Abstract
INTRODUCTION
Intraoral neurilemmomas (schwannoma) are rare, even rarer are intraosseous ones, and the rarest are the maxillary neurilemmomas. Going by the literature only 5 cases of maxillary neurilemomas are reported till now. Neurilemmomas are benign tumours of nerve sheath origin. Approximately 30% arise in head and neck region, of these 1–12% arise intraorally mainly involving tongue.
PRESENTATION OF CASE
Here we report two cases of maxillary neurilemmoma, one in a 9 year old girl and second one in a 27 year old female, both involving the lateral surface of maxilla on right side. Both the patients presented with a long standing history of swelling which was increasing gradually. 9-Year-old girl also had 1 lesion in the temporal region on right side and the 27-year-old patient had associated erosion of the soft palate. Diagnosis was made on the basis of histopathology and immunohistochemistry.
DISCUSSION
Neurilemmomas are slow growing benign tumour of the nerve sheath origin arising from the Schwann cells. Their aetiology is not known. Most common complaint is that of a gradually increasing swelling followed by pain and paresthesias. Surgery remains the treatment of choice with close follow up.
CONCLUSION
Maxillary neurilemmomas are rarest of the rare tumour which closely mimic benign odontogenic cysts and tumours, and should be kept in the differential diagnosis of these lesions. Knowledge of the radiologic and clinical behaviour of these tumours is extremely important for prompt diagnosis and treatment.
Keywords: Neurilemmoma, Intraoral, Maxillary, Intraosseous, Schwannoma
1. Introduction
Neurilemmoma also known as schwannoma is a benign tumour of nerve sheath origin arising from any nerve covered with a Schwann cell sheath, which include the cranial nerves (except for optic and olfactory), the spinal nerves and autonomic nervous system.1 They were first described by Verocay in 1910 who called it “neurinoma” then. In 1935, the term “neurilemmoma” was coined by Stout. The soft tissue of the head and neck region is one of the most common sites for benign nerve sheath tumours as well as the flexor surfaces of the extremities.2 Intraoral development is uncommon (only 1%). Most common site of occurrence is the tongue. In the current medical literature, there are 44 acceptable cases of intraosseous neurilemmomas of the jaw, 39 of the mandible and five in the maxilla, representing less than 1% of the primary tumours of the bones. Other sites reported include the sacrum, vertebra, clavicle, ribs, humerus, radius, ulna etc.3
2. Case report
2.1. Case 1
A nine year old girl presented with complaints of swelling involving the right upper jaw and right temporal region since six months with gradual increase in size. There was slight pain in the jaw swelling (Fig. 1).
-
•
Clinical examination revealed a diffuse mass 10 cm × 7 cm in the right side of maxilla in two parts, one associated with cheek and the other below the orbit and a 5 cm × 3 cm mass in the right temporal region which was slightly tender. Both masses were fixed to the underlying bone. Swelling was bulging inside oral cavity over the right gingivobuccal sulcus. There was no associated abnormality of vision or chewing.
-
•
CT scan was done followed by needle biopsy which confirmed the presence of spindle cell tumour. Total maxillectomy + excision of mass in temporal region + reconstruction by right temporalis muscle flap + nylon darning of orbital floor was done. Post operative course was uneventful.
-
•
Histopathological examination and immunohistochemistry confirmed the diagnosis.
Fig. 1.

Showing pre and intra-operative picture of 1st patient.
2.2. Case 2
A 27-year-old female with gradually increasing swelling in right upper jaw since one and a half year (Fig. 2).
-
•
On examination a large swelling of size 12 cm × 8 cm was present over the right side of face involving the underlying maxilla with a bulge inside the oral cavity.
-
•
After investigating thoroughly and reaching to the diagnosis, total maxillectomy was done completely removing the tumour. Post-operative course was uneventful.
-
•
Diagnosis was confirmed by histopathological examination and immunohistochemistry.
Fig. 2.

Showing pre and intra-operative picture of 2nd patient.
3. Discussion
Intraosseous neurilemmoma is of infrequent occurrence and an uncommon lesion. The mandible is the most common site.4 The incidence of the intraosseous neurilemmoma is less than 0.2% in primary bone tumours.5 This tumour presents as a painless, slow growing mass, and it may develop at any age ranging from 2 to 72 years. The peak prevalence occurs in the 2nd and 3rd decades of life with female predilection, with a ratio of 2:1 over males.4,6 44 cases of jaw neurilemmoma have been described by Chi et al., of which 39 were found involving mandible and only 5 involved maxilla. In this report only one case was younger than 10 years of age.4 Our first case was 9 years old at the time of surgery and she presented after six months from the onset of swelling.
As per the best of our research and going through the literature, our first case of a 9 year old girl is the first case in English literature presenting with two simultaneous neurilemmomas involving maxilla.
The tumour presents as an expansive growth pattern which may cause dislocation of teeth and may also involve the nerves.7 There is no pathognomonic radiological feature for intraosseous neurilemmoma although it shows a well defined, unilocular radiolucency with a thin sclerotic border.6
Our first case shows a large multilocular radiolucencies with tumour invading the maxillary antrum and floor of the orbit (Figs. 3 and 4).There are three mechanism by which neurilemmomas may involve a bone
-
1.
A tumour may arise centrally within a bone.
-
2.
A tumour may arise within a nutrient canal.
-
3.
A soft tissue or periosteal tumour may cause secondary erosion and penetration into the bone.8
Fig. 3.

Showing post-op picture of both patients.
Fig. 4.
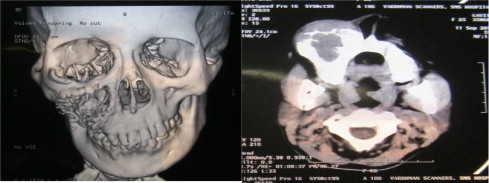
CT Scan showing tumour eroding antrum and orbital floor.
Most of these tumours are encapsulated and range in size from 9.5 cm and have a mean greatest diameter of 6.2 cm.9 Both the tumour in our cases were larger than 6.5 cm.
Microscopically, spindle shaped cells in Antoni-A and Antoni-B arrangement interspersed with Verocay bodies are the characteristic features.10 These tumour cells typically show a diffuse positive immunoreactivity for S-100 protein.11 In both our cases these characteristics were present (Fig. 5).
Fig. 5.
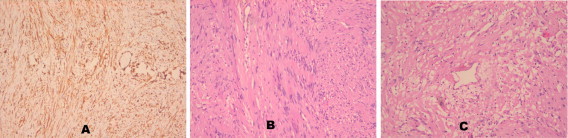
(A) S100; (B) HE 10× Antony B areas; (C) HE 10× Verocay bodies.
Neurilemmomas are resistant to radiotherapy12 and as they are well encapsulated the treatment of choice is conservative surgical enucleation with periodic follow up.
4. Conclusion
Maxillary neurilemmomas are rarest of the rare tumour which should always be included in the differential diagnosis of painless mass arising in and around the oral cavity, and careful attention should be directed towards reaching the diagnosis. In our cases wide excision of the tumours was done and both showed no signs of recurrence one year after surgery.
Conflicts of interest
The authors report that there are no conflicts of interest.
Funding
None.
Ethical approval
Written informed consents were obtained from the patients for publication of these cases and accompanying images. A copy of the written consents is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Dr. Ankit Verma involved in the study design, data collection, and data analysis. Dr. Kinjal Banerjee contributed in the study design and data analysis. Dr. Arpit Verma contributed in writing. Dr. Sugandha Singh involved in data analysis. Dr. Jagdeep Rao contributed in design and data collection. Dr. Prabha Om involved in data analysis.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
Contributor Information
Ankit Verma, Email: ankit.doc2004@gmail.com.
Kinjal Banerjee, Email: drrpsingh22@gmail.com.
Arpit Verma, Email: arpitvermadr@gmail.com.
Sugandha Singh, Email: dr.sugandha22@gmail.com.
Jagdeep Rao, Email: drrpsingh22@rediff.com.
Prabha Om, Email: drdhanwanti22@gmail.com.
References
- 1.Batsakis J.G. 2nd edition. Williams and Wilkins; Baltimore: 1979. Tumours of the peripheral nervous system; pp. 313–333. [Google Scholar]
- 2.Buric N., Jovanovich G., Pesic Z., Krasic D., Radovanovic Z., Mihailovic D. Mandible schwannoma (neurilemmoma) presenting as apical lesion. Dentomaxillofac Radiol. 2009;38:178–181. doi: 10.1259/dmfr/59344498. [DOI] [PubMed] [Google Scholar]
- 3.Colreavy M.P., Lacy P.D., Hughes J., Bouchier-Hayes D., Brennan P., O’Dwyer A.J. Head and neck schwannomas – a 10 year review. J Laryngo Otol. 2000;114:119–124. doi: 10.1258/0022215001905058. [DOI] [PubMed] [Google Scholar]
- 4.Chi A.C., Carey J., Muller S. Intraosseous schwannoma of the mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(1):54–65. doi: 10.1016/s1079-2104(03)00228-2. [DOI] [PubMed] [Google Scholar]
- 5.Fawcett K.J., Dahlin D.C. Neurilemmoma of bone. Am J Clin Pathol. 1967;47(6):759–766. doi: 10.1093/ajcp/47.6.759. [DOI] [PubMed] [Google Scholar]
- 6.Patil K., Mahima V., Srikanth H., Saikrishna D. Central schwanomma of mandible. J Oral Maxillofac Pathol. 2009;13:23–26. doi: 10.4103/0973-029X.48752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martins M.D., Taghloubi S.A., Bussadori S.K., Fernandes K.P., Palo R.M., Martins M.A. Intraosseous schwannoma mimicking a periapical lesion on the adjacent tooth: case report. Int Endod J. 2007;40:72–78. doi: 10.1111/j.1365-2591.2006.01195.x. [DOI] [PubMed] [Google Scholar]
- 8.Buranovic M., Macan D., Begovic E.A., Luksic I., Brajdic D., Manojlovic S. Schwanomma with secondary erosion of mandible: case report with review of literature. Dentomaxillofac Radiol. 2006;35:456–460. doi: 10.1259/dmfr/32200965. [DOI] [PubMed] [Google Scholar]
- 9.White W., Shiu M.H., Rosenblum M.K., Erlandson R.A., Woodruff J.M. Cellular schwanomma a clinicopathologic study of 57 patients and 58 tumours. Cancer. 1990;66:1266–1275. doi: 10.1002/1097-0142(19900915)66:6<1266::aid-cncr2820660628>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 10.Lacerda A.S., Brentegani L.G., Rosa A.L., Vespucio M.V., Salata L.A. Intraoral schwanomma of mandibular symphysis: case report. Braz Dent J. 2006;17:255–258. doi: 10.1590/s0103-64402006000300015. [DOI] [PubMed] [Google Scholar]
- 11.Gnepp D.R. 2nd edition. Saunders; Philadelphia: 2009. Diagnostic surgical pathology of the head and neck: expert consult – online and print; pp. 245–246. [Google Scholar]
- 12.Yusuf H., Fajemisin O.A., McWilliam L.J. Neurilemmoma involving the maxillary sinus: a case report. Br J Oral Maxillofac Surg. 1989;27:506–511. doi: 10.1016/s0266-4356(89)80010-5. [DOI] [PubMed] [Google Scholar]


