Abstract
Coping and negative cognitive style were studied in relation to depressive symptoms in children at risk for depression. In a sample of 165 children (ages 9–15) of depressed parents, the main and interaction effects of coping and negative cognitive style were examined in association with children’s depressive symptoms measured by parent and child report on questionnaires and diagnostic interviews. Negative cognitive style was related to three types of coping (primary control, secondary control, and disengagement). Furthermore, coping and negative cognitive style made independent contributions to depressive symptoms. Little support emerged for interactive effects on depressive symptoms. Implications for future research with this high-risk population of children are considered.
Keywords: Coping, Negative Cognitive Style, Children, Depression, Parental depression
Introduction
Research has clearly demonstrated the increased risk for psychopathology among children of depressed parents, with approximately 50% of children of depressed parents developing depression by adulthood (e.g., Goodman et al. 2011) and a twofold to sixfold higher risk of developing other psychopathology, including anxiety disorders and externalizing disorders (e.g., Weissman et al. 2006). With an estimated 10–15 million children under the age of 18 in the US living with a parent who has had at lease one depressive episode in their lifetime, identifying sources of risk and resilience for children of depressed parents is essential to select targets for intervention or prevention (e.g., Compas et al. 2011; England and Sim 2009). Processes that confer increased risk in children of depressed parents include biological and genetic predispositions, interpersonal processes, and psychological processes (Goodman 2007; Goodman and Gotlib 1999). Two important psychological characteristics that relate to psychopathology in this at-risk population are children’s coping and negative cognitive style.
Parental depression creates a chronically and unpredictably stressful environment for children because depression tends to recur (Weissman and Olfson 2009) and depressed parents vacillate between high levels of withdrawn (i.e., emotionally and physically unavailable) and intrusive (i.e., irritable and overly monitoring) behavior and emotions with their children (e.g., Hammen et al. 2004; Jaser et al. 2005, 2008). Because of the elevated levels of chronic stress in families of depressed parents, it is essential to understand how children cope with this stress. Coping can be broadly defined as “conscious, volitional efforts to regulate emotion, cognition, physiology and the environment in response to stressful events or circumstances,” (Compas et al. 2001) and includes efforts to directly act on or change the source of stress or one’s emotions (primary control coping), adapt to the stressor (secondary control coping), and attempts to avoid or deny the source of stress (disengagement coping; Connor-Smith et al. 2000).
Research has examined these three types of coping in children of depressed parents. Several studies have shown that greater use of secondary control coping strategies (e.g., acceptance, distraction, cognitive reappraisal) is associated with and predictive of lower levels of internalizing and depressive symptoms (e.g., Compas et al. 2010; Fear et al. 2009; Jaser et al. 2005, 2007, 2008; Langrock et al. 2002). On the other hand, previous studies with children of depressed parents have not found significant relations between primary control coping (e.g., problem-solving, emotional expression) and children’s depressive symptoms (Jaser et al. 2005; Langrock et al. 2002). In contrast, studies of adolescents coping with other types of stress (e.g., poverty and family conflict, peer stress, chronic pain) provide evidence that primary control coping is related to fewer internalizing, depression, and anxiety symptoms (e.g., Connor-Smith et al. 2000; Wadsworth and Compas 2002), and a more recent study of children of mothers with and without a history of depression found primary control coping to be related to lower levels of depressive symptoms (Jaser et al. 2011). Unlike primary and secondary control coping, studies have shown disengagement coping to be related to higher levels of depressive symptoms in children and adolescents (e.g., Agoston and Rudolph 2011; Santiago and Wadsworth 2009), but research with children of depressed parents has not found disengagement coping and children’s internalizing or externalizing symptoms to be significantly related (e.g., Jaser et al. 2005, 2007; Langrock et al. 2002).
Additional studies of children of depressed parents have provided similar evidence of an association between emotion-regulation skills, a construct closely related to coping, and children’s depressive symptoms (Compas et al. 2009). For example, Silk et al. (2006) found that children who were able to increase positive emotion during an adverse, negative emotion inducing laboratory-based task with their parent had lower levels of internalizing problems. Strategies such as distraction and cognitive reappraisal (which are both types of secondary control coping strategies) may underlie or enable this ability to up-regulate positive emotions (Jaser et al. 2011). Further, such emotion regulation skills may be similar to emotional modulation (one aspect of primary control coping). On the other hand, the use of more passive emotion regulation strategies by children of depressed parents, similar to disengagement coping, has been related to greater adjustment problems and lower abilities to reduce sadness and anger (e.g., Garber et al. 1991, 1995; Silk et al. 2003).
Cognitive vulnerability is a second significant psychological mechanism of risk for depression in children of depressed parents. One conceptualization of cognitive vulnerability is negative cognitive style, which refers to how a child thinks about the causes, consequences, and implications for one’s self after a negative event occurs (Hankin and Abramson 2002). The tendency to interpret causes of adverse events as stable (things will always be this way), global (this negative event affects many areas of life), and internal (this happened because of something about one’s self) defines negative attributional style. Negative cognitive style adds two additional elements to negative attributional style—expectations of other negative consequences and negative implications for one’s self as a result of adverse events, and is thus a more comprehensive measure of cognitive vulnerability for depression (Hankin & Abramson). There is robust evidence that children of depressed parents display a negative cognitive style in laboratory studies (e.g., Dearing and Gotlib 2009; Taylor and Ingram 1999), and higher levels of negative attributional style (e.g., Garber and Robinson 1997; Jaenicke et al. 1987) when compared to control children. Studies also provide consistent evidence that cognitive vulnerability, such as attributional style and negative self-schemas, is predictive of increased levels of depression symptoms in children of depressed parents even when accounting for initial levels of depression symptoms (e.g., Garber et al. 2002; Hammen 1988; Morris et al. 2008).
Although both cognitive vulnerability and coping are each related to depressive symptoms in children of depressed parents, the relationships between these processes have received relatively little attention. In a sample of college students, Hemenover and Dienstbier (1998) found that negative attributional style and avoidant coping both predicted depressive symptoms but coping and attributional style were not related to each other. Similarly, Ollendick et al. (2001) did not find a significant relationship between avoidant coping and attributional style in children who had experienced a traumatic event, but they found that avoidant coping and attributional style were significant and independent predictors of levels of children’s fear.
Prior studies of children of depressed parents have acknowledged that children’s cognitive vulnerabilities may interfere with their ability to cope effectively with stress (e.g., Goodman and Gotlib 1999; Hammen 1988) but this hypothesis has not been directly tested. Negative cognitive style may lead children to believe that they cannot control stressful situations or their reactions to those situations, that other negative events will occur in the future, and that there is no possibility that the situation can change. Thus, negative cognitive style may lead children to be more passive and less motivated in their responses to stressful events, engaging in fewer active coping strategies, such as primary and secondary control coping, and more passive coping strategies, such as disengagement coping. Further, it is possible that coping may modify or moderate the effects of negative cognitive style on depressive symptoms.
The current study tested hypotheses regarding the relations between coping, negative cognitive style, and depressive symptoms in a sample of children of depressed parents. First, we hypothesized that children1 with higher levels of negative cognitive style would use active coping strategies (primary and secondary control coping) less frequently and would use passive coping strategies (disengagement coping) more frequently. Second, we hypothesized secondary control coping to be related to lower levels of depressive symptoms; in addition we examined the association of primary control and disengagement coping with depressive symptoms. Third, we hypothesized that children who exhibit higher levels of negative cognitive style would have greater levels of depressive symptoms. Fourth, we hypothesized that negative cognitive style and secondary control coping would be independent predictors of depressive symptoms. In exploratory analyses we also examined interactions between negative cognitive style and each type of coping, testing whether primary and secondary control coping would act as protective factors at higher levels of negative cognitive style, and to test whether disengagement coping would act as an additional risk factor at higher levels of negative cognitive style.
Method
Participants
The sample consisted of 165 children (82 boys and 83 girls; ages 9–15-years-old) and their parents (17 fathers and 148 mothers). Mean parental age was 41.72 years, mean child age was 11.49 years, 73.3% of the children were Caucasian and 26.7% were of other racial and ethnic backgrounds (See Table 1 for additional demographic information). All parents had experienced at least one episode of major depressive disorder (MDD) during the lifetime of their child, with a median of 3 episodes of MDD during their child’s lifetime. In families with more than one child in the targeted age range, one child was randomly selected for inclusion in the analyses to avoid possible problems of non-independence of children within the same family.
Table 1.
Demographic variables of parents and children
| Parents (N = 165) |
Children (N = 165) |
|
|---|---|---|
| Age [mean (SD)] | 41.72 (7.50) | 11.49 (2.00) |
| Race [n (%)] | ||
| Caucasian | 135 (81.8) | 121 (73.3) |
| African–American | 19(11.5) | 23 (13.9) |
| Asian–American | 2 (1.2) | 4 (2.4) |
| Hispanic-American | 4 (2.4) | 3 (1.8) |
| American–Indian/Native Alaskan | 1 (0.6) | 1 (0.6) |
| Mixed ethnicity | 4 (2.4) | 13 (7.9) |
| Annual family income [n (%)] | ||
| <$5,000 | 11 (6.7) | |
| $5,000–$9,999 | 6 (3.6) | |
| $10,000–$14,999 | 3 (1.8) | |
| $15,000–24,999 | 17 (10.3) | |
| $25,000–39,999 | 34 (20.6) | |
| $40,000–59,999 | 28 (17.0) | |
| $60,000–$89,999 | 32 (19.4) | |
| $90,000–$179,999 | 22 (13.3) | |
| ≥$180,000 | 5 (3.0) | |
| Unknown | 7 (4.2) | |
| Education [n (%)] | ||
| Some high school | 9 (5.5) | |
| Graduated high school | 16 (9.7) | |
| Some college or technical school | 49 (29.7) | |
| Graduated college | 53 (32.1) | |
| One or more years graduate school | 38 (23.0) | |
| Marital status [n (%)] | ||
| Married/living with someone | 101 (61.2) | |
| Divorced | 35 (21.2) | |
| Separated | 9 (5.5) | |
| Never married | 18 (10.9) | |
| Widowed | 2 (1.2) |
Measures
Parental Depression Diagnoses
Parents’ past and current history of MDD was assessed and other Axis I disorders were screened with the Structured Clinical Interview for DSM (SCID; First et al. 2001), a semi-structured diagnostic interview used to assess current and previous episodes of psychopathology according to DSM-IV criteria (American Psychiatric Association 1994). Inter-rater reliability, calculated on a randomly selected subset of these interviews, indicated 93% agreement (κ = 0.71) for diagnoses of MDD.
Child Depressive Symptoms
The Child Behavior Checklist (CBCL) and the Youth Self-Report (YSR) were used to assess children’s symptoms of depression. Reliability and validity of the CBCL and YSR are well established (Achenbach and Rescorla 2001). The Affective Problems scale was used in the current analyses as an index of children’s depressive symptoms. Internal consistency for the scales used in this study were α = 0.72 for the CBCL and α = 0.81 for the YSR. 9 and 10 year-old children completed the YSR to allow for complete data on all measures. The internal consistency for the YSR scales was adequate with this younger age group in the current sample (all αs ≥ 0.75). Raw scores on the CBCL and YSR scores were used in all analyses to maximize variance (i.e., some variability is lost when the raw scores are converted to T-scores).
Children’s depressive symptoms were also quantified using the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL; Kaufman et al. 1997). The K-SADS-PL is a reliable and valid semi-structured interview that generates DSM-IV Axis I child psychiatric diagnoses. Separate interviews were conducted with parents and children and these responses were combined to yield both current and lifetime psychiatric diagnoses. Inter-rater reliability for diagnoses of MDD, calculated on a randomly selected subset of these interviews, indicated 96% agreement (κ = 0.76). The entire depression section of the K-SADS was administered to all children in the study and their participating parents. For data analyses, each threshold symptom was scored as a 2, each subthreshold symptom was scored as a 1, and any symptom not present was scored as 0. These symptom scores were then summed to represent the children’s total current depression symptoms on the K-SADS ranging from 0 to 18, giving more weight to a threshold symptom (2) than to a subthreshold symptom (1).
Parent and Child Reports of Children’s Coping
The parental depression version of the Responses to Stress Questionnaire (Connor-Smith et al. 2000; Jaser et al. 2005, 2008) was used to assess how the children responded to their parents’ depression. The three coping scales on the RSQ were used in the current study: primary control engagement coping (problem solving, emotional expression, emotional modulation), secondary control engagement coping (acceptance, distraction, positive thinking, cognitive reappraisal), and disengagement coping (denial, avoidance, wishful thinking) (Connor-Smith et al. 2000). Children and their parents individually rated each item with regard to the degree and/or frequency with which the children used the given coping strategy in response to a list of stressors associated with parental depression. To control for response bias and individual differences in base rates of item endorsement, proportion scores were calculated by dividing the total score for each coping and stress response factor by the total score for the entire RSQ (Vitaliano et al. 1987).
Internal consistency for primary control coping was α = 0.79 for parent report and child report, secondary control coping was α = 0.76 for parent report and α = 0.80 for child report and internal consistency for disengagement coping was α = 0.82 for parent report and α = 0.83 for child report. A separate composite measure was created for each scale (children’s primary control coping, secondary control coping, and disengagement coping) by converting scores from child and parent reports to z-scores and calculating the mean z-score for each participant (primary control composite: α = 0.81, secondary control composite: α = 0.76, disengagement composite: α = 0.83).
Child Reports of Negative Cognitive Style
The children’s negative cognitive style was measured using the mean score on the children’s report on the Adolescent Cognitive Style Questionnaire (ACSQ; Hankin and Abramson 2002). This measure presents the child with hypothetical negative events that were selected by the developers based on common experiences of childhood and adolescence. The original measure contains twelve situations, however, in this study, only four hypothetical situations were presented. The events used in the current study included “You get a bad report card for the semester”, “You get in a big fight with your parents”, “You don’t get chosen for an extracurricular activity (such as a sports team, club, or play) that you want to be a part of”, and “Someone says something bad about how you look”. The situations that were excluded for this study included several experiences more common for older adolescents (e.g., “You don’t get accepted to any colleges”; “You can’t get a date for a big dance you want to go to”).
The child is asked to write in a cause of the hypothetical experience then asked to rank 5 items on a scale of 1–7 (1 representing a low amount of negative cognitive style). A mean of these five items for all hypothetical events is computed to reach an overall score. The first three items measure attributional style: internal cause, stable cause and global cause. The additional two items ask the child to rate inferences for consequences and inferences for the self as a result of the hypothetical event. The internal consistency reliability for the ACSQ has been shown in prior research to be quite high. In this sample, internal consistency for the ACSQ overall score was α = 0.90, which reflects the findings of Hankin and Abramson (2002) in their original sample to test the psychometric properties of the measure (α = 0.95).
Procedure
Upon expressing interest in the study, each parent completed an initial phone interview to determine eligibility for the baseline assessment of the intervention study. If determined eligible via phone, the baseline assessment in the laboratory assessed psychological history and ultimately determined eligibility for randomization into the intervention trial via structured interviews and questionnaires.
Parent screening for eligibility for the intervention trial discerned that at least one parent in the family had experienced at least one major depressive episode or dysthymia during the child’s lifetime but also permanently excluded the following parental diagnoses or characteristics: bipolar I, schizophrenia, or schizoaffective disorder. If a parent was currently depressed and significantly impaired (established by a Global Assessment of Function, GAF, score at or below 50) or acutely actively suicidal, or met criteria for drug or alcohol use disorders accompanied by significant impairment (GAF ≤ 50), the family was placed on hold temporarily and then re-assessed at a later time (i.e. 2 months for depression with impairment or suicidality and 6 months for drug or alcohol problems with impairment). Once put on hold, the families were given treatment referrals if they wanted them. If suicidal ideation or impairment had improved at time of re-assessment, the family was then eligible to participate in the intervention. A family could be permanently excluded for certain child diagnoses as well: intellectual disability, pervasive developmental disorders, alcohol or substance use disorders, current conduct disorder, bipolar I disorder, and schizophrenia or schizoaffective disorder. Additionally, a family would be placed on hold for 2 months if a child met criteria for current depression or was acutely suicidal, then the same re-assessment procedure was applied as described above.
The University Institutional Review Boards at both sites approved all procedures in the study. Doctoral students in clinical psychology completed extensive training for the structured clinical interviews and conducted all interviews in university psychology laboratories at the two sites. All participants provided informed consent prior to participation in the study, and each participant received $40 compensation for their participation in the baseline assessments.
Data Analyses
To examine relationships between negative cognitive style, primary control coping, secondary control coping, disengagement coping, and depressive symptoms, bivariate Pearson correlations were used. To further examine negative cognitive style, primary control coping, secondary control coping, and disengagement coping as predictors of depressive symptoms, multiple linear regressions were conducted using the YSR/CBCL composite Affective Problems and the K-SADS MDD symptom score as dependent variables. Additionally, interactions between predictor variables in predicting depressive symptoms were also tested using multiple linear regression. We tested linear relationships, as opposed to conducting tests of nonlinear relationships because previous studies of the relations between coping and depressive symptoms and negative cognitive style and depressive symptoms have not suggested non-linear relationships.
With regard to missing data, all correlations and regressions were run using list-wise deletion, so the entire sample was analyzed in every test. If a child did not have data on every measure used in this study, he/she was excluded from analyses. On the item level, missing data were handled by creating pro-rated scores for each measure, such that a score was calculated if a child or parent had responded to at least 75% of the items on the measure.
Results
Means and standard deviations for all variables are presented in Table 2. Means and standard deviations were calculated on boys and girls separately and then on the sample as a whole. Due to prior research uncovering gender differences in negative cognitive style and depression (e.g., Hankin and Abramson 2002; Morris et al. 2008) t tests of means were conducted on all variables to test for gender differences, and none were significant. As a result, the sample as a whole was used for all analyses and gender was not included in any of these analyses.
Table 2.
Descriptive statistics for children’s coping, negative cognitive style, and depressive symptoms
| Entire sample (N = 165) Mean (SD) |
|
|---|---|
| Child negative cognitive style | 2.89 (1.07) |
| Child report primary control coping | 0.16 (0.04) |
| Parent report primary control coping | 0.17 (0.04) |
| Child report secondary control coping | 0.24 (0.05) |
| Parent report secondary control coping | 0.22 (0.05) |
| Child report disengagement coping | 0.21 (0.03) |
| Parent report disengagement coping | 0.20 (0.03) |
| YSR affective problems T score | 56.15 (7.71) |
| CBCL affective problems T score | 60.45 (8.00) |
| K-SADS symptoms of MDD | 3.59 (3.06) |
YSR Youth Self-Report, CBCL Child Behavior Checklist, K-SADS Kiddie Schedule for Affective Disorders and Schizophrenia
The mean on the ACSQ (M = 2.89) is comparable to that found in previous studies of negative cognitive style in adolescents (e.g., Hankin and Abramson 2002; Kercher and Rapee 2009). The mean T score on the YSR Affective Problems Scale was 56.15 (SD = 7.71), and on the CBCL Affective Problems scale, the mean T score was 60.45 (SD = 8.00), both of which are considered moderately elevated but below the clinical level of 70. A subgroup of children had scores on the affective symptoms scale at or above the clinical cut off of 70 (98th percentile) on the YSR (6.2%) and the CBCL (14.5%). These rates are 3–7 times higher than the rates found in the normative samples for these scales (2%) and suggest that this sample was at elevated risk for depression. On the K-SADS, the children in this sample were experiencing a mean of 2.11 (SD = 1.73) subthreshold symptoms of depression and a mean of 0.74 (SD = 1.11) threshold symptoms of depression, with a mean depressive symptoms score of 3.59 on the K-SADS. These data on the Affective Problems scale T scores and on the K-SADS support the at-risk nature of this sample of children.
Bivariate correlation analyses are presented in Table 3. These correlations ranged from small to medium in magnitude. As predicted by the first hypothesis, which described the relationships between negative cognitive style and coping, negative cognitive style was negatively related to primary control coping (r = −0.19, p < 0.05) and secondary control coping (r = −0.20,p < 0.01), and positively related to disengagement coping (r = 0.19, p < 0.05). In support of our second hypothesis, secondary control coping was negatively related to depressive symptoms (composite Affective Problems scale, r = −0.51, p < 0.001; K-SADS Symptoms of MDD, r = −0.35, p < 0.001). In our exploratory analyses, we found that primary control coping was negatively related to depressive symptoms (composite Affective Problems scale, r = −0.36, p < 0.001; K-SADS MDD Symptoms, r = −0.23, p < 0.01) and disengagement coping was positively related to depressive symptoms (composite Affective Problems scale, r = 0.19, p < 0.05). In regards to our third hypothesis, negative cognitive style was positively related to depressive symptoms (composite Affective Problems scale, r = 0.35, p < 0.001; K-SADS MDD Symptoms, r = 0.27, p < 0.01).
Table 3.
Bivariate correlation analyses
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Primary control coping | – | ||||
| 2. Secondary control coping | 0.24** | – | |||
| 3. Disengagement coping | −0 70*** | −0.17* | – | ||
| 4. Negative cognitive style | −0.19* | −0.20** | 0.19* | – | |
| 5. Composite affective problemsa | −0.36*** | −0.51*** | 0.19* | 0.35*** | – |
| 6. K-SADS symptoms of MDD | −0.23** | −0.35*** | 0.04 | 0.27** | 0.51*** |
N = 165
K-SADS Kiddie Schedule for Affective Disorders and Schizophrenia
p < 0.05;
p < 0.01;
p < 0.001
Composite affective problems refers to composite of Youth Self-Report and Child Behavior Checklist
Linear multiple regression analyses were conducted to test the remaining hypotheses (Tables 4, 5). Two models tested the main effects of negative cognitive style, primary control coping, secondary control coping and disengagement coping as independent predictors of depressive symptoms (Hypothesis four). These models also tested separate interactions between negative cognitive style and each type of coping (exploratory analysis). Blocks 1 and 2 in Table 4 present the main effects of negative cognitive style, primary control coping, secondary control coping, and disengagement coping predicting depressive symptoms measured by the YSR/CBCL Affective Problems Composite. Blocks 1 and 2 in Table 5 present the main effects with K-SADS MDD symptoms score as the dependent variable. Negative cognitive style was a significant predictor of depressive symptoms on both measures (Affective Problems, β = 0.21, p < 0.01; K-SADS MDD Symptoms, β = 0.15, p < 0.05). Primary control coping and secondary control coping were significant predictors of depressive symptoms on both measures (primary control coping: Affective Problems, β = −0.31, p < 0.01; K-SADS MDD Symptoms, β = −0.29, p < 0.01; secondary control coping: Affective Problems, β = −0.42, p < 0.001; K-SADS MDD Symptoms, β = −0.31, p < 0.001). Disengagement coping was a significant predictor of depressive symptoms as measured by the K-SADS MDD Symptoms (β = −0.26, p < 0.05), but not as measured by the Affective Problems composite (β = −0.14, NS). However, it is noteworthy that the beta weight is negative for disengagement coping in this model of main effects, despite the non-significant bivariate correlation between disengagement coping and depressive symptoms on the K-SADS, reflecting a possible suppressor effect.
Table 4.
Regression analyses testing negative cognitive style, primary control coping, secondary control coping, disengagement coping, and two-way interactions as predictors of affective symptoms
| β | sr2 | |
|---|---|---|
| DV: composite YSR/CBCL affective symptoms | ||
| Block 1: R2Δ = 0.12*** | ||
| Negative cognitive style | 0.35*** | 0.12 |
| Block 2: R2Δ = 0.26*** | ||
| Negative cognitive style | 0.24*** | 0.08 |
| Primary control coping | −0 32*** | 0.08 |
| Secondary control coping | −0.41*** | 0.20 |
| Disengagement coping | −0.15 | 0.02 |
| Block 3: R2Δ = 0.01 | ||
| Negative cognitive style | 0.21** | 0.06 |
| Primary control coping | −0.31** | 0.07 |
| Secondary control coping | 0.42*** | 0.20 |
| Disengagement coping | −0.14 | 0.02 |
| Negative cognitive style × primary control coping |
−0.16 | 0.02 |
| Negative cognitive style × secondary control coping |
0.02 | 0.00 |
| Negative cognitive style × disengagement Coping |
−0.08 | 0.00 |
| Final model R2 = 0.37***a |
N = 165
YSR Youth Self-Report, CBCL Child Behavior Checklist
β, Standardized beta; sr2, semi-partial correlation squared
p < 0.01;
p < 0.001
Model values are adjusted R2
Table 5.
Regression analyses testing negative cognitive style, primary control coping, secondary control coping, disengagement coping, and two-way interactions as predictors of K-SADS MDD symptoms
| β | sr2 | |
|---|---|---|
| DV: K-SADS MDD symptoms | ||
| Block 1: R2Δ = 0.07** | ||
| Negative cognitive style | 0.27** | 0.07 |
| Block 2: R2Δ = 0.14*** | ||
| Negative cognitive style | 0.20** | 0.05 |
| Primary control coping | −0.31** | 0.06 |
| Secondary control coping | −0.28*** | 0.08 |
| Disengagement coping | −0.27** | 0.04 |
| Block 3: R2Δ = 0.05* | ||
| Negative cognitive style | 0.15* | 0.03 |
| Primary control coping | −0.29** | 0.05 |
| Secondary control coping | −0.31*** | 0.10 |
| Disengagement coping | −0.26** | 0.04 |
| Negative cognitive style × primary control coping |
−0.27* | 0.04 |
| Negative cognitive style × secondary control coping |
0.08 | 0.01 |
| Negative cognitive style × disengagement coping |
−0.08 | 0.00 |
| Final model R2 = 0.23***a |
N = 165
K-SADS Kiddie Schedule for Affective Disorders and Schizophrenia
β, Standardized beta; sr2, semi-partial correlation squared
p < 0.05;
p < 0.01;
p < 0.001
Model values are adjusted R2
To explore possible two-way interactions of negative cognitive style and coping, predictor variables relevant to each interaction were centered and multiplied to create each interaction term, and the interaction terms were entered into the regression as independent variables to predict depressive symptoms (Aiken and West 1991). The results of these two-way interactions are displayed in Block 3 in Tables 4 and 5. Again, the dependent variable in Table 4 is the YSR/CBCL Affective Problems Composite and in Table 5 is the K-SADS index of MDD symptoms. The interaction between primary control coping and negative cognitive style was tested in Block 3 in Tables 4 and 5. When predicting the Affective Problems Composite score, this interaction was not significant (β = −0.16, NS), but when used to predict K-SADS MDD symptoms, the interaction between primary control coping and negative cognitive style was significant (β = −0.27, p = 0.01). The interaction between secondary control coping and negative cognitive style was also tested in Block 3 of Tables 4 and 5, and was not significant in predicting either the Affective Problems composite or the K-SADS MDD symptoms. Additionally, the interaction between disengagement coping and negative cognitive style (also seen in Block 3 of Tables 4, 5) was not significant in predicting depression symptoms as measured by the Affective Problems composite (β = −0.08, NS) or as measured by the K-SADS MDD symptoms (β = −0.08, NS).
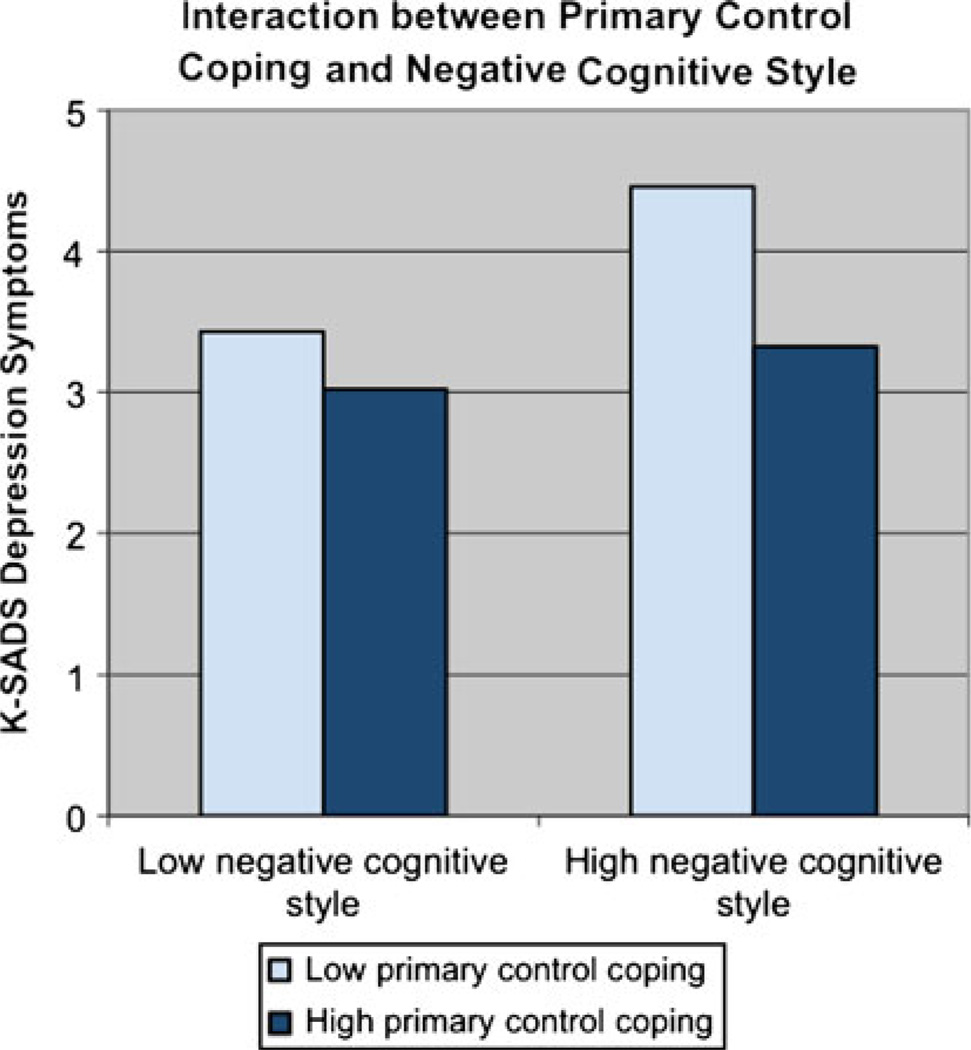
The significant interaction between primary control coping and negative cognitive style was explicated by dichotomizing primary control coping and negative cognitive style (using a median split of both variables) and then performing a univariate analysis of variance to compare the mean K-SADS symptom scores for each of the four groups. The results, presented in Fig. 1, indicate that, when negative cognitive style is high, a high (relative to a low) level of primary coping, appears to buffer children from depressive symptoms.
Fig. 1.
Interaction between negative cognitive style and primary control coping predicting K-SADS MDD symptoms. K-SADS Kiddie Schedule for Affective Disorders and Schizophrenia
Discussion
The current study contributes to research on children of depressed parents by examining coping and negative cognitive style as independent and interactive processes related to depressive symptoms and by and providing new evidence for relationships between negative cognitive style and coping and how they combine to predict depressive symptoms in this high risk population of youth. The findings provide clear support for the independent associations of primary control coping, secondary control coping, and negative cognitive style with depressive symptoms in children of depressed parents. Minimal support was found for the interaction of coping and negative cognitive style in predicting children’s depressive symptoms, further underscoring the relative independence of these two factors.
The current findings build on previous research by combining the constructs of negative cognitive style and coping. This study found a significant negative correlation between negative cognitive style and primary and secondary control coping and a significant positive correlation between negative cognitive style and disengagement coping. These relationships have been suggested in previous studies (Goodman and Gotlib 1999; Hammen 1988), but not empirically tested in children of depressed parents. These relationships suggest that children with more negative cognitive style may be more likely to use more passive strategies to cope with stress (i.e., disengagement coping) and less likely to use more active strategies to cope with stress (i.e., primary control and secondary control coping). The current study is the first to our knowledge to test this hypothesis in a sample of children of depressed parents. This finding is significant as it combines two previously separate areas of research on risk processes in children of depressed parents and provides a more complete picture of how these children think and cope in reaction to the stress associated with parental depression.
Evidence from the current correlation and regression analyses using questionnaire and interview measures of depressive symptoms adds support to the literature for the association between secondary control coping and fewer depressive symptoms (e.g., Jaser et al. 2005, 2007, 2008; Langrock et al. 2002). In terms of primary control coping, as shown in previous work with other populations of children and adolescents (e.g., Connor-Smith et al. 2000; Wadsworth and Compas 2002), higher levels of primary control coping were related to lower levels of depression on the questionnaire (CBCL, YSR composite) and interview (K-SADS) measures in correlations and regressions in this study. These findings differ from prior studies of offspring of depressed parents, which have not found significant relationships between primary control coping and depressive symptoms (e.g., Jaser et al. 2005; Langrock et al. 2002). It has been hypothesized that it may not be adaptive for a child to exercise problem solving in relation to the uncontrollable stress associated with parental depression (i.e., essentially trying to fix or solve the parent’s depression and related problems). However, the current findings suggest that problem solving along with the use of strategies such as emotional expression and emotional modulation (the other two aspects of primary control coping) to handle this type of stress may be adaptive.
In contrast to the consistent effects for primary and secondary control coping, minimal support was found for the association between disengagement coping and children’s depressive symptoms. Similar to other studies of children of depressed parents, the current study did not find conclusive or consistent evidence that more disengagement coping is related to more depressive symptoms, as it was weakly positively correlated with depressive symptoms measured on the questionnaires (YSR, CBCL Composite), but not with depressive symptoms measured by the interviews (e.g., Jaser et al. 2005, 2007; Langrock et al. 2002). In regression analyses, with depressive symptoms measured by questionnaires as the dependent variable, disengagement coping was not a significant predictor, but with K-SADS depressive symptoms as the dependent variable, it had a negative, statistically significant beta weight. The lack of correlation between disengagement coping and K-SADS depressive symptoms and the negative beta weight (i.e., in the opposite direction from the correlation between disengagement and depressive symptoms on the questionnaires) most likely indicate suppressor effects (Aiken and West 1991).
Also, similar to previous studies of cognitive vulnerability in children of depressed parents, we found negative cognitive style to be significantly positively related to depressive symptoms as measured by questionnaires (CBCL, YSR composite) and interview (K-SADS) in both correlations and regression (e.g., Garber et al. 2002; Hammen 1988; Morris et al. 2008). This provides additional evidence of the relationship between negative cognitive style and depressive symptoms in children and adolescents (Hankin 2008; Hankin and Abramson 2002) and adds to the growing literature on the association between cognitive vulnerability and depression in children of depressed parents.
When these processes were combined to predict depressive symptoms, negative cognitive style, primary control coping, and secondary control coping were all independent and significant predictors of depressive symptoms measured on questionnaires and interviews. Together, negative cognitive style and primary and secondary control coping accounted for 36% and 19% of the variance in children’s depressive symptoms measured by parent and child questionnaires and interviews, respectively. These findings are similar to those of Hemenover and Dienstbier (1998) and Ollendick et al. (2001) whose studies found that both avoidant coping and negative attributional style independently predicted adjustment (depressive symptoms and fear, respectively). Moreover, this current finding shows that there may be multiple avenues for intervention or prevention with children of depressed parents, including changing children’s negative cognitive style and their coping. It will be important for future prevention studies with children of depressed parents to incorporate both of these factors as intervention components.
Evidence was found for one of six interactions that were tested between negative cognitive style and coping—the interaction of primary control coping and cognitive style in predicting depressive symptoms on the K-SADS. The findings suggest that at high levels of negative cognitive style, coping can act as a buffer or protective factor for children of depressed parents. The other remaining five interactions tested were non-significant. As a consequence, negative cognitive style and coping appear, for the most part, to make independent contributions to children’s depressive symptoms.
The current study has several strengths. Coping was measured by a composite of parent and child report on the RSQ and depressive symptoms were measured by a composite of both the YSR and CBCL Affective Problems scale and by the total MDD symptoms as reported on the K-SADS. These measures of depressive symptoms represent multiple informant methods (i.e., parent and child reports on questionnaires and structured clinical interviews), thus reducing the likelihood of these findings resulting solely from the use of a single informant or single method and following recommendations for using multiple informants in the study of children of depressed parents (Goodman 2007; Kraemer et al. 2003).
This study also has several limitations, including the cross-sectional design, making it impossible to infer conclusions regarding causality. Additionally, the sample is not representative of all children of depressed parents since the study screened out children with current depression and current conduct disorder, among other disorders. Children with these diagnoses were excluded since this study was part of a larger family group preventive intervention study (Compas et al. 2009),
Future research should be conducted to address several goals. First, additional studies are needed to replicate the findings of relationships between negative cognitive style and coping. Additionally, research should focus on the independent and interactive relationships of negative cognitive style and coping with depressive symptoms. Longitudinal studies will help clarify these relationships and allow conclusions more congruent with causality to be reached. Finally, although gender differences did not emerge for any of the variables of interest in the current study, future studies should further examine the role of child gender.
In conclusion, the current study found significant relationships between coping (primary and secondary control and disengagement), negative cognitive style, and depressive symptoms in a sample of children of depressed parents. Some of these findings replicate past research, while others are new contributions to the field. The independent contributions of two types of coping and negative cognitive style to the prediction of depressive symptoms in this sample suggest the possibility of multiple avenues for prevention with this high-risk population of children. Future research, particularly longitudinal, is needed to replicate the new findings from this study in order to better understand children living in families with a depressed parent.
Acknowledgments
This research was supported by grants R01MH069940 and R01 MH069928 from the National Institute of Mental Health and by a gift from Patricia and Rodes Hart and Heinz and Rowena Ansbacher. The authors are grateful to Michelle Reising, Emily Hardcastle, Jennifer Thigpen, MJ Merchant, Lori Roberts, Kristen Reeslund, and Jessica Fear for their many contributions to this project.
Footnotes
The terms child and children will be used throughout to refer to our entire sample of 9–15 year old children and adolescents.
Contributor Information
Jennifer P. Dunbar, Department of Psychology and Human Development, Vanderbilt University, Peabody #552, 230 Appleton Place, Nashville, TN 37203, USA, jennifer.e.potts@vanderbilt.edu
Laura McKee, Psychology Department, Clark University, Worcester, MA, USA.
Aaron Rakow, Department of Psychology, University of Vermont, Burlington, VT, USA.
Kelly H. Watson, Department of Psychology and Human Development, Vanderbilt University, Peabody #552, 230 Appleton Place, Nashville, TN 37203, USA
Rex Forehand, Department of Psychology, University of Vermont, Burlington, VT, USA.
Bruce E. Compas, Department of Psychology and Human Development, Vanderbilt University, Peabody #552, 230 Appleton Place, Nashville, TN 37203, USA
References
- Achenbach TM, Rescorla LA. Manual for ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Agoston AM, Rudolph KD. Transactional associations between youths’ responses to peer stress and depression: The moderating roles of sex and stress exposure. Journal of Abnormal Child Psychology. 2011;39:157–171. doi: 10.1007/s10802-010-9458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbuy Park, CA: Sage; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Progress, problems, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. [PubMed] [Google Scholar]
- Compas BE, Forehand R, Champion JE, Reeslund KL, Fear JM, Hardcastle EJ, et al. Mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology. 2010;78:623–634. doi: 10.1037/a0020459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Keller G, Champion A, Cole DA, Reeslund KL, et al. Randomized clinical trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. 2009;77:1007–1020. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Keller G, Forehand R. Depression in adolescent girls: Science and prevention. New York, NY: Guilford Press; 2011. Preventive intervention in families of depressed parents: A family cognitive-behavioral intervention; pp. 318–339. [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68:976–992. [PubMed] [Google Scholar]
- Dearing KF, Gotlib IH. Interpretation of ambiguous information in girls at risk for depression. Journal of Abnormal Child Psychology. 2009;37:79–91. doi: 10.1007/s10802-008-9259-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- England MJ, Sim LJ. Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Fear JM, Champion JE, Reeslund KL, Forehand R, Colletti C, Roberts L, et al. Parental depression and interpersonal conflict: Children and adolescents’ self blame and coping responses. Journal of Family Psychology. 2009;23(5):762–766. doi: 10.1037/a0016381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, patient edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Garber J, Braafladt N, Weiss B. Affect regulation in depressed and nondepressed children and young adolescents. Development and Psychopathology. 1995;7:93–115. [Google Scholar]
- Garber J, Braafladt N, Zeman J. The regulation of sad affect: An information-processing perspective. In: Dodge KA, editor. The development of emotion regulation and dysregulation. Cambridge studies in social and emotional development. New York: Cambridge University Press; 1991. pp. 208–240. [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70(1):79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Garber J, Robinson NS. Cognitive vulnerability in children at risk for depression. Cognition and Emotion. 1997;11(5):619–635. [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Hammen C. Self cognitions, stressful events, and the prediction of depression in children of depressed parents. Journal of Abnormal Child Psychology. 1988;16(3):347–360. doi: 10.1007/BF00913805. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Shih JH. Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:994–1002. doi: 10.1097/01.chi.0000127588.57468.f6. [DOI] [PubMed] [Google Scholar]
- Hankin BL. Cognitive vulnerability-stress model of depression during adolescence: Investigating depressive symptom specificity in a multi-wave prospective study. Journal of Abnormal Child Psychology. 2008;36(1):999–1014. doi: 10.1007/s10802-008-9228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Measuring cognitive vulnerability to depression in adolescence: Reliability, validity and gender differences. Journal of Clinical Child and Adolescent Psychology. 2002;31(4):491–504. doi: 10.1207/S15374424JCCP3104_8. [DOI] [PubMed] [Google Scholar]
- Hemenover SH, Dienstbier RA. Prediction of health patterns from general appraisal, attributions, coping, and trait anxiety. Motivation and Emotion. 1998;22(3):231–253. [Google Scholar]
- Jaenicke C, Hammen C, Zupan B, Hiroto D, Gordon D, Adrian B, et al. Cognitive vulnerability in children at risk for depression. Journal of Abnormal Child Psychology. 1987;15(4):559–572. doi: 10.1007/BF00917241. [DOI] [PubMed] [Google Scholar]
- Jaser SS, Champion JE, Dharamsi KR, Reising MM, Compas BE. Coping and positive affect in adolescents of mothers with and without a history of depression. Journal of Child and Family Studies. 2011;20:353–360. doi: 10.1007/s10826-010-9399-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser SS, Champion JE, Reeslund KL, Keller G, Merchant MJ, Benson M, et al. Cross-situational coping with peer and family stressors in adolescent offspring of depressed parents. Journal of Adolescence. 2007;30:917–932. doi: 10.1016/j.adolescence.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Jaser SS, Fear JM, Reeslund KL, Champion JE, Reising MM, Compas BE. Maternal sadness and adolescents’ responses to stress in offspring of mothers with and without a history of depression. Journal of Clinical Child and Adolescent Psychology. 2008;37:736–746. doi: 10.1080/15374410802359742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser SS, Langrock AM, Keller G, Merchant MJ, Benson MA, Reeslund KL, et al. Coping with the stress of parental depression II: Adolescent and parent reports of coping and adjustment. Journal of Clinical Child and Adolescent Psychology. 2005;34:193–205. doi: 10.1207/s15374424jccp3401_18. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kercher A, Rapee RM. A test of a cognitive diathesis stress generation pathway in early adolescent depression. Journal of Abnormal Child Psychology. 2009;37(6):845–855. doi: 10.1007/s10802-009-9315-3. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Measelle JR, Ablow JC, Essex MJ, Boyce W, Kupfer DJ. A new approach to integrating data from multiple informants in psychiatric assessment and research: Mixing and matching contexts and perspectives. American Journal of Psychiatry. 2003;160:1566–1577. doi: 10.1176/appi.ajp.160.9.1566. [DOI] [PubMed] [Google Scholar]
- Langrock AM, Compas BE, Keller G, Merchant MJ, Copeland ME. Coping with the stress of parental depression: Parents’ reports of children’s coping, emotional, and behavioral problems. Journal of Clinical Child and Adolescent Psychology. 2002;31:312–324. doi: 10.1207/S15374424JCCP3103_03. [DOI] [PubMed] [Google Scholar]
- Morris MC, Ciesla JA, Garber J. A prospective study of the cognitive stress model of depressive symptoms in adolescents. Journal of Abnormal Psychology. 2008;117(4):719–734. doi: 10.1037/a0013741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, Langley AK, Jones RT, Kephart C. Fear in children and adolescents: Relations with negative life events, attributional style, and avoidant coping. Journal of Child Psychology and Psychiatry. 2001;42(8):1029–1034. [PubMed] [Google Scholar]
- Santiago CD, Wadsworth ME. Coping with family conflict: What’s helpful and what’s not for low-income adolescents. Journal of Child and Family Studies. 2009;18:192–202. [Google Scholar]
- Silk JS, Shaw DS, Forbes EE, Lane TL, Kovacs M. Maternal depression and child internalizing: The moderating role of child emotion regulation. Journal of Clinical Child and Adolescent Psychology. 2006;35:116–126. doi: 10.1207/s15374424jccp3501_10. [DOI] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Taylor L, Ingram RE. Cognitive reactivity and depressotypic information processing in children of depressed mothers. Journal of Abnormal Psychology. 1999;108(2):202–210. doi: 10.1037//0021-843x.108.2.202. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Maiuro RD, Russo J, Becker J. Raw versus relative scores in the assessment of coping strategies. Journal of Behavioral Medicine. 1987;10:1–18. doi: 10.1007/BF00845124. [DOI] [PubMed] [Google Scholar]
- Wadsworth ME, Compas BE. Coping with family conflict and economic strain: The adolescent perspective. Journal of Research on Adolescence. 2002;12(2):243–274. [Google Scholar]
- Weissman MM, Olfson M. Translating intergenerational research into clinical practice. Journal of America Medical Association. 2009;302(24):2695–2696. doi: 10.1001/jama.2009.1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]