Abstract
Background Understanding the anatomy of the ligaments of the distal radius aids in the surgical repair of ligamentous injuries and the prediction of intraarticular fracture patterns.
Purposes (1) to measure the horizontal and vertical distances of the origins of the radiocarpal ligaments from the most ulnar corner of the sigmoid notch and the joint line, respectively; and (2) to express them as a percentile of the total width of the bony distal radius.
Methods We dissected 8 cadaveric specimens and identified the dorsal radiocarpal, radioscaphocapitate, and the long and short radiolunate ligaments.
Results The dorsal radiocarpal ligament attached from the 16th to the 52nd percentile of the radial width. The radioscaphocapitate ligament attached around the radial styloid from the 86th percentile volarly to the 87th percentile dorsally. The long radiolunate ligament attached from the 59th to the 85th percentile, and the short radiolunate ligament attached from the 14th to the 41st percentile.
Discussion There was a positive correlation between the radial width and the horizontal distance of the ligaments from the sigmoid notch. These findings may aid individualized surgical repair or reconstruction adjusted to patient size and enable further standardized research on distal radial fractures and their relationship with radiocarpal ligaments.
Keywords: distal radius, morphology, wrist ligaments
Understanding the anatomy of the ligaments of the distal radius aids in the surgical repair of ligamentous injuries and the prediction of intraarticular fracture patterns. There have been many reports describing the anatomy of the ligaments of the distal radius.1 2 3 4. Only a few have measured their dimensions.5 6 To date, the radiocarpal ligaments have not been quantitatively analyzed in relation to the morphology of the radius. By assessing the location of the ligaments relative to the distal radius, we may better predict their location in any given sized individual.
The ligaments play a critical role in the stability of the carpus.3 5 7 8 Accurate (ideally anatomic) surgical repair optimizes carpal stability and kinematics. The ligament origins on the distal radius also influence fracture propagation.9 Mandziak et al found that intraarticular fractures tended to occur between the ligaments and that the Lister tubercle tended to be spared.
The bony dimensions of the radius are variable.10 11 An absolute measurement of the location of the ligament origins may not be precise in a particularly small or large individual. A better understanding of ligament dimensions relative to radius morphology enhances the study and prediction of fracture patterns across populations.
The ligaments have been previously described.1 2 3 4 5 6 The attachment of the dorsal radiocarpal (DRC) ligament spans the ulnar aspect of the dorsal rim of the distal radius from the ulnar margin of the Lister tubercle to the sigmoid notch.3 5 The radioscaphocapitate (RSC) ligament origin spans from the radial styloid to the volar rim of the distal radius at the level of the scaphoid fossa. The long radiolunate ligament (LRL) ligament originates from the volar rim of the scaphoid fossa. The short radiolunate ligament (SRL) ligament originates from the volar rim of the lunate fossa.1 2 3 4 5 6
The purpose of this study was to (1) identify the precise origin of the radiocarpal ligaments by measuring the horizontal distance from the ulnar corner of the sigmoid notch, and the vertical distance from the joint line, to the origin of the radiocarpal ligaments; and (2) express the horizontal distances as a percentile of the total width of the bony distal radius.
Material and Methods
Five thawed fresh frozen cadaveric wrists and three formalin-preserved wrists were examined. The specimens had been donated and consent obtained for anatomical research. There was no record or evidence of trauma or inflammatory arthritis. The radiocarpal joints were carefully exposed. The DRC, RSC, LRL, and SRL ligaments were identified. All measurements were performed by two investigators simultaneously (both qualified surgeons), using a digital caliper (Total Tools Inc., Victoria. Australia, accuracy of 0.03 mm).
First, bony dimensions were measured (Fig. 1). A baseline plane connecting the dorsal and volar corners of the sigmoid notch was established by manually distracting the distal radioulnar joint (DRUJ). A 1-mm wire was placed along this plane in the joint. From this sigmoid notch baseline, a perpendicular line was established to measure the distance from the sigmoid notch baseline to the most radial aspect of the radius. This was identified as the radius width (W). Parallel to the sigmoid notch baseline, the distance from the most volar to the most dorsal aspects of the distal radius was identified as the depth of the distal radius (D).
Fig. 1.
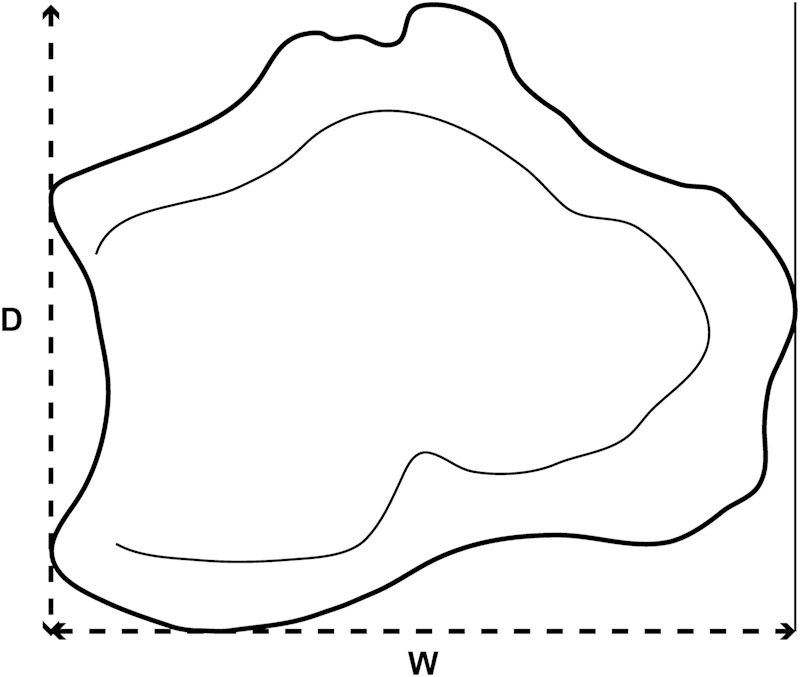
Afterthe sigmoid notch baseline was identified, radial width (W) was measured perpendicular to it, and depth (D) along the sigmoid notch baseline.
Subsequently, the distance of the Lister tubercle from the dorsal corner of the sigmoid notch was measured in a horizontal plane perpendicular to the sigmoid notch baseline.
Second, the dimensions of the origins of the radiocarpal ligaments on the distal radius were measured (Fig. 2). The DRC, RSC, LRL, and SRL ligaments' radius origins were assessed in the following fashion. The horizontal distance from the volar (or dorsal for the DRC) corner of the sigmoid notch to the ulnar border of the ligament origin was recorded. The same measurement was made to the radial border of the ligament origin. This was in the same plane as the radius width (Fig. 1).
Fig. 2.
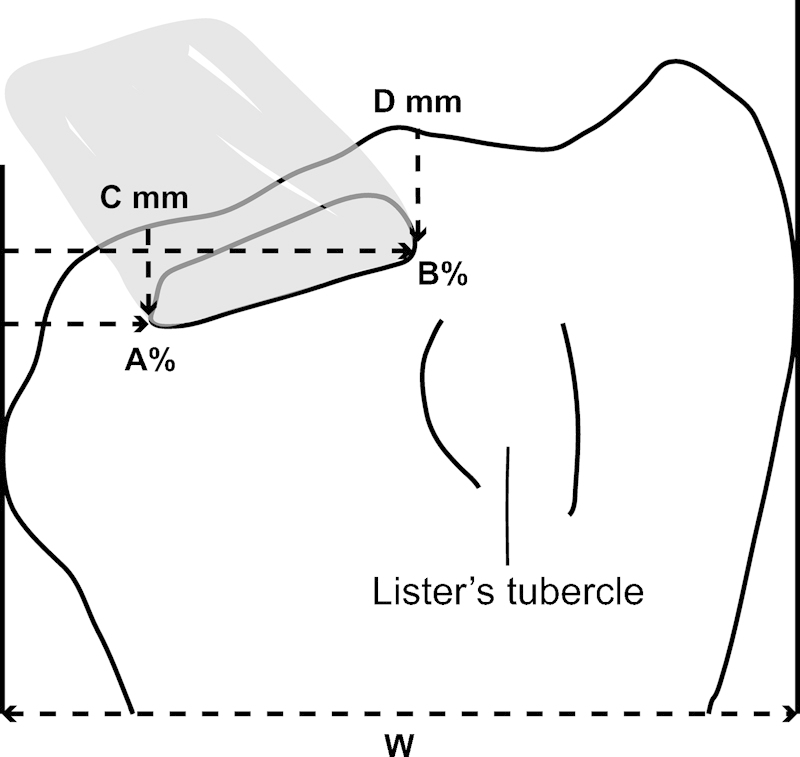
Parameters measured for each ligament, using DRC as an example. W: total width of distal radius. A: distance (in mm and as a percentile of W) from dorsal corner of sigmoid notch to ulnar border of ligament origin. B: distance (in mm and as a percentile of the W) from dorsal corner of sigmoid notch to radial border of ligament origin. C: distance (in mm) of ulnar border of ligament origin from articular surface. D: distance (in mm) of radial border of ligament origin from articular surface.
The horizontal distance of the ligament origin from the corner of the sigmoid notch was then expressed as a percentile of the radius width W. The vertical (distal to proximal) distance from the rim of the articular surface (parallel to the radial diaphysis) to the ulnar and radial border of the ligament origin was also measured (Fig. 2).
Statistical Analysis
The mean and standard deviation (SD) of each dimension for the eight specimens was calculated. Correlation between bony width and horizontal distance of the ligament origin from the sigmoid notch was assessed using Pearson's r test. A two-tailed t-test was used to test significance, which was set at 0.05. SPSS (IBM Corp., New York, NY) software was used for analysis.
Results
The mean age of the fresh frozen specimens was 83 (range 81–87 years). There were two males and three females. The formalin-preserved wrists did not have age or sex data available. Overall, there were three right wrists and five left wrists.
The mean bony width of the radius was 37 (SD 4.8) mm, and the depth was 28 (SD 3.1) mm. In all specimens the widest point of the distal radius from the sigmoid notch was proximal to the radial styloid (Fig. 3). The most prominent points were the Lister tubercle dorsally and the ulnar aspect of the watershed line volarly.
Fig. 3.
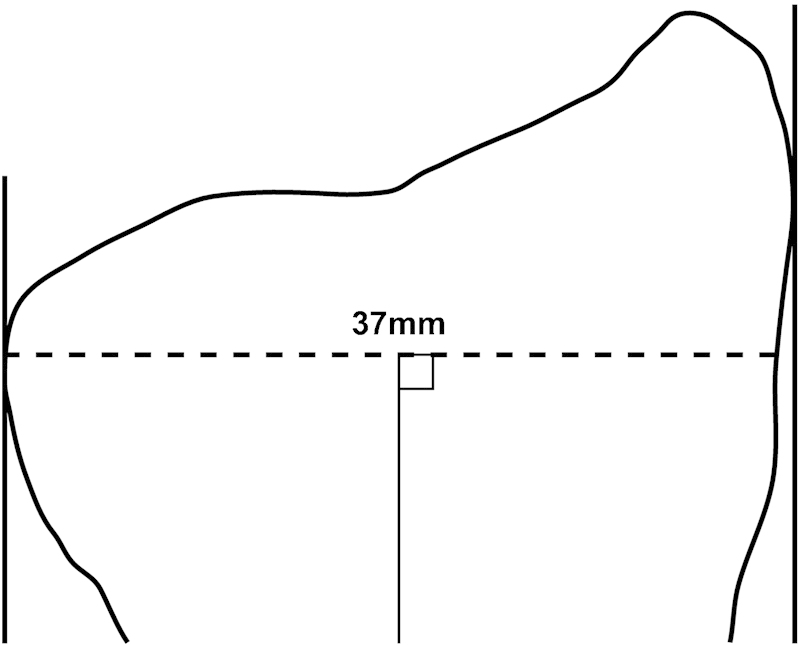
Mean radial horizontal width measured perpendicular to radial diaphysis.
The dimensions of each ligament relative to the radial width are presented in Fig. 4 and in Table 1. The DRC ligament attached from the 16th to the 52nd percentile of the radius width. The RSC ligament attached around the radial styloid from the 86th percentile volarly to the 87th percentile dorsally. The LRL ligament attached from the 59th to the 85th percentile, and the SRL attached from the 14th to the 41st percentile (Fig. 4).
Fig. 4.
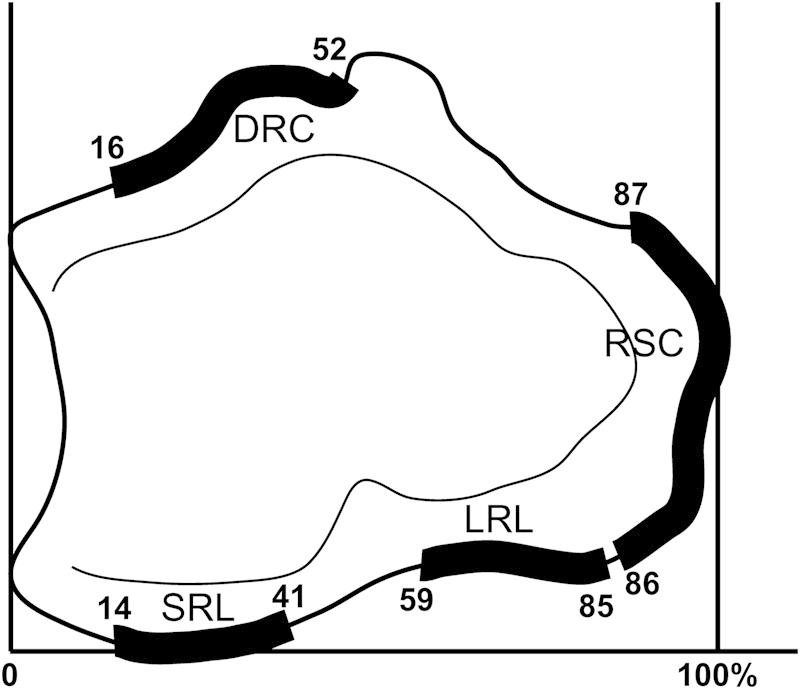
Ligament origins expressed as percentiles of the total bony width of the radius.
Table 1. Mean ligament measurements (mean and SD measurements in mm).
| Horizontal (from sigmoid notch) | Vertical (from joint line) | |||
|---|---|---|---|---|
| Ulnar bordera to Radial bordera | Widthb | Ulnar borderc | Radial borderc | |
| Lister tubercle | 19.6 (± 1.8) to 24.2 (± 2.2) | |||
| DRC | 6.2 (± 2.6) to 19.2 (± 1.7) | 13.1 (± 2.9) | 5.3 (± 1.4) | 6.5 (± 1.9) |
| RSC | 32.3 (± 5.0) dorsal to 31.5 (± 5.5) volard | 7.4 (± 1.4) | 4.8 (± 1.4) | 4.1 (± 0.9) |
| LRL | 21.4 (± 2.4) to 30.5 (± 3.0) | 9.2 (± 2.3) | 5.3 (± 0.6) | 6.2 (± 1.2) |
| SRL | 5.2 (± 3.3) to 15.0 (± 3.3) | 9.8 (± 1.4) | 3.9 (± 1.3) | 4.4 (± 1.0) |
Abbreviations: DRC, dorsal radiocarpal ligament; LRL, the long radiolunate ligament; RSC, the radioscaphocapitate ligament; SRL, the short radiolunate ligament.
Measured distance (mm) from sigmoid notch to the ulnar border (A in Fig. 2) and radial border (B in Fig. 2) of the ligament origin.
Measured width (mm) of the ligament.
Measured distance (in mm) from articular surface to the ulnar border (C in Fig. 2) and radial border (D in Fig. 2) of the ligament origin.
Note the RSC passed from dorsal to volar around the radial styloid.
We found that the DRC ligament consistently attached on the ulnar border of the Lister tubercle. The space between the radial border of the SRL ligament and the ulnar border of the LRL ligament lay between the 41st and the 59th percentile of the radial width. The RSC ligament curved around the radial styloid.
There was a positive correlation between the bony width of the radius and the horizontal distance of the ligament origins from the ulnar border of the sigmoid notch (Table 2).
Table 2. Statistical correlation between bony radial width and horizontal distance of ligament origin from the sigmoid notch.
| Ulnar border | Radial border | ||
|---|---|---|---|
| DRC | Pearson's r | 0.7 | 0.7 |
| Significance | 0.1 | 0.09 | |
| RSC | Pearson's r | 0.95 | 0.8 |
| Significance | 0.00 | 0.03 | |
| LRL | Pearson's r | 0.7 | 0.7 |
| Significance | 0.08 | 0.06 | |
| SRL | Pearson's r | 0.3 | 0.5 |
| Significance | 0.5 | 0.3 |
Discussion
This study has described the ligaments' origins as a percentile of the width of the distal radius, measured from the most ulnar border of the radius. The distance of the ligament origins from the sigmoid notch tended to increase as the bony dimensions increased, suggesting that a percentile may be more valid than an absolute measure when dealing with different-sized individuals, although this was statistically significant only for the RSC.
Our ligament dissections were anatomically consistent with previous work.2 6 We did not find any of the less common variations of the DRC ligament described by Viegas et al.5
The total width of the distal radius has not been extensively studied, although inclination, variance and palmar tilt are more frequently reported because of their clinical utility.12 Our results were similar to a German study10 (mean width 34.9 mm) and were slightly larger than previously reported in Indian dry bone populations (mean width 26.7 mm).11 This may be due to ethnic variations. Our specimens were Anglo-Saxon, with no Indian specimens.
It is well established that ligament heights and widths vary.13 The DRC ligament is well described by Viegas et al, with a mean width of 20.5 mm. Our results are comparable, with all of our specimens showing a type 1 DRC.5 The dimensions of the volar ligaments are similar to those reported by Nagao et al,6 who found a mean width of 6 mm for the LRL ligament and 11 mm for the SRL. They performed a computerized model of the ligament insertions but did not relate them to radial width.
Intraarticular distal radius fracture patterns are influenced by the ligament origins. The fracture lines traverse the cortices between the ligaments, whereas the origins of ligaments are relatively protected.9 Mandziak et al postulated that this was due to the ligaments avulsing the fragments or the attachment site having higher bone density. This study provides percentile data against which future radiographic studies of fracture propagation can be standardized.
The insertion of the brachioradialis tendon has also been implicated in fracture propagation. Radial fractures were found to breach the cortex proximal to the brachioradialis insertion. Koh et al proposed that the tendon reinforced the radial aspect of the distal radius, as well as being a deforming force.14 The extensor retinaculum may also influence fracture patterns, particularly the septa.15
If soft tissue attachments on the distal radius alter the pattern of fracture propagation, further research regarding the capsule insertion on the distal radius, and the proximal and distal extent of the extensor retinaculum, would be important. The relationship to the watershed line would also be informative. Mandziak et al studied cortical breaches of distal radius fractures in the axial plane only at the level of the articular surface. However, fractures also extend to breach the cortices more proximally. Studying the relationship of metaphyseal cortical breaches to soft tissue attachments may aid our understanding of fracture propagation.
Our study contained eight specimens of mixed preservation method. Although there were no statistical differences between the formalin-fixed group and the fresh frozen group, it is unclear what effect the fixative had. This is unlikely to have significantly affected the anatomic ligament origins or the bone morphology.16 It may affect the biomechanical properties,17 18 19 but these were not relevant in our study. A weakness of this study is the small number of specimens and lack of statistical significance, which makes it difficult to draw any definitive conclusions.
Acknowledgments
We thank the Ray Last Laboratory for their generous support and providing access to the specimens.
Conflict of Interest None
Note
Study performed at the University of Adelaide Ray Last Anatomy Laboratory, South Australia, Australia.
References
- 1.Berger R A, Landsmeer J M. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg Am. 1990;15(6):847–854. doi: 10.1016/0363-5023(90)90002-9. [DOI] [PubMed] [Google Scholar]
- 2.Berger R A. The ligaments of the wrist. A current overview of anatomy with considerations of their potential functions. Hand Clin. 1997;13(1):63–82. [PubMed] [Google Scholar]
- 3.Berger R A. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;(383):32–40. doi: 10.1097/00003086-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Kijima Y, Viegas S F. Wrist anatomy and biomechanics. J Hand Surg Am. 2009;34(8):1555–1563. doi: 10.1016/j.jhsa.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Viegas S F, Yamaguchi S, Boyd N L, Patterson R M. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg Am. 1999;24(3):456–468. doi: 10.1053/jhsu.1999.0456. [DOI] [PubMed] [Google Scholar]
- 6.Nagao S, Patterson R M, Buford W L Jr, Andersen C R, Shah M A, Viegas S F. Three-dimensional description of ligamentous attachments around the lunate. J Hand Surg Am. 2005;30(4):685–692. doi: 10.1016/j.jhsa.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Smith D K. Volar carpal ligaments of the wrist: normal appearance on multiplanar reconstructions of three-dimensional Fourier transform MR imaging. AJR Am J Roentgenol. 1993;161(2):353–357. doi: 10.2214/ajr.161.2.8333377. [DOI] [PubMed] [Google Scholar]
- 8.Mizuseki T Ikuta Y The dorsal carpal ligaments: their anatomy and function J Hand Surg [Br] 198914191–98. (British and European Volume) [DOI] [PubMed] [Google Scholar]
- 9.Mandziak D G, Watts A C, Bain G I. Ligament contribution to patterns of articular fractures of the distal radius. J Hand Surg Am. 2011;36(10):1621–1625. doi: 10.1016/j.jhsa.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Pichler W, Mazzurana P, Clement H, Grechenig S, Mauschitz R, Grechenig W. Frequency of instrument breakage during orthopaedic procedures and its effects on patients. J Bone Joint Surg Am. 2008;90(12):2652–2654. doi: 10.2106/JBJS.H.00163. [DOI] [PubMed] [Google Scholar]
- 11.Prithishkumar I J. et al. Morphometry of the distal radius–an osteometric study in the Indian population. Indian Journal of Basic & Applied Medical Research. 2012;1(3):166–171. [Google Scholar]
- 12.Schuind F A, Linscheid R L, An K N, Chao E Y. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am. 1992;74(9):1418–1429. [PubMed] [Google Scholar]
- 13.Feipel V, Rooze M. Three-dimensional motion patterns of the carpal bones: an in vivo study using three-dimensional computed tomography and clinical applications. Surg Radiol Anat. 1999;21(2):125–131. doi: 10.1007/s00276-999-0125-7. [DOI] [PubMed] [Google Scholar]
- 14.Koh S, Andersen C R, Buford W L Jr, Patterson R M, Viegas S F. Anatomy of the distal brachioradialis and its potential relationship to distal radius fracture. J Hand Surg Am. 2006;31(1):2–8. doi: 10.1016/j.jhsa.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Iwamoto A, Morris R P, Andersen C, Patterson R M, Viegas S F. An anatomic and biomechanic study of the wrist extensor retinaculum septa and tendon compartments. J Hand Surg Am. 2006;31(6):896–903. doi: 10.1016/j.jhsa.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 16.Nazarian A, Hermannsson B J, Muller J, Zurakowski D, Snyder B D. Effects of tissue preservation on murine bone mechanical properties. J Biomech. 2009;42(1):82–86. doi: 10.1016/j.jbiomech.2008.09.037. [DOI] [PubMed] [Google Scholar]
- 17.Currey J D, Brear K, Zioupos P, Reilly G C. Effect of formaldehyde fixation on some mechanical properties of bovine bone. Biomaterials. 1995;16(16):1267–1271. doi: 10.1016/0142-9612(95)98135-2. [DOI] [PubMed] [Google Scholar]
- 18.Ohman C, Dall'Ara E, Baleani M, Van Sint Jan S, Viceconti M. The effects of embalming using a 4% formalin solution on the compressive mechanical properties of human cortical bone. Clin Biomech (Bristol, Avon) 2008;23(10):1294–1298. doi: 10.1016/j.clinbiomech.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Cömert A, Kökat A M, Akkocaoğlu M, Tekdemir I, Akça K, Cehreli M C. Fresh-frozen vs. embalmed bone: is it possible to use formalin-fixed human bone for biomechanical experiments on implants? Clin Oral Implants Res. 2009;20(5):521–525. doi: 10.1111/j.1600-0501.2008.01682.x. [DOI] [PubMed] [Google Scholar]


