Abstract
Background
Using reverse genetics, we generated a recombinant low-pathogenic LaSota strain Newcastle disease virus (NDV) expressing the glycoprotein (GP) of Ebola virus (EBOV), designated rLa-EBOVGP, and evaluated its biological characteristic in vivo and in vitro.
Results
The introduction and expression of the EBOV GP gene did not increase the virulence of the NDV vector in poultry or mice. EBOV GP was incorporated into the particle of the vector virus and the recombinant virus rLa-EBOVGP infected cells and spread within them independently of exogenous trypsin. rLa-EBOVGP is more resistant to NDV antiserum than the vector NDV and is moderately sensitive to EBOV GP antiserum. More importantly, infection with rLa-EBOVGP was markedly inhibited by IPA3, indicating that rLa-EBOVGP uses macropinocytosis as the major internalization pathway for cell entry.
Conclusions
The results demonstrate that EBOV GP in recombinant NDV particles functions independently to mediate the viral infection of the host cells and alters the cell-entry pathway.
Keywords: Recombinant Newcastle disease virus, Ebola virus, Glycoprotein, Virus entry, Macropinocytosis
Background
Ebola virus (EBOV) causes severe hemorrhagic fever in humans, with a case fatality rate of up to 90% [1,2]. Its high fatality rate and human-to-human spread renders the virus a potential bioterrorism weapon. Currently, there are no licensed vaccines or therapeutic regimens for the disease. A safe and efficient vaccine for EBOV is yet to be developed. EBOV is an enveloped single-stranded negative-sense RNA virus belonging to the family Filoviridae[3]. The envelope glycoprotein (GP) of EBOV is an important virulence factor and mediates cell receptor binding and virus–cell membrane fusion [2,4-10]. GP protein also plays a central role in inducing protective neutralizing antibodies in the host [11,12]. Several recombinant GP-expressing viruses have been developed, including replication-defective adenovirus-5 (rAd5) [13,14], replication-competent vesicular stomatitis virus (VSV) [15,16], Newcastle diseases virus (NDV)[17], rabies virus (RV) [18] and human parainfluenza virus type 3 (HPAIV) (Bukreyev et al., 2007).
Newcastle disease virus (NDV) is a member of the genus Avulavirus of the family Paramyxoviridae. NDV strains are classified as nonvirulent (lentogenic), moderately virulent (mesogenic), or highly virulent (velogenic) in poultry [19]. NDV has two envelope glycoproteins, hemagglutinin-neuramidinase (HN) and fusion protein (F). HN functions sialic acid receptor binding and F induces fusion during cell entry of NDV [20]. Viral virulence is mainly determined by the amino acid sequence at the protease cleavage site of theF precursor [20]. Lentogenic strains contain fewer basic amino acids at this site and can only be cleaved by trypsin-like extracellular proteases, which are largely confined to the respiratory tract, whereas highly virulent strains are cleaved by ubiquitous intracellular proteases, potentially resulting in systemic infections [21]. The attractions of NDV as a vaccine vector for emerging human infectious diseases include: preexisting immunity and maternal antibodies to mammalian paramyxoviruses do not interfere with the infection or replication of NDV because NDV is antigenically distinct from the mammalian paramyxoviruses [22,23]; lentogenic NDV usually shows limited replication in mammalian host cells because it requires a trypsin-like proteinase for the cleavage of the F glycoprotein [20,21,24,25]. Currently, lentogenic NDV strains, such as the LaSota strain, are used as live attenuated vaccines against NDV in poultry [26] and have been actively developed and evaluated as vaccine vectors for the control of human and animal infectious diseases, including influenza [27,28], severe acute respiratory syndrome [29], human parainfluenza [30], highly pathogenic H5N1 [13,31,32], human immunodeficiency virus [33,34], rabies [35], Nipah disease [36], and Rift Valley fever [37]. The safety and efficacy of NDV has been demonstrated in mice [32,36], dogs [35], pigs [36], cattle [38,39], sheep [37], African green and rhesus monkeys [17,30], and humans [40-43]. Recently, a study by DiNapoli et al. showed that a recombinant NDV expressing EBOV GP was immunogenic and caused no abnormalities or disease symptoms after its inoculation into rhesus monkeys [17]. Their study also showed that EBOV GP was incorporated into the recombinant NDV particles, which raised a serious question. Does EBOV GP function biologically normally in the virus particle during cell entry? If so, this entails biosafety concerns regarding the candidate vaccine vector.
In this study, we generated a recombinant lentogenic NDV, based on the LaSota strain, that expresses the EBOV GP protein. Its safety for poultry and mice in vivo, its infection and spreadability among cells in vitro, its sensitivity to anti-NDV and anti-EBOV neutralizing antibodies, and the internalization pathway of this recombinant virus were characterized.
Results
Expression of EBOV GP does not increase the pathogenicity of the NDV vector in poultry or mice
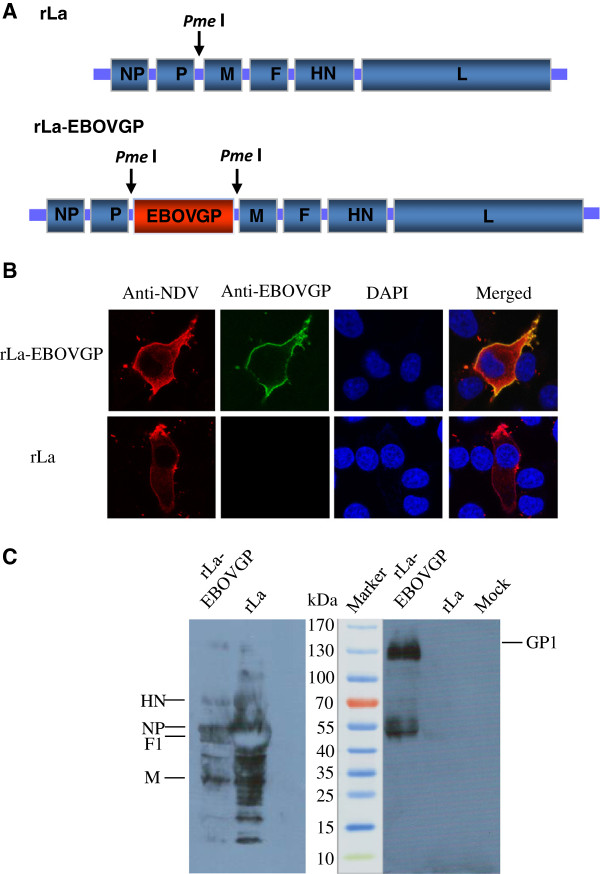
Recombinant NDV expressing the Zaire EBOV GP (rLa-EBOVGP) was generated by inserting the EBOV GP gene between the P and M genes in the genomic cDNA of the NDV LaSota strain (rLa) (Figure 1A). Expression of the GP gene was confirmed by indirect confocal immunofluorescent staining of rLa-EBOVGP-infected BHK-21 cells. rLa-EBOVGP-infected BHK-21 cells were stained with mouse anti-EBOV GP antiserum, whereas rLa-infected BHK-21 cells were not stained with the antiserum (Figure 1B). NDV antigens and EBOV GP protein colocalized on the surfaces of the BHK-21 cells, confirming the surface expression of the EBOV GP protein in the rLa-EBOVGP-infected BHK-21 cells (Figure 1B).
Figure 1.
Generation of recombinant NDV expressing the EBOV GP gene. (A) Schematic representation of the rLa genome, showing the restriction site for endonuclease PmeI, introduced between the P and M genes, and the EBOV GP gene inserted into the PmeI site. (B) Indirect immunofluorescent staining of rLa-EBOVGP-infected BHK-21 cells with chicken anti-NDV antiserum and mouse anti-EBOV GP antiserum, observed with confocal laser microscopy. (C) Western blotting of sucrose-gradient-purified rLa and rLa-EBOVGP, hybridized with chicken anti-NDV antiserum and mouse anti-EBOV GP antiserum.
rLa-EBOVGP showed similar growth properties to those of rLa, with a maximum titer of 109.6 × 50% embryo infectious doses (EID50) at 72 h after inoculation in specific-pathogen-free (SPF) chicken eggs. rLa-EBOVGP retained its low pathogenicity, as a lentogenic strain, in eggs and chickens [44], with a mean death time (MDT) > 140 h, an intracerebral pathogenicity index (ICPI) of 0, and an intravenous pathogenicity index (IVPI) of 0. During the three-week observation period after the mice were inoculated either intramuscularly (i.m.) or intranasally (i.n.) with a high dose of rLa-EBOVGP, they showed no signs of sickness or death, and did not differ in weight gain from the mice inoculated with rLa. These results suggest that the expression of EBOV GP does not increase the pathogenicity of the NDV vector in poultry or mice.
EBOV GP is incorporated into the vector virus particles and the recombinant virus rLa-EBOVGP infects cells and spreads among them independently of exogenous trypsin
Previous studies have reported that the envelope glycoproteins of heterogeneous viruses can be expressed by recombinant NDV and incorporated into the viral vector particles [17,35]. To investigate whether the EBOV GP expressed by the recombinant NDV is incorporated into the viral vector particles, the viral particles of rLa-EBOVGP and rLa were purified by sucrose gradient centrifugation and subjected to immunoblotting analysis with mouse anti-EBOV GP antiserum as the primary antibody. A clear GP1 band of ~130 kDa was apparent in the rLa-ZEBOVGP sample but not in the rLa sample. This indicates that the GP protein was expressed by rLa-EBOVGP and incorporated into the recombinant NDV particles, which is consistent with a previous report [17].
The cleavage of the F glycoprotein is a prerequisite for the infectivity of NDV. Because it is a lentogenic NDV strain, the infectivity of rLa depends on exogenous trypsin-like extracellular proteases [35,36]. To investigate whether the incorporation of EBOV GP alters the infectivity of the recombinant NDV, rLa and rLa-EBOVGP were propagated in eggs (rLa-egg and rLa-EBOVGP-egg, respectively) and in BHK-21 cells with or without TPCK-trypsin (Sigma) in the medium (rLa-cell/TPCK, rLa-EBOVGP-cell/TPCK, rLa-cell, and rLa-EBOVGP-cell respectively). These prepared viruses were then used to infect BHK-21 cells at a multiplicity of infection (MOI) of 0.02–0.05 with no exogenous trypsin in the medium. As expected, rLa-cell did not infect any cells (Figure 2, column 2), whereas rLa-egg and rLa-cell/TPCK infected individual cells but did not spread between the cells. However, rLa-EBOVGP-egg, rLa-EBOVGP-cell, and rLa-EBOVGP-cell/TPCK showed similar infectivity and spreadability in the cells. At 120 h postinfection (PI), more than 90% of cells were infected by all the differently prepared rLa-EBOVGP viruses (Figure 2, columns 3 and 4). These results suggest that the expression and incorporation of EBOV GP allow the vector NDV to infect cells and to spread among the cells independently of exogenous trypsin.
Figure 2.
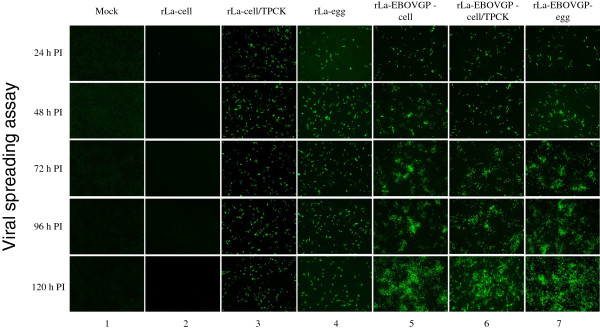
Viral spreading assay. Confluent BHK-21 cells were infected with rLa-cell, rLa-cell/TPCK, rLa-EBOVGP-cell, rLa-ZEBOVGP-cell/TPCK, rLa-egg, or rLa-EBOVGP-egg at MOIs of 0.05. The cells were fixed at different time points and detected with chicken anti-NDV antiserum, then incubated with an FITC-conjugated rabbit anti-chicken antibody.
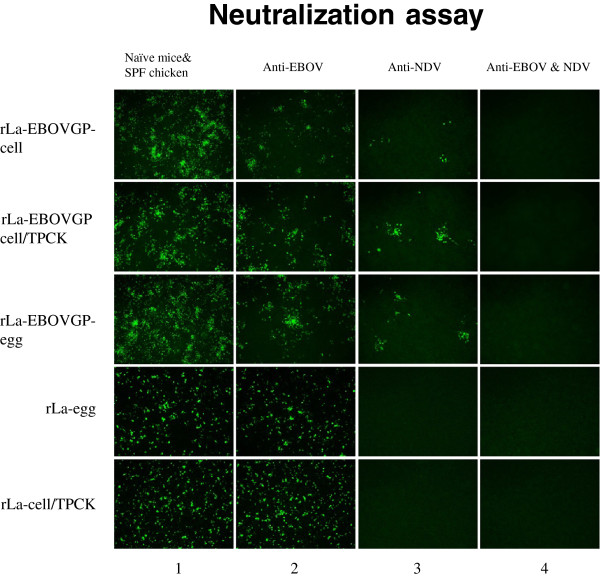
rLa-EBOVGP is more resistant to NDV antiserum than vector NDV and partially sensitive to EBOV antiserum
The two envelope glycoproteins of NDV, HN and F, are indispensablefor cell entry, which includes receptor binding and virus-cell membrane fusion. This is the first step in infection and a prerequisite for viral replication [26]. EBOV has only one envelope glycoprotein, which functions in receptor binding and membrane fusion [4-8]. To understand the impact of EBOV GP on the infectivity of the NDV vector, the sensitivities of rLa and rLa-EBOVGP to NDV antiserum and EBOV GP antiserum were evaluated and compared (Figure 3). As expected, both rLa-egg and rLa-cell were resistant to mouse anti-EBOV GP antiserum (diluted 1:10) but were completely neutralized by chicken anti-NDV antiserum (diluted 1:100). However, both anti-NDV antiserum (diluted 1:100) and anti-EBOV GP antiserum (diluted 1:10) only partially neutralized rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, and rLa-EBOVGP-egg (Figure 3, column 2). The anti-NDV antiserum and anti-EBOV GP antiserum reduced the infection with each rLa-EBOVGP virus by about 90% and 60%, respectively (Figure 3, column 3). When the anti-NDV antiserum (diluted 1:100) and anti-EBOV GP antiserum (diluted 1:10) were mixed, infection with rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, or rLa-EBOVGP-cell was completely blocked (Figure 3, column 4). The same dilution of SPF chicken0020serum, naïve mouse serum, or a mixture of SPF chicken serum and naïve mouse serum, used as the controls, showed no neutralization activity against any of the differently prepared rLa or rLa-EBOVGP viruses. These results suggest that the incorporation of EBOV GP into the recombinant viral particle made the NDV vector more resistant to anti-NDV antiserum and more sensitive to anti-EBOV antiserum.
Figure 3.
Neutralization assay. rLa-cell/TPCK, rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, rLa-egg, and rLa-EBOVGP-egg (each 5 × 102 TCID50) were mixed individually with chicken anti-NDV antiserum (diluted 1:100), mouse anti-EBOV GP antiserum (diluted 1:10), or a mixture of chicken and mouse antisera at the same dilutions. The viruses were also mixed with a combination of SPF chicken serum and naïve mouse serum as the mock-treated groups. After incubation, the viruses were allowed to infect BHK-21 cells for 1 h. The cells were fixed 48 h after infection, treated with chicken anti-NDV antiserum, and then incubated with a FITC-conjugated rabbit anti-chicken antibody.
rLa-EBOVGP uses macropinocytosis as the major internalization pathway for cell entry
NVD envelope glycoproteins HN and F usually bind to receptor and induce virus-cell membrane fusion at neutral pH. A previous study reported that NDV can also partially enter the host cells by caveolae-mediated endocytosis [45], whereas EBOV mainly enters cells via macropinocytosis [46-48] in a GP-dependent manner [46,49]. Because EBOV GP is incorporated into the vector NDV particles and independently mediates the cell entry of rLa-EBOVGP, it is necessary to determine whether the incorporation of the GP protein alters the endocytosis pattern of rLa-EBOVGP during infection. To address this question, we used two chemicals, IPA3 and methyl β-cyclodextrin (MβCD) to treat BHK-21 cells before their infection with the rLa or rLa-EBOV virus. IPA3 inhibits the activation of PAK1 kinase, which is required for macropinocytosis [50,51] and MβCD sequesters cholesterol from the cell membrane, thus inhibiting clathrin- and caveolae-mediated endocytosis [52,53]. As shown in Figure 4, the infection of IPA3-pretreated BHK-21 cells with rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, or rLa-EBOVGP-egg was greatly reduced, whereas IPA3 had no inhibitory effect on the infectivity of rLa-egg or rLa-cell/TPCK. Fewer than 10% of IPA3-pretreated cells were infected with rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, or rLa-EBOVGP-egg compared with the untreated cells. Infection by rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, or rLa-EBOVGP-egg was not inhibited in cells pretreated with MβCD, but their infection by rLa-cell/TPCK and rLa-egg was moderately reduced. Pretreatment with a combination of IPA3 and MβCD almost completely blocked the infection of cells by rLa-EBOVGP-cell, rLa-EBOVGP-cell/TPCK, and rLa-EBOVGP-egg, and also mildly inhibited the infection of cells by rLa-cell/TPCK and rLa-egg. To further testify the role of EBOV GP on the internalization of the recombinant virus, we use 800 mU/ml bacterial neuraminidase (NA, Sigma N2876) to treat cells with chemical inhibitors together with IPA3 or alone before infection. Our preliminary data showed use 800 mU/ml NA to treat cells could block over 90% of NDV infection, thus in this assay we used NA to exclude the influence of HN protein in the internalizaiton of rLa-EBOVGP-egg and rLa-EBOVGP-cell/TPCK. Also shown in Figure 4 (right panel), NA treatment reduced over 90% of rLa-egg and rLa-cell/TPCK infection, while it had almost no reduction on the infection of rLa-EBOVGP-egg, rLa-EBOVGP-cell/TPCK and rLa-EBOVGP-cell. The NA + IPA3 treatment could block 90% of the recombinant viruses from infection, while NA + MβCD had no inhibition on these viruses. These results futher explicated the role of GP on the macropinocytotic internalization of the recombinant viruses. In conclusion, Our results indicate that recombinant rLa-EBOVGP uses macropinocytosis as its major internalization pathway for cell entry, rather than the direct fusion at the cell plasma membrane at neutral pH like NDV.
Figure 4.
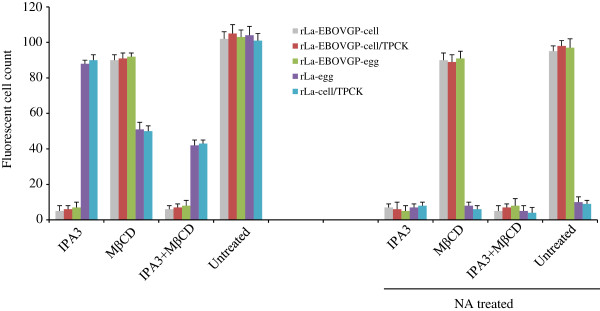
Chemical inhibition of virus internalization pathways. BHK-21 cells were pretreated with (right panel) or without (left panel) NA alone or together with inhibitor 10 μM IPA3 or 10 mM MβCD or a mixture of the two chemicals at 37°C for 1 h. The cells were washed and infected with 5 × 102 TCID50 of rLa-egg, rLa-EBOVGP-egg, rLa-cell/TPCK rLa-EBOVGP-cell, or rLa-EBOVGP-cell/TPCK at 4°C for 1 h in the presence of the chemical(s). The cells were then washed and incubated at 37°C. At 7 h after infection, the cells were washed, fixed, permeabilized, and immunostained with chicken anti-NDV antiserum, then incubated with a FITC-conjugated rabbit anti-chicken antibody.
Discussion
Using reverse genetics, we generated a recombinant low-pathogenic LaSota NDV that expresses GP of EBOV, designated rLa-EBOVGP, and evaluated its biological characteristics in vivo and in vitro. The introduction and expression of the EBOV GP gene did not increase the virulence of the NDV vector in poultry or mice, which is consistent with the results of a previous study in monkeys [17]. EBOV GP was incorporated into the viral particles of rL-EBOVGP and allowed the NDV vector to infect mammalian cells independently of exogenous trypsin.
The restriction of NDV replication in mammalian host cells is one of the most attractive properties of lentogenic NDV in terms of its safety when used as a live vaccine vector in animals and humans, as is also the case for fowlpox virus [54,55] and a modified vaccinia virus Ankara [56,57]. The V protein encoded by the NDV P gene functions as an interferon antagonist and is usually less efficient in mammalian cells [58-60]; NDV is usually a strong inducer of the interferon response in mammalian cells and is highly sensitive to the interferon induced in these cells [61,62]. The limited replication in mammalian cells of low-pathogenic NDV, like the LaSota strain, is also determined by its trypsin-dependent infectivity. The trypsin-independent infectivity acquired by rLa-EBOVGP means that this virus behaves like a velogenic NDV in mammalian host cells. Its restricted replication may have to depend on the only defense line in host, the native immunity.
The ability of foreign envelope proteins to function as new cell-entry proteins has also been demonstrated in other enveloped negative-strand RNA viruses [63]. The function of EBOV GP in mediating the cell entry of VSV when the G gene had been deleted from the VSV genome could be compensated by several foreign envelope glycoproteins from different viruses in trans or with recombinant expression, including Ebola virus, Marburg virus, Lassa fever virus, Hantaan virus, and Nipah virus [4,6,7,64-67]. Therefore, it is reasonable to infer that the incorporation of EBOV GP into the viral particle may cause the trypsin-independent infectivity of rL-EBOVGP.
So far, very few studies have examined the biological functions of native and foreign envelope glycoproteins when they are incorporated into the same viral particle. Our previous study showed that the G proteins of the rabies virus were incorporated on the surface of a recombinant NDV LaSota particle. An anti-rabies virus antiserum did not reduce the infectivity of the recombinant NDV [35]. The G proteins on the virion surface of the rabies virus did not mediate the infection of cells by the recombinant NDV particle [35]. The reasons for these phenomena are unclear. Another study showed that EBOV GP was incorporated into the viral particle of recombinant human parainfluenza virus 3 (hPIV3) and that the recombinant hPIV3 became more sensitive to neutralizing antibody directed against EBOV than to neutralizing antibody directed against hPIV3 [63]. Because the biological functions of the hPIV3 envelope glycoproteins could not be abolished, it was difficult to clarify whether EBOV GP on the virion surface functioned independently to mediate the infection of cells by the recombinant hPIV3 particle. In the present study, the recombinant NDV rLa-EBOVGP-cell was prepared in BHK-21 cells in the absence of trypsin, so the membrane fusion function of the F protein, essential for viral entry, was completely abolished. Therefore, we can confidently conclude that the EBOV GP that was incorporated into the viral particle independently mediated the cell entry of the recombinant NDV.
As a prototype member of the paramyxoviruses, NDV usually enters host cells by direct fusion at the plasma membrane via a pH-independent mechanism [68-70]. However, NDV can also enter host cells by an endocytic pathway [45]. It had been shown that the cellular entry of EBOV involves a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes [46,47,71]. Recently, Niemann-Pick C1, a protein involved in the endocytic pathways, has been identified as an important host factor in the cell-entry process [72,73]. In this study, the neutralization assay showed that the mixture of anti-NDV antiserum and anti-EBOV GP antiserum completely blocked the infectivity of rLa-EBOVGP, whereas either anti-NDV antiserum or anti-EBOV GP antiserum only partially blocked the infectivity of this virus. Therefore, we infer that both the NDV envelope proteins F/HN and EBOV GP contribute to the cell entry of rLa-EBOVGP. It is surprising that the inhibition of macropinocytosis almost completely abolished the infectivity of rLa-EBOVGP, whereas it did not markedly reduce the infectivity of rLa. These results indicate that the direct fusion between rLa-EBOVGP and the plasma membrane facilitated by F/HN may not allow viral entry into the cell. EBOV GP plays a major role in the cell-entry process of rLa-EBOVGP, and may predominate over NDV F/HN in the cell-entry function of this recombinant virus. The exact mechanism underlying this predominance requires further investigation. The recombinant virus rLa-EBOVGP provides an interesting model with which to explore the functional interactions between native and foreign envelope glycoproteins in one viral particle.
Although animal tests have shown that recombinant NDV expressing EBOV GP is safe for monkeys [17] and for poultry and mice (this study), safety concerns remain. Because the incorporation of EBOV GP protein into NDV particles significantly alters the behavior of the vector virus, the use of an NDV-vectored EBOV vaccine should be investigated with caution and evaluated rigorously.
Methods
Cells and viruses
The BSR-T7/5 cells for virus rescue and the BHK-21 cells for virus growth and titration were maintained in complete Dulbecco’s modified Eagle’s medium (DMEM) containing 10% fetal bovine serum (FBS). The NDV strains were propagated and titrated in 9-day-old SPF embryonated chicken eggs [44] or BHK-21 cells in the presence or absence of TPCK-trypsin (Sigma).
Plasmid construction and virus rescue
To construct a full-length recombinant genomic cDNA, the cDNA of the GP gene of Zaire EBOV was amplified from synthesized cDNA (GenBank accession no. AF086833.2) using the following primers: 5′-GACTGTTTAAACttagaaaaaaTacgggtagaaCgccaccATGGGCGTTACAGGAATATTGCAG-3′ and 5′-CTGAGTTTAAACGCTAAAAGACAAATTTGCATATACAG-3′. The GP gene was flanked by the restriction site for endonuclease PmeI (boldface letters); the NDV gene start sequence (GS, 5′-acgggtagaa-3′) and gene end sequence (GE, 5′-ttagaaaaaa-3′) are included before the optimal Kozak sequence (italic lowercase letters) and the GP sequence (italic uppercase letters). The amplified fragment was digested with PmeI and then inserted into the P–M intergenic region at nucleotide position 3165 of the NDV genome, as described previously [32]. The resultant plasmid was used for recombinant NDV rescue, as described previously [32]. The expression of EBOV GP was confirmed with an immunofluorescence assay (IFA) and western blotting. The resultant recombinant virus was designated “rLa-EBOVGP”.
Immunofluorescence assay
NDV infection was detected in cells with IFA with chicken anti-NDV antiserum, as previously described [32]. For the confocal assays, BHK-21 cells were grown in 24-well plates or plated on cover slips in dishes (35 mm diameter) and infected with rLa or rLa-EBOVGP. At 24 h after infection, the cells were fixed in prechilled 3% paraformaldehyde in phosphate-buffered saline (PBS) for 15 min at room temperature, washed three times with PBS, and then blocked with PBS containing 1% (wt/vol) bovine serum albumin at room temperature for 1 h. The cells were then incubated with mouse anti-EBOV GP antiserum (the antiserum was prepared in mice immunized with two doses of recombinant VSV expressing EBOV GP, which was generated in our laboratory) or chicken anti-NDV antiserum for 1 h at room temperature. The cells were then washed three times with PBS containing 0.05% Tween 20 and stained with a fluorescein isothiocyanate (FITC)-conjugated goat anti-mouse antibody (Sigma) or a tetramethylrhodamine isothiocyanate-conjugated rabbit anti-chicken antibody (Sigma) for 30 min. The cells were washed three times with PBS, stained with DAPI, and then analyzed with fluorescence microscopy or confocal laser microscopy. The images were acquired with a Zeiss (Thornwood, NY) Axioskop microscope equipped for epifluorescence with a Sensys charge-coupled device camera (Photometrics, Tucson, AZ) using the IPLab software (Scanalytics, Vienna, VA).
Western blotting
Egg-propagated rLa and rLa-EBOVGP were purified by sucrose gradient ultracentrifugation. The total protein (5 μg) of each purified virus was subjected to SDS–PAGE under denaturing conditions. After the proteins were transferred from the gel to nitrocellulose membrane, the target band (s) were detected with chicken anti-NDV antiserum or mouse anti-EBOV GP antiserum as the primary antibody and the corresponding horseradish-peroxidase-conjugated goat anti-chicken or goat anti-mouse immunoglobulin G as the secondary antibody. The bands were visualized with ECL Plus Western Blotting Detection Reagents (GE Health Science) on Kodak X-ray film.
Virus neutralization
Each recombinant virus (5 × 102 TCID50) was mixed with chicken anti-NDV antiserum (diluted 1:100) or mouse anti-EBOV GP antiserum (diluted 1:10) or with a mixture of chicken and mouse antisera (at the same dilutions). The viruses were also mixed with a mixture of SPF chicken serum and naïve mouse serum as the mock-treated group. The virus–serum mixtures were incubated at 37°C for 1 h and then used to infect monolayers of BHK-21 cells in a 12-well plate. At 1 h after infection, the supernatants were discarded and the cells were washed three times with DMEM. At 48 h after infection, the cells were fixed, and IFA was performed with chicken anti-NDV antiserum as the primary antibody.
Assessment of viral pathogenicity
To determine the pathogenicity of rLa-EBOVGP in poultry, MDT, ICPI, and IVPI were determined according to the OIE Manual [44]. To assess the pathogenicity of rLa-EBOVGP in mammalian cells, two groups of 10 six-week-old female Balb/c mice (Vital River, Beijing, China) were inoculated i.m. with 108 EID50 of rLa-EBOVGP or rLa, and simultaneously i.n. with 3 × 107 EID50 of rLa-EBOVGP or rLa. The third group of 10 mice was inoculated i.m. with 0.1 mL and i.n. with 0.03 mL of PBS as the mock-infection control. The mice were monitored daily to detect any weight changes, signs of illness, or death.
Chemical inhibition of virus internalization pathways
BHK-21 cells were pretreated with either the inhibitor 10 μM IPA3 (Sigma) or 10 mM MβCD (Sigma) alone or together at 37°C. To exclude the influence of HN of vector NDV virus on the internalization of the recombinant viruses, another plate of BHK-21 cells were pretreated with 800 mU/ml bacterial neuraminadase (NA, Sigma N2876) alone or together with the inhibitors at 37°C. At 1 h after treatment, the cells were washed three times and infected with 5 × 102 TCID50 of rLa or rLa-EBOVGP at 4°C for 1 h in the presence of the inhibitor(s). The cells were then washed three times on ice. DMEM containing 10% FBS was added and the samples were incubated in 37°C for 7 h. After incubation, the cells were fixed with 3% paraformaldehyde and permeabilized with 0.1% saponin. Cells infected with rLa or rLa-EBOVGP were detected with immunofluorescence assay, as described above. The mean number of flurorecent possitive cells of a minimum of 5 fields of view were counted.The data was expressed as means and standard deviations.
Ethics statements
The present study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the Ministry of Science and Technology of the People's Republic of China. The protocol was approved by the Animal Research Ethics Committee of Harbin Veterinary Research Institute, Chinese Academy of Agricultural Sciences (approval numbers 20132085 for chickens and 20132138 for mice).
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ZB designed and oversaw the experiments. ZB and ZW wrote the manuscript. BZ and JG rescued the recominant viruses and characterized the viruses. ZW carried out the neutralization assay and in vitro cell entry assay. KS, XH, WC and DK carried out the plasmids construction and animal studies. All authors have read and approved the submitted manuscript.
Contributor Information
Zhiyuan Wen, Email: zywen7@yahoo.com.
Bolin Zhao, Email: berlin0001@sina.com.
Kun Song, Email: songkun1234567@163.com.
Xule Hu, Email: xiaoguanjun258@163.com.
Weiye Chen, Email: chenweiye1980@163.com.
Dongni Kong, Email: kongdongni@hotmail.com.
Jinying Ge, Email: gjy2003@163.com.
Zhigao Bu, Email: zgbu@yahoo.com.
Acknowledgement
We thank Dr. Chinglai Yang at Emory University School of Medicine for his constructive suggestions on the experiment design and critical discussions on the manuscript. This study was supported by The National Key Technology R&D Program (2013BAD12B05).
References
- Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet. 2011;10:849–862. doi: 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoenen T, Groseth A, Falzarano D, Feldmann H. Ebola virus: unravelling pathogenesis to combat a deadly disease. Trends Mol Med. 2006;10:206–215. doi: 10.1016/j.molmed.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Feldmann H, Klenk HD, Sanchez A. Molecular biology and evolution of filoviruses. Arch Virol Suppl. 1993;10:81–100. doi: 10.1007/978-3-7091-9300-6_8. [DOI] [PubMed] [Google Scholar]
- Chan SY, Speck RF, Ma MC, Goldsmith MA. Distinct mechanisms of entry by envelope glycoproteins of Marburg and Ebola (Zaire) viruses. J Virol. 2000;10:4933–4937. doi: 10.1128/JVI.74.10.4933-4937.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito H, Watanabe S, Sanchez A, Whitt MA, Kawaoka Y. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. J Virol. 1999;10:8907–8912. doi: 10.1128/jvi.73.10.8907-8912.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A, Robison C, Goto H, Sanchez A, Murti KG, Whitt MA, Kawaoka Y. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;10:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wool-Lewis RJ, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol. 1998;10:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z, Delgado R, Xu L, Todd RF, Nabel EG, Sanchez A, Nabel GJ. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;10:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]
- Volchkov VE, Volchkova VA, Muhlberger E, Kolesnikova LV, Weik M, Dolnik O, Klenk HD. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science. 2001;10:1965–1969. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- Yang ZY, Duckers HJ, Sullivan NJ, Sanchez A, Nabel EG, Nabel GJ. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;10:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- Maruyama T, Rodriguez LL, Jahrling PB, Sanchez A, Khan AS, Nichol ST, Peters CJ, Parren PW, Burton DR. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol. 1999;10:6024–6030. doi: 10.1128/jvi.73.7.6024-6030.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson JA, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn AL, Hart MK. Epitopes involved in antibody-mediated protection from Ebola virus. Science. 2000;10:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- Sullivan NJ, Geisbert TW, Geisbert JB, Shedlock DJ, Xu L, Lamoreaux L, Custers JH, Popernack PM, Yang ZY, Pau MG. et al. Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPs. PLoS Med. 2006;10:e177. doi: 10.1371/journal.pmed.0030177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan NJ, Hensley L, Asiedu C, Geisbert TW, Stanley D, Johnson J, Honko A, Olinger G, Bailey M, Geisbert JB. et al. CD8+ cellular immunity mediates rAd5 vaccine protection against Ebola virus infection of nonhuman primates. Nat Med. 2011;10:1128–1131. doi: 10.1038/nm.2447. [DOI] [PubMed] [Google Scholar]
- Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA. et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med. 2005;10:786–790. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- Qiu X, Fernando L, Alimonti JB, Melito PL, Feldmann F, Dick D, Stroher U, Feldmann H, Jones SM. Mucosal immunization of cynomolgus macaques with the VSVDeltaG/ZEBOVGP vaccine stimulates strong ebola GP-specific immune responses. PLoS One. 2009;10:e5547. doi: 10.1371/journal.pone.0005547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNapoli JM, Yang L, Samal SK, Murphy BR, Collins PL, Bukreyev A. Respiratory tract immunization of non-human primates with a Newcastle disease virus-vectored vaccine candidate against Ebola virus elicits a neutralizing antibody response. Vaccine. 2010;10:17–25. doi: 10.1016/j.vaccine.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaney JE, Wirblich C, Papaneri AB, Johnson RF, Myers CJ, Juelich TL, Holbrook MR, Freiberg AN, Bernbaum JG, Jahrling PB. et al. Inactivated or live-attenuated bivalent vaccines that confer protection against rabies and Ebola viruses. J Virol. 2011;10:10605–10616. doi: 10.1128/JVI.00558-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander DJ. Newcastle Disease. American Association for Avian Pathologists: Kennett Square, PA; 1989. [Google Scholar]
- Peeters BP, de Leeuw OS, Koch G, Gielkens AL. Rescue of Newcastle disease virus from cloned cDNA: evidence that cleavability of the fusion protein is a major determinant for virulence. J Virol. 1999;10:5001–5009. doi: 10.1128/jvi.73.6.5001-5009.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda A, Huang Z, Elankumaran S, Rockemann DD, Samal SK. Role of fusion protein cleavage site in the virulence of Newcastle disease virus. Microb Pathog. 2004;10:1–10. doi: 10.1016/j.micpath.2003.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charan S, Mahajan VM, Agarwal LP. Newcastle disease virus antibodies in human sera. Indian J Med Res. 1981;10:303–307. [PubMed] [Google Scholar]
- Schirrmacher V, Haas C, Bonifer R, Ahlert T, Gerhards R, Ertel C. Human tumor cell modification by virus infection: an efficient and safe way to produce cancer vaccine with pleiotropic immune stimulatory properties when using Newcastle disease virus. Gene Ther. 1999;10:63–73. doi: 10.1038/sj.gt.3300787. [DOI] [PubMed] [Google Scholar]
- Morrison T, McQuain C, Sergel T, McGinnes L, Reitter J. The role of the amino terminus of F1 of the Newcastle disease virus fusion protein in cleavage and fusion. Virology. 1993;10:997–1000. doi: 10.1006/viro.1993.1214. [DOI] [PubMed] [Google Scholar]
- Nagai Y, Klenk HD, Rott R. Proteolytic cleavage of the viral glycoproteins and its significance for the virulence of Newcastle disease virus. Virology. 1976;10:494–508. doi: 10.1016/0042-6822(76)90178-1. [DOI] [PubMed] [Google Scholar]
- Alexander D. Newcastle Disease and Other Avian Paramyxoviridae Infections. Ames: Iowa State University Press; 1997. [Google Scholar]
- Ge J, Tian G, Zeng X, Jiang Y, Chen H, Bua Z. Generation and evaluation of a Newcastle disease virus-based H9 avian influenza live vaccine. Avian Dis. 2010;10:294–296. doi: 10.1637/8731-032509-ResNote.1. [DOI] [PubMed] [Google Scholar]
- Nakaya T, Cros J, Park MS, Nakaya Y, Zheng H, Sagrera A, Villar E, Garcia-Sastre A, Palese P. Recombinant Newcastle disease virus as a vaccine vector. J Virol. 2001;10:11868–11873. doi: 10.1128/JVI.75.23.11868-11873.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNapoli JM, Kotelkin A, Yang L, Elankumaran S, Murphy BR, Samal SK, Collins PL, Bukreyev A. Newcastle disease virus, a host range-restricted virus, as a vaccine vector for intranasal immunization against emerging pathogens. Proc Natl Acad Sci USA. 2007;10:9788–9793. doi: 10.1073/pnas.0703584104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Huang Z, Yang L, Elankumaran S, St Claire M, Murphy BR, Samal SK, Collins PL. Recombinant newcastle disease virus expressing a foreign viral antigen is attenuated and highly immunogenic in primates. J Virol. 2005;10:13275–13284. doi: 10.1128/JVI.79.21.13275-13284.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNapoli JM, Nayak B, Yang L, Finneyfrock BW, Cook A, Andersen H, Torres-Velez F, Murphy BR, Samal SK, Collins PL, Bukreyev A. Newcastle disease virus-vectored vaccines expressing the hemagglutinin or neuraminidase protein of H5N1 highly pathogenic avian influenza virus protect against virus challenge in monkeys. J Virol. 2010;10:1489–1503. doi: 10.1128/JVI.01946-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge J, Deng G, Wen Z, Tian G, Wang Y, Shi J, Wang X, Li Y, Hu S, Jiang Y. et al. Newcastle disease virus-based live attenuated vaccine completely protects chickens and mice from lethal challenge of homologous and heterologous H5N1 avian influenza viruses. J Virol. 2007;10:150–158. doi: 10.1128/JVI.01514-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattar SK, Samal S, Devico AL, Collins PL, Samal SK. Newcastle disease virus expressing human immunodeficiency virus type 1 envelope glycoprotein induces strong mucosal and serum antibody responses in Guinea pigs. J Virol. 2011;10:10529–10541. doi: 10.1128/JVI.05050-11. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Carnero E, Li W, Borderia AV, Moltedo B, Moran T, Garcia-Sastre A. Optimization of human immunodeficiency virus gag expression by newcastle disease virus vectors for the induction of potent immune responses. J Virol. 2009;10:584–597. doi: 10.1128/JVI.01443-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge J, Wang X, Tao L, Wen Z, Feng N, Yang S, Xia X, Yang C, Chen H, Bu Z. Newcastle disease virus-vectored rabies vaccine is safe, highly immunogenic, and provides long-lasting protection in dogs and cats. J Virol. 2011;10:8241–8252. doi: 10.1128/JVI.00519-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong D, Wen Z, Su H, Ge J, Chen W, Wang X, Wu C, Yang C, Chen H, Bu Z. Newcastle disease virus-vectored Nipah encephalitis vaccines induce B and T cell responses in mice and long-lasting neutralizing antibodies in pigs. Virology. 2012;10:327–335. doi: 10.1016/j.virol.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Kortekaas J, de Boer SM, Kant J, Vloet RP, Antonis AF, Moormann RJ. Rift Valley fever virus immunity provided by a paramyxovirus vaccine vector. Vaccine. 2010;10:4394–4401. doi: 10.1016/j.vaccine.2010.04.048. [DOI] [PubMed] [Google Scholar]
- Kortekaas J, Dekker A, de Boer SM, Weerdmeester K, Vloet RP, de Wit AA, Peeters BP, Moormann RJ. Intramuscular inoculation of calves with an experimental Newcastle disease virus-based vector vaccine elicits neutralizing antibodies against Rift Valley fever virus. Vaccine. 2010;10:2271–2276. doi: 10.1016/j.vaccine.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Khattar SK, Collins PL, Samal SK. Immunization of cattle with recombinant Newcastle disease virus expressing bovine herpesvirus-1 (BHV-1) glycoprotein D induces mucosal and serum antibody responses and provides partial protection against BHV-1. Vaccine. 2010;10:3159–3170. doi: 10.1016/j.vaccine.2010.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Collins PL. Newcastle disease virus as a vaccine vector for humans. Curr Opin Mol Ther. 2008;10:46–55. [PubMed] [Google Scholar]
- Pecora AL, Rizvi N, Cohen GI, Meropol NJ, Sterman D, Marshall JL, Goldberg S, Gross P, O’Neil JD, Groene WS. et al. Phase I trial of intravenous administration of PV701, an oncolytic virus, in patients with advanced solid cancers. J Clin Oncol. 2002;10:2251–2266. doi: 10.1200/JCO.2002.08.042. [DOI] [PubMed] [Google Scholar]
- Ockert D, Schirrmacher V, Beck N, Stoelben E, Ahlert T, Flechtenmacher J, Hagmuller E, Buchcik R, Nagel M, Saeger HD. Newcastle disease virus-infected intact autologous tumor cell vaccine for adjuvant active specific immunotherapy of resected colorectal carcinoma. Clin Cancer Res. 1996;10:21–28. [PubMed] [Google Scholar]
- Karcher J, Dyckhoff G, Beckhove P, Reisser C, Brysch M, Ziouta Y, Helmke BH, Weidauer H, Schirrmacher V, Herold-Mende C. Antitumor vaccination in patients with head and neck squamous cell carcinomas with autologous virus-modified tumor cells. Cancer Res. 2004;10:8057–8061. doi: 10.1158/0008-5472.CAN-04-1545. [DOI] [PubMed] [Google Scholar]
- OIE. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals 2011. Paris: Office International des Epizooties; 2011. [Google Scholar]
- Cantin C, Holguera J, Ferreira L, Villar E, Munoz-Barroso I. Newcastle disease virus may enter cells by caveolae-mediated endocytosis. J Gen Virol. 2007;10:559–569. doi: 10.1099/vir.0.82150-0. [DOI] [PubMed] [Google Scholar]
- Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog. 2010;10:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog. 2010;10:e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleksandrowicz P, Marzi A, Biedenkopf N, Beimforde N, Becker S, Hoenen T, Feldmann H, Schnittler HJ. Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. J Infect Dis. 2011;10(Suppl 3):S957–S967. doi: 10.1093/infdis/jir326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JA. Shaping cups into phagosomes and macropinosomes. Nat Rev Mol Cell Biol. 2008;10:639–649. doi: 10.1038/nrm2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr MC, Teasdale RD. Defining macropinocytosis. Traffic. 2009;10:364–371. doi: 10.1111/j.1600-0854.2009.00878.x. [DOI] [PubMed] [Google Scholar]
- Mercer J, Helenius A. Virus entry by macropinocytosis. Nat Cell Biol. 2009;10:510–520. doi: 10.1038/ncb0509-510. [DOI] [PubMed] [Google Scholar]
- Rodal SK, Skretting G, Garred O, Vilhardt F, van Deurs B, Sandvig K. Extraction of cholesterol with methyl-beta-cyclodextrin perturbs formation of clathrin-coated endocytic vesicles. Mol Biol Cell. 1999;10:961–974. doi: 10.1091/mbc.10.4.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subtil A, Gaidarov I, Kobylarz K, Lampson MA, Keen JH, McGraw TE. Acute cholesterol depletion inhibits clathrin-coated pit budding. Proc Natl Acad Sci USA. 1999;10:6775–6780. doi: 10.1073/pnas.96.12.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingartl HM, Berhane Y, Caswell JL, Loosmore S, Audonnet JC, Roth JA, Czub M. Recombinant nipah virus vaccines protect pigs against challenge. J Virol. 2006;10:7929–7938. doi: 10.1128/JVI.00263-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odunsi K, Matsuzaki J, Karbach J, Neumann A, Mhawech-Fauceglia P, Miller A, Beck A, Morrison CD, Ritter G, Godoy H. et al. Efficacy of vaccination with recombinant vaccinia and fowlpox vectors expressing NY-ESO-1 antigen in ovarian cancer and melanoma patients. Proc Natl Acad Sci USA. 2012;10:5797–5802. doi: 10.1073/pnas.1117208109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cebere I, Dorrell L, McShane H, Simmons A, McCormack S, Schmidt C, Smith C, Brooks M, Roberts JE, Darwin SC. et al. Phase I clinical trial safety of DNA- and modified virus Ankara-vectored human immunodeficiency virus type 1 (HIV-1) vaccines administered alone and in a prime-boost regime to healthy HIV-1-uninfected volunteers. Vaccine. 2006;10:417–425. doi: 10.1016/j.vaccine.2005.08.041. [DOI] [PubMed] [Google Scholar]
- Vaccari M, Halwani R, Patterson LJ, Boasso A, Beal J, Tryniszewska E, Hryniewicz A, Venzon D, Haddad EK, El-Far M. et al. Antibodies to gp120 and PD-1 expression on virus-specific CD8+ T cells in protection from simian AIDS. J Virol. 2013;10:3526–3537. doi: 10.1128/JVI.02686-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park MS, Garcia-Sastre A, Cros JF, Basler CF, Palese P. Newcastle disease virus V protein is a determinant of host range restriction. J Virol. 2003;10:9522–9532. doi: 10.1128/JVI.77.17.9522-9532.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park MS, Shaw ML, Munoz-Jordan J, Cros JF, Nakaya T, Bouvier N, Palese P, Garcia-Sastre A, Basler CF. Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J Virol. 2003;10:1501–1511. doi: 10.1128/JVI.77.2.1501-1511.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z, Krishnamurthy S, Panda A, Samal SK. Newcastle disease virus V protein is associated with viral pathogenesis and functions as an alpha interferon antagonist. J Virol. 2003;10:8676–8685. doi: 10.1128/JVI.77.16.8676-8685.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blach-Olszewska Z. Interferon induction by Newcastle disease virus in mice. Arch Immunol Ther Exp (Warsz) 1970;10:418–441. [PubMed] [Google Scholar]
- Brehm G, Kirchner H. Analysis of the interferons induced in mice in vivo and in macrophages in vitro by Newcastle disease virus and by polyinosinic-polycytidylic acid. J Interferon Res. 1986;10:21–28. doi: 10.1089/jir.1986.6.21. [DOI] [PubMed] [Google Scholar]
- Bukreyev A, Yang L, Zaki SR, Shieh WJ, Rollin PE, Murphy BR, Collins PL, Sanchez A. A single intranasal inoculation with a paramyxovirus-vectored vaccine protects guinea pigs against a lethal-dose Ebola virus challenge. J Virol. 2006;10:2267–2279. doi: 10.1128/JVI.80.5.2267-2279.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunz S, Rojek JM, Perez M, Spiropoulou CF, Oldstone MB. Characterization of the interaction of lassa fever virus with its cellular receptor alpha-dystroglycan. J Virol. 2005;10:5979–5987. doi: 10.1128/JVI.79.10.5979-5987.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogino M, Ebihara H, Lee BH, Araki K, Lundkvist A, Kawaoka Y, Yoshimatsu K, Arikawa J. Use of vesicular stomatitis virus pseudotypes bearing hantaan or seoul virus envelope proteins in a rapid and safe neutralization test. Clin Diagn Lab Immunol. 2003;10:154–160. doi: 10.1128/CDLI.10.1.154-160.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaku Y, Noguchi A, Marsh GA, McEachern JA, Okutani A, Hotta K, Bazartseren B, Fukushi S, Broder CC, Yamada A. et al. A neutralization test for specific detection of Nipah virus antibodies using pseudotyped vesicular stomatitis virus expressing green fluorescent protein. J Virol Methods. 2009;10:7–13. doi: 10.1016/j.jviromet.2009.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Ge J, Hu S, Wang Q, Wen Z, Chen H, Bu Z. Efficacy of DNA immunization with F and G protein genes of Nipah virus. Ann N Y Acad Sci. 2006;10:243–245. doi: 10.1196/annals.1373.029. [DOI] [PubMed] [Google Scholar]
- Lamb RA, Kolakofsky D, editor. Fields Virology. 3. Philadelphia: Lippincott-Williams & Wilkins; 2001. [Google Scholar]
- Hernandez LD, Hoffman LR, Wolfsberg TG, White JM. Virus-cell and cell-cell fusion. Annu Rev Cell Dev Biol. 1996;10:627–661. doi: 10.1146/annurev.cellbio.12.1.627. [DOI] [PubMed] [Google Scholar]
- Lamb RA. Paramyxovirus fusion: a hypothesis for changes. Virology. 1993;10:1–11. doi: 10.1006/viro.1993.1561. [DOI] [PubMed] [Google Scholar]
- Quinn K, Brindley MA, Weller ML, Kaludov N, Kondratowicz A, Hunt CL, Sinn PL, McCray PB Jr, Stein CS, Davidson BL. et al. Rho GTPases modulate entry of Ebola virus and vesicular stomatitis virus pseudotyped vectors. J Virol. 2009;10:10176–10186. doi: 10.1128/JVI.00422-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G. et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;10:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI. et al. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. Embo J. 2012;10:1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]