Abstract
Background
In China, there are 2.5 million new stroke cases each year and 7.5 million stroke survivors. However, stroke incidence in some island populations is obviously lower compared with inland regions, perhaps due to differences in diet and lifestyle. As the lifestyle in China has changed significantly, along with dramatic transformations in social, economic and environmental conditions, such changes have also been seen in island regions. Thus, we analyzed stroke in the Chinese island regions over the past 30 years.
Methods
We conducted a systematic review to identify reliable and comparable epidemiologic evidence about stroke in the Chinese island regions between 1980 and 2013. Two authors independently assessed the eligibility and the quality of the articles and disagreement was resolved by discussion. Owing to the great heterogeneity among individual study estimates, a random-effects or fixed-effects model was used to incorporate the heterogeneity among records into a pooled estimate for age-standardized rates. Age-standardized rates were calculated by the direct method with the 2000 world population if included records provided the necessary information.
Results
During the past three decades, the overall pooled age-standardized prevalence of stroke is 6.17 per 1000 (95% CI 4.56–7.78), an increase from 5.54 per 1000 (95% CI 3.88–7.20) prior to 2000 to 8.34 per 1000 (95% CI 5.98–10.69) after 2000. However, this difference was not found to be statistically significant. The overall pooled age-standardized incidence of stroke is 120.42 per 100,000 person years (95% CI 26.17–214.67). Between 1982 and 2008, the incidence of stroke increased and mortality declined over time.
Conclusions
Effective intervention and specific policy recommendations on stroke prevention should be required, and formulated in a timely fashion to effectively curb the increased trend of stroke in Chinese island regions.
Introduction
According to WHO criteria, stroke events are defined as “rapidly developing signs of focal (or global) disturbance of cerebral function lasting greater than 24 hours (unless interrupted by surgery or death) with no apparent nonvascular cause.” [1]. Stroke remains one of the most devastating of all neurological conditions, causing an estimated 5.7 million deaths in 2005 [2]. Stroke is also a major cause of long-term disability [3], [4], with an average of 44 million disability-adjusted life-years lost, with devastating emotional and socioeconomic effects on patients, their families, and the health care system.
In China, with a population of 1.4 billion, the annual stroke mortality rate is approximately 1.6 million, or 157 per 100,000, exceeding heart disease as the leading cause of adult death and disability. In addition, China has 2.5 million new stroke cases each year and 7.5 million stroke survivors [5]. There is also a geographical difference of stroke incidence in China. Northeast China has the highest incidence (486 per 100,000 person-years), whereas in southern China, the incidence is significantly lower (136 per 100,000 person-years), with a male to female ratio of 1.3 to 1.5∶1 [6].
The lifestyle in China has changed rapidly, along with dramatic transformations in social, economic, and environmental conditions over the past 30 years. As a result of an aging population, urbanization, and westernization, the main risk factors for stroke have increased substantially [7], [8]. For example, total fat intake increased from 88.1 grams per day in 1983 to 97.4 grams per day in 2002 [9]. The average serum cholesterol level increased by 24% (4.30 mmol/L to 5.33 mmol/L) and the diabetes prevalence increased from 2.8% to 8.6% from 1984 to1999 [10]. The obesity rate in Beijing increased from 10.19% to 10.41% in urban areas and 6.44% to 20.45% in rural regions between 1984 and 1999 [11]. Thus, China now faces similar risk factors for stroke as Western nations: hypertension, diabetes mellitus, hypercholesterolemia, smoking, coronary artery disease, atrial fibrillation, physical inactivity, obesity, among others. The rising incidence and impact of stroke have created serious public health issues in China [12].
A multi-center collaborative epidemiologic study monitored the incidence of stroke in approximately 100,000 residents in each of 14 study populations between 1991 and 1995 using the MONICA procedure [13]. This study demonstrated that the lowest age-standardized average annual incidence was found in Zhoushan island, in both men (59/100,000 person-years) and women (19/100,000 person-years). The lowest and highest rates (men from Hebei miners and women from Beijing residents) were 7 and 14 times, respectively. The stroke incidence rate in the population of Zhoushan island was obviously low compared with other regions. This may be attributed to the characteristics of their diet, such as high fish protein and unsaturated fatty acids, or less contamination on the island, and a comparatively more comfortable pace of life [14]. Because of the lower incidence of stroke in this region, we found it prudent to perform an analysis of stroke in the island regions.
The islands of China are located in eastern Eurasia and the western edge of the Pacific Ocean, distributed across 38 latitudes and 17 longitudes. From north to south, these islands belong to Liaoning, Tianjin, Hebei, Shandong, Jiangsu, Shanghai, Zhejiang, Fujian, Taiwan, Guangdong, Guangxi, Hainan and other coastal provinces (municipalities and autonomous regions). The aims of this systematic review are to provide current knowledge of stroke in Chinese island populations with all available population-based stroke prevalence, incidence, or mortality studies, and to analyze secular trends in stroke. We hope to advance our understanding of stroke frequency and discover the determinants in Chinese island populations, providing evidence for formulating the strategy for the prevention and control of stroke in the Chinese island populations.
Methods
Search Strategy
We searched the Chinese Biomedical literature database (CBM), Chinese National Knowledge Infrastructure (CNKI), Medline, Embase, Web of Science, Science Citation Index, and Cochrane Library electronic databases (1980 to 2013). Keywords included in the search were: stroke, stroke disease, cerebral hemorrhage, cerebral ischemia, cerebral infarction, cerebrovascular, island, fishermen, insular, China, and Chinese. For example, search strategy for Medline: “(((((((stroke [Title/Abstract]) OR cerebral hemorrhage [Title/Abstract]) OR cerebral ischemia [Title/Abstract]) OR cerebral infarction [Title/Abstract]) OR cerebrovascular [Title/Abstract])) AND (((((((((((((((((((((island [Title/Abstract]) OR island counties [Title/Abstract]) OR insular areas [Title/Abstract]) OR island populations [Title/Abstract]) OR island residents [Title/Abstract]) OR fishermen [Title/Abstract]) OR island people [Title/Abstract]) OR island masses [Title/Abstract]) OR Changhai [Title/Abstract]) OR Changdao [Title/Abstract]) OR Chongming [Title/Abstract]) OR Zhoushan [Title/Abstract]) OR Shengsi [Title/Abstract]) OR Daishan [Title/Abstract]) OR Dinghai [Title/Abstract]) OR Putuo [Title/Abstract]) OR Yuhuan [Title/Abstract]) OR Dongtou [Title/Abstract]) OR Pingtan [Title/Abstract]) OR Dongshan [Title/Abstract]) OR Nanao [Title/Abstract])) AND (((("China" [MeSH Terms] OR "China" [All Fields]) OR ("asian continental ancestry group" [MeSH Terms] OR ("asian" [All Fields] AND "continental" [All Fields] AND "ancestry" [All Fields] AND "group" [All Fields]) OR "asian continental ancestry group" [All Fields] OR "Chinese" [All Fields]))).” In our search strategy for Medline, the words “Changhai,” “Changdao,” “Chongming,” “Zhoushan,” “Shengsi,” “Daishan,” “Dinghai,” “Putuo,” “Yuhuan,” “Dongtou,” “Pingtan,” “Dongshan,” and “Nanao,” names of administrative counties in the Chinese islands, were used in order to avoid missing reports that did not contain the search terms “island,” “fishermen,” “insular areas,” and others.
To optimize our data search, we also scanned reference lists of each original and review article identified for relevant studies, in addition to reviews and meta-analyses, and consulted with key experts in the field. The search was restricted to articles published in English or Chinese. Identified publications were reviewed by one of the authors (Wu XM).We identified 23 additional records from this process (Figure 1).
Figure 1. Flow diagram (selection strategy) of included studies.
Study Selection
Two authors (Wu XM and Zhu B) independently assessed articles and abstracts for eligibility, and any disagreements were resolved by discussion. In this review, we refer to a record as any unique report from the published, grey, or unpublished literature. If several records were reported from the same population during overlapping periods, we included the record, providing the longest time span for analysis.
Records had to fulfill the following criteria to be eligible for inclusion in our review: (1) research conducted wholly or partially in Chinese island populations; (2) clear diagnostic criteria for stroke; (3) adult population-based study; (4) original article published from January 1980 to January 2013; and (5) published in English or Chinese.
Exclusion criteria were as follows: (1) Han population living on non-Chinese islands; (2) special population-based or hospital-based studies; (3) the original article did not involve the available data for outcomes; (4) repeated report; (5) reviews, letters, and comments; (6) low-quality article; (7) confined to only one pathologic type of stroke; and (8) results presented only as abstracts. We identified 20 records through this process that provided relevant prevalence, incidence, or mortality data. Different subsets of records were potentially eligible for different parts of this review (Figure 1).
Data Extraction
Data extraction was managed in Microsoft Excel. Records meeting inclusion criteria were formally reviewed by pairs of reviewers, using a data extraction form based on previous reviews. Our definition included records with sufficient data to derive an estimate, even if a rate had not been explicitly reported in the original records. Derived rates were calculated and rechecked (Wu XM and Zhu B). Data abstracted for each record were confirmed by reviewer consensus.
For each record that fulfilled criteria, we extracted the following information: first author’s name, title, publication year, publication source (or unpublished), publication reference, object age (mean or range), object gender, case-finding methodology, case-finding duration (years), geographic region, diagnostic outcomes (stroke, ischemic stroke, or hemorrhagic stroke), method of outcome assessment (prevalence, incidence, or mortality rate), diagnostic criteria, number of events, sample size, and adjustment type (crude, adjusted or standardized).
Quality Assessment
Table 1, which contained 7 items, was utilized to evaluate the quality of the records. Two authors assessed all records. A study was considered low quality if it did not meet more than 2 items. Disagreements between reviewers were resolved by discussion.
Table 1. Quality assessment of the individual studies.
| first author | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Pan BJ [19] |

|

|

|

|

|
○ |

|
| Wang DX [20] |

|

|

|

|
○ | ○ |

|
| Hu HH [21] |

|

|

|

|

|
○ |

|
| Hu HH [22] |

|

|

|

|

|

|

|
| Hu HH [23] |

|

|

|

|

|

|

|
| Su CL [24] |

|

|

|

|

|
○ |

|
| Lee TK [25] |

|

|

|

|

|
○ |

|
| Fuh JL [26] |

|

|

|

|

|

|

|
| Fuh JL [27] |

|

|

|

|

|

|

|
| Huang ZS [28] |

|

|

|

|

|

|

|
| Zhou BF [13] |

|

|

|

|

|
○ |

|
| Lee YT [30] |

|

|

|

|

|

|

|
| Liu CG [31] |

|

|

|

|
○ | ○ |

|
| Wang JF [14] |

|

|

|

|
○ | ○ |

|
| Lin HC [32] |

|

|

|

|

|
○ |

|
| Zou SY [34] |

|

|

|

|

|
○ |

|
| Song SZ [35] |

|

|

|

|

|
○ |

|
| Miu S [36] |

|

|

|

|
○ | ○ |

|
| Ye Z [37] |

|

|

|

|
○ | ○ |

|
| Hu GZ [38] |

|

|

|

|

|
○ |

|
 : The item is met.
: The item is met.
○: The item is not met.
1. Describe the locations.
2. Describe periods of recruitment, follow-up, and data collection.
3. Give the eligibility criteria, and the sources and methods of selection of participants.
4. Involve the available data on outcomes.
5. Report numbers of individuals at each stage of study.
6. Give reasons for non-participation at each stage.
7. Give characteristics of study participants.
Data Analysis and Statistical Methods
Owing to the great heterogeneity among individual study estimates, which could be due to genuine regional differences and wide age ranges, age-standardized rates were calculated by the direct method with 2000 world population data, if included records provided the necessary information. Based on these reasons, the random-effects or fixed-effects model attempts to incorporate heterogeneity among records into a pooled estimate only for age-standardized rates [15].
Extracted data were analyzed using Stata (version 12.0) software. To calculate the pooled age-standardized rates of prevalence or incidence, we used the random-effects model, with the standard method proposed by Dersimonian, and the Laird [16] or fixed-effects model using an inverse variance statistical method [17]. In each meta-analysis, χ2 and I2 values were first calculated to assess the heterogeneity of the included records. When there was no statistically significant heterogeneity, the pooled effect was calculated using a fixed-effects model; otherwise, a random-effects model was employed.
Results
Flow of Included Studies
A total of 835 records were identified by the search strategy, 815 of which were excluded (Figure 1). 20 records met inclusion criteria, 18 were published articles, and the remaining 2 were graduate theses. Of all 20 records, the prevalence, incidence, and mortality analyses were included in 9, 7, and 7 records, respectively (Figure 1).
Study Characteristics
Table 1 presents the quality of individual studies; Table 2 presents the characteristics (summary and results) of individual studies. For stroke mortality rate, we were more concerned about whole population data, as most of the included records also did. Therefore a record (Gao CW [18]) about mortality rate of stroke in age-specific population was excluded for the above reason.
Table 2. Characteristics of records and patients included in the review.
| first author | publication year | age(range) | gender | case-finding duration(years) | geographical region | outcome | sample size | crude rate | adjustmentrate # | diagnostic criteria |
| Pan BJ [19] | 1984 | 40– | both | 1982 | Taiwan Province | prevalence | NR | 14.0 | 4.83 | NR |
| Wang DX [20] | 1986 | 35–59 | both | 1982 | Putuo County, Zhejiang Province | prevalence | 1590 | 6.3 | 1.87 | WHO |
| Hu HH [21] | 1986 | all | Ma/Fe | 1972–1983 | Taiwan Province | mortality | NR | 88.0/72.5 | NR | ICD-9 |
| Hu HH [22] | 1989 | 36– | both | 1986.10.1–12.3 | Taiwan Province | prevalence | 8705 | 16.4 | 5.76 | WHO |
| Hu HH [23] | 1992 | 36– | both | 1986.10–1990.10 | Taiwan Province | incidence | 31502 | 330 | 136.41 | WHO |
| Su CL [24] | 1992 | all | Ma/Fe | 1989 | Taiwan Province | mortality | no | 76.6/67.7 | no | no |
| Lee TK [25] | 1995 | 65– | both | 1990–1992 | Taiwan Province | prevalence | 2600 | 59.6 | 5.77 | WHO |
| Fuh JL [26] | 1996 | 50– | both | 1993.8.1–1994.9.17 | Kinmen, Taiwan Province | prevalence | 3915 | 24.5 | 4.87 | WHO |
| Fuh JL [27] | 2000 | 50– | both | 1993.8–1997.12 | Kinmen, Taiwan Province | incidence | 10057 | 527 | 105.12 | WHO |
| Huang ZS [28] | 1997 | all | both | 1994.10–12 | Taiwan Province | prevalence | 11925 | 5.95 | 6.56 | Other [29] |
| Zhou BF [13] | 1998 | 25–74 | both | 1991–1995 | Zhoushan City, Zhejiang Province | incidence | 255380 | 31.33 | 16.96 | WHO |
| Lee YT [30] | 2000 | 35– | both | 1990 | Taipei, Taiwan Province | prevalence | 3602 | 21.9 | 9.12 | Other† |
| Lee YT [30] | 2000 | 35– | both | 1990–1995 | Taipei, Taiwan Province | incidence | 12542 | 590 | 245.76 | Other† |
| Liu CG [31] | 2002 | all | both | 1982–2001 | Putuo County, Zhejiang Province | mortality | 2011492 | 12.88 | NR | ICD-9 |
| Liu CG [31] | 2002 | all | both | 1982–2001 | Putuo County, Zhejiang Province | incidence | 2011492 | 20.73 | NR | WHO |
| Wang JF [14] | 2007 | all | both | 1998–2006 | Daishan County, Zhejiang Province | incidence | 495000 | 95.85 | NR | Other‡ |
| Lin HC [32] | 2007 | 35– | both | 2001.8–2002.1 | Taiwan Province | prevalence | 9794 | 19.3 | 9.21 | Other [33] |
| Zou SY [34] | 2008 | all | both | 2000–2004 | LongIsland County, Shandong Province | mortality | 86371 | 152.83 | NR | ICD-10 |
| Song SZ [35] | 2008 | all | both | 2002–2005 | Xiangshan County, Zhejiang Province | mortality | 2107534 | 128.54 | NR | ICD-10 |
| Miu S [36] | 2010 | all | both | 2005–2008 | Chongming County, Shanghai | mortality | NR | 229 | NR | ICD-10 |
| Miu S [36] | 2010 | all | both | 2005–2008 | Chongming County, Shanghai | incidence | NR | 268 | NR | Other‡ |
| Ye Z [37] | 2011 | 25– | both | 2009 | Xiangshan County, Zhejiang Province | prevalence | 2313 | 11.7 | 6.69 | NR |
| Hu GZ [38] | 2011 | all | both | 1986–1988 | Daishan County, Zhejiang Province | mortality | 644448 | 74.17 | NR | ICD-9 |
| Hu GZ [38] | 2011 | all | both | 2009–2010 | Daishan County, Zhejiang Province | mortality | 382464 | 136.22 | NR | ICD-10 |
Unless otherwise stated, all prevalence sample sizes and rates are expressed as persons and per 1000 population; all incidence and mortality sample sizes and rates are expressed as person-years and per 100,000 person-years.
#: Adjust to the WHO (2000) world population calculated from available data.
NR: not reported and not calculated from available data.
: a history of hemiparesis or hemiplegia confirmed by neurologists from National Taiwan University Hospital (NTUH) by physical examination.
: 1995 Fourth National cerebrovascular disease Conference.
Prevalence of Stroke in Chinese Island Populations
During the three decades, data relating to stroke prevalence containing at least 44,444 persons, from 9 records were available for analysis. The total crude stroke prevalence rates ranged from 5.95 to 59.6 per 1000; the lowest crude prevalence was noted by Huang [28] (1994, age range: all), and the highest crude prevalence was observed by Lee [25] (1992, age range: more than 65) (Table 2).
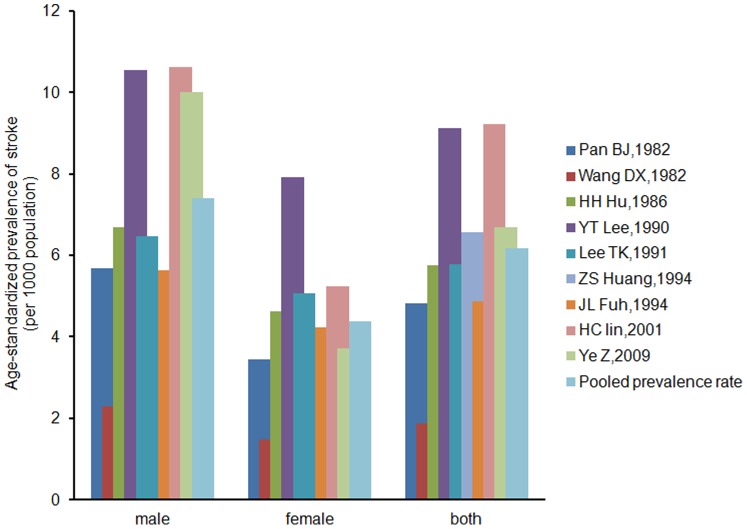
Age-standardized prevalence rates in 9 records ranged from 1.87 per 1000 (Wang [20], 1982) to 9.21 per 1000 (Lin [31], 2001) (Figure 2). The results of the meta-analysis showed that the overall pooled prevalence of stroke was 6.17 per 1000 (95% CI 4.56–7.78, p for heterogeneity = 0.000, I2 = 77.6%), as determined using the random-effects model; the male pooled stroke prevalence was 7.40 per 1000 (95% CI 4.43–10.37, p for heterogeneity = 0.004, I2 = 71.6%), as determined by the random-effects model; the female pooled stroke prevalence was 4.37 per 1000 (95% CI 3.18–5.55, p for heterogeneity = 0.131, I2 = 41.2%), as determined by the fixed-effects model.
Figure 2. Age-standardized prevalence of stroke per 1000 in selected studies (adjusted to the WHO world population).
Studies are arranged in ascending order of research time.
The age-specific stroke prevalence was reported in 4 records (Hu [22], Lee [25], Huang [28], Lin [31]). In general, data indicated that stroke prevalence increased with age. But according to Hu [22] and Lin [31], stroke prevalence began to decline in the oldest age group (Figure 3).
Figure 3. Graph showing the prevalence of stroke by different ages in selected studies.
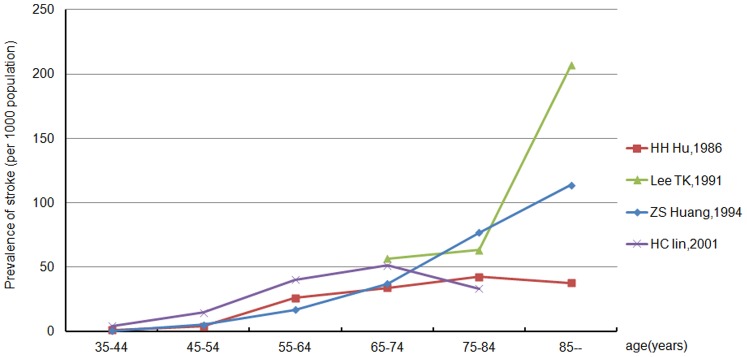
Studies are arranged in ascending order of research time.
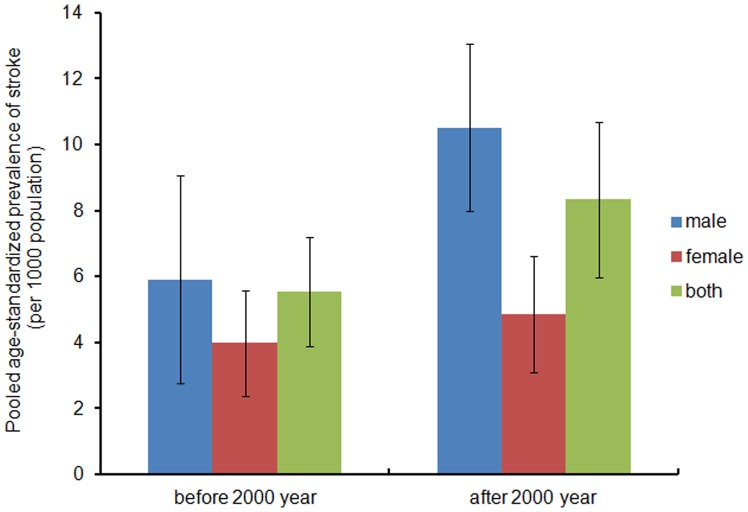
The pooled estimates of age-standardized stroke prevalence rate was 5.54 per 1000 (95% CI 3.88–7.20) prior to 2000 and 8.34 per 1000 (95% CI 5.98–10.69) after 2000; in males, the pooled age-standardized prevalence was 5.91(95% CI 2.76–9.06) prior to 2000 and 10.51(95% CI 7.97–13.05) after 2000; in females, it was 3.98 (95% CI 2.38–5.58) and 4.84 (95% CI 3.07–6.61). The values of pooled age-standardized prevalence increased, especially in the male population. However, this change was not found to be statistically significant, possibly as a result of fewer reports (Figure 4).
Figure 4. Pooled age-standardized prevalence of stroke (per 1000) in selected studies by different periods.
Incidence of Stroke in Chinese Island Populations
Data relating to stroke incidence containing at least 2,815,973 cumulative person years from 7 records were available for analysis. During the study period, a total of 1155 stroke patients were found (not including patients from Miu [36], because they were not reported in his thesis). The average annual crude incidence (per 100,000 person years) ranged from 20.73 to 590.0, with the lowest incidence reported by Liu [31](1982–2001, age range: all) and the highest by Lee [30] (1990–1995, age range: more than 35) (Table 2).
Average annual age-standardized incidence rates (per 100,000 person years) among 4 of 7 records (not calculated from available data in Liu [31], Wang [14], and Miu [36]) ranged from 16.96 (Zhou [13], 1991–1995) to 245.76 (Lee [30], 1990–1995). The meta-analysis revealed the heterogeneity of the 4 included studies (I2 = 95.4%, p for heterogeneity = 0.000). Analysis using a random-effects model revealed an overall pooled incidence of 120.42 (95% CI 26.17–214.67); for males 127.96 (95% CI 29.07–226.85, I2 = 90.5%, p for heterogeneity = 0.000) and for females 104.36 (95% CI 11.64–197.09, I2 = 91.4%, p for heterogeneity = 0.000) (Figure 5).
Figure 5. Annual age-standardized incidence of stroke per 100,000 person-years in selected studies (adjusted to the WHO world population).
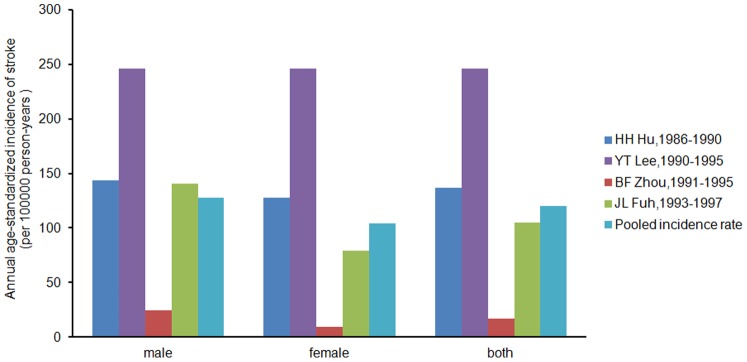
Studies are arranged in ascending order of research.
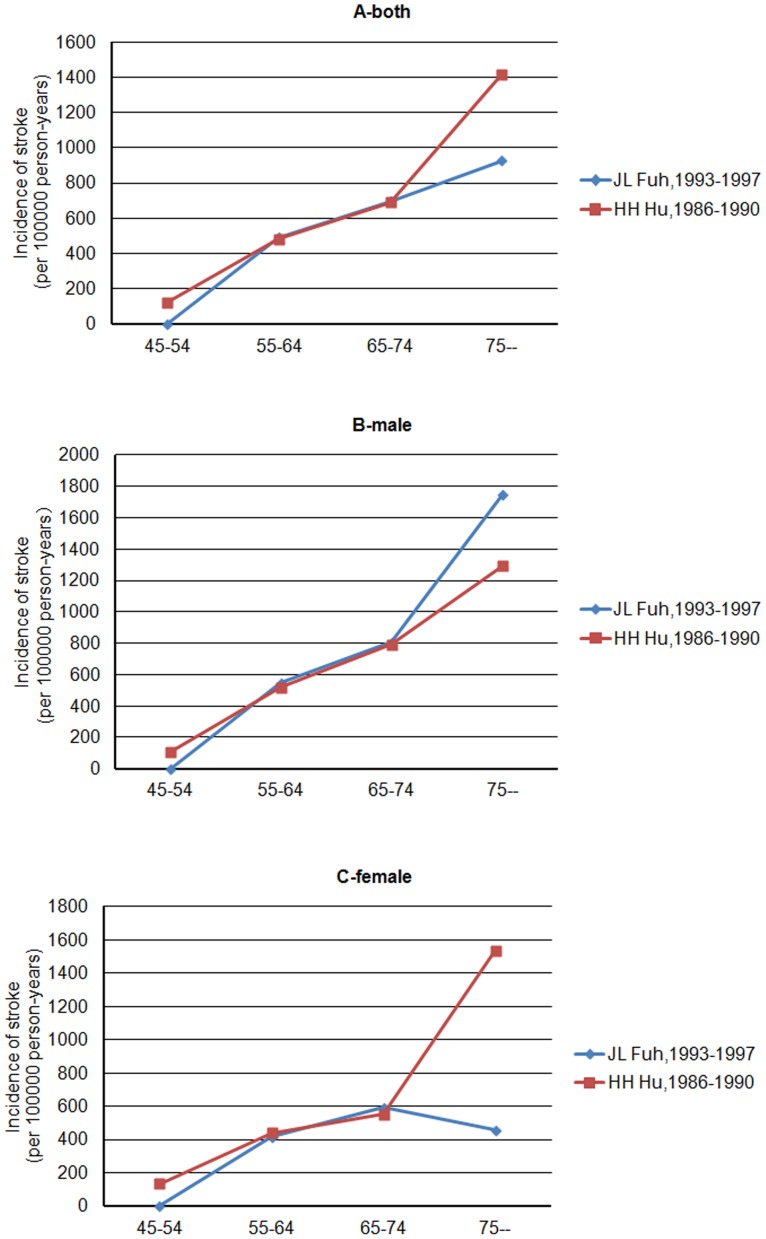
The age-specific incidence of stroke was reported only from 2 records (Hu [23], Fuh [27]) and both data indicated that stroke incidence increased with age. But according to Fuh [27], stroke incidence in females began to decline in patients older than 75 years (Figure 6).
Figure 6. Graph showing the incidence of stroke by different ages in selected studies, for both (panel A) and men or women (panel B or C).
We identified 3 primary records from 7 studies that directly investigated possible changes in the crude stroke incidence over time in Chinese island populations, ranging from 20 year (Liu [31], 1982–2001), 9 years (Wang [14],1998–2006) and 4 years (Miu [36], 2005–2008), respectively.
Wang [14] reported an increase in stroke incidence between 1998 and 2006 (from 41.8 to 138.2 per 100,000 person years), at the same rates for males and females. Liu(1982–2001) [31] and Miu(2005–2008) [36] found a slight increase in stroke incidence over time. As a whole, these three records (1982–2008) demonstrated an increase of stroke incidence with time (Figure 7).
Figure 7. Graphs showing the secular trend of annual crude incidence of stroke in selected studies included objects of all ages, for both (panel A) and men or women (panel B or C).
Mortality of Stroke in Chinese Island Populations
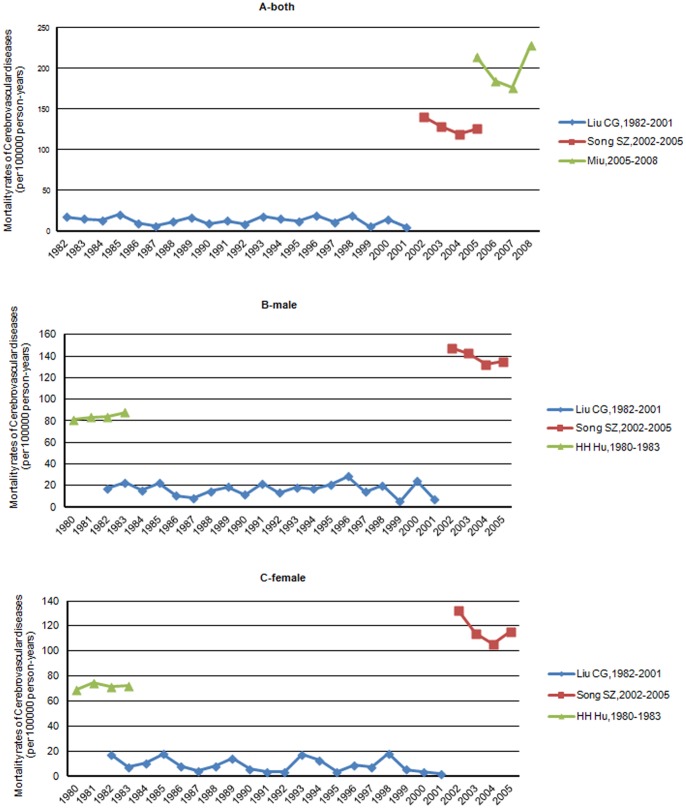
Between 1982–2010, the lowest crude mortality rate of stroke was reported by Liu [31], between 1982–2001 (12.88 per 100,000 person years) and the highest reported by Miu [36] in 2008 (229 per 100,000 person years) (Table 2, Figure 8).
Figure 8. Annual crude mortality rates of cerebrovascular diseases per 100,000 person-years in selected studies.
Records evaluating secular trends in annual crude stroke mortality rate in Chinese island populations were available only for Liu [31] (1982–2001), Song [35] (2002–2005), Miu [36] (2005–2008), and Hu [21] (male and female respectively, 1980–1983).
Over the three decades, the crude stroke mortality rates in the target population of Liu [31] decreased by 72.21% (from 17.47 in 1982 to 4.85 in 2001, per 100,000 person-years); the crude mortality rates of Song [35] declined by 10.49% (from140.31 in 2002 to 125.59 in 2005, per 100,000 person-years). There is no clear secular trend displayed in data from Miu [36]. However, during the earlier period (1980–1983), a similar increase for both males and females was observed by Hu [21].
Overall, the crude stroke mortality rate is declining with time, although mortality rates in different records increased over time (12.88, Liu [31]1982–2001; 128.54, Song [35]2002–2005; 229, Miu [36]2005–2008) because of the heterogeneity between studies, from regional or research methodological differences(Figure 9).
Figure 9. Graphs showing the secular trend of annual crude mortality rates of cerebrovascular diseases in selected studies included objects of all ages, for both (panel A) and men or women (panel B or C).
Discussion
To the best of our knowledge, this is the first systematic review to provide pooled estimates on stroke in Chinese island populations. Stroke incidence rates in Chinese island populations increased over the past three decades (Figure 7), at an even faster rate than in surrounding areas [14]. This is probably due to improvements in health care systems and diagnostic ability [8], [12]; however, more likely due to health and epidemiological transition [9], [39], [40]. Currently, there are no adequate analyses for the causes of the increased incidence of stroke in Chinese island populations. More research on this issue is required.
An increased frequency of stroke-related risk factors, such as hypertension, diabetes mellitus, body-mass index, hyperlipidemia, smoking, and alcoholism[41]–[44], are due to nutrition and lifestyle changes in Chinese island populations over the past thirty years [45]. First, transportation and exchanges between the island and mainland has improved in recent years, leading to decreased intake of marine fish food and increased intake of poultry and other food [14]. Second, a habitual high-salt diet[46]–[50] (salted or pickled fish) and low intake of fresh fruits and vegetables [51], [52] are still very common in island residents, which has been corrected through education in the mainland population [40]. Third, due to changes in industrial structure, the number of island residents engaged in manual labor reduced although with the same labor intensity [40]. Fourth, with an aging population, increased life expectancy or unplanned urbanization or air pollution brought by industry development plays an environmental role[40], [53]–[55].
Hypertension as an independent risk factor for stroke has been surveyed in several recent trials[56]–[58]. According to the World Health Organization, 62% of all strokes are attributable to high blood pressure [59]. The age-standardized prevalence of hypertension among island residents of Zhoushan City (Zhang [60]) increased from 5.28% to 14.96%, or 183.33% overall between 1990 and 2003.
Abnormal glucose regulation, including diabetes, impaired fasting glucose, and impaired glucose tolerance, have been recognized as important risk factors for occurrence and recurrence of ischemic stroke in Europe and America[61]–[63]. The prevalence of diabetes in China is now approaching that of the United States (7%) [6]. The age-standardized prevalence of diabetes in the population of Zhoushan island had been 12.5% in men and 7.2% in women (1998) [64].
The mean serum total cholesterol (TC) level of 160.7 mg/dl for men and 158.5 mg/dl for women was lower in the population of Zhoushan island compared to other populations between 1992–1994 [13]. However the age-standardized prevalence of high serum TC increased substantially from 7.6% to 23.0% in men and from 10.4% to 23.6% in women between 1992 and 1998, close to the average level [64].
The age-standardized prevalence of overweight in the population of Zhoushan island increased from 6.2% to 17.1% in men and 7.3% to 23.6% in women, 175.81% and 223.29% overall respectively, between 1982 and 1998 [64]. This finding will undoubtedly lead to an increased prevalence and incidence of stroke.
Alcohol and tobacco use are increasingly common in China. With the exception of Mongolia, smoking rates are higher in Chinese men than in any other country. The age-standardized prevalence of alcohol use was 71.0% and tobacco was 67.4% in men of Zhoushan island in1998 [64].
Most risk factors for stroke appeared in the Chinese island populations during the last 30 years, and approximated the nationwide average. However, our findings regarding stroke incidence and mortality do not provide evidence that changes in stroke mortality correlate with stroke incidence. In actuality, WHO MONICA project data [65] suggests that changes in stroke mortality are largely attributable to early fatality rather than increasing incidence in most populations. With economic development and medical progress fatality [9] and long-term morbidity has decreased [3], [66], [67]. Therefore, Chinese island populations may have benefited from access to advanced treatment, lowering mortality rates (Figure 9; Liu [31], Song [35]). However, the burden of stroke has increased with the cumulative effect of risk factors for stroke [12]. Effective preventive measures will not only improve health, but will contribute to sustainable economic development in the Chinese islands [40], [68].
The prevalence and incidence of stroke in one record in this review is higher in men (Figure 2, 5), similar to most studies. This may be due to differences in risk factors such as hypertension, diabetes, hyperlipidemia, and alcohol and tobacco use [69].
Figures 3 and 6 show data on age-specific prevalence and incidence, which rose exponentially with age; this was not unexpected, since the strongest risk factor for stroke is age. The prevalence rate, however, fell in the oldest age group (Hu [22], Lin [31]) which may be due to smaller sample size, increasing the uncertainty around prevalence, or because of the higher mortality rates in the highest age group.
The strengths of this study are four-fold. First, we used population-based stroke studies on prevalence, incidence, or mortality. 20 included studies ensured that the data provided was accurate. Second, the study period was comprised of the past three decades, a long period. Third, in addition to descriptive analyses, we used meta-analytic techniques, providing pooled estimates [15] over different study periods, thus increasing statistical reliability. Fourth, we provided a detailed account of our search strategy and data extraction methodology, which allowed us to identify all citations relevant to our review.
Our review has several limitations. There was still not enough data for pooled estimates of population-based stroke mortality and some subgroup analyses (stroke subtypes). Second, there was heterogeneity on stroke incidence and prevalence in the included records; we used a random effects model to incorporate this statistical heterogeneity, which we were unable to explain. The heterogeneity may have come from the complex interplay between genetics, vascular risk factors, and health seeking behavior, which must also be highlighted as a potential weakness.
Supporting Information
PRISMA Checklist of this systematic review.
(DOC)
Funding Statement
The authors have no support or funding to report.
References
- 1. Hatano S (1976) Experience from a multicentre stroke register: a preliminary report. Bulletin of the World Health Organization 54: 541–543. [PMC free article] [PubMed] [Google Scholar]
- 2. Strong K, Mathers C, Bonita R (2007) Preventing stroke: saving lives around the world. The Lancet Neurology 6: 182–187. [DOI] [PubMed] [Google Scholar]
- 3. Johnston SC, Mendis S, Mathers CD (2009) Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. The Lancet Neurology 8: 345–354. [DOI] [PubMed] [Google Scholar]
- 4. Reinhardt UE, Cheng TM (2000) The world health report 2000-Health systems: improving performance. Bulletin of the World Health Organization 78: 1064–1064. [Google Scholar]
- 5.Chen Z (2008) The mortality and death cause of national sample areas. In: Chen Z, ed. The Third National Survey on the Cause of Death, I ed Beijing: Peking Union Medical University Press: 14–15.
- 6. Liu LP, Wang D, Wong KSL, Wang YJ (2011) Stroke and Stroke Care in China: Huge Burden, Significant Workload, and a National Priority. Stroke 42: 3651–3654. [DOI] [PubMed] [Google Scholar]
- 7. Jiang B, Wang WZ, Chen HL, Hong Z, Yang QD, et al. (2006) Incidence and trends of stroke and its subtypes in China results from three large cities. Stroke 37: 63–65. [DOI] [PubMed] [Google Scholar]
- 8. Wang LD, Kong LZ, Wu F, Bai YM, Burton R (2005) Preventing chronic diseases in China. The Lancet 366: 1821–1824. [DOI] [PubMed] [Google Scholar]
- 9. Zhao D, Liu J, Wang W, Zeng ZC, Cheng J, et al. (2008) Epidemiological Transition of Stroke in China Twenty-One–Year Observational Study From the Sino-MONICA-Beijing Project. Stroke 39: 1668–1674. [DOI] [PubMed] [Google Scholar]
- 10. Critchley J, Liu J, Zhao D, Wei W, Capewell S (2004) Explaining the Increase in Coronary Heart Disease Mortality in Beijing Between 1984 and 1999. Circulation 110: 1236–1244. [DOI] [PubMed] [Google Scholar]
- 11. Liu S, Zhao D, Wang W, Liu J, Qin L (2006) The trends of cardiovascular risk factors in urban and rural areas of Beijing during 1984–1999. J Cardiovascular & Pulmonary Disease 25: 129–134. [Google Scholar]
- 12. Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, et al. (2007) Stroke in China: epidemiology, prevention, and management strategies. Lancet neurology 6: 456–464. [DOI] [PubMed] [Google Scholar]
- 13. Zhou BF, Zhang HY, Wu YF, Li Y, Yang J, et al. (1998) Ecological Analysis of the Association Between Incidence and Risk Factors of Coronary Heart Disease and Stroke in Chinese Populations. CVD Prevention 1: 207–216. [Google Scholar]
- 14. Wang JF (2007) The incidence of stroke in the residents of Qushan island, Zhoushan city, Zhejiang province. Chin J Prev Contr Chron Non-commun Dis 15: 593–594. [Google Scholar]
- 15. Feigin VL, Lawes CMM, Bennett DA, Barker-Collo SL, Parag V (2009) Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. lancet neurology 8: 355–369. [DOI] [PubMed] [Google Scholar]
- 16. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Controlled clinical trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 17.Hedges LV, Olkin I, Statistiker M, Olkin I, Olkin I (1985) Statistical methods for meta-analysis. Academic Press New York.
- 18. Gao CW (1997) Changshan archipelago elderly death analysis. Journal of Mathematical Medicine 10: 323–325. [Google Scholar]
- 19.Pan BJ, Chen CJ (1984) Community-wide epidemiological investigation of cardiovascular diseases and diabetes mellitus of residents in six areas of Taiwan, R.O.C.: prevalence survey and risk factor analysis.
- 20. Wang DX, Deng YL, Liu J, Li Q (1986) A survey of prevalence and risk factors for hypertension, coronary heart disease and stroke in Xiashi fishing areas, Putuo county. Zhejiang Journal of Medicine 8: 56–57. [Google Scholar]
- 21. Hu HH, Chu FL, Wong WJ, Lo YK, Sheng WY (1986) Trends in mortality from cerebrovascular disease in Taiwan. Stroke 17: 1121–1125. [DOI] [PubMed] [Google Scholar]
- 22. Hu HH, Chu FL, Chiang BN, Lan CF, Sheng WY, et al. (1989) Prevalence of stroke in Taiwan. Stroke 20: 858–863. [DOI] [PubMed] [Google Scholar]
- 23. Hu HH, Sheng WY, Chu FL, Lan CF, Chiang BN (1992) Incidence of stroke in Taiwan. Stroke 23: 1237–1241. [DOI] [PubMed] [Google Scholar]
- 24. Su CL, Chang SF, Hung TP (1992) Secular trends in mortality for cerebrovascular diseases in Taiwan(1959–1989). J Formos Med Assoc 91: 52–61. [PubMed] [Google Scholar]
- 25. Lee TK, Huang ZS, Ng SK, Chan KWA, Wang YS, et al. (1995) Impact of alcohol consumption and cigarette smoking on stroke among the elderly in Taiwan. Stroke 26: 790–794. [DOI] [PubMed] [Google Scholar]
- 26. Fuh JL, Wang SJ, Larson EB, Liu HC (1996) Prevalence of stroke in Kinmen. Stroke 27: 1338–1341. [DOI] [PubMed] [Google Scholar]
- 27. Fuh JL, Wang SJ, Liu HC, Shyu HY (2000) Incidence of stroke on Kinmen, Taiwan. Neuroepidemiology 19: 258–264. [DOI] [PubMed] [Google Scholar]
- 28. Huang ZS, Chiang TL, Lee TK (1997) Stroke prevalence in Taiwan. Findings from the 1994 National Health Interview Survey. stroke 28: 1579–1584. [DOI] [PubMed] [Google Scholar]
- 29.Chiang TL, Chang MJ, Hung YT (1995) Final report on the 1994 national health interview survey, Republic of China. College of Public Health, National Taiwan University, Taiwan, Republic of China.
- 30. Lee YT, Lin RS, Sung FC, Yang CY, Chien KL, et al. (2000) Chin-Shan Community Cardiovascular Cohort in Taiwan–baseline data and five-year follow-up morbidity and mortality. Journal of Clinical Epidemiology 53: 838–846. [DOI] [PubMed] [Google Scholar]
- 31. Liu CG, Ruan LS (2002) A prospective survey of the change of stroke incidences over 20 years in Putuo fishing village of Zhoushan, Zhejiang Province- a primary exploration on the protective factors for stroke. Chin J Prev Contr Chron Non-commun Dis 10: 150–152. [Google Scholar]
- 32. Lin HC, Lin YJ, Liu TC, Chen CS, Chiu WT (2007) Urbanization and stroke prevalence in Taiwan: analysis of a nationwide survey. J Urban Health (Bulletin of the New York Academy of Medicine) 84: 604–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shih YT, Chang HY, Le KH (2002) Introduction to the National Health Interview Survey (NHIS). Vol 1. NHIS Brief Communication.
- 34. Zou SY, Chu LM, Tian YM, Chu CJ, Liang P, et al. (2008) A sample survey of death in Changdao County residents from 2000 to 2004. Chinese Journal of Health Statistics 25: 101–102. [Google Scholar]
- 35.Song SZ (2008) The analytic study on the death causes of inhabitant in Xiangshan county from 2002 to 2005. Public Health School of Zhejiang University.
- 36.Miu S (2010) Trends of stroke in Shanghai. Public Health School of Fudan University.
- 37. Ye Z, Pei GJ, Xu JR (2011) Survey on prevalence of chronic disease among population in community of Xiangshan island. Chin J of PHM 27: 292–293. [Google Scholar]
- 38. Hu GZ, He CH, Qiu FM (2011) Death causes in residents in two periods in Daishan county in Zhejiang province. Disease Surveillance 26: 993–1003. [Google Scholar]
- 39. Connor MD, Walker R, Modi G, Warlow CP (2007) Burden of stroke in black populations in sub-Saharan Africa. Lancet Neurology 6: 269–278. [DOI] [PubMed] [Google Scholar]
- 40. Yang G, Wang Y, Zeng Y, Gao GF, Liang X, et al. (2013) Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 381: 1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Brämer GR (1988) Internatind related health problems. Tenth revision. World health statistics quarterly 41: 32–36. [PubMed] [Google Scholar]
- 42. Cannon CP (2010) An Overview of Stroke and the Impact of Atrial Fibrillation. Am J Manag Care 16: 273–277. [PubMed] [Google Scholar]
- 43. Ishigami K, Okuro M, Koizumi Y, Satoh K, Iritani O, et al. (2012) Association of severe hypertension with pneumonia in elderly patients with acute ischemic stroke. Hypertension Research 35: 648–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Galimanis A, Mono ML, Arnold M, Nedeltchev K, Mattle HP (2009) Lifestyle and stroke risk: a review. Current opinion in neurology 22: 60–68. [DOI] [PubMed] [Google Scholar]
- 45. Huang CY (2007) Nutrition and stroke. Asia Pac J Clin Nutr 16: 266–274. [PubMed] [Google Scholar]
- 46. Li XY, Cai XL, Bian PD, Hu LR (2012) High Salt Intake and Stroke: Meta-analysis of the Epidemiologic Evidence. CNS neuroscience & therapeutics 18: 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nagata C, Takatsuka N, Shimizu N, Shimizu H (2004) Sodium intake and risk of death from stroke in Japanese men and women. Stroke 35: 1543–1547. [DOI] [PubMed] [Google Scholar]
- 48. Kokubo Y (2012) Traditional risk factor management for stroke: a never-ending challenge for health behaviors of diet and physical activity. Current Opinion in Neurology 25: 11–17. [DOI] [PubMed] [Google Scholar]
- 49. Legetic B, Campbell N (2011) Reducing salt intake in the Americas: Pan American Health Organization actions. Journal of health communication 16: 37–48. [DOI] [PubMed] [Google Scholar]
- 50. Tomonari T, Fukuda M, Miura T, Mizuno M, Wakamatsu TY, et al. (2011) Is salt intake an independent risk factor of stroke mortality? Demographic analysis by regions in Japan. Journal of the American Society of Hypertension 5: 456–462. [DOI] [PubMed] [Google Scholar]
- 51. Foroughi M, Akhavanzanjani M, Maghsoudi Z, Ghiasvand R, Khorvash F, et al. (2013) Stroke and Nutrition: A Review of Studies. International Journal of Preventive Medicine 4: 165–179. [PMC free article] [PubMed] [Google Scholar]
- 52. Sharma S, Cruickshank JK, Green DM, Vik S, Tome A, et al. (2013) Impact of Diet on Mortality From Stroke: Results From the U.S. Multiethnic Cohort Study. Journal of the American College of Nutrition 32: 151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Qian Y, Zhu M, Cai B, Yang Q, Kan H, et al. (2012) Epidemiological evidence on association between ambient air pollution and stroke mortality. J Epidemiol Community 67: 635–640. [DOI] [PubMed] [Google Scholar]
- 54. Chen R, Zhang Y, Yang C, Zhao Z, Xu X, et al. (2013) Acute Effect of Ambient Air Pollution on Stroke Mortality in the China Air Pollution and Health Effects Study. Stroke 44: 954–960. [DOI] [PubMed] [Google Scholar]
- 55. Xiang H, Mertz KJ, Arena VC, Brink LL, Xu X, et al. (2013) Estimation of Short-Term Effects of Air Pollution on Stroke Hospital Admissions in Wuhan, China. PLoS One 8: e61168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang XF, Attia J, D’Este C, Yu XH (2004) Prevalence and magnitude of classical risk factors for stroke in a cohort of 5092 Chinese steelworkers over 13.5 years of follow-up. Stroke 35: 1052–1056. [DOI] [PubMed] [Google Scholar]
- 57. Fang XH, Zhang XH, Yang QD, Dai XY, Su FZ, et al. (2006) Subtype Hypertension and Risk of Stroke in Middle-Aged and Older Chinese A 10-Year Follow-Up Study. Stroke 37: 38–43. [DOI] [PubMed] [Google Scholar]
- 58. Teng WY, Wang HL, Shi JP, Fu LY, Li H, et al. (2007) Study on the influencing factors to cerebral stroke in a region with high prevalence rate of hypertension. Chinese Journal of Epidemiology 28: 441–444. [PubMed] [Google Scholar]
- 59. Brundtland GH (2002) Reducing risks to health, promoting healthy life. JAMA: The Journal of the American Medical Association 288: 1974. [DOI] [PubMed] [Google Scholar]
- 60. Zhang JH, Le XP, Zheng YK (2004) An Epidemiological Survey and Risk Factors Analysis on Hypertension in Zhoushan City. Zhejiang Prev Med 16: 5–9. [Google Scholar]
- 61. Tanne D, Koren-Morag N, Goldbourt U (2004) Fasting Plasma Glucose and Risk of Incident Ischemic Stroke or Transient Ischemic Attacks A Prospective Cohort Study. Stroke 35: 2351–2355. [DOI] [PubMed] [Google Scholar]
- 62. Tanne D (2008) Impaired glucose metabolism and cerebrovascular diseases. Adv Cardiol 45: 107–113. [DOI] [PubMed] [Google Scholar]
- 63. Vermeer SE, Sandee W, Algra A, Koudstaal PJ, Kappelle LJ, et al. (2006) Impaired glucose tolerance increases stroke risk in nondiabetic patients with transient ischemic attack or minor ischemic stroke. Stroke 37: 1413–1417. [DOI] [PubMed] [Google Scholar]
- 64. WU YF (2001) Current status of major cardiovascular risk factors in Chinese populations and their trends in the past two decades. Chin J Cardiol 29: 74–79. [Google Scholar]
- 65. Sarti C, Stegmayr B, Tolonen H, Mähönen M, Tuomilehto J, et al. (2003) Are changes in mortality from stroke caused by changes in stroke event rates or case fatality? Results from the WHO MONICA Project. Stroke 34: 1833–1840. [DOI] [PubMed] [Google Scholar]
- 66. Kim AS, Johnston SC (2011) Global Variation in the Relative Burden of Stroke and Ischemic Heart DiseaseClinical Perspective. Circulation 124: 314–323. [DOI] [PubMed] [Google Scholar]
- 67. Zhang XH, Guan TR, Mao JW, Liu LS (2007) Disparity and Its Time Trends in Stroke Mortality Between Urban and Rural Populations in China 1987 to 2001 Changing Patterns and Their Implications for Public Health Policy. Stroke 38: 3139–3144. [DOI] [PubMed] [Google Scholar]
- 68. Mukherjee D, Patil CG (2011) Epidemiology and the global burden of stroke. World neurosurgery 76: 85–90. [DOI] [PubMed] [Google Scholar]
- 69. Di Carlo A, Launer LJ, Breteler MM, Fratiglioni L, Lobo A, et al. (2000) Frequency of stroke in Europe: A collaborative study of population-based cohorts. ILSA Working Group and the Neurologic Diseases in the Elderly Research Group. Italian Longitudinal Study on Aging. Neurology 54: 28–33. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist of this systematic review.
(DOC)