was calculated using the inverse sinus function and the circular opening of the cup projecting as an ellipse with the simplified method to determine acetabular cup anteversion from plain radiographs described by Widmer and Ing [37].
Among the 82 hips revised, we examined the operative reports for comments about the macroscopic characteristics of the two bearing couples at revision. The amount of fluid present in the joint was estimated at revision by joint aspiration (volume of liquid filling the syringe) in 76 hips before opening the capsule. Time from revision to dislocation (for hips with dislocation) was average 2 years (range 1–5 years). In the first six revisions (resulting from all causes) in the AL/AL hips, we used the term fibrous and thick capsule to describe the capsule. This led us to routinely measure capsular thickness with a caliper in the subsequent 76 revisions. Measurements (two or three for each capsule) were performed on the posterior part of the capsule and the mean of these measurements calculated. Histology (frozen section) of the capsule was obtained in hips that underwent revision; from the reports we recorded presence of PE or AL particles and inflammatory response as giant cell reactions to debris. We lacked data regarding the capsule on six of the revised hips and of course have no data on the capsule of those hips that had no revision. However, we have also experience on revision of other AL/AL and AL/PE hips (than in these bilateral comparative hip studies) to support our data in the discussion.
Qualitative data (sex, cause of osteonecrosis, and presence of PE or AL particles and giant cell reactions to debris from the histological sections) were expressed as counts and percentages between the two groups of cups and quantitative data by mean ± SD or range. Qualitative data between the two groups were compared with use of the chi-square test or Fisher’s exact test. Multivariate analysis was used to compare dislocation rates between AL/AL and AL/PE hips while adjusting for age, wear, acetabular abduction angle, and anteversion angle. Kaplan-Meier survivorship analysis [20], with 95% confidence intervals, was used to estimate the cumulative probability of not having a dislocation in the whole series. Differences in survival between the two groups were determined using the log-rank test. The cumulative risk of dislocation as reported by Berry et al. [2] was estimated using the Kaplan-Meier method [20].
Results
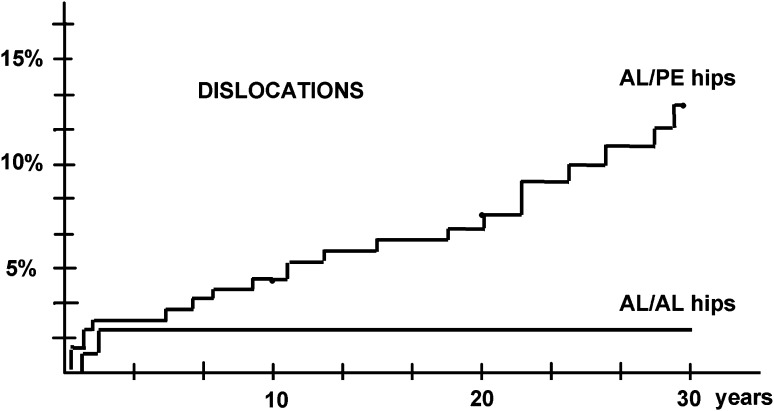
The cumulative number of dislocations (both first-time and recurrent dislocation) differed for the two groups of cups (Table 1). For the AL/PE group, the percentage of a first-time dislocation (Fig. 1) was 1% at 1 month and 2% at 1 year and then rose to 13% at 30 years (for patients who were alive and had not had a revision by that time); this percentage was higher (p = 0.01) than the 2% observed at 30 years for the AL/AL group. Recurrent hip dislocations also were more frequent (p = 0.02) with PE cups (15 in AL/AL hips compared with two in AL/PE hips). At last followup, we found a lower cumulative number of dislocations (p = 0.02) in patients with AL/AL hips compared with the AL/PE hips: four versus 31, respectively. Five hips with PE cups and late recurrent dislocations had revision for this problem treated with a constrained cup. In the group of AL/AL hips, only one patient had early (within 2 years) recurrent dislocations twice. No hip had revision for dislocation in the AL/AL group. Except during the first period (within 2 years followup) in which anterior and posterior dislocations were observed, all late dislocations (after 2 years followup) were posterior.
Table 1.
Dislocations in AL/AL and AL/PE hips
| Dislocation | AL/AL hips (n = 126) | AL/PE hips (n = 126) | p value |
|---|---|---|---|
| Early first time < 2 years | 2 (1.6%) | 2 (1.6%) | 0.82 |
| Late first time > 2 years | 0 (0%) | 14 (11%) | < 0.001 |
| Recurrent | 2 (1.6%) | 15 (12%) | 0.01 |
| Cumulative number | 4 (3.2%) | 31 (25%) | < 0.001 |
Values are expressed as number of dislocations with percentage in parentheses. For recurrent dislocations, the first time was not counted; AL/AL = alumina-on-alumina; AL/PE = alumina-on-polyethylene.
Fig. 1.
For hips with PE cups, the percentage of first-time dislocations was 1% at 1 month and 2% at 1 year, rose with an increasing rate of 2.4% from Year 2 to 10 to reach 4.5% at 10 years, rose with an increasing rate of 3.6% from Year 10 to 20 to reach 8% at 20 years, and then rose with an increasing rate of 5% from Year 20 to 30 to elevate to 13% (95% confidence interval, 9%–17%) at 30 years for patients who were alive and had not had a revision by that time. For hips with AL cups, the percentage of first-time dislocations was 1% at 1 month, 2% at 1 year, and then did not change at 20 years and at 30 years (2%; 95% confidence interval, 1%–3%) for patients who were alive and had not had a revision by that time.
Patient factors (cause of osteonecrosis, age, sex) affected the number of dislocations (Table 2). Alcohol (p = 0.04) as the underlying cause of osteonecrosis of the femoral head, occurrence of cognitive dysfunction (confusion, dementia, psychosis) or neuromuscular dysfunction (stroke, or Parkinson’s disease) in older patients (p = 0.02), and particularly in women (p = 0.04) were associated with a greater risk of dislocation in AL/PE hips. However, late dislocations occurred only in hips with PE bearings.
Table 2.
Patient parameters
| Parameters | Early dislocations | Late dislocation | Without dislocation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AL/PE (n = 2/126) |
AL/AL (n = 2/126) |
p value | AL/PE (n = 14/126) |
AL/AL (n = 0/126) |
p value | AL/PE (n = 110/126) |
AL/AL (n = 124/126) |
p value | |
| Age at the most recent followup | |||||||||
| 63 patients < 75 years (number, %) | 2/63 (3.2%) | 2/63 (3.2%) | 0.75 | 1/63 (3.2%) | 0/63 (0%) | 0.66 | 60/63 (92.6%) | 61/63 (96.8%) | 0.66 |
| 63 patients > 75 years (number, %) | |||||||||
| 21 with cognitive or neurologic dysfunction (number, %) | 0/21 (0%) | 0/21 (0%) | NA | 10/21 (47.7%) | 0/21 (0%) | 0.02 | 11/21 (52.3%) | 21/21 (100%) | 0.02 |
| 42 without cognitive or neurologic dysfunction (number, %) | 0/42 (0%) | 0/42 (0%) | NA | 3/42 (7.1%) | 0/42 (0%) | 0.07 | 39/42 (92.9%) | 42/42 (100%) | 0.07 |
| Sex | |||||||||
| 70 men (number, %) | 1/70 (1.4%) | 1/70 (1.4%) | 0.66 | 4/70 (5.7%) | 0/70 (0%) | 0.08 | 65/70 (92.9%) | 69/70 (98.6%) | 0.08 |
| 56 women (number, %) | 1/56 (1.8%) | 1/56 (1.8%) | 0.72 | 10/56 (17.9%) | 0/56 (0%) | 0.04 | 45/56 (80.3%) | 55/56 (98.2%) | 0.04 |
| Cause of osteonecrosis | |||||||||
| 28 alcohol abuse (number, %) | 2/28 (7.1%) | 2/28 (7.1%) | 0.52 | 6/28 (21.4%) | 0/28 (0%) | 0.04 | 20/28 (71.4%) | 26/28 (92.9%) | 0.04 |
| 32 corticosteroid (number, %) | 0/32 (0%) | 0/32 (0%) | NA | 3/32 (9.4%) | 0/32 (0%) | 0.24 | 29/32 (90.6%) | 32/32 (100%) | 0.24 |
| 26 sickle cell disease (number, %) | 0/26 (0%) | 0/26 (0%) | NA | 2/26 (7.7%) | 0/26 (0%) | 0.24 | 24/26 (92.3%) | 26/26 (100%) | 0.24 |
| 40 others (number, %) | 0/40 (0%) | 0/40 (0%) | NA | 3/40 (7.5%) | 0/40 (0%) | 0.16 | 37/40 (92.5%) | 40/40 (100%) | 0.24 |
AL/PE = alumina-on-polyethylene; AL/AL = alumina-on-alumina; NA = not available.
There was no difference between the two groups of cups when mechanical hip factors (component malposition) affecting risk of dislocation (Table 3) were analyzed. The acetabular abduction angle (p = 0.43) and the anteversion angles (p = 0.36) were not different between the two groups, and the AL/PE group also was not different between those with and without late dislocations (p = 0.41). Head penetration resulting from creep and wear was similar (p = 0.24) in the 14 AL/PE hips with late and recurrent dislocations as compared with the penetration in the AL/PE hips without any late dislocations.
Table 3.
Mechanical hips parameters
| Parameters | Early dislocations | Late dislocations | Without dislocations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AL/PE (n = 2) |
AL/AL (n = 2) |
p value | AL/PE (n = 14) |
AL/AL (n = 0) |
p value | AL/PE (n = 110) |
AL/AL (n = 124) |
p value | |
| Anteversion angle in degrees: mean (range) | 19° (17°–21°) | 16° (11°–22°) | 0.36 | 20° (10°–36°) | NA | NA | 21° (14°–30°) | 18° (10°–25°) | 0.36 |
| Abduction angle in degrees: mean (range) | 45° (41°–49°) | 45° (42°–48°) | 0.54 | 46° (32°–57°) | NA | NA | 45° (28°–51°) | 47° (31°–55°) | 0.43 |
| Wear as cup penetration in mm/year: mean (range) | 0.04 (0.02–0.06) | None | NA | 0.04 (0.02–0.07) | NA | NA | 0.06 (0.03–0.09) | 0.002 (0.001–0.007) | < 0.001 |
AL/PE = alumina-on-polyethylene; AL/AL = alumina-on-alumina; NA = not available.
There was a difference in thickness of the capsule, volume of joint fluid, and histology (PE or AL particles and inflammatory response as giant cells reactions to debris) affecting risk of dislocation (Table 4) analyzed at revision. Of the number of variables explored with multivariate analysis, the thickness of the capsule was deemed to be the most relevant to the risk of late dislocation. During revisions macroscopically, the capsule was fibrous and thick (mean, 4.5 mm; range, 3–7 mm) with AL/AL hips and thinner (p = 0.03) (mean, 1.2 mm; range, 0.2–2 mm) with PE cups. Hips with AL cups had a small volume of fluid inside the joint (mean, 3.2 cc; range, 2–5 cc). At revision, hips with PE cups had more fluid (p = 0.02) inside the joint with a mean volume of 18 cc (range, 12–31 cc). In the AL/PE group, we identified PE in all the capsules that were analyzed. Typical macrophage and giant cell reactions to PE debris were frequent. In the ceramic-on-ceramic capsules, we identified particles of AL (yellow color with brown outlines); giant cells were not observed.
Table 4.
Biologic joint parameters (capsule, volume of fluid, histology) in hips that had revision
| Parameters | AL/AL hips (n = 32) | AL/PE hips (n = 44) | p value |
|---|---|---|---|
| Capsule thickness | |||
| With late dislocation: mean (range) | NA | 1.1 mm (0.3–1.6 mm) | NA |
| Without dislocation: mean (range) | 4.5 mm (3–7 mm) | 1.3 mm (0.2–2 mm) | 0.03 |
| Volume of fluid in the joint | |||
| With late dislocation: mean (range) | NA | 17 mL (12–26 mL) | NA |
| Without dislocation: mean (range) | 3.2 mL (2–5 mL) | 20 mL (14–31 mL) | 0.02 |
| Histology of capsule | |||
| With late dislocation | |||
| AL debris: yes/no | NA | No | NA |
| PE debris: yes/no | NA | Yes | NA |
| Giant cells: yes/no | NA | Yes | NA |
| Without late dislocation | |||
| AL debris: yes/no | Yes | No | < 0.001 |
| PE debris: yes/no | No | Yes | < 0.001 |
| Giant cells: yes/no | No | Yes | < 0.001 |
Values are expressed as mean with range in parentheses. There are no data for AL/AL hips with late dislocation; AL/AL = alumina-on-alumina; AL/PE = alumina-on-polyethylene; NA = not available.
Discussion
Boutin [6] and Boutin and Blanquaert [7] reported the use of AL/AL bearing couples in THA in 1972. Although ceramic implants have been in use for many years [4, 10, 11, 13, 16, 21, 24, 27, 31–33], few reports [8, 25] describe the risk of dislocation associated with ceramic bearing couples. Because wear has previously been suspected as a risk for late dislocation [2, 9], the risk of late dislocation should be decreased with an AL/AL bearing surface. We therefore determined (1) whether the cumulative number of dislocations differed with AL/AL or AL/PE; (2) whether patient factors (age, sex, and diseases) affecting risk of dislocation; (3) whether mechanical hip factors (component malposition, penetration resulting from creep and wear); and (4) whether biologic hip factors at revision (thickness of the capsule, volume of the joint, histology) affecting risk of dislocation differed with the two bearing couples.
We note several limitations to our study. First, ours was a retrospective study of a nonrandomized patient population. The two different procedures were performed in the same patients but at different times, although the surgeon was the same and attempted to keep the same approaches and same perioperative treatments except for the cup. Second, the followup was longer with the AL/AL bearing couple; however, this difference is moot because the higher number of dislocations was observed in the group with the shortest followup. Third, some patients were lost to followup during this study; others died. It is possible some patients had unknown dislocations treated in another hospital and not related. Fourth, although we performed a multivariate analysis, we did not evaluate all the parameters that are at risk for dislocation such as limb length discrepancy or femoral anteversion. Only patients who had a primary arthroplasty with the same implant during the study period were included, which may have affected the ability to detect differences associated with other implants. Lastly, the size of our population is small. However, one of the advantages of our series is that surgery was performed in the same patients with a consistent surgical technique and the same arthroplasty, which reduced some variability. A single implant design (with two different bearing couples) was chosen for this study to minimize variables (such as head size, prosthetic neck geometry, and acetabular component design) that might confound analysis.
The number of dislocations (Table 5) observed in different series appears related to bearing couples and femoral head size, but also related to the followup. The present study demonstrates that after THA with a PE cup with a 32-mm head, the longer patients were followed, the greater the cumulative risk for THA with a PE cup exactly as described with a Charnley THA using a 22-mm cup [2, 8]. In this series of patients followed for 30 years, the total number of late dislocations (27 cases) was higher than the number of early dislocations (four cases) with AL/PE cups. Our observations also demonstrate the bearing couples influence this risk because no late dislocation was observed on AL/AL hips. Given each patient served as his or her own control, this implies some “local” factor protected AL/AL hips against late dislocation.
Table 5.
Followup and associated dislocation rates according to the couple of fraction and head size
| Publication | Bearing couples | Size (mm) | Mean length of followup | Number of THAs | Percent dislocations (number of dislocations) |
|---|---|---|---|---|---|
| Berry et al. [2] | Metal-on-polyethylene | 22 | 25 years | 693 | 7 (49) |
| Berry et al. [3] | Metal-one-polyethylene | 22 | 10 years | 8691 | 3.8 (334) |
| 28 | 8797 | 4.3 (381) | |||
| 32 | 3559 | 2.7 (97) | |||
| Peters et al. [29] | Metal-on-polyethylene | 28 | 52 months | 160 | 2.5 (4) |
| 38 | 28 months | 136 | 0 | ||
| Cuckler et al. [10] | Metal-on-metal | 28 | 5.3 years | 78 | 2.6 (2) |
| 38 | 1.1 years | 616 | 0 | ||
| Peters et al. [29] | Metal-on-metal | 38 | 36 months | 370 | 0.3 (1) |
| 40–56 | 99 | 1.0 (1) | |||
| Amstutz et al. [1] | Metal-on-metal | 36–54 | 3.5 years | 400 | 0.8 (3) |
| Colwell et al. [8] | Ceramic-on-ceramic | 28 | 35 months | 158 | 1.9 (3) |
| 32 | 1154 | 1.3 (15) | |||
| 36 | 323 | 0 | |||
| Current study | AL/PE | 32 | 32 years | 126 | 12.6 (15) |
| Current study | AL/AL | 32 | 29 years | 126 | 1.6 (2) |
Number and percentage of dislocations are approximated from data in the articles; AL/PE = alumina-on-polyethylene; AL/AL = alumina-on-alumina.
Patient factors influence in many ways the risk of dislocation after THA. In the early period, patient factors such as poor early adherence to postoperative regimens, osteonecrosis, obesity, sex, and substance abuse (alcohol) creating neurologic dysfunction have been reported in the literature [26]. Some are confirmed by our series in which patients with osteonecrosis related to alcohol abuse had an increased number of first-time and recurrent dislocations on both sides (AL/AL and AL/PE) during the early postoperative period (within 2 years followup) as compared with patients presenting other causes of osteonecrosis. Late dislocation patient factors such as increase age, sex (female), and neurological decline have previously been recognized or suspected in the literature. The present study confirms that both the age of the patient and sex (woman) are related to the probability of late dislocation. However, for late dislocation, the risk occurred only on the AL/PE side.
Hip mechanical factors affecting risk of dislocation include operative approach, component design [1, 10, 29] and selection, component positioning [28], failure to restore proper hip mechanics, and head penetration in the cup [9]. The same posterior approach, with absence of capsular repair and absence of rotator muscle reattachment to the femoral bone, was performed for all the hips of our series. On the femoral side, the femoral stem had a unique offset at this period, and the length of the neck choice was limited (as a result of ceramic head use), but this inconvenience did not appear vital in this series for the early or late risk of dislocation in AL/AL hips. For late dislocations, because all late dislocations were posterior, abnormal orientation of the cup could have been suspected as a risk factor in our series; however, hips with late dislocations had a similar anteversion and abduction as the hips without dislocation. Wear has previously been suspected as a risk factor, but the present study provides some interrogation about the risk of wear in late dislocations. Although AL cups can be assumed to have little or no wear [15, 21, 27, 30], AL/PE hips with late dislocation had no more wear than the other PE cups without dislocation.
Biologic hip factors affecting late risk of dislocation include the capsule of the joint. A fibrous and thick capsule present in ceramic-on-ceramic hips was present at all revisions we performed whatever the cause of revision in contrast to a thin capsule without resistance present in hips with PE cups. Hips with AL cups had no fluid inside the joint (or a few centimeters; less than 5 cc). Hips with PE cups had fluid inside the capsule with a volume of more than 20 cc creating distention of the capsule and probably a decrease in thickness of the capsule. The reasons for these differences are probably attributable to different biologic responses of the capsule to wear debris as previously suggested [5, 22]. A possible explanation is that the thick capsule of AL/AL hips protects the hip against late dislocation when general factors such as age or cognitive and neuromuscular-related disorders occurred in these patients. At this time it is difficult to know if the thickness of the capsule increased with followup in AL/AL hips and on the contrary decreased with time in AL/PE hips as a result of the different biologic responses (as is suspected by the authors), and this will be explored in the future. Also we do not know if the PE liners (with or without large heads) used today will behave differently despite the fact that wear was not the presumed cause for dislocations.
In conclusion, AL/AL bearing couples decreased the cumulative risk of dislocation as compared with AL/PE bearing couples in the same patients. The reasons for the lower rate of dislocation with AL/AL bearings likely related to the difference between the histology of the capsule of the hips with the two bearing couples (fibrous and thick with ceramic on ceramic; thin and more elastic with PE cups) and we suspect to inflammatory reactions related to wear debris.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 2.Berry DJ, Von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 4.Bizot P, Banallec L, Sedel L, Nizard R. Alumina-on-alumina total hip prostheses in patients 40 years of age or younger. Clin Orthop Relat Res. 2000;379:68–76. doi: 10.1097/00003086-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Bos I, Henssge EJ, Willmann G. Morphological characterization of joint capsules around hip prostheses with alumina or alumina combinations. In: Puhl W, editor. Die Keramikpaarung Biolox in der Hueftendoprothetik. Stuttgart, Germany: Enke Verlag; 1996. pp. 24–30. [Google Scholar]
- 6.Boutin P. [Total hip arthroplasty with alumina on alumina bearing friction] [in French] Rev Chir Orthop. 1972;58:229–246. [PubMed] [Google Scholar]
- 7.Boutin P, Blanquaert D. [Alumina on alumina friction in total hip arthroplasty. 1205 hips from 1970 to 1980] [in French] Rev Chir Orthop. 1970;1981(67):279–287. [PubMed] [Google Scholar]
- 8.Colwell CW, Jr, Hozack WJ, Mesko JW, D’Antonio JA, Bierbaum BE, Capello WN, Jaffe WL, Mai KT. Ceramic-on-ceramic total hip arthroplasty early dislocation rate. Clin Orthop Relat Res. 2007;465:155–158. doi: 10.1097/BLO.0b013e31815072e4. [DOI] [PubMed] [Google Scholar]
- 9.Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985;67:832–841. [PubMed] [Google Scholar]
- 10.Cuckler JM, Moore KD, Lombardi AV, Jr, McPherson E, Emerson R. Large versus small femoral heads in metal-on-metal total hip arthroplasty. J Arthroplasty. 2004;19:41–44. doi: 10.1016/j.arth.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Fenollosa J, Seminario P, Montijano C. Ceramic hip prostheses in young patients. Clin Orthop Relat Res. 2000;379:55–67. doi: 10.1097/00003086-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Cimbrelo E, Munuera L. Dislocation in low-friction arthroplasty. J Arthroplasty. 1992;7:149–155. doi: 10.1016/0883-5403(92)90008-E. [DOI] [PubMed] [Google Scholar]
- 13.Hamadouche M, Boutin P, Daussange J, Bolander ME, Sedel L. Alumina-on-alumina total hip arthroplasty: a minimum 18.5 year follow-up study. J Bone Joint Surg Am. 2002;84:69–77. [PubMed] [Google Scholar]
- 14.Hernigou P, Bahramy T. Zirconia and alumina ceramics in comparison with metal heads: polyethylene wear after a minimum ten year follow-up. J Bone Joint Surg Br. 2003;85:504–509. doi: 10.1302/0301-620X.85B4.13397. [DOI] [PubMed] [Google Scholar]
- 15.Hernigou P, Dupuy N, Pidet O, Homma Y, Flouzat Lachaniette CH. Alumina heads minimize wear and femoral osteolysis progression after isolated simple acetabular revision. Clin Orthop Relat Res. 2012 Apr 24 [Epub ahead of print]. PMID: 22528390. [DOI] [PMC free article] [PubMed]
- 16.Hernigou P, Filippini P, Flouzat-Lachaniette CH, Batista SU, Poignard A. Constrained liner in neurologic or cognitively impaired patients undergoing primary THA. Clin Orthop Relat Res. 2010;468:3255–3262. doi: 10.1007/s11999-010-1340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hernigou P, Intrator L, Bahrami T, Bensoussan A, Farcet JP. Interleukin 6 in the blood of patients with total hip arthroplasty without loosening. Clin Orthop Relat Res. 1999;366:147–154. doi: 10.1097/00003086-199909000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Hernigou P, Zilber S, Filippini P, Poignard A. Ceramic-ceramic bearing decreases osteolysis: a 20-year study versus ceramic-polyethylene on the contralateral hip. Clin Orthop Relat Res. 2009;467:2274–2280. doi: 10.1007/s11999-009-0773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kabo JM, Gebhard JS, Loren G, Amstutz H. In vivo wear of polyethylene acetabular component. J Bone Joint Surg Br. 1993;75:254–258. doi: 10.1302/0301-620X.75B2.8444946. [DOI] [PubMed] [Google Scholar]
- 20.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 21.Kummer FJ, Stuchin SA, Frankel VH. Analysis of removed Autophor ceramic-on-ceramic components. J Arthroplasty. 1990;5:28–33. doi: 10.1016/S0883-5403(06)80006-9. [DOI] [PubMed] [Google Scholar]
- 22.Lerouge S, Huk O, Yahia L. Ceramic-ceramic or metal-PE. A comparison of periprosthetic tissues from loosened total hip arthroplasty. J Bone Joint Surg Br. 1997;79:135–139. doi: 10.1302/0301-620X.79B1.6621. [DOI] [PubMed] [Google Scholar]
- 23.Lindberg HO, Carlsson AS, Gentz CF, Pettersson H. Recurrent and non-recurrent dislocation following total hip arthroplasty. Acta Orthop Scand. 1982;53:947–952. doi: 10.3109/17453678208992853. [DOI] [PubMed] [Google Scholar]
- 24.Lusty PJ, Watson A, Tuke MA, Walter WL, Walter WK, Zicat B. Orientation and wear of the acetabular component in third generation alumina-on-alumina ceramic bearings. J Bone Joint Surg Br. 2007;89:1158–1164. doi: 10.2106/JBJS.F.01466. [DOI] [PubMed] [Google Scholar]
- 25.Mai K, Hardwick ME, Walker RH, Copp SN, Ezzet KA, Colwell CW., Jr Early dislocation rate in ceramic-on-ceramic total hip arthroplasty. HSS J. 2008;4:10–13. doi: 10.1007/s11420-007-9060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meek RMD, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 27.Nevelos JE, Prudhommeaux F, Hamadouche M, Doyle C, Ingham E, Meunier A, Nevelos AB, Sedel L, Fisher J. Comparative analysis of two different types of alumina-alumina hip prosthesis retrieved for aseptic loosening. J Bone Joint Surg Br. 2001;83:598–603. [PubMed] [Google Scholar]
- 28.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Peters CL, McPherson E, Jackson JD, Erickson JA. Reduction in early dislocation rate with large-diameter femoral heads in primary total hip arthroplasty. J Arthroplasty. 2007;22:140–144. doi: 10.1016/j.arth.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 30.Refior JJ, Plitz W, Walter A. Ex vivo and in vitro analysis of the alumina/alumina bearing system for hip joint prostheses. Bioceramics. 1997;10:127–130. [Google Scholar]
- 31.Schuller HM, Marti RK. Ten-year socket wear in 66 hip arthroplasties. Ceramic versus metal heads. Acta Orthop Scand. 1990;61:240–243. doi: 10.3109/17453679008993508. [DOI] [PubMed] [Google Scholar]
- 32.Sedel L, Kerboull L, Christel P, Meunier A, Witvoiet J. Alumina-on-alumina hip replacement. Results and survivorship in young patients. J Bone Joint Surg Br. 1990;72:658–663. doi: 10.1302/0301-620X.72B4.2380223. [DOI] [PubMed] [Google Scholar]
- 33.Sedel L, Nizard R, Kerboull L, Witwoet J. Alumina-alumina hip replacement in patients younger than 50 years old. Clin Orthop Relat Res. 1994;298:175–183. [PubMed] [Google Scholar]
- 34.Sugano N, Nishii T, Nakata K, Masuhara K, Takaoka K. Polyethylene sockets and alumina ceramic heads in cemented total hip arthroplasty. A ten-year study. J Bone Joint Surg Br. 1995;77:548–556. [PubMed] [Google Scholar]
- 35.Urban JA, Garvin KL, Boese CK, Bryson L, Pedersen DR, Callaghan JJ, Miller RK. Ceramic-on-polyethylene bearing couples in total hip arthroplasty: seventeen to twenty-one-year results. J Bone Joint Surg Am. 2001;83:1688–1694. doi: 10.2106/00004623-200111000-00011. [DOI] [PubMed] [Google Scholar]
- 36.von Knoch M, Berry DJ, Harmsen WS, Morrey BF. Late dislocation after total hip arthroplasty. J Bone Joint Surg Am. 2002;84:1949–1953. doi: 10.2106/00004623-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Widmer KH, Ing D. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. doi: 10.1016/j.arth.2003.10.016. [DOI] [PubMed] [Google Scholar]