Abstract
Background This study created an anatomic reconstruction of the distal oblique bundle (DOB) of the interosseous membrane to determine its effect on distal radioulnar joint (DRUJ) instability and compare this technique with distal radioulnar ligament (DRUL) reconstruction.
Questions/Purposes We hypothesized that this reconstruction would provide equivalent stability to DRUL reconstruction and that combining the two techniques would enhance stability.
Methods Six cadaveric upper limbs were affixed to a custom frame. The volar/dorsal translation of the radius relative to the ulna was measured in 60° pronation, neutral, and 60° supination. Translation was sequentially measured with the DRUJ intact, with sectioned DRULs and triangular fibrocartilaginous complex (TFCC), and with sectioned DOBs. Reconstructions were performed on the DRULs, on the DOB tensioned in both neutral and supination, and employing both techniques.
Results The DOB reconstruction, tensioned both in the neutral position and in 60° supination, was more stable than the partial and complete instability in 6/6 specimens in pronation and the neutral position and in 5/6 specimens in supination. The DOB reconstruction and the DOB reconstruction tensioned in supination were more stable than the DRUL reconstruction in 4/6 patients. Combining the two techniques did not further reduce translation.
Conclusions The DOB reconstruction is capable of improving stability in the unstable DRUJ.
Keywords: distal oblique bundle, distal radioulnar joint, stability, wrist
Instability of the distal radioulnar joint (DRUJ) is a difficult clinical problem, evidenced by the extensive spectrum of procedures in the literature, each unified by the common goals of increasing stability and decreasing pain through resection, fusion, or soft tissue reconstruction. In the setting of DRUJ instability without arthritis and failed nonoperative management, the distal radioulnar ligament (DRUL) reconstruction described by Adams is a commonly employed technique, with clinical results demonstrating resolved or improved instability in 12/14 patients between 1–4 years after surgery (l,10).
Though this technique mimics the action of the volar and dorsal DRUL and foveal attachment of the triangular fibrocartilage to achieve stability, less is known about the distal portion of the interosseous membrane and any potential contribution to stability at the DRUJ. In 1966, Radin described an axial load as a potential injury mechanism of the distal interosseous membrane.1 Watanabe et al tested 8 cadaver forearms both quantitatively and clinically in neutral and 60 degrees of pronation and supination. They found that the distal interosseous membrane (IOM) constrained volar and dorsal translation in all forearm positions tested. According to their results, dorsal dislocation of the radius indicated a distal IOM rupture.2 However, they found a variable presence of discrete fibers in this region. Despite the variable presence of discrete fibers in the distal IOM, an anatomical study conducted by Noda et al identified five ligaments comprised in the IOM, including the distal IOM: the central band (CB), accessory band (AB), proximal oblique cord, dorsal obique accessory cord, and the distal oblique bundle (DOB).3
The DOB is a coalescence of obliquely oriented ligamentous fibers within the distal interosseous membrane that run from the dorsal ulna to the inferior rim of the sigmoid notch and contributes stability to the DRUJ in all positions of forearm rotation.3 4 5 6 Moritomo et al concluded that the DOB formed an isometric collateral ligament in conjunction with the triangular fibrocartilage to stabilize the forearm during rotation because the ulnar insertions coincide with the axis of rotation.7 Kitamura et al tested 10 cadaver arms and found the DOB was present in 4/10. They demonstrated that cadaveric specimens with a DOB possessed significantly greater DRUJ stability, as manifested by decreased DRUJ translation in the neutral forearm, position than those without a DOB.8 Most recently, a biomechanical study evaluating DRUJ stability after ulnar shortening osteotomy found a stabilizing effect of the DOB with ulnar osteotomy performed distal to the ulnar insertion of the ligament, further supporting the static stabilization potential of this ligament.4 Though support exists for a contributing role to stability, variation exists in the anatomy. Discrete bundles of fibers have been found in 4/10 specimens dissected during anatomical studies, perhaps accounting for the variable levels of innate and postoperative stability at the DRUJ.3 8 Furthermore, no published studies exist on the effects of repair or reconstruction of the DOB.
The purpose of this study was to create a novel and easily reproducible reconstruction technique of the DOB and determine the effects of the reconstruction on volar/dorsal stability of the intact DRUJ, the DRUL reconstruction by Adams in an unstable DRUJ, and a combination of the two techniques. We hypothesized that the reconstruction would provide equal stability when compared with the Adams DRUJ reconstruction, and the two techniques employed together would further enhance stability at the DRUJ.
Materials and Methods
Institutional review was obtained prior to the start of this study. Seven fresh frozen cadaveric upper extremities were chosen for use, each without radiographic or clinical evidence of DRUJ pathology, and each lacking incisional scars over the volar or dorsal aspects of the wrist. No substantial intraarticular osteochondral or periarticular soft tissue pathology was demonstrated after dissection. Thirty-six hours prior to testing, each specimen was thawed in a refrigerator. A custom-built semicircular frame was constructed with a polyurethane base containing metal clamps to secure the humerus, and a fiberglass stand with two C-rings bolted to the fiberglass stand.
On the day of testing, each thawed specimen was stripped of soft tissue proximal to the deltoid tuberosity and secured with the two metal clamps. The forearm was secured with two Steinmann pins placed into the ulna, and the hand was fixed with one Steinmann pin in the small finger metacarpal and secured to the frame through bolted eyelets (Fig. 1).
Fig. 1.
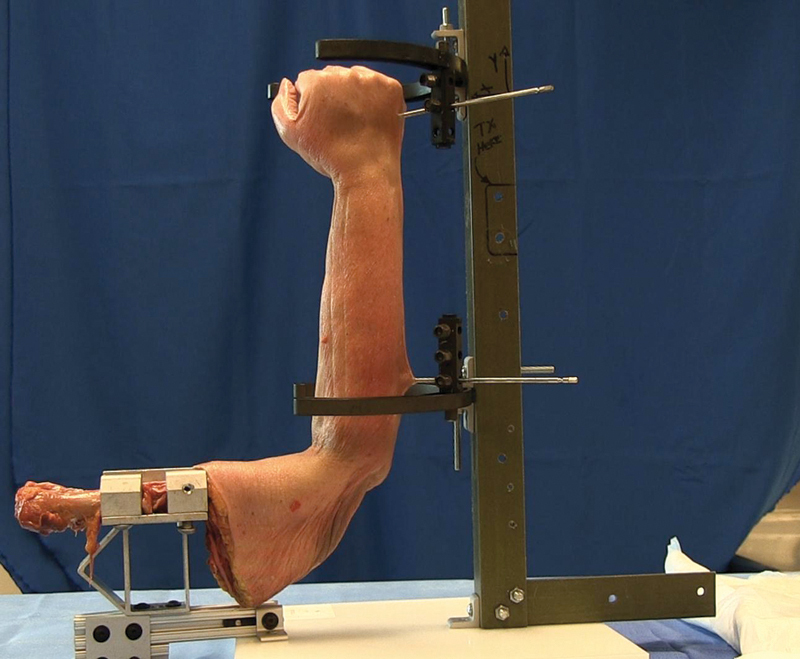
Cadaveric arm mounted in tower.
An electromagnetic motion-tracking system (Liberty, Polhemus Inc., Colchester, Vermont, USA) was used to assess the amount of volar/dorsal translation of the radius relative to the ulna during testing. The Liberty device uses electromagnetic fields to establish the three-dimensional position and the orientation of its sensors. It detects angular motions with an accuracy of 0.3° within its optimal operating range of 10–70 cm.9 This technology has been used extensively in previous studies by our department and others to document motion in cadavers.10 This system consists of one transmitter, which emits an electromagnetic field, and sensors with embedded orthogonal coils that detect position and orientation. Signals from the sensors were recorded and processed at a sampling rate of 240 Hz using custom software developed in LabView (National Instruments, San Antonio, Texas, USA). Two Liberty sensors were secured to fiberglass brackets, placed over the dorsal midshafts of the radius and ulna, and secured with 3.5-mm cortical screws. Relative motion between virtual landmarks on the radius and ulna were calculated. The Lister tubercle and the most radial portion of the dorsal ulnar head were chosen as the reference points for calculation of sagittal motion and were kept constant during each trial.
Testing was performed in neutral, 60° of pronation, and 60° of supination. These positions were achieved by moving the bracket securing the Steinmann pin into the metacarpal. Appropriate rotational motion was verified with a protractor prior to translational testing. The radius was then manually translated dorsally and volarly until resistance from the intact soft tissues was encountered and an endpoint was appreciated preventing further motion; at this point translation continued in the opposite direction. Three consecutive dorsal/volar translations were performed and recorded with real time data, each time ensuring that appropriate parabolic patterns were generated with the data collection program. In all tests, volar translation referred to volar displacement of the radius relative to the ulna. In addition, the term “dorsal translation” referred to the dorsal displacement of the radius relative to the ulna. This process was repeated three times, ensuring continuity with the series of measurements. The bolt securing the Steinmann pin in the metacarpal was repositioned at different locations in the C-ring to maintain the desired position of forearm rotation. The principal investigator (MDR) performed dissection, ligamentous sectioning, ligament reconstructions, and translational testing on all specimens.
Seven specimens were tested. The data from one specimen were excluded due to sensor malalignment. Each specimen was prepared as described and examined under progressive degrees of DRUJ instability. The amount of volar/dorsal translation was initially measured for intact DRUJ complexes. A standard dorsal approach to the DRUJ was performed via a 5-cm incision through the fifth compartment and the joint was exposed with a subligamentous arthrotomy beneath the triangular fibrocartilaginous complex (TFCC). The dorsal radioulnar ligament, TFCC foveal and sigmoid notch attachments, and the pronator quadratus were sectioned, creating partial instability. A 2-cm volar incision was then created over the palmaris longus (or in line with the fourth ray if no palmaris was present), and the interval between the ulnar neurovascular bundle and the flexor tendons exposed the volar aspect of the joint for release of the pronator quadratus, volar radioulnar, and the ulnolunate and ulnotriquetral ligaments. Volar/dorsal translation was then tested to determine motion with partial instability.
The dorsal incision was extended proximally to expose the distal fibers of the interosseous membrane. The ulna was then measured in length from the tip of the ulnar styloid to the olecranon and recorded. If a coalescence of fibers was identified, the origin and insertion were recorded based on lengths measured from the tip of the ulnar styloid and proximal aspects of the sigmoid notch. If a coalescence was not present, a 1-cm thickness of the distal interosseous membrane was sectioned based on the location of the fibers according to Noda et al and Kitamura et al.3 8 This additional sectioning of the DOB or distal interosseous membrane caused complete instability of the DRUJ.
Volar/dorsal translation of the radius was then measured with the forearm in neutral, 60° of pronation, and 60° of supination after four reconstruction combinations were performed: DRUL reconstruction, DOB reconstruction tensioned in neutral forearm rotation, a combined DRUL and DOB reconstruction, and DOB reconstruction with the ligament tensioned in 60° of supination.
The DRUL reconstruction incorporated the technique described by Adams.11 The palmaris longus or a split extensor carpi radialis longus graft was used, depending on palmaris longus availability.
The DOB reconstruction technique incorporated the extensor indicis proprius tendon graft, which was harvested through a transverse incision over the index metacarpophalangeal joint and the base of the dorsal longitudinal incision used to access the distal radioulnar joint. If a DOB or remnant was identified (Fig. 2), the graft was placed through 3.0-mm holes drilled obliquely from the dorsal ulnar shaft, creating a 3–5-mm bone bridge. A second 3.0-mm drill hole was placed at the radial insertion of the DOB just proximal to the sigmoid notch. The hole was oriented obliquely, emerging just under the sigmoid notch with a 3–5-mm bone bridge. Both holes maintained a position at the level of the interosseous membrane. When a DOB could not be located, the drill holes were made at approximately one-sixth the length of the ulnar shaft proximal to the ulnar head and 2–3 mm proximal to the sigmoid notch of the radius, as indicated by Noda et al and Kitamura et al1 12 (Fig. 3). A Huston suture passer was then used to pass the leading end of the tendon graft through the ulnar hole and then dorsally through the radial hole, creating a simple loop (Figs. 3, 4). Tension was applied to reduce the DRUJ and the tendon was clamped in its midsubstance with a mosquito clamp while the forearm was in a neutral position (Fig. 5). The DOB reconstruction was performed as described and tensioned with the ligament tensioned in 60° of supination.
Fig. 2.
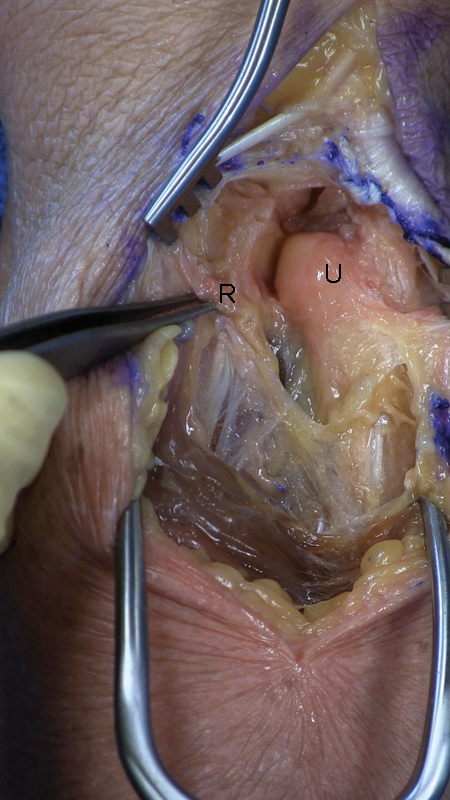
Specimen showing distal oblique bundle (Radius: R, Ulna: U).
Fig. 3.
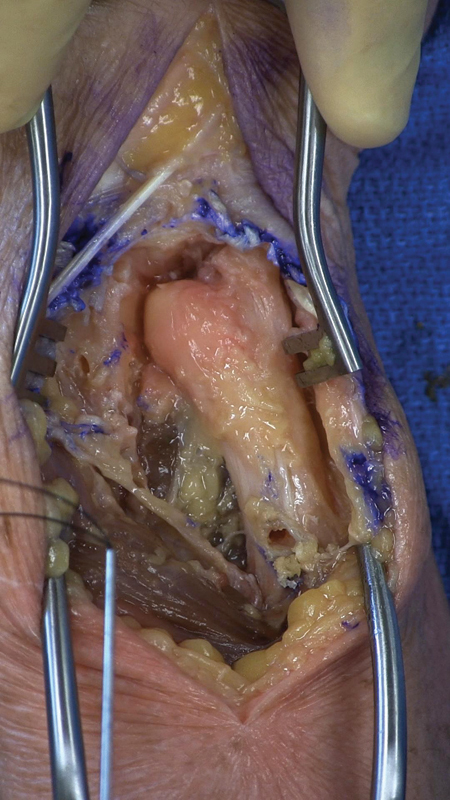
Suture passer retrieving tendon graft through ulnar drill hole placed approximately 3/8 the length of the ulna proximal to the ulnar articular surface.
Fig. 4.
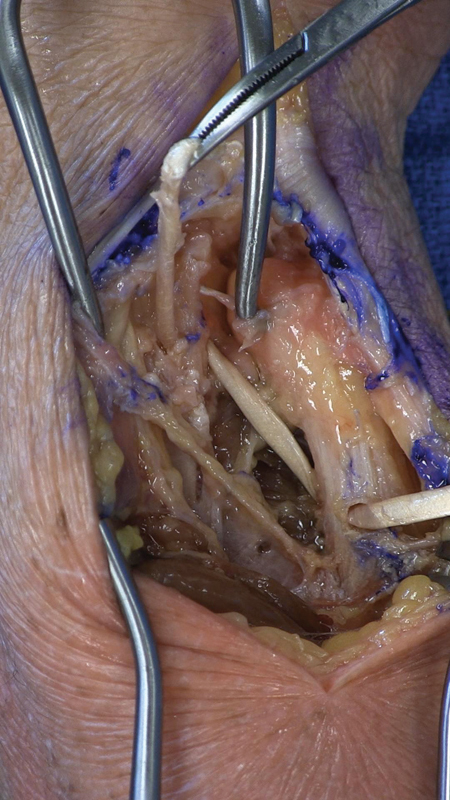
Tendon graft retrieved through radial tunnel drilled just inferior to the sigmoid notch.
Fig. 5.
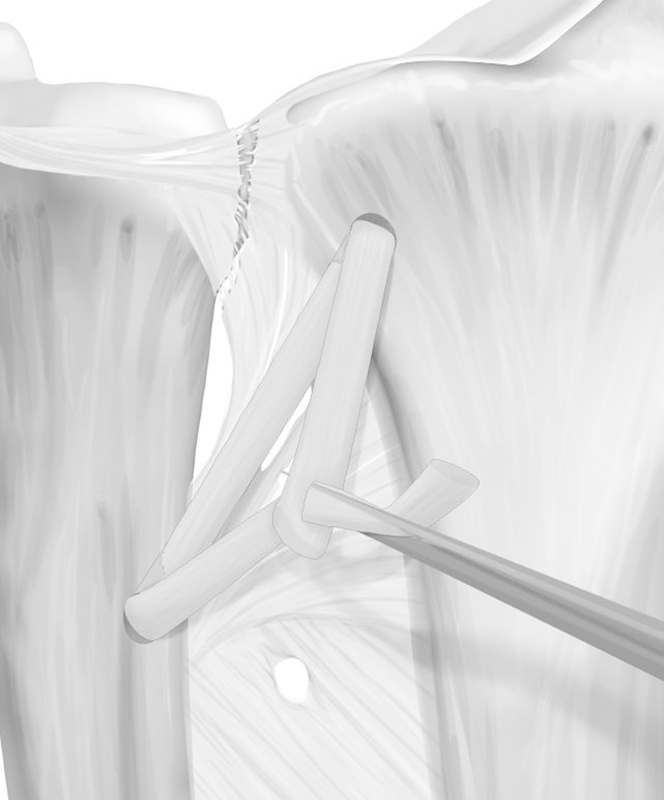
Tensioning the tendon graft.
The DOB + DRUL reconstructions combined the technique described by Adams11 and the DOB reconstruction technique previously described.
Reconstructions were tested on complete instability only and the order varied for each specimen. Mosquito clamps were used to secure tendons to eliminate failure by suture breakage and facilitate the interchange between reconstructions.
Data and Statistical Analysis
To evaluate the effect of different reconstructions on wrist stability, separate analysis of variance (ANOVA) calculations were performed with repeated measures to test the effect of the six wrist-stability conditions. One ANOVA was performed for each forearm position: neutral, pronation, and supination. Planned pairwise comparisons were made between each condition and the intact and unstable conditions. All statistical procedures were performed using SPSS statistical software. For all statistical tests, a P value of <0.05 determined significance.
Results
Three of the six specimens (50%) contained a DOB located an average of 9 mm (7–12 mm) proximal to the sigmoid notch of the radius and 46 mm (41–52 mm) proximal to the ulnar articular surface. In the pronated position, partial and complete instability allowed significantly more motion than the intact DRUJ (P = 0.002, P = 0.022, respectively). The DRUL and DOB reconstructions both reduced motion at the DRUJ (2.15 mm and 1.76 mm, respectively), although these values were not statistically significant when compared with partial and complete instability. The combined DRUL and DOB reconstruction afforded greater stability that was statistically significant when compared with partial (P = 0.007) and complete instability (P = 0.027) and was not significantly different from the intact condition. The DOB reconstruction in supination was significantly more stable than the partial (P = 0.042) and complete instability (P = 0.034) and was not significantly different from the intact DRUJ. The DOB reconstruction was significantly more stable than the partial instability (P = 0.007) and complete instability (P = 0.013) and was not significantly different from the intact condition. Table 1 lists measurements in translation for each reconstruction or instability scenario.
Table 1. DRUJ translation in pronation.
| DRUJ translation in pronation | |||||||
|---|---|---|---|---|---|---|---|
| Specimen | Normal | Partial Inst. | Complete Inst. | BAR + DOB | BAR | DOB | DOB in sup |
| 1 | 4.712 | 6.299 | 5.931 | 4.638 | 3.218 | 3.925 | 1.977 |
| 2 | 0.365 | 1.705 | 1.321 | 1.162 | 2.055 | 0.876 | 0.911 |
| 3 | 0.915 | 2.117 | 3.233 | 1.61 | 3.36 | 1.46 | 1.578 |
| 4 | 2.579 | 2.837 | 2.251 | 2.378 | 2.625 | 2.051 | 1.336 |
| 5 | 0.421 | 1.949 | 1.721 | 0.547 | 0.65 | 0.605 | 0.727 |
| 6 | 1.175 | 2.559 | 2.682 | 0.998 | 0.974 | 1.622 | 1.641 |
| Average | 1.694 | 2.911 | 2.856 | 1.889 | 2.147 | 1.756 | 1.362 |
| SD | 1.535 | 1.56 | 1.507 | 1.353 | 1.038 | 1.079 | 0.43 |
Abbreviations: BAR, Bryan Adams reconstruction, DOB, distal oblique bundle; DRUJ, distal radioulnar joint; Inst., instability; SD, standard deviation; sup, supination.
In the neutral position, complete instability allowed significantly more motion than the intact DRUJ (P = 0.015). The DOB, DOB in supination, and DRUL + DOB reconstructions improved instability (n = 2.41 mm, n = 1.90 mm, n = 1.94 mm); however, these were not statistically significant. The DRUL reconstruction was more stable than either the partial instability (n = 1.97 mm, P = 0.01) or the complete instability (P = 0.01) and was not significantly different from the intact condition. Table 2 lists translation measurements for each reconstruction or instability scenario.
Table 2. DRUJ translation in neutral.
| DRUJ translation in neutral | |||||||
|---|---|---|---|---|---|---|---|
| Specimen | Normal | Partial inst. | Complete inst. | BAR + DOB | BAR | DOB | DOB in sup |
| 1 | 3.218 | 3.453 | 5.962 | 1.378 | 2.635 | 3.794 | 0.997 |
| 2 | 1.099 | 2.611 | 3.512 | 2.354 | 2.063 | 1.146 | 0.618 |
| 3 | 1.107 | 3.631 | 3.491 | 3.227 | 1.75 | 2.455 | 3.105 |
| 4 | 2.174 | 4.213 | 3.852 | 1.761 | 2.362 | 2.366 | 2.79 |
| 5 | 2.315 | 1.872 | 2.017 | 1.905 | 1.337 | 3.564 | 2.775 |
| 6 | 1.305 | 2.322 | 2.44 | 1.011 | 1.641 | 1.126 | 1.146 |
| Average | 1.87 | 3.017 | 3.546 | 1.941 | 1.965 | 2.408 | 1.897 |
| SD | 0.774 | 0.811 | 1.258 | 0.712 | 0.44 | 1.04 | 0.993 |
Abbreviations: BAR, Bryan Adams reconstruction, DOB, distal oblique bundle; DRUJ, distal radioulnar joint; Inst., instability; SD, standard deviation; sup, supination.
In the supinated position, the DOB and DOB in supination reconstructions improved stability compared with the partial and complete instability conditions; however, these results were not statistically significant and were not statistically similar to the stability of the intact DRUJ. Table 3 lists translation measurements for each reconstruction or instability scenario. The combined DRUL and DOB reconstructions did not offer significantly increased stability to translation in any scenario.
Table 3. DRUJ translation in supination.
| DRUJ translation in supination | |||||||
|---|---|---|---|---|---|---|---|
| Specimen | Normal | Partial inst. | Complete inst. | BAR + DOB | BAR | DOB | DOB in sup |
| 1 | 1.611 | 1.298 | 2.655 | 1.325 | 0.948 | 0.801 | 1.299 |
| 2 | 1.488 | 0.919 | 1.094 | 3.78 | 3.805 | 3.204 | 0.743 |
| 3 | 1.363 | 2.575 | 3.17 | 3.064 | 2.535 | 1.148 | 1.44 |
| 4 | 5.596 | 8.856 | 9.3 | 7.476 | 8.266 | 8.007 | 8.078 |
| 5 | 1.775 | 2.735 | 2.3 | 1.237 | 2.64 | 2.705 | 3.412 |
| 6 | 1.155 | 2.25 | 3.676 | 1.679 | 2.115 | 1.847 | 1.8322 |
| Average | 2.165 | 3.106 | 3.699 | 3.093 | 3.385 | 2.952 | 2.8 |
| SD | 1.546 | 2.654 | 2.169 | 2.169 | 2.339 | 2.407 | 2.5 |
Abbreviations: BAR, Bryan Adams reconstruction, DOB, distal oblique bundle; DRUJ, distal radioulnar joint; Inst., instability; SD, standard deviation; sup, supination.
Discussion
The DOB reconstruction not only exceeded the stability afforded by the native DOB, determined during partial instability, but also achieved comparable results to the DRUL reconstruction. The DOB reconstruction tensioned in supination demonstrated a smaller mean translation than the DRUL reconstruction at all forearm positions, with the most pronounced decline in translation occurring with the forearm in pronation. This reinforces a previous conclusion citing the DOB as an important stabilizer to dorsal translation of the ulna relative to the radius in pronation.13 Translation increased with the transition to neutral and supination. The decreased stability in supination with the DOB may result from the lack of a volar tether, which has been shown to be tight in supination.12 This does not explain the laxity seen in the DRUL reconstruction, which contains a volar ligamentous component. A previous biomechanical analysis noted increased dorsal translation in pronation and increased volar translation in supination with a modified Fulkerson-Watson (distal radioulnar tether) procedure.14 The current study calculated only total translation, which was higher with the forearm in supination for all constructs. While the DOB reconstruction tensioned in supination allowed the least translation of all reconstruction techniques, it also allowed less translation than the normal intact state. Despite this increased constraint, full pronation and supination could be achieved during the testing. It is unknown whether this would lead to increased contact forces and potentially precipitate arthritic changes at the DRUJ. Tensioning the reconstruction in supination may be the most beneficial method in this instance, especially if relaxation of the collagen fibers in the tendon graft occurs. Though the DOB technique tensioned in neutral did not approach statistical significance in each testing scenario, significance was seen with all reconstruction techniques tested in pronation, restoring stability that was statistically similar to the intact state and different from the instability states.
Translation for the combined techniques of DRUL and DOB reconstructions did not offer any statistically significant difference in translation at any position tested. In the neutral position, it was comparable to the DRUL reconstruction. This result, however, may be due to an inadequate sample size, creating type II error.
A literature search uncovered two biomechanical evaluations of DRUJ stabilization techniques.14 15 One evaluated DRUJ reconstruction procedures and found that tenodesis and ulnocarpal stabilization procedures were inferior to distal radioulnar slings.15 In the second, capsular imbrication and three different radioulnar sling techniques, including the DRUL reconstruction by Adams, were performed.14 All were found to increase stability; however, capsular repair most accurately replicated intact DRUJ kinematics. The investigators concluded that wrist capsular repair is an effective means of restoring stability and acknowledged that in a chronic situation, soft tissues may be grossly attenuated, prohibiting repair or even imbrication. In this situation, a reconstruction may be warranted. Clinical extrapolation of the DRUL reconstruction described by Adams demonstrated restoration of radioulnar stability in 12/14 patients with at least 80% motion.16 A more recent review found that stability had been achieved and maintained at 6-month follow-up in 9/13 patients.
There are several limitations to this study. Seven specimens were included, one requiring exclusion due to sensor malfunction during testing. A power analysis was not performed to determine the necessary number required for inclusion, introducing the potential for type II error. Though these numbers are suboptimal, existing biomechanical studies in the literature employed similar numbers. The numbers did result, however, in large standard deviations.
An extensor indicis proprius graft was used for the DOB reconstruction. It was chosen based on size comparisons with intact DOB. It is unknown whether using a larger graft, such as the palmaris longus used for the DRUL reconstruction, would result in greater stability and improved results. A significant source of error was the fact that the amount of stress applied to each specimen was not standardized. This may account for the fact that partial sectioning of the DRUJ was more unstable than complete sectioning in 3/6 specimens in pronation, 2/6 specimens in neutral and 1/6 specimens in supination. This also introduces a source of error, since the same surgeon performed the reconstructions and tested each reconstruction. Using a blinded second surgeon and standardizing the amount of tension on each repair would minimize this error. Similarly, the amount of tension on each reconstruction was not standardized, which also introduces error. Nevertheless, the DOB reconstruction tensioned in both the neutral position and in 60° of supination was more stable than the partial and complete DRUJ sectioning in 6/6 specimens in pronation and the neutral position and in 5/6 specimens in supination.
Lastly, this is a biomechanical study evaluating the initial stability of cadaveric specimens and does not test the long-term extrapolation seen in a blinded, prospective, randomized clinical trial. Prospective randomized trials could compare this technique with other reconstruction techniques or simply compare the efficacy of supplementing this technique with those currently available. A clinical trial is currently under way to test the efficacy of this reconstruction.
Reconstruction of the DOB recreates an anatomic static tether to the DRUJ that, when tensioned with the wrist in supination, decreases sagittal translation more than the DRUL reconstruction described by Adams and Berger. It is a technically simpler procedure to perform and can be performed in conjunction with the DRUL reconstruction should intraoperative or postoperative evaluation fail to achieve adequate stability at the DRUJ; however, this study indicates that no additional stability is afforded. Further clinical studies are recommended to determine the clinical efficacy of this technique.
Footnotes
Funding Funding provided by University of Florida Orthopaedics Conflict of Interest None
References
- 1.Radin E L, Riseborough E J. Fractures of the radial head. A review of eighty-eight cases and analysis of the indications for excision of the radial head and non-operative treatment. J Bone Joint Surg Am. 1966;48(6):1055–1064. [PubMed] [Google Scholar]
- 2.Watanabe H, Berger R A, Berglund L J, Zobitz M E, An K N. Contribution of the interosseous membrane to distal radioulnar joint constraint. J Hand Surg Am. 2005;30(6):1164–1171. doi: 10.1016/j.jhsa.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 3.Noda K, Goto A, Murase T, Sugamoto K, Yoshikawa H, Moritomo H. Interosseous membrane of the forearm: an anatomical study of ligament attachment locations. J Hand Surg Am. 2009;34(3):415–422. doi: 10.1016/j.jhsa.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 4.Arimitsu S, Moritomo H, Kitamura T. et al. The stabilizing effect of the distal interosseous membrane on the distal radioulnar joint in an ulnar shortening procedure: a biomechanical study. J Bone Joint Surg Am. 2011;93(21):2022–2030. doi: 10.2106/JBJS.J.00411. [DOI] [PubMed] [Google Scholar]
- 5.Petersen M S, Adams B D. Biomechanical evaluation of distal radioulnar reconstructions. J Hand Surg Am. 1993;18(2):328–334. doi: 10.1016/0363-5023(93)90370-I. [DOI] [PubMed] [Google Scholar]
- 6.Moritomo H. The distal interosseous membrane: current concepts in wrist anatomy and biomechanics. J Hand Surg Am. 2012;37(7):1501–1507. doi: 10.1016/j.jhsa.2012.04.037. [DOI] [PubMed] [Google Scholar]
- 7.Moritomo H, Noda K, Goto A, Murase T, Yoshikawa H, Sugamoto K. Interosseous membrane of the forearm: length change of ligaments during forearm rotation. J Hand Surg Am. 2009;34(4):685–691. doi: 10.1016/j.jhsa.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Kitamura T, Moritomo H, Arimitsu S. et al. The biomechanical effect of the distal interosseous membrane on distal radioulnar joint stability: a preliminary anatomic study. J Hand Surg Am. 2011;36(10):1626–1630. doi: 10.1016/j.jhsa.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Polhemus Inc. Liberty Specifications Available at: http://polhemus.com/polhemus_editor/assets/LIBERTY.pdf
- 10.Conrad B P, Rossi G D, Horodyski M B, Prasarn M L, Alemi Y, Rechtine G R. Eliminating log rolling as a spine trauma order. Surg Neurol Int. 2012;3 03:S188–S197. doi: 10.4103/2152-7806.98584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams B D. Anatomic reconstruction of the distal radioulnar ligaments for DRUJ instability. Tech Hand Up Extrem Surg. 2000;4(3):154–160. doi: 10.1097/00130911-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Acosta R, Hnat W, Scheker L R. Distal radio-ulnar ligament motion during supination and pronation. J Hand Surg [Br] 1993;18(4):502–505. doi: 10.1016/0266-7681(93)90159-d. [DOI] [PubMed] [Google Scholar]
- 13.Kihara H, Short W H, Werner F W, Fortino M D, Palmer A K. The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg Am. 1995;20(6):930–936. doi: 10.1016/S0363-5023(05)80139-X. [DOI] [PubMed] [Google Scholar]
- 14.Gofton W T, Gordon K D, Dunning C E, Johnson J A, King G J. Comparison of distal radioulnar joint reconstructions using an active joint motion simulator. J Hand Surg Am. 2005;30(4):733–742. doi: 10.1016/j.jhsa.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Petersen M S, Adams B D. Biomechanical evaluation of distal radioulnar reconstructions. J Hand Surg Am. 1993;18(2):328–334. doi: 10.1016/0363-5023(93)90370-I. [DOI] [PubMed] [Google Scholar]
- 16.Adams B D, Berger R A. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg Am. 2002;27(2):243–251. doi: 10.1053/jhsu.2002.31731. [DOI] [PubMed] [Google Scholar]


