Abstract
Background
During the last two decades, uncemented fixation has been increasingly preferred worldwide during cup revision surgery. In Sweden, the number of uncemented cup revisions has been increasing during the last decade. However, it is unclear whether the risk of rerevision differs between cemented and uncemented cups.
Question/purposes
We determined (1) the risk of rerevision after cemented and uncemented fixation; (2) the influence of concomitant stem revision on the risk of rerevision of the cup; (3) the difference in risk of rerevision of an uncemented cup revision compared with liner revision only; and (4) whether the surgical incision influenced the risk of rerevision.
Methods
Between 1979 and 2010, 19,342 first-time cup revisions were reported to the Swedish Hip Arthroplasty Register. From these, 749 were excluded (hip resurfacing, cases with tumor diagnoses, and missing data) leaving 18,593 (73% cemented) for further analysis. We used a Cox regression model adjusted for age, sex, primary diagnosis, method of fixation, concomitant stem revision, and cemented/uncemented fixation to assess risk of rerevision.
Results
The relative risk for rerevision for any reason did not differ between cemented and uncemented fixation (relative risk [RR], 0.94). If the stem was not revised at index revision, the risk of further cup revision increased twofold (RR, 1.91). Liner revisions were associated with a 70% increased risk for rerevision of the cup as a result of any reason and especially because of dislocation (RR, 2.94). The surgical incision did not influence the overall risk for rerevision (direct lateral/posterolateral: RR, 1.02) or the risk of rerevision resulting from dislocation (RR, 0.91).
Conclusions
We found no difference in the overall risk of rerevision between cemented and uncemented fixation. Liner exchange had a higher risk for rerevision when compared with cases being rerevised with a new uncemented cup.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
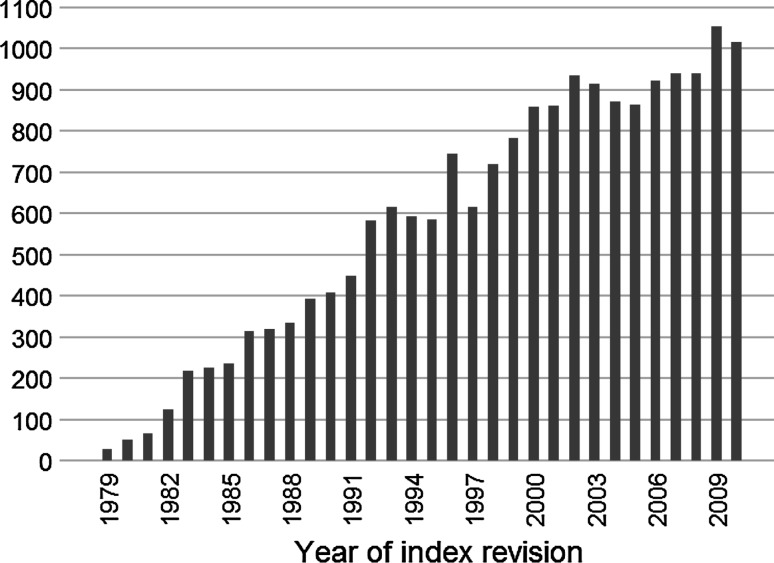
With an increasing number of elderly in the population and a growing number of primary hip arthroplasties being implanted, the prevalence of patients with THA will increase as will the need for revision hip arthroplasty. During the last two decades, the number of hip revision surgeries reported to the Swedish Hip Arthroplasty Register (SHAR) has increased twofold (Fig. 1). According to Kurtz et al. [21], revision hip arthroplasties are projected to increase twofold by 2030. Cemented fixation when revising the cup and the stem was common until the mid-1980s [32]. A high rate of failure for this technique (16%–48% at 4.5–11.9 years) [19, 20, 31] and a belief that the cement itself had a destructive effect on the bone tissue [7] encouraged the use of uncemented fixation in hip revision surgery [8, 12, 22]. The reported long-term survival after cup revision surgery, regardless of method of fixation, varies considerably in different publications [8, 10, 12, 15, 18–20, 22, 27, 29–31, 34, 36, 37, 39]. This discrepancy is in part related to time of followup but is undoubtedly also influenced by other variables (Table 1). In a publication from the Norwegian Arthroplasty Register, the authors report a reduced risk of failure for uncemented revisions both with (relative risk [RR], 0.66; 95% confidence interval [CI], 0.43–0.99) and without (RR, 0.37; 95% CI, 0.22–0.61) allograft [25]. However, the followup in this study was 3 to 5 years.
Fig. 1.
The graph shows an increasing number of revisions reported to the Swedish Hip Arthroplasty Register (SHAR) in 1979–2010.
Table 1.
Publications in cup revision surgery with minimum mean followup of 7 years
| Author | Publication year | Number of cup revisions | Mean age of patients (years; range) | Mean followup (years; range) | Reoperation rate* |
|---|---|---|---|---|---|
| Uncemented | |||||
| Della Valle et al. [8] | 2005 | 138 | 55 (20–79) | 17.1 (15–19.3) | 15.9% |
| Etienne et al. [12] | 2004 | 108 | 66 (39–93) | 7.1 (5–10) | 2.0% |
| Lachiewicz and Poon [22] | 1998 | 57 | 56 (22–82) | 7 (5–12) | 0% |
| Palm et al. [29] | 2007 | 87 | 67 (30–81) | 9 (7–11) | 9.5% |
| Park et al. [30] | 2009 | 138 | 50 (20–79) | 21.3 (20–24) | 15.2% |
| Cemented | |||||
| Engelbrecht et al. [10] | 1990 | 138 | 59 (25–85) | 7.4 (3–15.5) | 8.8% |
| Garcia-Cimbrelo et al. [15] | 1995 | 148 | 59 (22–82) | 11.5(0.1–20) | 12.8% |
| Hultmark et al. [18] | 2003 | 46 | 63 (22–75) | 10.7 (0.5–16.3) | 6.5% |
| Marti et al. [27] | 1990 | 60 | 71 (26–86) | 8.9 (5–14) | 13.00% |
| Pellici et al. [31] | 1985 | 99 | 64 (29–89) | 8.1 (5–12.5) | 19.0% |
| Schreurs et al. [34] | 2009 | 62 | 59 (23–82) | 22.2 (20–25) | 21.0% |
| Strömberg and Herberts [37] | 1996 | 53 | 47 (29–55) | 7 (4–11) | 15.1% |
| Van Haaren et al. [39] | 2007 | 71 | 69 (33–91) | 7.2 (1.6–9.7) | 35.0% |
| Current study | |||||
| Uncemented cups | 5067 | 67 (20–94) | 6.3 (0–27) | 15.1% | |
| Cemented cups | 13,526 | 71 (17–101) | 8.1 (0–32) | 15.8% | |
* Calculated by dividing all rerevisions (regardless of reason) with the number of hips included.
Because there is a variance in the literature concerning the long-term survival in cup revision surgery, based on method of fixation, and no published studies comparing long-term survival in cemented versus uncemented first-time cup revisions, we decided to analyze data from the SHAR on all revisions reported to the same registry since 1979. We calculated the risk of rerevision based on (1) fixation method; (2) the influence of concomitant stem revision on the risk of rerevision of the cup; (3) risk of rerevision between first-time revision of an uncemented cup and revision of the liner only; and (4) if choice between a direct lateral or posterolateral incision had any effect on the risk of rerevision.
Patients and Methods
All units performing THA and revision arthroplasty in Sweden report to the SHAR. With primary THA, the register has a 100% compliance rate of reporting from hospitals in Sweden and a 98% completeness rate regarding number of surgeries performed in Sweden [16]. The compliance rate for reporting revisions/reoperations is 90% [35]. Revision cases have been reported in detail, including social security number, since the foundation of the SHAR in 1979. Reports of revision/reoperation procedures are validated by each hospital sending a copy of the case records to the SHAR for data extraction into the database. All patients entering the register are notified and are free to disclaim participation according to the Swedish Patient Data Act. The data in the SHAR are linked to the patients by a personal identification number given to each individual in Sweden at the time of birth and to immigrants after entry into Sweden. The date of death is retrieved by SHAR being linked to the population register administered by the Swedish Tax Agency. The end of this study was set to the end of December 2010. Rerevision in our analysis was defined as exchange of the cup or the liner. The study was approved by the local ethics committee (reference number 591-12).
Between 1979 and 2010, 19,342 first-time cup revisions in 17,999 patients had been reported to the SHAR. The cases with missing data (n = 297) and two-stage revisions were removed (n = 391). Furthermore, cases in which hip resurfacings or tumor prostheses had been used, during the index revision (n = 61), were excluded leaving 18,593 cases. From the Register we extracted the following data: sex; age at revision; primary diagnosis; method of fixation of the cup in previous hip surgery; the fixation method of the revision cup; and components revised at index revision (Table 2). At the index revisions, there were 10,008 (54%) women and 8585 (46%) men. The most common primary diagnosis was primary osteoarthritis (75%) followed by inflammatory arthritis (9%) and status postfracture (7%). The mean age at the time of index revision was 70 years (range, 17–101 years) and this procedure was performed after a mean of 10 years (range, 0–31 years) after the primary operation. In 73% (13,526 first-time cup revisions), cemented fixation had been used and in the remaining 5067 cases (27%), the cup was uncemented.
Table 2.
Demography of patients reported to the Swedish Hip Arthroplasty Register
| Demographic | Cemented | Uncemented | p value | Liner revision | Uncemented§ | p value |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Female/male (%) | 54.3/45.7 | 52.5/47.5 | 0.03‡ | 49.7/50.3 | 57.2/42.8 | 0.001‡ |
| Primary diagnosis | ||||||
| Primary/secondary arthritis (%) | 74.6/25.4 | 74.2/25.8 | 0.49‡ | 71.8/28.2 | 63.4/36.6 | < 0.001‡ |
| Age at index revision (years)* | 70.7 (17–101) | 66.6 (20–94) | < 0.001† | 60.8 (24–88) | 59.6 (20–87) | 0.03† |
| ± Stem revision (%) | 64.0/36.0 | 55.2/48.8 | < 0.001‡ | 42.4/56.6 | 31.6/68.4 | < 0.001‡ |
| Followup (years)* | 8.1 (0–31.9) | 6.3 (0–27.1) | < 0.001† | 5.7 (0–18.8) | 7.3 (0–25.6) | < 0.001† |
| Total number of revisions | 13526 | 5067 | 928 | 906 | ||
* Mean (minimum-maximum); †t-test; ‡Mann-Whitney U-test; §failed primary uncemented cup revised with an uncemented cup.
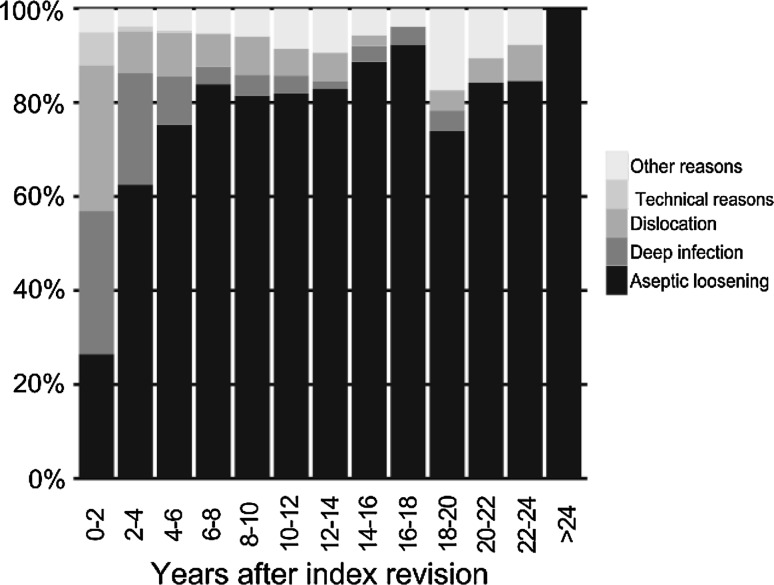
The followup started the day after the index operation and continued until revision, death, or December 31, 2010. The minimum followup was 0 years (mean, 7.6 years; range, 0–32 years). Patients with followup shorter than 2 years were thus included, also to account for early complications. The mean time from the index revision to any second revision was 6.4 years (range, 0–26 years). During the first 2 years after the first revision, the most common cause for a rerevision was dislocation followed by infection, aseptic loosening, technical failures, and other reasons. During the remaining part of the followup period, the main reason for a second revision was aseptic loosening (Fig. 2). In 62% (n = 11,457), the stem was also revised at the index revision. There were 928 liner revisions. Information about incision used at the index operation was recorded in 15,196 cases. One of three general approaches was used: 8350 a posterolateral approach, 5998 a direct lateral transgluteal approach with the patient in the lateral or supine position, and 848 various transtrochanteric approaches.
Fig. 2.
The graph shows changes in the relative percentages of indications for the second revision in first-time cup revisions reported to SHAR in 1979–2010. Infections and dislocation as causes decreased, whereas the proportion of patients with aseptic loosening increased.
In the cemented group, there were more women (cemented/uncemented cup at index operation: 54.3%/52.5%, p = 0.03) (Table 2). The mean age at index revision was higher (70.7 [17–101]/66.6 [20–94] years, p < 0.001) and the mean followup was almost 2 years longer (8.1 [0–31.9]/6.3 [0–27.1] years, p < 0.001) than in the uncemented group. Concomitant stem revision at the index procedure was also more common in the cemented group (64.0%/55.3%, p < 0.001) (Table 2). Demographic data for the liner revisions and the group of uncemented cup revision used for comparison are presented (Table 2).
The outcome of liner revisions was compared with those cases in which an uncemented cup had been exchanged to a new uncemented cup at the index revision (n = 906).
Kaplan-Meier analysis, with life tables, was used to compare the survival rate in cemented and uncemented first-time cup revision. As a result of differences in demographic data between groups and to compensate for these covariates, a Cox regression analysis adjusted for age at revision surgery (categorized into five groups: 40–49, 50–59, 60–69, 70–79, and > 80 years), sex, primary diagnosis (two categories: primary and secondary arthritis), method of fixation in primary surgery (two categories: cemented and uncemented), concomitant stem revision or not, and cemented/uncemented fixation at index revision was performed. To compare the liner exchanges with uncemented cup revisions, another Cox regression was applied; in this model, the same covariates mentioned earlier were used but because the primary fixation method in both groups was uncemented, the method of fixation was not included. A third Cox regression model (adjusted for covariates mentioned earlier) was used to evaluate the influence of the two most commonly used incisions: direct lateral (with the patient supine or on the side) or posterolateral. Incisions including trochanteric osteotomy were comparatively few, were not performed in a similar manner, and were mainly used during the early period of this study. They were therefore excluded from this analysis.
All calculations were performed using IBM SPSS Statistics, Version 20 (IBM Corp, Somers, NY, USA). The proportional hazard assumption was controlled by computing and plotting the Schoenfeld residuals for each covariate using the survival and graphic packages in R statistics [1, 13, 33]. The cumulative survival and histogram graphs were created with the graphics package in R statistics.
Results
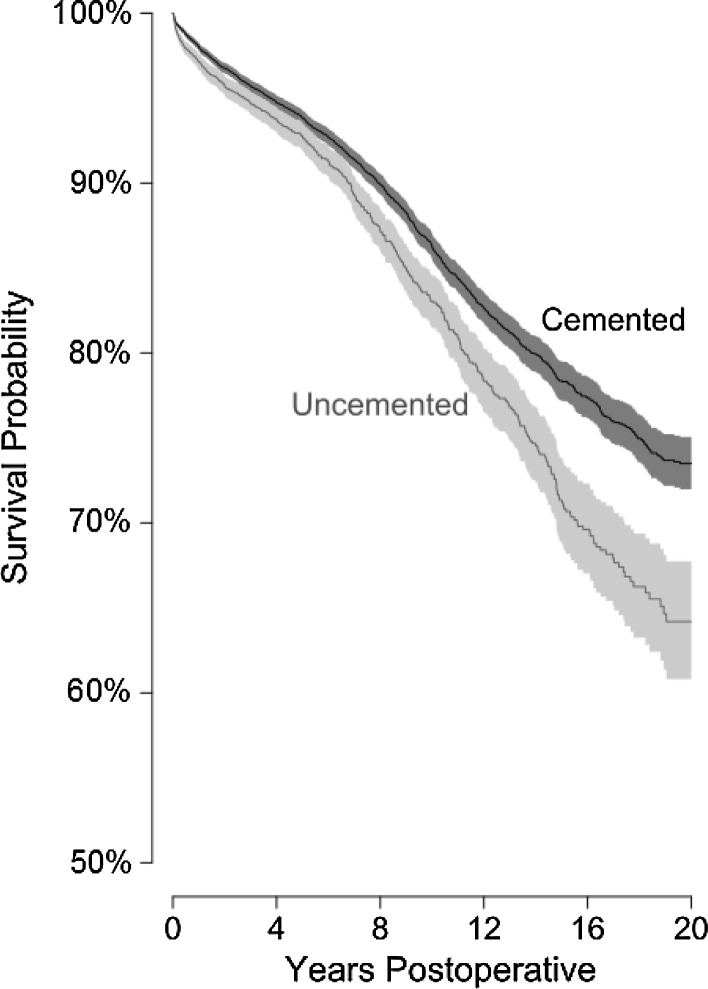
The unadjusted cumulative survival rate in the cemented group was higher (p < 0.001, log-rank test) than in the uncemented group both at 10 years (84.4% versus 80.8%) and at 20 years (72.8% versus 60.2%) (Fig. 3). Using rerevision of the cup or liner, as a result of any reason, as the end point, we found an increased risk with decreasing age (Table 3). In patients 49 years of age and younger, the relative risk was 2.5 times higher (RR, 2.51; p < 0.001) than in the reference group (70–79 years). Hips in which a primary cemented cup had been used had a higher risk (RR, 1.14; p = 0.02) of being rerevised. Male sex was associated with increased risk (RR, 1.16; p < 0.001) of rerevision. Diagnosis at the primary operation did not influence the risk for a second revision. The choice between a cemented or uncemented revision cup had no influence on the risk (cemented/uncemented: RR, 0.94; p = 0.19) for a second cup revision. Cemented cups had, however, a slightly increased risk (RR, 1.14; p = 0.04) (Table 4) to become revised as a result of loosening or osteolysis after adjustment for the same covariates as in the previous analysis. On the other hand, the cemented cups were less likely to become rerevised (RR, 0.51; p < 0.001) (Table 4) if dislocation was used as an end point.
Fig. 3.
Twenty-year crude cumulative survival probability in cemented and uncemented first-time cup revisions with 95% confidence interval (shadows) is shown.
Table 3.
Risk factors for rerevision of the cup or liner as a result of any reason, all causes (Cox regression analysis)
| Risk factor | RR | 95% CI | p value |
|---|---|---|---|
| Sex | |||
| Female* | 1 | ||
| Male | 1.16 | 1.07–1.27 | < 0.001 |
| Age (years) | |||
| 0–49 | 2.51 | 2.16–2.93 | < 0.001 |
| 50–59 | 2.24 | 1.97–2.55 | < 0.001 |
| 60–69 | 1.51 | 1.35–1.69 | < 0.001 |
| 70–79* | 1 | ||
| 80+ | 0.69 | 0.57–0.83 | < 0.001 |
| Primary diagnosis | |||
| Primary osteoarthritis* | 1 | ||
| Secondary osteoarthritis† | 1.03 | 0.94–1.14 | 0.50 |
| Extracted cup | |||
| Uncemented* | 1 | ||
| Cemented | 1.14 | 1.02–1.27 | 0.02 |
| Fixation at index revision | |||
| Uncemented* | 1 | ||
| Cemented | 0.94 | 0.85–1.03 | 0.19 |
| Components revised at index revision | |||
| Cup/liner + stem*,‡ | 1 | ||
| Cup/liner | 1.91 | 1.75–2.09 | < 0.001 |
* Reference; †primary osteoarthritis (74%), inflammatory hip disease (9%), fracture (7%), sequelae after childhood disease (6%), avascular necrosis (2%), and others (2%); ‡ components revised at index revision; RR = relative risk; CI = confidence interval.
Table 4.
Risk of rerevision in cemented and uncemented first time cup revisions*
| End point in the analysis | Total number of revisions | Number of revisions | RR | 95% CI | p value |
|---|---|---|---|---|---|
| Any reason for rerevision | 18,593 | 2250 | |||
| Cemented revision cup | 13,526 | 1622 | 0.94 | 0.85–1.03 | 0.19 |
| Uncemented revision cup† | 5067 | 628 | 1 | – | – |
| Aseptic loosening | 18,593 | 1446 | |||
| Cemented revision cup | 13,526 | 1082 | 1.14 | 1.00–1.29 | 0.04 |
| Uncemented revision cup† | 5067 | 364 | 1 | – | – |
| Infection | 18,593 | 321 | |||
| Cemented revision cup | 13,526 | 234 | 0.92 | 0.71–1.19 | 0.51 |
| Uncemented revision cup† | 5067 | 87 | 1 | – | – |
| Dislocation | 18,593 | 307 | |||
| Cemented revision cup | 13,526 | 182 | 0.51 | 0.40–0.66 | < 0.001 |
| Uncemented revision cup† | 5067 | 125 | 1 | – | – |
| Other reasons | 18,593 | 176 | |||
| Cemented revision cup | 13,526 | 154 | 0.65 | 0.51–0.83 | 0.005 |
| Uncemented revision cup† | 5067 | 22 | 1 | – | – |
* Cox regression analysis adjusted for age, sex, primary diagnosis, type of fixation in prior hip surgery, components revised, and method of fixation with end point as indicated; †reference; RR = relative risk; CI = confidence interval.
The risk for a second revision resulting from any reason increased if the stem had not been revised at the index revision (RR, 1.91; p < 0.001). This increase was above all caused by a greater risk of further cup or liner revision resulting from dislocation (RR, 2.86; p < 0.001) and less so as a result of aseptic loosening (RR, 1.65; p < 0.001).
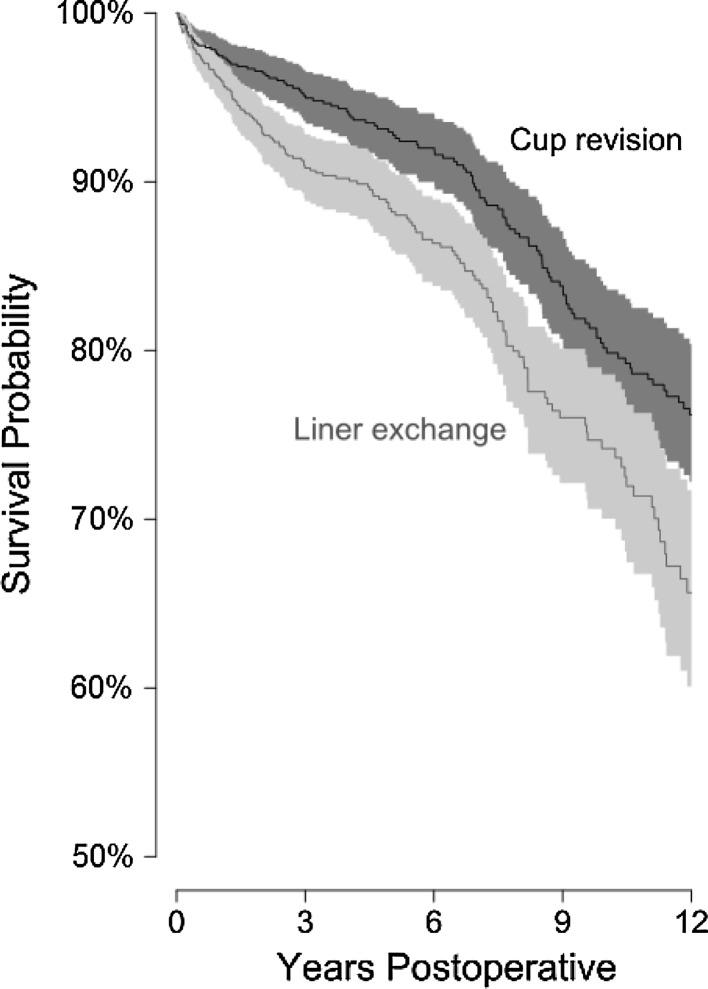
The unadjusted cumulative survival rates at 10 years in the uncemented to uncemented and the liner revision groups were 79.2% ± 3.81% and 72.0% ± 4.74%, respectively (Fig. 4). Adjusting for covariates in a Cox regression model showed that liner exchange resulted in an increased risk (RR, 1.70; p < 0.001) for a second revision of the cup or liner. This risk became even higher (RR, 2.94; p < 0.001) if revision resulting from dislocation was used as the end point (Table 5).
Fig. 4.
Twelve-year crude cumulative survival probability after first-time liner exchange and uncemented to uncemented cup revisions with 95% confidence interval (shadows) is illustrated.
Table 5.
Risk factors for rerevision of the cup or liner as a result of any reason versus dislocation, comparison between liner exchange and uncemented with uncemented cup revision (Cox regression analysis)
| Risk factor | Rerevision, all causes | Rerevision as a result of dislocation | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p value | RR | 95% CI | p value | |
| Sex | ||||||
| Female* | 1 | 1 | ||||
| Male | 1.06 | 0.84–1.33 | 0.64 | 0.93 | 0.57–1.53 | 0.78 |
| Age (years) | ||||||
| 0–49 | 2.52 | 1.48–4.31 | 0.001 | 1.75 | 0.67–4.57 | 0.25 |
| 50–59 | 2.21 | 1.34–3.66 | 0.002 | 1.35 | 0.57–3.24 | 0.50 |
| 60–69 | 1.66 | 1.00–2.75 | 0.05 | 1.24 | 0.53–2.90 | 0.61 |
| 70–79* | 1 | 1 | ||||
| 80+ | 1.90 | 0.44–8.2 | 0.39 | 2.32 | 0.28–18.9 | 0.43 |
| Primary diagnosis | ||||||
| Primary osteoarthritis* | 1 | 1 | ||||
| Secondary osteoarthritis† | 0.90 | 0.70–1.17 | 0.43 | 0.79 | 0.44–1.41 | 0.43 |
| Components revised at index revision | ||||||
| Cup/liner + stem* | 1 | 1 | ||||
| Cup/liner | 1.65 | 1.29–2.12 | < 0.001 | 2.86 | 1.55–5.29 | < 0.001 |
| Components revised at index revision | ||||||
| Cup* | 1 | 1 | ||||
| Liner | 1.70 | 1.34–2.14 | < 0.001 | 2.94 | 1.72–5.03 | < 0.001 |
* Reference; †primary osteoarthritis (68%), sequelae after childhood disease (15%), inflammatory hip disease (8%), avascular necrosis (5%), fracture (3%), and others (1%); RR = relative risk; CI = confidence interval.
The choice of direct lateral or posterolateral incision used at the index revision did not influence the overall risk for a second revision as a result of any reason (direct lateral/posterolateral: RR, 1.02; p = 0.68) or the risk of rerevision resulting from dislocation (RR, 0.91; p = 0.49).
Discussion
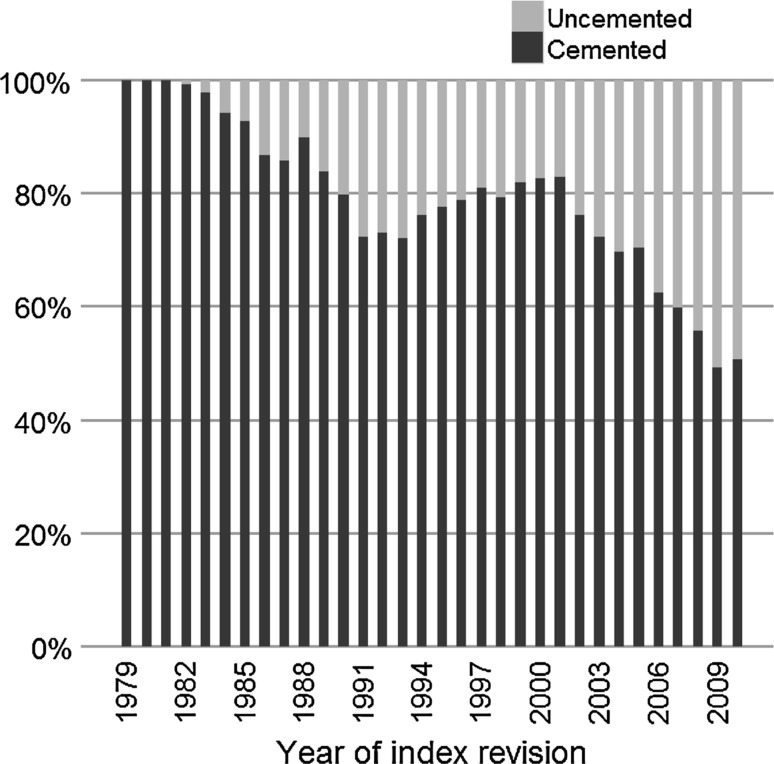
Between 1979 and 1999, approximately 81% of the first-time cup revisions in Sweden were cemented. Reports on low survival rates for the cemented cup revisions, encouraging studies of uncemented cups of press-fit design, and lack of sufficiently well-performed comparisons between cemented and uncemented cup revisions have stimulated an increasing use of the uncemented technique in revision surgery also in Sweden (Fig. 5; Table 6). The main purpose of this study was to evaluate differences in the rerevision rate concerning method of fixation in cup revision surgery by analyzing data on first-time cup revisions reported to SHAR during 1979 to 2010. Furthermore, the influence of concomitant stem revision was evaluated and a comparison between liner exchange and revision with a new uncemented cup was done. In a subpopulation of the material, we also studied if the choice between direct lateral and posterolateral incision had any effect on the rate of rerevision.
Fig. 5.
The graph shows the distribution of cemented and uncemented cups, used at first-time cup revisions, reported to SHAR between 1979 and 2010. There was a decreasing percentage of cemented revisions over time.
Table 6.
Most frequently used cups at index revision, liner exchanges excluded
| Cups | Frequency | Percent | Revision year |
|---|---|---|---|
| Cemented cups | |||
| Lubinus (Link, W. Link, Germany) | 3154 | 23.3% | 1979–2010 |
| Charnley* | 2426 | 17.9% | 1979–2010 |
| Charnley Elite* | 1305 | 9.6% | 1990–2010 |
| Exeter Duration* | 989 | 7.3% | 1999–2010 |
| Exeter* | 965 | 7.1% | 1982–2009 |
| Müller* | 850 | 6.3% | 1980–2010 |
| Exeter Polished (Stryker, Newbury, UK) | 755 | 5.6% | 2000–2010 |
| Reflection (Smith & Nephew, Memphis, TN, USA) | 384 | 2.8% | 1991–2010 |
| OPTICUP* | 367 | 2.7% | 1994–2007 |
| Lubinus FAL (Link, W. Link, Germany) | 353 | 2.6% | 1999–2010 |
| Scan Hip Cup* | 341 | 2.5% | 1985–1999 |
| ZCA All-Poly (Zimmer, Warsaw, IN, USA) | 331 | 2.4% | 1994–2010 |
| Others† | 1305 | 9.6% | 1979–2010 |
| Total | 13,525 | ||
| Uncemented cups | |||
| Trilogy HA (Zimmer) | 1570 | 38.0% | 1995–2010 |
| TMT (Zimmer) | 523 | 12.6% | 2006–2010 |
| Mallory-Head (Zimmer) | 312 | 7.5% | 1992–2010 |
| Trident HA (Stryker Orthopaedics, Mahwah, NJ, USA) | 226 | 5.5% | 1994–2010 |
| Romanus* | 220 | 5.3% | 1989–2006 |
| Harris-Galante I* | 158 | 3.8% | 1986–1993 |
| Harris-Galante II* | 149 | 3.6% | 1990–1999 |
| ABG (Howmedica, Staines, UK) | 133 | 3.2% | 1991–2008 |
| PCA* | 118 | 2.9% | 1984–1998 |
| Others† | 727 | 17.6% | 1979–2010 |
| Total | 4136 | ||
* No longer marketed in Sweden; †cups used in less than 2% of revisions in each group.
We recognize the following limitations to this study. First, our analysis included patients operated on during a time period when old cemented and uncemented cup designs, now abandoned because of higher revision risk resulting from loosening, wear, or regarding uncemented designs with unfavorable locking mechanisms, were used [11, 38]. This will probably be reflected in the results of both cemented and uncemented cup revisions analyzed in this study. Second, the cementing techniques used during the early 1980s had not gone through the evolution resulting in the standards of today [28], which should be considered when analyzing the survival rates in cemented cup revisions. Our results reflect the outcome of techniques used when data on each of the first-time revisions were entered into the register without any specific selection. Thus, our results correspond to those of the surgical techniques and implants selected in Sweden during the time period studied. The majority of these techniques and implants were used internationally but with varying proportionality and time for introduction between countries. The implant selection in Sweden is characterized by a high share of cemented fixation. On the other hand, the total number of uncemented cups in our study was still sufficiently high for a relevant comparison. Despite that Swedish surgeons from a historical perspective have preferred cement, the relative share of cementless fixation has increased in primary cases [16] and revisions (Fig. 5). During 2010, almost 50% of all cups in first-time revisions were uncemented. More than 50% of the uncemented and cemented revision cups in our study were performed in nine and 15 hospitals, respectively, as an effect of centralization of these procedures. This observation suggests that surgeons familiar with revision surgery performed the majority of the revisions and especially those with use of an uncemented cup. Third, our analysis included all grafted cases. In the study by Lie et al. [25], bone grafting had a negative influence on the survival of uncemented cups. In the SHAR, only the use of bone graft or not is recorded, but there is no certain information about the volume of graft used. Thus, we could not separate between impaction grafting and cases in which minor osteolysis had been filled with graft and therefore decided not to include this variable in the analysis. Fourth, our study was restricted to first-time revisions, which most certainly will exclude many difficult cases with severe bone defects but definitely not all of them. Existence of a severe bone defect might influence the survival of the cup in revision surgery. However, because there is an ongoing debate in the literature concerning the optimal method of fixation in the presence of bone defects [6, 14, 17, 23, 34], we do not believe Swedish surgeons specifically prefer either of these methods to treat bone defects and therefore the last two reflections should not influence the results in our study.
According to our observations, there was no difference in overall survival when comparing cemented and uncemented fixation in first-time cup revisions. Contrary to our findings, a Norwegian Arthroplasty Register study showed higher rerevision rates in cemented cup revisions [25]. This discrepancy could perhaps partly be explained by certain differences in demographic data; in the Norwegian study, there were more women and the age at revision was lower compared with our study. However, other factors such as the different time periods analyzed are likely of greater importance. According to our analysis, uncemented designs are superior to the cemented in regard to fixation. This difference was moderate in our analysis, probably because old designs including screw rings with a smooth surface and press-fit designs with poor liner locking mechanisms were included. The advances made in contemporary uncemented cup designs with improved liner fixation and wear resistance will probably influence the long-term survival. Loosening and osteolysis may become a less common problem in the new design, but this hypothesis remains to be confirmed. The inferior survival for the uncemented cups, when dislocation was used as the end point, could depend on various new uncemented cup designs being introduced during the last decade and the low volume of each uncemented cup being inserted by single revision surgeons in Sweden. On the other hand, an increased revision rate resulting from dislocation has also been observed in Sweden for primary uncemented cups [16], which could indicate an inherent problem to obtain an optimum position of the cup in at least some of these designs.
We found no studies comparing isolated cup revision with a total revision. In our analysis, the revision of both the stem and the cup at the index operation resulted in reduced risk of further revisions compared with revision of the cup only regardless of the reason for a second revision. The explanation for this discrepancy is not known but might be the result of better biomechanical stability being achieved when both components have been exchanged during the index revision. In cases in which only the cup was revised, it is most probable that the stem was well fixed. Revision of a well-fixed stem is associated with various degrees of complications and morbidities. Thus, this finding is difficult to transform to a general clinical recommendation without taking all risk factors into consideration.
Our data are consistent with the findings in the Norwegian register and other studies [2–5, 9, 24] showing an increased risk for a second revision if solely the liner is exchanged. The increased rerevision rate after liner exchange could partly depend on difficulties to address osteolysis during the index revision. We could, however, not further explore this issue because in the SHAR, revisions mainly performed as a result of osteolysis are often recorded as loosening resulting from difficulties in extracting correct information from the case records in these cases. Our finding that liner revisions were not associated with increased rerevision resulting from loosening does not support that loosening/osteolysis was the main problem, but rather a problem related to insufficient joint stability at the index revision. One might speculate that an artificial joint susceptible to accelerated wear has a certain amount of biomechanical imbalance and thus cases revised with liner exchange, resulting from wear, represent a selection of revisions with an increased risk of dislocation.
In a previous study from the Swedish Hip Arthroplasty Register [26], Lindgren et al. found that the risk of revision using direct lateral or posterolateral incision varied between different designs of primary THAs. Interestingly, we found no certain difference between these two approaches in first-time cup revisions. This observation might include a certain amount of bias; a wide variation of designs and cup/stem combinations with different head sizes were included and we had no information about any use of hooded or constrained liners and other types of measures to reduce the risk of dislocation in different groups. However, considering the large number of cases in this study, our observation suggests that the choice of any of these two approaches could be left to the preference of the surgeon.
Different techniques have been suggested in cup revision surgery [32] and the revision surgeon must be familiar with several approaches to cover all types of patients and bone defects. In the absence of comparative studies, observational studies might be able to act as guidance to the orthopaedic surgeons in decision-making. Our study does not favor uncemented nor cemented fixation of the cup in first-time revisions and does not provide information concerning the influence of various amounts of bone grafting used with either of the two alternatives. It does, however, illustrate that cemented fixation is a reasonable alternative provided the surgeon is familiar with the technique. Although limitations exist in observational studies, with including more than 18,000 first-time cup revisions, we are able to conclude that (1) there are no differences in the overall risk for a second revision based on method of fixation in cup revisions surgery; (2) the risk of rerevision is decreased when the stem is revised concomitantly; that (3) there is a two- to threefold increase for a second revision influence when solely the liner is exchanged; and (4) the choice of direct lateral or posterolateral incision did not alter the risk of rerevision of the cup after a first-time cup revision. Further studies and followups are needed to investigate the performance of contemporary cups used in revision surgery and the influence of bone defects related to the type of fixation chosen.
Acknowledgments
We thank the Swedish Orthopaedic surgeons, the secretaries at the individual hospitals, and the local staff at the Swedish Hip Arthroplasty Register who, by reporting and compiling data for more than three decades, made this study possible.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abeysekera W, Sooriyarachchi M. Use of Schoenfeld’s global test to test the proportional hazards assumption in the cox proportional hazards model: an application to a clinical study. J Natl Sci Found Sri Lanka. 2009;37:41–51. [Google Scholar]
- 2.Beaulé PE, Ebramzadeh E, LeDuff M, Prasad R, Amstutz HC. Cementing a liner into a stable cementless acetabular shell: the double-socket technique. J Bone Joint Surg Am. 2004;86:929–934. doi: 10.2106/00004623-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Biviji AA, Ezzet KA, Pulido P, Colwell CW. Modular femoral head and liner exchange for the unstable total hip arthroplasty. J Arthroplasty. 2009;24:625–630. doi: 10.1016/j.arth.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 4.Boucher HR, Lynch C, Young AM, Engh CA, Engh C. Dislocation after polyethylene liner exchange in total hip arthroplasty. J Arthroplasty. 2003;18:654–657. doi: 10.1016/S0883-5403(03)00266-3. [DOI] [PubMed] [Google Scholar]
- 5.Carter AH, Sheehan EC, Mortazavi SMJ, Purtill JJ, Sharkey PF, Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;26:46–52. doi: 10.1016/j.arth.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 6.Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular revision surgery with impacted bone allografts and cemented cups in patients younger than 55 years. Int Orthop. 2009;33:611–616. doi: 10.1007/s00264-007-0503-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dahl OE, Garvik LJ, Lyberg T. Toxic effects of methylmethacrylate monomer on leukocytes and endothelial cells in vitro. Acta Orthop. 1994;65:147–153. doi: 10.3109/17453679408995423. [DOI] [PubMed] [Google Scholar]
- 8.Della Valle CJ, Shuaipaj T, Berger RA, Rosenberg AG, Shott S, Jacobs JJ, Galante JO. Revision of the acetabular component without cement after total hip arthroplasty: A concise follow-up, at fifteen to nineteen years, of a previous report. J Bone Joint Surg Am. 2005;87:1795–1800. doi: 10.2106/JBJS.D.01818. [DOI] [PubMed] [Google Scholar]
- 9.Earll MD, Fehring TK, Griffin WL, Mason JB, McCoy T, Odum S. Success rate of modular component exchange for the treatment of an unstable total hip arthroplasty. J Arthroplasty. 2002;17:864–869. doi: 10.1054/arth.2002.34823. [DOI] [PubMed] [Google Scholar]
- 10.Engelbrecht D, Weber F, Sweet M, Jakim I. Long-term results of revision total hip arthroplasty. J Bone Joint Surg Br. 1990;72:41. doi: 10.1302/0301-620X.72B1.2298793. [DOI] [PubMed] [Google Scholar]
- 11.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop. 2006;77:57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- 12.Etienne G, Bezwada HP, Hungerford DS, Mont MA. The incorporation of morselized bone grafts in cementless acetabular revisions. Clin Orthop Relat Res. 2004;428:241. doi: 10.1097/01.blo.0000145889.94276.61. [DOI] [PubMed] [Google Scholar]
- 13.Fox J. Cox proportional-hazards regression for survival data. 2011. SAGE Publications, Inc. Available at: http://socserv.mcmaster.ca/jfox/books/companion/appendix/Appendix-Cox-Regression.pdf. Accessed October 7, 2012.
- 14.Garcia-Cimbrelo E, Cruz-Pardos A, Garcia-Rey E, Ortega-Chamarro J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin Orthop Relat Res. 2010;468:3304–3313. doi: 10.1007/s11999-010-1395-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia-Cimbrelo E, Munuera L, Diez-Vazquez V. Long-term results of aseptic cemented Charnley revisions. J Arthroplasty. 1995;10:121–131. doi: 10.1016/S0883-5403(05)80118-4. [DOI] [PubMed] [Google Scholar]
- 16.Garellick G, Kärrholm J, Rogmark C, Herberts P. The Swedish Hip Arthroplasty Register, Annual Report 2010. 2011. Department of Orthopaedics, Sahlgrenska University Hospital. Available at: http://www.shpr.se/Libraries/Documents/AnnualReport-2010-2-eng.sflb.ashx. Accessed October 1, 2012.
- 17.Gross AE. Restoration of acetabular bone loss 2005. J Arthroplasty. 2006;21:117–120. doi: 10.1016/j.arth.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Hultmark P, Kärrholm J, Strömberg C, Herberts P. Cemented first-time revision using Charnley cups: clinical outcome after 7 to 15 years follow-up. J Arthroplasty. 2003;18:999–1004. doi: 10.1016/S0883-5403(03)00404-2. [DOI] [PubMed] [Google Scholar]
- 19.Katz RP, Callaghan JJ, Sullivan PM, Johnston RC. Long-term results of revision total hip arthroplasty with improved cementing technique. J Bone Joint Surg Br. 1997;79:322–326. doi: 10.1302/0301-620X.79B2.7245. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh F, Ilstrup DM, Fitzgerald RH., Jr Revision total hip arthroplasty. Clin Orthop Relat Res. 1985;193:133–140. [PubMed] [Google Scholar]
- 21.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 22.Lachiewicz PF, Poon ED. Revision of a total hip arthroplasty with a Harris-Galante porous-coated acetabular component inserted without cement. A follow-up note on the results at five to twelve years. J Bone Joint Surg Am. 1998;80:980–984. doi: 10.2106/00004623-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Lakstein D, Backstein D, Safir O, Kosashvili Y, Gross AE. Trabecular Metal™ Cups for acetabular defects with 50% or less host bone contact. Clin Orthop Relat Res. 2009;467:2318–2324. doi: 10.1007/s11999-009-0772-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lie S, Hallan G, Furnes O, Havelin L, Engesaeter L. Isolated acetabular liner exchange compared with complete acetabular component revision in revision of primary uncemented acetabular components. A study of 1649 revisions from the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2007;89:591–594. doi: 10.1302/0301-620X.89B5.18623. [DOI] [PubMed] [Google Scholar]
- 25.Lie SA, Havelin LI, Furnes ON, Engesæster LB, Vollset SE. Failure rates for 4762 revision total hip arthroplasties in the Norwegian arthroplasty register. J Bone Joint Surg Br. 2004;86:504–509. [PubMed] [Google Scholar]
- 26.Lindgren V, Garellick G, Kärrholm J, Wretenberg P. The type of surgical approach influences the risk of revision in total hip arthroplasty. Acta Orthop. 2012;83:1–7. doi: 10.3109/17453674.2012.742394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marti RK, Schüller H, Besselaar PP, Vanfrank HEL. Results of revision of hip arthroplasty with cement. A five to fourteen-year follow-up study. J Bone Joint Surg Am. 1990;72:346. [PubMed] [Google Scholar]
- 28.Mulroy R, Harris W. The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Joint Surg Br. 1990;72:757–760. doi: 10.1302/0301-620X.72B5.2211749. [DOI] [PubMed] [Google Scholar]
- 29.Palm L, Jacobsson S-A, Kvist J, Lindholm A, Öjersjö A, Ivarsson I. Acetabular revision with extensive allograft impaction and uncemented hydroxyapatite-coated implants. Results after 9 (7–11) years follow-up. J Arthroplasty. 2007;22:1083–1091. doi: 10.1016/j.arth.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 30.Park DK, Della Valle CJ, Quigley L, Moric M, Rosenberg AG, Galante JO. Revision of the acetabular component without cement. A concise follow-up, at twenty to twenty-four years, of a previous report. J Bone Joint Surg Am. 2009;91:350–355. doi: 10.2106/JBJS.H.00302. [DOI] [PubMed] [Google Scholar]
- 31.Pellicci PM, Wilson PD, Sledge C, Salvati E, Ranawat C, Poss R, Callaghan J. Long-term results of revision total hip replacement. J Bone Joint Surg Am. 1985;67:513. [PubMed] [Google Scholar]
- 32.Pulido L, Rachala S, Cabanela M. Cementless acetabular revision: past, present, and future. Int Orthop. 2011;35:289–298. doi: 10.1007/s00264-010-1198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.R: A Language and Enviroment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2010. [Google Scholar]
- 34.Schreurs B, Keurentjes J, Gardeniers J, Verdonschot N, Slooff T, Veth R. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component: a 20-to 25-year follow-up. J Bone Joint Surg Br. 2009;91:1148. doi: 10.2106/JBJS.G.01701. [DOI] [PubMed] [Google Scholar]
- 35.Söderman P, Malchau H, Herberts P, Zügner R, Regnér H, Garellick G. Outcome after total hip arthroplasty: Part II. Disease-specific follow-up and the Swedish National Total Hip Arthroplasty Register. Acta Orthop. 2001;72:113–119. doi: 10.1080/000164701317323345. [DOI] [PubMed] [Google Scholar]
- 36.Strömberg CN, Herberts P. A multicenter 10-year study of cemented revision total hip arthroplasty in patients younger than 55 years old: a follow-up report. J Arthroplasty. 1994;9:595–601. doi: 10.1016/0883-5403(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 37.Strömberg CN, Herberts P. Cemented revision total hip arthroplasties in patients younger than 55 years old: a multicenter evaluation of second-generation cementing technique. J Arthroplasty. 1996;11:489–499. doi: 10.1016/S0883-5403(96)80099-4. [DOI] [PubMed] [Google Scholar]
- 38.Thanner J, Kärrholm J, Malchau H, Herberts P. Poor outcome of the PCA and Harris-Galante hip prostheses: randomized study of 171 arthroplasties with 9-year follow-up. Acta Orthop. 1999;70:155–162. doi: 10.3109/17453679909011255. [DOI] [PubMed] [Google Scholar]
- 39.Van Haaren E, Heyligers I, Alexander F, Wuisman P. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg Br. 2007;89:296. doi: 10.1302/0301-620X.89B3.18080. [DOI] [PubMed] [Google Scholar]