Abstract
Background and Purpose
Recent advances in distal sensor technologies have made distal sensor ureteroscopes both commercially and technically feasible. We evaluated performance characteristics and optics of a new generation distal sensor Flex-XC (XC) and a standard flexible fiberoptic ureteroscope Flex-X2 (X2), both from Karl Storz, Tuttlingen, Germany.
Materials and Methods
The ureteroscopes were compared for active deflection, irrigation flow, and optical characteristics. Each ureteroscope was evaluated with an empty working channel and with various accessories. Optical characteristics (resolution, grayscale imaging, and color representation) were measured using United States Air Force test targets. We digitally recorded a renal porcine ureteroscopy and laser ablation of a stone with the X2 and with the XC. Edited footage of the recorded procedure was shown to different expert surgeons (n=8) on a high-definition monitor for evaluation by questionnaire for image quality and performance.
Results
The XC had a higher resolution than the X2 at 20 and 10 mm 3.17 lines/mm vs 1.41 lines/mm, 10.1 vs 3.56, respectively (P=0.003, P=0.002). Color representation was better in the XC. There was no difference in contrast quality between the two ureteroscopes. For each individual ureteroscope, the upward deflection was greater than the downward deflection both with and without accessories. When compared with the X2, the XC manifested superior deflection and flow (P<0.0005, P<0.05) with and without accessory present in the working channel. Observers deemed the distal sensor ureteroscope superior in visualization in clear and bloody fields, as well as for illumination (P=0.0005, P=0.002, P=0.0125).
Conclusions
In this in vitro and porcine evaluation, the distal sensor ureteroscope provided significantly improved resolution, color representation, and visualization in the upper urinary tract compared with a standard fiberoptic ureteroscope. The overall deflection was also better in the XC, and deflection as well as flow rate was less impaired by the various accessories.
Introduction
Recent advances in distal sensor optics and endoscope design have improved the urologist's ability to perform ureteroscopic procedures for diagnosis and management of upper tract renal pathology. Initial introduction of distal sensor cystoscopes revealed that these endoscopes show improved endoscopic vision by better resolution, contrast discrimination, and red color differentiation.1 Quale and colleagues2 demonstrated in an in vitro study that distal sensor cystoscopes improve the visibility in a simulated challenging working environment compared with a standard fiberoptic cystoscope. Distal sensor technology has improved such that the contemporary metal oxide sensors (CMOS) and charge coupled devices (CCD) chips can now be manufactured at a size at which distal sensor ureteroscope manufacture is both technically and commercially feasible.
Contemporary fiberoptic flexible ureterosopes offer an outer diameter of the distal tip of 5.3F to 8.7F, a 3.6F sized single working channel, and optics based on fragile fiberoptic fibers. The resolution of a standard flexible fiberoptic ureteroscope, determined by the number of individual fibers in the fiberoptic bundle (between 3400 and 5000), is limited by the shaft diameter.3
Recently, distal sensor ureteroscopes with an 8.5F outer diameter have been introduced into clinical practice. The Flex XC ureteroscope (Karl Storz, Tuttlingen, Germany) uses a CMOS sensor and an integrated light emitting diode to produce an image (Figs. 1, 2). We measured and compared the performance characteristics and optics of the XC with a standard flexible fiberoptic ureteroscope, the X2 (Karl Storz, Tuttlingen, Germany).
FIG. 1.
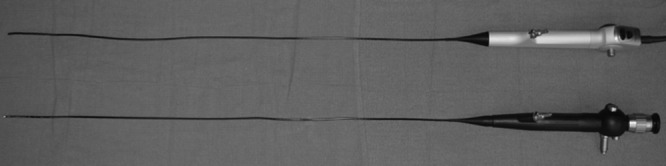
Storz flexible ureteroscopes XC and X2.
FIG. 2.

Comparison of distal tip design of X2 (left) and XC (right).
Materials and Methods
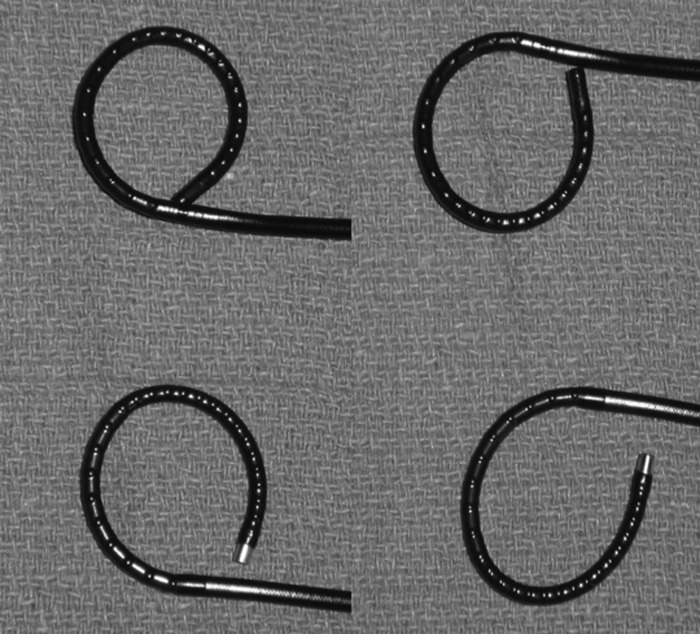
The Flex-X2 was compared with a new Flex-XC ureteroscope. The two brand-new ureteroscopes were subjectively and objectively assessed. Measured data included distal tip and shaft diameter, active upward and downward deflection (up and down) (Fig. 3), irrigation flow rates (mL/sec), and optical characteristics.
FIG. 3.
XC up and downward deflection; X2 up and downward deflection.
Measurement of upward and downward deflection was made by photocopying the ureteroscope completely deflected and taking measurements using a protractor as described by Parkin and coworkers.4 Measurements for each ureteroscope and each instrument were taken three times. The intersection angle between the tangents to the active deflection segment and deflected tip was considered the deflection angle.5 Each ureteroscope was evaluated for flow and deflection with an empty working channel and with various accessories. Accessories included the following 200 μm and 273 μm OptiLite single use holmium laser fiber (Cook Urological Inc, Spencer, IN), 3.2F Delta Wire Grasper (Cook Urological Inc, Spencer, IN), 1.7F NCompass Nitinol Stone Extractor, 2.2F NGage Nitinol Stone Extractor (Cook Urological Inc, Spencer, IN), and 200 μm/272 μm ScopeSafe Fiber with Scope Guardian Sheath (Optical Integrety Inc, Panama City Beach, FL).
Irrigation flow was measured by connecting the working channel inlet of each ureteroscope to a pump irrigation system set to a pressure of 100 mm Hg. For each ureteroscope, the system was allowed to equilibrate for 5 minutes before flow measurements were recorded.6
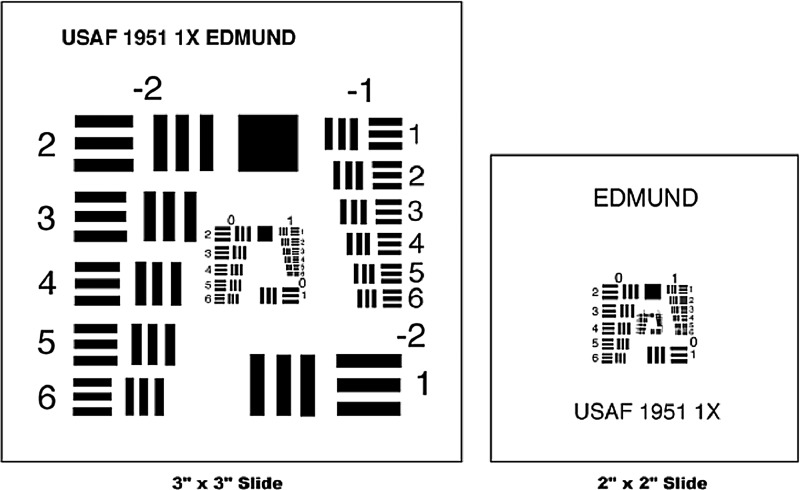
Optical characteristics, including resolution, grayscale imaging, and color representation, were measured using test targets (Edmund Optics, Barrington, NJ). Resolution was measured using a United States Air Force (UASF) resolving test pattern (Stock Number NT53-714, Edmund Optics, Barrington, NJ) (Fig. 4); the data were analyzed in accordance with the manufacturer's instructions. USAF 1951 Resolution target is compliant with US government specification MIL-STD-150. Resolution was defined per test target manufacturer as an imaging system ability to distinguish object detail. The test target measures resolution in terms of line pairs per millimeter. The USAF 1951 Resolution Target uses a repeating series of parallel bars decreasing in size. These bars are separated into group and element numbers. System resolution is defined as the highest group and element in which the three bars can still be distinguished.
FIG. 4.
USAF 1951. From Web site of Edmund Optics, Barrington, NJ.
Contrast was assessed using a grayscale gradient having 15 density steps from a density of 0.07 (low) to 1.5 (high) corresponding to optical density increments of 0.10. The difference between density steps is linear, which leads to a logarithmic change in diffuse reflectivity. The two ureteroscopes were positioned at a 20-mm distance above the target, directly over the darkest square, and were then moved slowly along the scale toward the lightest square, until the observer noted an inability to distinguish a difference between two steps of contrast.
Color representation was measured using a Gregtag Macbeth Color Checker Target (Stock Number NT56-292, Edmund Optics, Barrington, NJ) (Fig. 5). The ureteroscopes were evaluated 10- and 20-mm away from the test target and were tested in a laboratory setting using a new Storz tower with a high definition (HD) monitor and an HD recording system.
FIG. 5.
Color Checker. From Web site of Edmund Optics, Barrington, NJ.
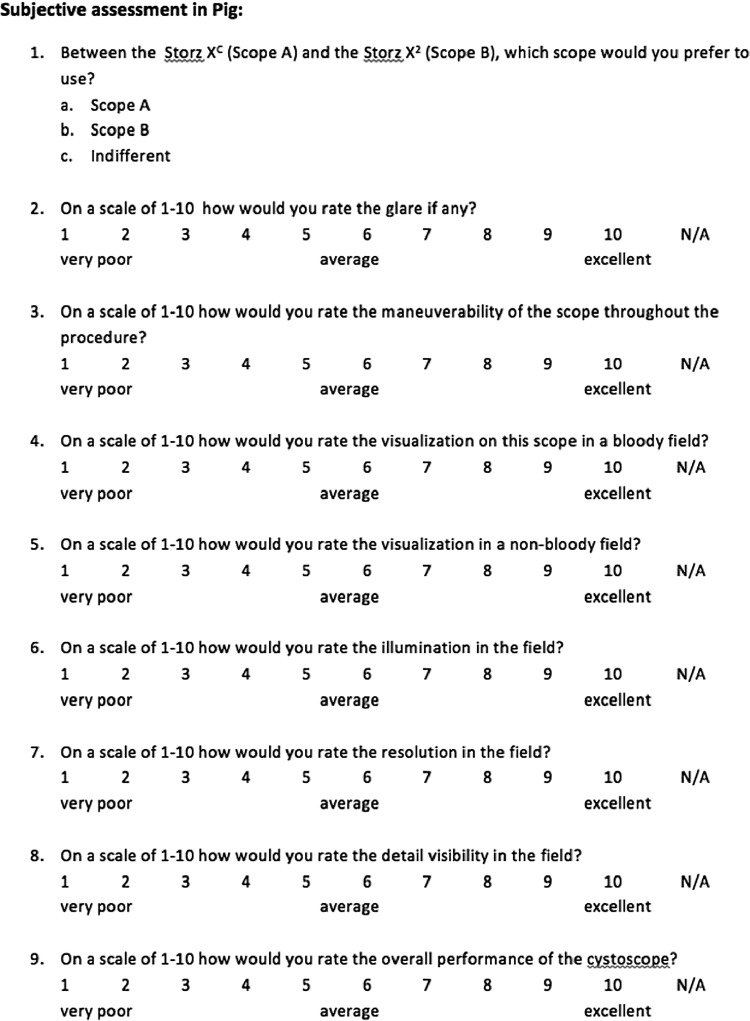
In addition, calcium oxalate stones were placed into the porcine renal pelvis in a retrograde manner through an access sheath. We created a standardized, HD digital recording of the laser ablation of the stones using both the X2 and also the XC. The laser was then used to purposely ablate the wall of the renal pelvis and supporting renal parenchyma to create active bleeding. Edited footage including stone comminution, clear renal endoscopy, and endoscopy in a bloody field were shown to different expert surgeons (n=8) on a HD monitor for evaluation by questionnaire (Addendum) for image quality and performance.
Addendum. Questionnaire
Statistical comparison for continuous variables were analyzed using a Student t test and a two-way analysis of variance. All subjective rankings were compared with the Mann-Whitney rank sum test. All analyses were performed with SPSS version 19 (IBM Corporation, Armonk, NY).
Results
Technical specifications
The Flex-X2 has a outer diameter of the distal tip of 7.5F and a shaft diameter of 7.5F, compared with 8.5F and 8.4F for the Flex-XC, respectively. Both ureteroscopes have a working channel size of 3.6F.
Deflection
Table 1 demonstrates deflection in up and downward direction for the two ureteroscopes with several instruments in the working channel. The results show a significant higher angle of maximum tip deflection (up and down) for the XC (296.83±0.29 up, 292.67±0.29 down for the XC, 279.83±0.29 and 273.50±0.87 for the X2, respectively) and significantly less deflection for X2 than for XC under all conditions (working channel with accessories) (P<0.0005).
Table 1.
Angles of Deflection
| |
|
X2 |
XC |
|
||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t test P value | ||
| Empty | Up | 279.83 | 0.29 | 296.83 | 0.29 | <0.0005 |
| Down | 273.50 | 0.87 | 292.67 | 0.29 | <0.0005 | |
| Laser 200 μm | Up | 269.33 | 0.29 | 289.17 | 0.29 | <0.0005 |
| Down | 264.33 | 0.58 | 286.17 | 0.29 | <0.0005 | |
| Laser 273 μm | Up | 245.83 | 0.29 | 256.83 | 0.29 | <0.0005 |
| Down | 240.33 | 0.29 | 250.17 | 0.29 | <0.0005 | |
| Delta Wire Grasper (3.2F) | Up | 176.33 | 0.29 | 188.83 | 0.29 | <0.0005 |
| Down | 170.83 | 0.29 | 186.00 | 0.50 | <0.0005 | |
| 1.7F Nitinol Stone Extractor | Up | 272.67 | 0.29 | 295.17 | 0.29 | <0.0005 |
| Down | 268.00 | 0.00 | 290.33 | 0.29 | n/a | |
| 2.2F Nitinol Stone Extractor | Up | 252.33 | 0.29 | 272.50 | 0.50 | <0.0005 |
| Down | 245.17 | 0.29 | 268.00 | 0.50 | <0.0005 | |
SD=standard deviation.
The maximum reduction in deflection of both ureteroscopes was observed by a 3.2F Delta Wire Grasper and the minimum reduction by 1.7F NCompass Nitinol Stone Extractor. The insertion of the 1.7F NCompass Nitinol Stone Extractor resulted in an approximate reduction in deflection (up/down) of 48%/45% for the XC and a 52%/55% for the X2, likewise the 3.2F Grasper in a 98.5%/99% reduction and a 99%/99% reduction. The comparison between upward and downward deflection shows that the deflection is significantly less for downward than for upward deflection, and the difference between an empty ureteroscope and ureteroscope with accessories is greater for downward deflection then for upward deflection (Table 2). The X2 manifested less diminishment of deflection with instruments in the working channel compared with the XC (P<0.0005 combined for up and down deflection) (Table 3).
Table 2.
Comparison Between Upward and Downward Deflection
| |
|
X2 |
XC |
|
||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Interaction P value | ||
| Empty | Up | 279.83 | 0.29 | 296.83 | 0.29 | |
| Down | 273.50 | 0.87 | 292.67 | 0.29 | 0.0056 | |
| Laser 200 μm | Up | 269.33 | 0.29 | 289.17 | 0.29 | |
| Down | 264.33 | 0.58 | 286.17 | 0.29 | 0.0019 | |
| Laser 273 μm | Up | 245.83 | 0.29 | 256.83 | 0.29 | |
| Down | 240.33 | 0.29 | 250.17 | 0.29 | 0.0081 | |
| Delta Wire Grasper (3.2F) | Up | 176.33 | 0.29 | 188.83 | 0.29 | |
| Down | 170.83 | 0.29 | 186.00 | 0.50 | 0.0002 | |
| 1.7F Nitinol Stone Extractor | Up | 272.67 | 0.29 | 295.17 | 0.29 | |
| Down | 268.00 | 0.00 | 290.33 | 0.29 | 0.5796 | |
| 2.2F Nitinol Stone Extractor | Up | 252.33 | 0.29 | 272.50 | 0.50 | |
| Down | 245.17 | 0.29 | 268.00 | 0.50 | 0.0005 | |
SD=standard deviation.
Table 3.
Difference in Deflection Between Empty Channel and Channel with Accessory Between the Two Ureteroscopes (Analysis of Variance, P value for Combined Up and Down)
| |
|
X2 |
XC |
|
||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Interaction P value | ||
| Empty | Up | 279.83 | 0.29 | 296.83 | 0.29 | |
| Down | 273.50 | 0.87 | 292.67 | 0.29 | ||
| Laser 200 μm | Up | 269.33 | 0.29 | 289.17 | 0.29 | |
| Down | 264.33 | 0.58 | 286.17 | 0.29 | <0.0005 | |
| Laser 273 μm | Up | 245.83 | 0.29 | 256.83 | 0.29 | |
| Down | 240.33 | 0.29 | 250.17 | 0.29 | <0.0005 | |
| Delta Wire Grasper (3.2F) | Up | 176.33 | 0.29 | 188.83 | 0.29 | |
| Down | 170.83 | 0.29 | 186.00 | 0.50 | <0.0005 | |
| 1.7F Nitinol Stone Extractor | Up | 272.67 | 0.29 | 295.17 | 0.29 | |
| Down | 268.00 | 0.00 | 290.33 | 0.29 | <0.0005 | |
| 2.2F Nitinol Stone Extractor | Up | 252.33 | 0.29 | 272.50 | 0.50 | |
| Down | 245.17 | 0.29 | 268.00 | 0.50 | <0.0005 | |
SD=standard deviation.
Flow rate
The XC had better flow under all conditions. (P<0.05) Irrigation flow was most diminished by the 3.2F Delta Wire Grasper and least impaired by the 200 μm OptiLite single use holmium laser fiber for both ureteroscopes (Table 2). The insertion of the 200 μm laser fiber resulted in an approximate reduction in flow rates of 48% for the XC and 52% for the X2, likewise the 3.2F Grasper in a 98.5% reduction and a 99% reduction for these ureteroscopes, respectively (Table 4).
Table 4.
Irrigation Flow Rates mL/min (100 mm Hg Normal Saline)
| |
|
X2 |
XC |
|
||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Interaction P value | ||
| Empty | Flow | 59.33 | 0.29 | 62.83 | 0.58 | 0.0007 |
| Laser 200 μm | Flow | 28.33 | 0.29 | 32.50 | 0.00 | n/a |
| Laser 273 μm | Flow | 26.50 | 0.00 | 28.00 | 0.00 | n/a |
| Delta Wire Grasper (3.2F) | Flow | 0.50 | 0.10 | 0.97 | 0.06 | 0.0022 |
| 1.7F Nitinol Stone Extractor | Flow | 16.336.83 | 0.29 | 18.33 | 0.29 | 0.0011 |
| 1.7F Nitinol Stone Extractor | Flow | 0.29 | 8.83 | 0.29 | 0.0011 | |
SD=standard deviation.
Optical characteristics
The XC had a higher resolution power on the USAF test chart than the X2 under all conditions—at 20 and 10 mm 3.17 line pairs/mm vs 1.41 line pairs/mm, and 10.1 vs 3.56, respectively (P=0.003, P=0.002). The XC was slightly better than the X2 ureteroscope for color representation, but contrast evaluation was similar for both ureteroscopes (Table 5). Observers deemed the distal sensor ureteroscope superior in visualization in clear and bloody fields as well as for illumination (P=0.0005, P=0.002, P=0.0125). The viewers' interpretation of maneuverability was comparable between the X2 and the XC, but the overall handling performance was also superior in the distal sensor ureteroscope (P=1.00, P=0.004) (Table 6).
Table 5.
Comparing Optical Results for Storz XC vs Storz X2
| Storz XC | Storz X2 | P value | |
|---|---|---|---|
| Resolution (lines/mm) at | |||
| 10 mm | 3.17 | 1.41 | 0.003 |
| 20 mm | 10.10 | 3.56 | 0.002 |
| Grayscale imaging | Equal | Equal | |
| Color reproducibility | Slightly better | ||
| Pixel | 60,000.00 | 4000.00 | |
Table 6.
Results Questionnaire
| Mean (XC) | SD | Mean (X2) | SD | P value | |
|---|---|---|---|---|---|
| Superior scope | Scope XC | Scope X2 | |||
| Glare | 8.88 | 0.64 | 6.50 | 0.53 | 0.0005 |
| Maneuverability | 9.50 | 0.53 | 9.50 | 0.53 | 1.00 |
| Visualization bloody field | 9.38 | 0.52 | 6.63 | 0.74 | 0.0005 |
| Visualization nonbloody field | 9.50 | 0.53 | 7.75 | 0.89 | 0.0021 |
| Illumination | 9.25 | 0.89 | 7.88 | 0.83 | 0.0125 |
| Resolution | 9.50 | 0.53 | 6.13 | 0.35 | 0.0004 |
| Visibility | 9.13 | 0.35 | 6.38 | 0.52 | 0.0003 |
| Overall performance | 9.25 | 0.46 | 7.25 | 0.46 | 0.0004 |
SD=standard deviation.
Discussion
Ureteroscopic diagnosis and management has become a minimally invasive standard for the management of upper tract renal pathology.2,7 The introduction of distal sensor technology in cystoscopes has led to a significant improvement in visual optics. Distal sensor technology does not require white balancing and camera focusing; it also eliminates the need for an external camera and light source, which significantly reduces the weight of the ureteroscope. The Storz XC weights 320 g compared with the 576 g of the Storz X2 fiberoptic ureteroscope with external camera. This 55% reduction in weight may result in better handling during endoscopic procedures, although this theoretic advantage was not evaluated in the current study.
The current study demonstrates that the CMOS ureteroscope provides significant improved visualization in the upper tract in both clear and simulated bloody conditions. Similarly, the distal sensor ureteroscope demonstrated better deflection, and surgeons rated the overall handling performance to be superior. The perceived superiority in maneuverability may have been a function of improved optics. Indeed, in a recent clinical comparison of more than 1000 cystoscopy procedures performed with fiberoptic and distal sensor cystoscopes, Okhunov and colleagues8 demonstrated clearly that while these cystoscopes had no difference in deflection characteristics, surgeons perceived that the distal sensor cystoscopes were significantly more maneuverable in clinical practice. The authors concluded that the superior optics gave the sense of greater maneuverability despite similar deflection performance characteristics. This may be the case in the current study as well.
One of the most important improvements of the distal sensor technology is the increased resolution of the XC compared with the standard fiberoptic endoscope.9 Optical resolution as measured by the USAF is determined by measuring the scope's ability to differentiate between two different lines, or line pairs, at a certain distance; the greater the number of line pairs per mm, the greater the resolution of the scope. In the current study, when the XC was compared with the X2, at a set distance of 20 mm and 10 mm, the XC demonstrated a clear superiority in resolution (3.17 vs 1.41 line pairs/mm and 10.1 vs 3.56 line pairs/mm, respectively (P=0.003, P=0.002).
The improved resolution in combination with the better color representation may have important clinical implications in detection, surveillance, and treatment of transitional-cell carcinoma in the upper urinary tract. Furthermore, the X C is uniquely capable of a threefold digital magnification of the image, a feature that may have an impact on the surgeon's ability to detect very small upper tract recurrences or residual disease. Recently, several articles have shown that optics and performance are better for distal sensor cystoscopes and ureteroscopes, but reliable clinical studies showing improved efficacy for tumor detection and surveillance are still lacking.3,10
Despite the fact that the manufacturer specifies that the XC and X2 have the same working channel size of 3.6F, the irrigation flow rate is significantly less for the X2 compared with the XC under all conditions. It is feasible that internal components of the ureteroscope may be altering the width of the working channel in different angles of deflection; a possible impression of the working channel by fiberoptic fibers may lead to a measurable reduction in flow and therefore to worse visualization during the procedure. Consultation with the manufacturer about the internal components of the X2 vs XC suggested that this may be the result of a small metal bar at the intersection of the working and irrigation channel that may cause turbulence in the X2. The result is no laminar flow with a measurable flow reduction.
In our ex vivo evaluation, the XC showed a significantly higher angle of maximum tip deflection than the fiberoptic ureteroscope. Despite the better overall deflection for the XC, the deflection showed less change from empty working channel to each accessory for X2 than for XC. With regard to deflection, the manufacturer suggested that both endoscopes are manufactured by hand, and that this may lead to small variations in performance such as upward and downward deflection and flow. Regarding the maximum tip deflection, all vertebrae (structural supports of the ureteroscope) in the XC have the same diameter with a larger distance between the individual vertebrae, whereas in the X2 the vertebral bodies have two different diameters, and a lower distance between the vertebra, which may have been responsible for the slightly lower performance in overall deflection. In addition, the friction between the vertebrae during the active deflection is because of the smaller components and lower distance of the vertebral bodies higher in the endoscope X2.
There remain two major issues that have precluded the widespread adoption of distal sensor ureteroscopes to date. First, contemporary distal sensor ureteroscopes have a larger diameter that does limit the utility of these devices. The XC has a shaft diameter ranging from 8.4F to 8.5F from the handle to the distal tip. In comparison, other contemporary distal sensor ureteroscopes range from 9.3F to 9.9F. For digital flexible ureteroscopy to be embraced in an increasingly cost-contentious clinical environment, the cost of ownership, which comprises acquisition cost of a new scope and cost of maintenance inclusive of all repairs, should be carefully considered. Application of the Flex XC with a newly designed protective sheathed laser fiber may significantly improve durability and therefore positively impact the cost of ownership. Clinical evaluations of both Flex XC and sheathed laser fibers will be needed to quantify the actual cost of using distal sensor endoscopes.
As an in vitro evaluation, this study has intrinsic limitations. Clinical application of the ureteroscopes will be needed to confirm these initial findings. In addition, we did not evaluate ureteroscope durability, which always remains a major issue. While Okhunov and coworkers8 found no difference in cystoscope durability in their comparison of distal sensor and fiberoptic cystoscopes, this remains to be proven for ureteroscopes, and it remains to be determined if this will be true for distal sensor ureteroscopes. In addition, the distal sensor ureteroscopes do remain larger in diameter. The clinical limitations of this size discrepancy similarly remain to be determined.
Conclusion
In this in vitro and porcine in vivo trial, the distal sensor ureteroscopes evaluated provide substantially improved visualization in the upper urinary tract compared with a standard fiberoptic ureteroscope. The image has a significantly higher resolution and better visualization in a bloody as well as in a nonbloody field. Moreover, the increased deflection rate, the superior flow, and the lower weight may lead to a better performance for diagnosis and management of upper tract renal pathologies.
Abbreviations Used
- CCD
charged coupled device
- CMOS
complimentary metal oxide sensor
- HD
high definition
- USAF
United States Air Force
- X2
fiberoptic ureteroscope
- XC
distal sensor ureteroscope
Disclosure Statement
No competing financial interests exist.
References
- 1.Borin JF. Abdelshehid CS. Clayman RV. Comparison of resolution, contrast, and color differentiation among fiberoptic and digital flexible cystoscopes. J Endourol. 2006;20:54–58. doi: 10.1089/end.2006.20.54. [DOI] [PubMed] [Google Scholar]
- 2.Quayle SS. Ames CD. Lieber D, et al. Comparison of optical resolution with digital and standard fiberoptic cystoscopes in an in vitro model. Urology. 2005;66:489–493. doi: 10.1016/j.urology.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell S. Havaranek E. Patel A. First digital flexible ureterorenoscope: Initial experience. J Endourol. 2008;22:47–49. doi: 10.1089/end.2007.0046. [DOI] [PubMed] [Google Scholar]
- 4.Parkin J. Keeley FX., Jr Timoney AG. Flexible ureteroscopes: A user's guide. BJU Int. 2002;90:640–643. doi: 10.1046/j.1464-410x.2002.03017.x. [DOI] [PubMed] [Google Scholar]
- 5.Chow GK. Patterson DE. Blute ML. Segura JW. Ureteroscopy: Effect of technology and technique on clinical practive. J Urol. 2003;170:99–102. doi: 10.1097/01.ju.0000070883.44091.24. [DOI] [PubMed] [Google Scholar]
- 6.Abdelshehid C. Ahlering MT. Chou D, et al. Comparison of flexible ureteroscopes: Deflection, irrigant flow and optical characteristics. J Endourol. 2005;173:2017–2021. doi: 10.1097/01.ju.0000158139.65771.0a. [DOI] [PubMed] [Google Scholar]
- 7.Smith RD. Patel A. Impact of flexible ureterorenoscopy in current management of nephrolithiasis. Curr Opin Urol. 2007;17:114–119. doi: 10.1097/MOU.0b013e328028fe0c. [DOI] [PubMed] [Google Scholar]
- 8.Okhunov Z. Hruby GW. Mirabelle G, et al. Prospective comparision of flexible fiberoptic and digital cystoscopes. J Urol. 2009;01:427–430. doi: 10.1016/j.urology.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Borin JF. Abdelshedid CS. Deane LA, et al. The distal sensor digital flexible ureteroscope: An optical evaluation. J Endourol. 2006;20:A199. [Google Scholar]
- 10.Multescu R. Geavlete B. Georgescu D. Geavlete P. Conventional fiberoptic flexible ureteroscope versus fourth generation digital flexible ureteroscope: A critical comparison. J Endourol. 2010;24:17–21. doi: 10.1089/end.2009.0390. [DOI] [PubMed] [Google Scholar]