Abstract
Systemic lupus erythematosus (SLE) is a complex autoimmune disease characterized by an overproduction of autoantibodies. The loss of self-tolerance in SLE is believed to be caused by the dysregulation of both innate and adaptive immune systems. Neutrophils, the most abundant effector cells of innate immunity, have long been shown to be associated with SLE. However, their role in the pathogenesis of SLE was not clear until recent studies discovered abnormal regulation of neutrophil extracellular traps (NETs) in SLE patients. NETs are web-like structures composed of chromatin backbones and granular molecules. They are released by activated neutrophils through a process called “NETosis”. Nets were first described in 2004 as a novel host defense mechanism to trap and kill foreign pathogens. Recent evidence shows that NETs also participate in the pathogenesis of a variety of inflammatory and autoimmune diseases, including SLE. An imbalance between NET formation and clearance in SLE patients may play a prominent role in the perpetuation of autoimmunity and the exacerbation of disease, as well as the induction of end-organ manifestations. This review summarizes the current findings regarding the contribution of NETs to the pathogenesis of SLE.
Keywords: Neutrophils, Neutrophil extracellular traps, Lupus, Pathogenesis, Autoimmune, Interferon
Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disorder with diverse clinical manifestations. The symptoms range from mild skin rashes to life-threatening multi-organ manifestations. SLE is characterized by the loss of tolerance to self antigens and the overproduction of autoantibodies. Over the past decades, major efforts have been attributed to the study of the dysregulation of adaptive immunity [1,2]. Indeed, abnormalities of B and T lymphocytes and their interplays with other factors, such as genetics, hormone and environment, are crucial to the development of SLE [3]. In recent years, accumulated evidence has brought more attention to the innate immune system’s active role in driving the autoimmune response and tissue damage in SLE. Indeed, components of innate immunity, including macrophages, dendritic cells and neutrophils, have been suggested to play pivotal roles in the pathogenesis of SLE [4–6].
Neutrophils are the dominant immune cells in the circulation and serve as the front line of host defense against invading pathogens. Upon activation, neutrophils attack and destroy pathogens by phagocytosis, along with releasing bactericidal peptides, proteolytic enzymes, reactive oxygen species (ROS), and the recently described neutrophil extracellular traps (NETs) [7–10]. Meanwhile, the activation of neutrophils could damage local host tissues and lead to organ manifestations in diseased conditions [8,11]. It is now well appreciated that neutrophils not just play a destructive role, but also a driving role in the pathogenesis of a variety of inflammatory and autoimmune disorders, such as sepsis, vasculitis, and SLE [12–14].
Neutrophils derived from SLE patients display a number of abnormal features in their phenotype and function, such as increased aggregation, increased apoptosis that may lead to neutropenia, impaired phagocytosis that may lead to delayed clearance of apoptotic cell debris, and enriched low-density granulocytes (LDG) in the peripheral blood [5,15–17]. Moreover, elevated levels of various neutrophil granular proteins and anti-neutrophil cytoplasmic antibodies (ANCA) have been found in the sera of SLE patients, although their exact role in SLE remains unclear [18–21]. In the past three years, several intriguing studies have linked NETs to the pathogenesis of SLE. In this review, we discuss our current understanding of NETs and their role in the pathogenesis of SLE.
Neutrophil Extracellular Traps
In 2004, Dr. Zychlinsky’s group discovered that activated neutrophils release neutrophil extracellular traps (NETs) as a novel antimicrobial mechanism [10]. NETs are formed through a unique cell death process, termed “NETosis”. They are composed of decondensed chromatin DNA in association with histones, granular proteins, and a few cytoplasmic proteins [10,22–24]. Neutrophils die through this beneficial suicide to ensnare and kill the extracellular bacteria, fungi, and parasites, and furthermore to neutralize viruses, by delivering a high local concentration of antimicrobial agents, such as histones, myeloperoxidase (MPO), neutrophil elastase (NE), LL37, and reactive oxygen species (ROS) [10,25–29].
A variety of stimuli can trigger NETosis, including pathogens, pro-inflammatory cytokines (interleukin 8 (IL-8), tumor necrosis factor α (TNFα)), activated platelets and endothelial cells, phorbol 12-myristate 13-acetate (PMA), nitric oxide, monosodium urate crystals, ANCAs, and immune complexes [10,12,30–35]. This process involves different receptors, such as Toll-like receptors (TLRs), Ig Fc receptors, and receptors for cytokines [10,35]. Although the detailed signaling pathways for NET formation remain elusive, it is believed that the generation of ROS by nicotinamide adenine dinucleotide phosphate (NADPH) oxidase is indispensable, as treatment with diphenyleneiodonium (DPI), a NADPH oxidase inhibitor, can prevent NETosis. Moreover, neutrophils from patients with chronic granulomatous disease, who have mutations in NADPH oxidase, fail to make NETs [22]. Following the ROS production, the nuclear envelope and granule membranes rupture, and the chromatin decondenses in the cytoplasm and binds to granular and cytoplasmic proteins before releasing to the extracellular space. Other processes, such as histone citrullination by peptidylarginine deiminase 4 (PAD4), microtubule polymerization, actin filamentation, and autophagy have been shown to be involved in NETosis [36–41].
The Adverse Effects of NETs
Despite their beneficial effects in host defense, NETs occur at the expense of injury to the host. The formation and removal of NETs should be timely regulated and failure to do so will lead to unfavorable consequences.
The tissue damaging effects of NET have been observed under many pathological conditions. In severe sepsis, interaction between platelets and neutrophils and the activation of Toll-like receptor pathways lead to the rapid formation of NETs, which trap and kill bacteria in circulation. However, this antibacterial mechanism has been shown to also bring damage to the endothelium in vitro and in vivo [12]. Moreover, excessive NETs inside the vasculature provide a scaffold and stimulus for thrombus formation [42–46]. Cystic fibrosis (CF) patients suffer from chronic neutrophilic inflammation that leads to lung destruction. Recently, it has been shown that abundant NETs are present in the sputum of CF patients, which are associated with impaired lung function [47]. Moreover, NETs have been detected in the lungs and plasma of patients with transfusion-related acute lung injury (TRALI); along with in the alveoli of mice with antibody-mediated TRALI. These findings suggest that NETs are responsible for the endothelial damage and capillary leakage in the lung [48,49].
The integrity of the NET structure and its components such as histones, granular enzymes, and ROS, mediate the tissue damaging effects of NET. NET-induced cytotoxicity could be abrogated or reduced by treatment with NADPH inhibitors that block NETosis, deoxyribonuclease (DNase) that disrupts NET, or blocking antibodies against histones or MPO [31,50]. Notably, administration of histone blocking antibody or DNase I protected mice from TRALI and anti-histone H4 antibody treatment reduced the mortality of mice in a sepsis model [48,49,51].
Another dark side of NETosis is that it may provide a novel source of autoantigens. This view is supported by the observation that infections by pathogens which frequently involve NETosis are prime candidates for initiating or enhancing autoimmune disease [52]. The first evidence for the association of NETosis with autoimmunity was obtained in a study of small vessel vasculitis (SVV) [33]. SVV is a chronic autoimmune disease with necrotic inflammation of small blood vessels and is usually associated with anti-neutrophil cytoplasmic antibodies (ANCAs), such as proteinase-3 (PR3) and MPO ANCAs. ANCAs activate neutrophils to release ROS, destructive granular molecules, and proinflammatory cytokines, as shown in vitro and in animal models [53–55]. In 2009, Kessenbrock et al. [33] reported that ANCAs from SVV patients could stimulate neutrophils to release NETs which contain the autoantigens MPO and PR3. Moreover, the levels of circulating NET components were elevated in active SVV patients and NETs were detected in inflamed kidney biopsies from SVV patients. This study implicates that NETosis plays a pathogenic role in autoimmune SVV by both presenting autoantigens to the immune system and mediating vascular damage.
Impaired NET Degradation in SLE
The hallmark of SLE is the over-production of autoantibodies against a range of nuclear antigens including double-stranded DNA (dsDNA) and histones. In addition, 25%–56% SLE patients have ANCAs in their sera [56]. Since these autoantigens are the major components of NETs, it is reasonable to postulate that the dysregulation of NETs may be involved in the SLE etiology. Indeed, two recent independent studies showed that sera from SLE patients have a decreased ability to degrade NETs and the impaired NET degradation is associated with increased anti-dsDNA antibody titers.
In 2010, Hakkim et al. [57] found that serum endonuclease DNase I is responsible for NET degradation. Interestingly, a subset of SLE sera (36.1%) in their cohort degraded NET poorly. Those “non-degraders” can be further divided into two groups. Group 1’s degradation activity could be rescued by an irrelevant micrococcal nuclease (MNase), while group 2 could not. Therefore, two mechanisms responsible for the impaired NET degradation in SLE were proposed: the presence of DNase I inhibitors (group 1) or anti-NET antibodies that protect NETs from degradation (group 2). This observation was in agreement with previous reports that some SLE patients have DNase I inhibitory antibodies in their sera, and that anti-DNA antibodies protect DNA from DNase digestion [58,59]. Notably, DNase I gene mutation and polymorphism are shown to be associated with SLE in Japanese and Korea cohorts [60,61]. It is tempting to speculate that patients with the mutated DNase I gene have an impaired ability to degrade NETs.
Furthermore, Hakkim et al. [57] showed that patients with defective NET degradation tended to have higher levels of anti-NET and anti-dsDNA autoantibodies as well as a higher frequency of developing lupus nephritis. These finding can be explained by the fact that NETs act as a source of antigens to stimulate autoantibody production.
Using a different SLE cohort, Leffer et al. [62] confirmed the impaired NET degradation in SLE patients. However, unlike the observations by Hakkim et al. [57], the impaired NET degradation of all their non-degraders could be rescued by the addition of exogenous DNase I. They also found that the NET-degrading ability is not a constant feature of an individual patient, but varies with the disease activity. Most of their “non-degraders” restored their ability to degrade NETs when they are in remission. Impaired NET degradation was also strongly correlated with glomerulonephritis, as well as pleuritis. Leffer et al. [62] found that NETs bind to the classical complement pathway component C1q to activate a complement cascade and consume complement factors in the serum. Interestingly, C1q deposited to NETs could in turn serve as a DNase I inhibitor to protect NETs from degradation. The deposition of complement on NETs may also promote autoantibody production, as the co-ligation of the antigen receptor with the complement receptor 2 (CD21) by the NET-complement complexes can reduce the threshold for B cell activation [63].
Taken together, these two studies provide convincing evidences that a subset of SLE patients display impaired NET degradation in their sera and the impaired NET degradation is associated with increased anti-dsDNA titers and lupus nephritis. The persistence of non-degraded NETs may lead to the production of autoantibodies against NETs and the activation of the complement system, which in turn block NET degradation, thus forming a vicious circle. The association of impaired NET degradation with organ involvement provides a potential diagnostic marker and therapeutic target.
NETs Drive Plasmacytoid Dendritic Cells to Produce Type I Interferon in SLE
Type I interferons (IFNs) play a crucial pathogenic role in SLE. The levels of type I interferons are elevated in the sera of SLE patients and correlated with disease activity [64,65]. A large number of IFN-inducible genes are upregulated in peripheral blood mononuclear cells from SLE patients with active disease (the so-called “IFNα signature”) [66,67]. Type I IFNs contribute to the breakdown of the peripheral tolerance in SLE by sustaining the differentiation of monocytes to myeloid dendritic cells (mDCs). These IFN-matured mDCs efficiently present autoantigens to CD4+ T cells, leading to the expansion of autoreactive T and B cells [68]. Currently, plasmacytoid dendritic cells (pDCs) are thought to be the main producer of type I IFNs. In SLE, immune complexes containing self-DNA or -RNA can activate pDCs to release IFN-α through the engagement of TLR9 and TLR7 respectively [68–70].
In 2011, Lange [34] and Garcia-Romo et al. [35] reported that neutrophils from SLE patients are more prone to release NETs and that NETs can potently activate pDCs to produce IFN-α. Lande et al. [34] showed that DNA immune complexes containing neutrophil-derived antimicrobial peptides, such as LL37 and human neutrophil peptide (HNP) in SLE patient sera can activate pDCs with subsequent INF-a production. The antimicrobial peptides in the complexes protect DNA from extracellular degradation and are required for the complexes to activate pDCs. They further showed that such immunogenic self DNA-antimicrobial peptide complexes were originated from NETosis, which could be triggered by anti-LL37 and anti-HNP autoantibodies in SLE patient sera. Interestingly, the authors also found that IFN-α can prime neutrophils to express more LL37 and HNP on their surface, thereby promoting the release of more NETs upon anti-LL37 and anti-HNP antibody stimulation. Accordingly, neutrophils from SLE patients were shown to be poised to release more NETs than neutrophils from healthy controls in response to anti-LL37 and anti-HNP antibodies.
In a parallel study, Garcia-Romo et al. [35] analyzed gene expression profiles of neutrophils from pediatric SLE patients and demonstrated a prominent transcriptional signature of type I IFN and TLR signaling. Based on the observation that expression of TLR7 is up-regulated in SLE patients, Garcia-Romo et al. [35] further showed that anti-ribonucleoprotein (RNP) immune complexes could activate neutrophils from SLE patients, but not those from healthy controls, to release NETs. This process requires FcRIIa internalization and TLR7 activation and is dependent on the ROS formation. These NETs could potently activate pDCs, leading to secretion of high levels of IFN-α.
In agreement with the work of Lande et al. [34], Garcia-Romo et al. [35] also revealed that IFN-α treatment can make neutrophils from healthy controls more susceptible to NETosis.
Collectively, the above studies revealed a novel mechanism for the involvement of neutrophils in SLE pathogenesis. A potential self-amplifying feedback loop is also elucidated: SLE neutrophils readily release NETs in response to autoantibodies or exogenous stimuli, such as bacterial or viral infection; these NETs can then potently activate pDCs to release high levels of IFN-α which in turn primes neutrophils for additional NETosis. This loop works in concert with the other effects of IFN-α to promote the disease development and progression in SLE.
Low Density Granulocytes Have Heightened Capacity to Make NETs in SLE
In addition to the “IFN signature”, SLE patients also display a granulopoiesis signature with an increased expression of neutrophil-specific genes in their peripheral blood mononuclear cell fractions (PBMCs) [67]. The granulopoiesis signature is due to an increased percentage of low density granulocytes (LDGs) co-purified with PBMCs [67,71]. Compared with normal-density neutrophils, LDGs have an impaired phagocytic ability with a proinflammatory phenotype and are likely to be pathogenic as they synthesize increased levels of type I IFNs and induce cytotoxicity to endothelial cells [5].
Villanueva et al. [72] further characterized LDGs from SLE patients by gene array and found that a number of bactericidal proteins and alarmins were up-regulated in LDGs when compared with normal-density SLE and control neutrophils. In addition, LDGs show enhanced capacity to release NETs, leading to an increased externalization of NET antigens including LL37 and dsDNA, as well as the proinflammatory cytokine IL-17 [72]. Through NETosis, LDGs mediate enhanced cytotoxicity to endothelial cells, which may lead to the development of premature vascular damage in SLE. Furthermore, NETing neutrophils were detected in the affected kidneys and skin lesions of SLE patients, with the exposure of LL37 and dsDNA at the tissue level. In accordance with the hypothesis that NETosis could provide a new source of autoantigens, patients with netting neutrophils in tissues also had higher levels of anti-dsDNA antibodies in their sera [72]. Overall, these findings have provided direct evidence for the pathogenic role of LDGs in SLE, to which augmented NETosis may contribute significantly.
NETs Mediate Enhanced Inflammasome Activation in SLE
Inflammasomes are intracellular multiprotein complexes that mediate the activation of caspase-1 in response to pathogens or endogenous “danger” stimuli, and lead to the release of mature proinflammatory cytokines IL-1β and IL-18 [73]. Aberrant inflammasome activation and enhanced IL-18 production may contribute to the development of cardiovascular disease in SLE, as IL-18 impairs the differentiation of endothelial progenitor cells (EPCs) and circulating angiogenic cells (CACs) to mature endothelial cells, which is crucial for vascular repair. IL-18 may also play a pathogenic role in renal and cutaneous manifestations in SLE [74–77].
Intriguingly, both NETs and NET-associated LL37 can effectively activate the inflammasome machinery [77]. Exposure of LPS-primed primary macrophages to NETs or LL37 leads to the activation of caspase-1, the central enzyme of the inflammasomes, resulting in the release of IL-1β and IL-18 [77]. LL37 activates caspase-1 by promoting the assembly of NOD-like receptor pyrin domain containing-3 (NLRP3) inflammasome in macrophages. Furthermore, NET and LL37-stimulated inflammasome activation is enhanced in SLE macrophages due to their lower threshold for activation than control macrophages [77], which may account for the elevated IL-18 levels in SLE patients [78,79]. In turn, both the secreted IL-1β and IL-18 are able to induce NET formation, thus forming a positive feedback loop which exacerbates the disease progression in SLE [40,77].
NETs in Mouse Models of SLE
All of the above patient studies suggest a critical role of NETs in the induction of autoimmunity and the development of tissue damage in SLE. However, the pathogenic role of NETs in mouse models of SLE still remains to be clarified.
Controversial results are reported in different lupus-prone mouse strains. In 2010, Guiducci et al. [80] developed a mouse model of inflammatory skin disease using tape stripping, which resulted in rapid but transient infiltration of activated pDCs with type I IFN production and activated neutrophils with robust NET formation in normal mice. The same tape-stripping treatment in lupus-prone New Zealand Black/New Zealand White (NZB/W) F1 mice caused the development of chronic skin lesions with many similarities to human cutaneous lupus. TLR7 and TLR9 signaling as well as pDC and neutrophil activation are all required for the induction and maintenance of the skin lesions. As persistent infiltration of NET-producing neutrophils were detectable in the skin lesions of NZB/NZW F1 mice, Guiducci et al. [80] postulated that the released NET fibers containing DNA and RNA might serve as a source of ligands for TLR9 and TLR7, thus contributing to the chronic skin inflammation in lupus-prone NZB/W F1 mice.
In agreement with the above study, Knight et al. [81] reported in a meeting abstract that neutrophils from lupus-prone New Zealand Mixed (NZM) 2328 mice displayed enhanced spontaneous NETosis compared to neutrophils from C57BL/6 and BALB/c mice. Those NZM mice also develop anti-NET autoantibodies. In addition, NET-like complexes were detected in both nephritic NZM kidneys and in non-affected NZM skin, which implicates the potential role of NETosis in organ damage in SLE. However, Campbell et al. [82] revealed that neutrophils from lupus-prone MRL.Faslpr mice showed similar levels of spontaneous NET formation compared to BALB/c and BALB/c.Faslpr mice.
According to the observation that NETosis requires the activity of NADPH oxidase, Campbell et al [82] generated a Nox2 (a subunit of NADPH)-deficient MRL.Faslpr mouse model in which neutrophils cannot undergo NETosis. Surprisingly, they found that the Nox2-deficient mice had exacerbated lupus-related symptoms, suggesting that Nox2-dependent NET formation is not the driver of lupus and NADPH oxidase rather has a protective role in this lupus model.
These contradicting results obtained from different murine models of lupus may be due to the intrinsic differences among those mouse strains, which may or may not represent what happens in human patients. As a complex and heterogeneous autoimmune disease, SLE etiology involves the interplay of multiple pathways and networks in the immune system. This will make it difficult to find a certain pathway essential for the development of SLE. Nevertheless, as a novel strategy for host defense against invading pathogens, NETosis normally occurs with beneficial effects to the host and only causes disease when occurring at the wrong time, in the wrong place, or with the wrong magnitude [83].
Conclusion
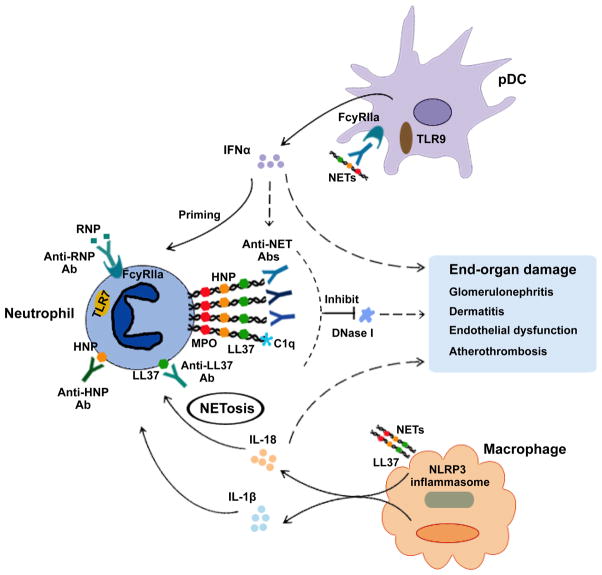
The contribution of NETs to SLE and autoimmunity is an expanding field of research. The studies mentioned above have led to some intriguing conclusions, but have also left many questions unanswered. Like all immune responses, a homeostasis should be maintained to avoid unfavorable consequences. Neutrophils from SLE patients are more susceptible to produce NETs and a subset of SLE patients display an impaired NET clearance ability. The persistently exposed NET components may directly damage tissues and may also serve as a novelsource of autoantigens to augment the autoimmune response. Furthermore, the interplay among NETs, type I interferons, and inflammasomes results in several pathogenic positive feedback loops that could perpetuate the inflammation and exacerbate the disease progression in SLE (Figure 1). However, the pathogenic role of NETs in lupus in vivo remains to be clarified. Nevertheless, it is of great interest to determine whether the prevalence of NETs can be used as a diagnostic biomarker or as a predictor for SLE disease activity and tissue/organ damage. Finally, as our understanding of NETs increases, the modulation of NETosis may open up new avenues for the development of therapeutic strategies for SLE and other inflammatory diseases.
Figure 1. Self-amplifying feed-forward loops of NETosis in SLE.
In SLE patients, NETosis can be triggered by anti-LL37 or HNP autoantibodies or RNP/anti-RNP immune complexes with subsequent engagement of TLR7. A subset of SLE patients failed to clear NETs due to the DNase I inhibitory components in the serum (such as NET-associated anti-NET Abs, LL37 or C1q). NETs are taken up by pDC in an FcRIIa and TLR9 dependent manner, leading to the release of IFNα. IFNα in turn can prime neutrophils for enhanced NETosis by upregulating TLR7 and surface granular proteins (such as LL37 and HNP). IFN also triggers autoreactive T and B cell activation, resulting in the production of anti-NET Abs, such as anti-dsDNA, anti-LL37, and anti-HNP Abs. NETs and LL37 alone can activate the NLRP3 inflammasome in macrophages to induce the synthesis of IL-1β and IL-18, both of which can stimulate NETosis. Those pathogenic loops may eventually lead to an imbalanced immune homeostasis that contributes to the disease initiation and progression of SLE.
Abbreviations: SLE: Systemic Lupus Erythematosus; FcRIIa: Immunoglobulin- Fc region receptor II-a; RNP: Ribonucleoprotein; Ab: Antibody; TLR: Toll-like Receptor; NET: Neutrophil Extracellular Traps; DNase: Deoxyribonuclease; pDC: Plasmacytoid Dendritic Cell; IFN: Interferon; HNP: Human Neutrophil Peptide; NLRP3: NOD-like receptor, pyrin domain containing-3; IL: Interleukin.
Acknowledgments
We thank Dr. Zhixin Zhang, Dallas Jones, and Chuck Hay for their review of the manuscript. Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01AR059351 to KS and by a Research Support Fund grant from the Nebraska Medical Center and the University of Nebraska Medical Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Crispín JC, Kyttaris VC, Terhorst C, Tsokos GC. T cells as therapeutic targets in SLE. Nat Rev Rheumatol. 2010;6:317–325. doi: 10.1038/nrrheum.2010.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dörner T, Jacobi AM, Lee J, Lipsky PE. Abnormalities of B cell subsets in patients with systemic lupus erythematosus. J Immunol Methods. 2011;363:187–197. doi: 10.1016/j.jim.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Crispín JC, Liossis SN, Kis-Toth K, Lieberman LA, Kyttaris VC, et al. Pathogenesis of human systemic lupus erythematosus: recent advances. Trends Mol Med. 2010;16:47–57. doi: 10.1016/j.molmed.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denny MF, Chandaroy P, Killen PD, Caricchio R, Lewis EE, et al. Accelerated macrophage apoptosis induces autoantibody formation and organ damage in systemic lupus erythematosus. J Immunol. 2006;176:2095–2104. doi: 10.4049/jimmunol.176.4.2095. [DOI] [PubMed] [Google Scholar]
- 5.Denny MF, Yalavarthi S, Zhao W, Thacker SG, Anderson M, et al. A distinct subset of proinflammatory neutrophils isolated from patients with systemic lupus erythematosus induces vascular damage and synthesizes type I IFNs. J Immunol. 2010;184:3284–3297. doi: 10.4049/jimmunol.0902199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ding D, Mehta H, McCune WJ, Kaplan MJ. Aberrant phenotype and function of myeloid dendritic cells in systemic lupus erythematosus. J Immunol. 2006;177:5878–5889. doi: 10.4049/jimmunol.177.9.5878. [DOI] [PubMed] [Google Scholar]
- 7.Finkel T. Neutrophils with a license to kill: permeabilized, not stirred. Dev Cell. 2003;4:146–148. doi: 10.1016/s1534-5807(03)00023-6. [DOI] [PubMed] [Google Scholar]
- 8.Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol. 2006;6:173–182. doi: 10.1038/nri1785. [DOI] [PubMed] [Google Scholar]
- 9.Nauseef WM. How human neutrophils kill and degrade microbes: an integrated view. Immunol Rev. 2007;219:88–102. doi: 10.1111/j.1600-065X.2007.00550.x. [DOI] [PubMed] [Google Scholar]
- 10.Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 11.Borregaard N, Sørensen OE, Theilgaard-Mönch K. Neutrophil granules: a library of innate immunity proteins. Trends Immunol. 2007;28:340–345. doi: 10.1016/j.it.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Clark SR, Ma AC, Tavener SA, McDonald B, Goodarzi Z, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med. 2007;13:463–469. doi: 10.1038/nm1565. [DOI] [PubMed] [Google Scholar]
- 13.Jennette JC, Falk RJ. New insight into the pathogenesis of vasculitis associated with antineutrophil cytoplasmic autoantibodies. Curr Opin Rheumatol. 2008;20:55–60. doi: 10.1097/BOR.0b013e3282f16c0a. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan MJ. Neutrophils in the pathogenesis and manifestations of SLE. Nat Rev Rheumatol. 2011;7:691–699. doi: 10.1038/nrrheum.2011.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abramson SB, Given WP, Edelson HS, Weissmann G. Neutrophil aggregation induced by sera from patients with active systemic lupus erythematosus. Arthritis Rheum. 1983;26:630–636. doi: 10.1002/art.1780260509. [DOI] [PubMed] [Google Scholar]
- 16.Brandt L, Hedberg H. Impaired phagocytosis by peripheral blood granulocytes in systemic lupus erythematosus. Scand J Haematol. 1969;6:348–353. doi: 10.1111/j.1600-0609.1969.tb02420.x. [DOI] [PubMed] [Google Scholar]
- 17.Courtney PA, Crockard AD, Williamson K, Irvine AE, Kennedy RJ, et al. Increased apoptotic peripheral blood neutrophils in systemic lupus erythematosus: relations with disease activity, antibodies to double stranded DNA, and neutropenia. Ann Rheum Dis. 1999;58:309–314. doi: 10.1136/ard.58.5.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sthoeger ZM, Bezalel S, Chapnik N, Asher I, Froy O. High alpha-defensin levels in patients with systemic lupus erythematosus. Immunology. 2009;127:116–122. doi: 10.1111/j.1365-2567.2008.02997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vordenbäumen S, Fischer-Betz R, Timm D, Sander O, Chehab G, et al. Elevated levels of human beta-defensin 2 and human neutrophil peptides in systemic lupus erythematosus. Lupus. 2010;19:1648–1653. doi: 10.1177/0961203310377089. [DOI] [PubMed] [Google Scholar]
- 20.Ma CY, Jiao YL, Zhang J, Yang QR, Zhang ZF, et al. Elevated plasma level of HMGB1 is associated with disease activity and combined alterations with IFN-α and TNF-α in systemic lupus erythematosus. Rheumatol Int. 2012;32:395–402. doi: 10.1007/s00296-010-1636-6. [DOI] [PubMed] [Google Scholar]
- 21.Pradhan VD, Badakere SS, Bichile LS, Almeida AF. Anti-neutrophil cytoplasmic antibodies (ANCA) in systemic lupus erythematosus: prevalence, clinical associations and correlation with other autoantibodies. J Assoc Physicians India. 2004;52:533–537. [PubMed] [Google Scholar]
- 22.Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007;176:231–241. doi: 10.1083/jcb.200606027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steinberg BE, Grinstein S. Unconventional roles of the NADPH oxidase: signaling, ion homeostasis, and cell death. Sci STKE. 2007;2007:pe11. doi: 10.1126/stke.3792007pe11. [DOI] [PubMed] [Google Scholar]
- 24.Urban CF, Ermert D, Schmid M, Abu-Abed U, Goosmann C, et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 2009;5:e1000639. doi: 10.1371/journal.ppat.1000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beiter K, Wartha F, Albiger B, Normark S, Zychlinsky A, et al. An endonuclease allows Streptococcus pneumoniae to escape from neutrophil extracellular traps. Curr Biol. 2006;16:401–407. doi: 10.1016/j.cub.2006.01.056. [DOI] [PubMed] [Google Scholar]
- 26.Urban CF, Reichard U, Brinkmann V, Zychlinsky A. Neutrophil extracellular traps capture and kill Candida albicans yeast and hyphal forms. Cell Microbiol. 2006;8:668–676. doi: 10.1111/j.1462-5822.2005.00659.x. [DOI] [PubMed] [Google Scholar]
- 27.Brinkmann V, Zychlinsky A. Beneficial suicide: why neutrophils die to make NETs. Nat Rev Microbiol. 2007;5:577–582. doi: 10.1038/nrmicro1710. [DOI] [PubMed] [Google Scholar]
- 28.Guimarães-Costa AB, Nascimento MT, Froment GS, Soares RP, Morgado FN, et al. Leishmania amazonensis promastigotes induce and are killed by neutrophil extracellular traps. Proc Natl Acad Sci U S A. 2009;106:6748–6753. doi: 10.1073/pnas.0900226106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saitoh T, Komano J, Saitoh Y, Misawa T, Takahama M, et al. Neutrophil extracellular traps mediate a host defense response to human immunodeficiency virus-1. Cell Host Microbe. 2012;12:109–116. doi: 10.1016/j.chom.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 30.Gupta AK, Hasler P, Holzgreve W, Gebhardt S, Hahn S. Induction of neutrophil extracellular DNA lattices by placental microparticles and IL-8 and their presence in preeclampsia. Hum Immunol. 2005;66:1146–1154. doi: 10.1016/j.humimm.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 31.Gupta AK, Joshi MB, Philippova M, Erne P, Hasler P, et al. Activated endothelial cells induce neutrophil extracellular traps and are susceptible to NETosis-mediated cell death. FEBS Lett. 2010;584:3193–3197. doi: 10.1016/j.febslet.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Patel S, Kumar S, Jyoti A, Srinag BS, Keshari RS, et al. Nitric oxide donors release extracellular traps from human neutrophils by augmenting free radical generation. Nitric Oxide. 2010;22:226–234. doi: 10.1016/j.niox.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Kessenbrock K, Krumbholz M, Schönermarck U, Back W, Gross WL, et al. Netting neutrophils in autoimmune small-vessel vasculitis. Nat Med. 2009;15:623–625. doi: 10.1038/nm.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lande R, Ganguly D, Facchinetti V, Frasca L, Conrad C, et al. Neutrophils activate plasmacytoid dendritic cells by releasing self-DNA-peptide complexes in systemic lupus erythematosus. Sci Transl Med. 2011;3:73ra19. doi: 10.1126/scitranslmed.3001180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garcia-Romo GS, Caielli S, Vega B, Connolly J, Allantaz F, et al. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci Transl Med. 2011;3:73ra20. doi: 10.1126/scitranslmed.3001201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Papayannopoulos V, Metzler KD, Hakkim A, Zychlinsky A. Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J Cell Biol. 2010;191:677–691. doi: 10.1083/jcb.201006052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y, Li M, Stadler S, Correll S, Li P, et al. Histone hypercitrullination mediates chromatin decondensation and neutrophil extracellular trap formation. J Cell Biol. 2009;184:205–213. doi: 10.1083/jcb.200806072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li P, Li M, Lindberg MR, Kennett MJ, Xiong N, et al. PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J Exp Med. 2010;207:1853–1862. doi: 10.1084/jem.20100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Neeli I, Dwivedi N, Khan S, Radic M. Regulation of extracellular chromatin release from neutrophils. J Innate Immun. 2009;1:194–201. doi: 10.1159/000206974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mitroulis I, Kambas K, Chrysanthopoulou A, Skendros P, Apostolidou E, et al. Neutrophil extracellular trap formation is associated with IL-1β and autophagy-related signaling in gout. PLoS One. 2011;6:e29318. doi: 10.1371/journal.pone.0029318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Remijsen Q, Vanden Berghe T, Wirawan E, Asselbergh B, Parthoens E, et al. Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res. 2011;21:290–304. doi: 10.1038/cr.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fuchs TA, Brill A, Duerschmied D, Schatzberg D, Monestier M, et al. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci U S A. 2010;107:15880–15885. doi: 10.1073/pnas.1005743107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Massberg S, Grahl L, von Bruehl ML, Manukyan D, Pfeiler S, et al. Reciprocal coupling of coagulation and innate immunity via neutrophil serine proteases. Nat Med. 2010;16:887–896. doi: 10.1038/nm.2184. [DOI] [PubMed] [Google Scholar]
- 44.von Brühl ML, Stark K, Steinhart A, Chandraratne S, Konrad I, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209:819–835. doi: 10.1084/jem.20112322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brill A, Fuchs TA, Savchenko AS, Thomas GM, Martinod K, et al. Neutrophil extracellular traps promote deep vein thrombosis in mice. J Thromb Haemost. 2012;10:136–144. doi: 10.1111/j.1538-7836.2011.04544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fuchs TA, Kremer Hovinga JA, Schatzberg D, Wagner DD, Lämmle B. Circulating DNA and myeloperoxidase indicate disease activity in patients with thrombotic microangiopathies. Blood. 2012;120:1157–1164. doi: 10.1182/blood-2012-02-412197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Manzenreiter R, Kienberger F, Marcos V, Schilcher K, Krautgartner WD, et al. Ultrastructural characterization of cystic fibrosis sputum using atomic force and scanning electron microscopy. J Cyst Fibros. 2012;11:84–92. doi: 10.1016/j.jcf.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 48.Caudrillier A, Kessenbrock K, Gilliss BM, Nguyen JX, Marques MB, et al. Platelets induce neutrophil extracellular traps in transfusion-related acute lung injury. J Clin Invest. 2012;122:2661–2671. doi: 10.1172/JCI61303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thomas GM, Carbo C, Curtis BR, Martinod K, Mazo IB, et al. Extracellular DNA traps are associated with the pathogenesis of TRALI in humans and mice. Blood. 2012;119:6335–6343. doi: 10.1182/blood-2012-01-405183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saffarzadeh M, Juenemann C, Queisser MA, Lochnit G, Barreto G, et al. Neutrophil extracellular traps directly induce epithelial and endothelial cell death: a predominant role of histones. PLoS One. 2012;7:e32366. doi: 10.1371/journal.pone.0032366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu J, Zhang X, Pelayo R, Monestier M, Ammollo CT, et al. Extracellular histones are major mediators of death in sepsis. Nat Med. 2009;15:1318–1321. doi: 10.1038/nm.2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Christen U, von Herrath MG. Infections and autoimmunity--good or bad? J Immunol. 2005;174:7481–7486. doi: 10.4049/jimmunol.174.12.7481. [DOI] [PubMed] [Google Scholar]
- 53.Falk RJ, Terrell RS, Charles LA, Jennette JC. Anti-neutrophil cytoplasmic autoantibodies induce neutrophils to degranulate and produce oxygen radicals in vitro. Proc Natl Acad Sci U S A. 1990;87:4115–4119. doi: 10.1073/pnas.87.11.4115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiao H, Heeringa P, Hu P, Liu Z, Zhao M, et al. Antineutrophil cytoplasmic autoantibodies specificfor myeloperoxidase cause glomerulonephritis and vasculitis in mice. J Clin Invest. 2002;110:955–963. doi: 10.1172/JCI15918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Primo VC, Marusic S, Franklin CC, Goldmann WH, Achaval CG, et al. Anti-PR3 immune responses induce segmental and necrotizing glomerulonephritis. Clin Exp Immunol. 2010;159:327–337. doi: 10.1111/j.1365-2249.2009.04072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fauzi AR, Kong NC, Chua MK, Jeyabalan V, Idris MN, et al. Antibodies in systemic lupus antineutrophil cytoplasmic erythematosus: prevalence, disease activity correlations and organ system associations. Med J Malaysia. 2004;59:372–377. [PubMed] [Google Scholar]
- 57.Hakkim A, Fürnrohr BG, Amann K, Laube B, Abed UA, et al. Impairment of neutrophil extracellular trap degradation is associated with lupus nephritis. Proc Natl Acad Sci U S A. 2010;107:9813–9818. doi: 10.1073/pnas.0909927107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yeh TM, Chang HC, Liang CC, Wu JJ, Liu MF. Deoxyribonuclease-inhibitory antibodies in systemic lupus erythematosus. J Biomed Sci. 2003;10:544–551. doi: 10.1159/000072382. [DOI] [PubMed] [Google Scholar]
- 59.Emlen W, Ansari R, Burdick G. DNA-anti-DNA immune complexes. Antibody protection of a discrete DNA fragment from DNase digestion in vitro. J Clin Invest. 1984;74:185–190. doi: 10.1172/JCI111400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yasutomo K, Horiuchi T, Kagami S, Tsukamoto H, Hashimura C, et al. Mutation of DNASE1 in people with systemic lupus erythematosus. Nat Genet. 2001;28:313–314. doi: 10.1038/91070. [DOI] [PubMed] [Google Scholar]
- 61.Shin HD, Park BL, Kim LH, Lee HS, Kim TY, et al. Common DNase I polymorphism associated with autoantibody production among systemic lupus erythematosus patients. Hum Mol Genet. 2004;13:2343–2350. doi: 10.1093/hmg/ddh275. [DOI] [PubMed] [Google Scholar]
- 62.Leffler J, Martin M, Gullstrand B, Tyden H, Lood C, et al. Neutrophil extracellular traps that are not degraded in systemic lupus erythematosus activate complement exacerbating the disease. J Immunol. 2012;188:3522–3531. doi: 10.4049/jimmunol.1102404. [DOI] [PubMed] [Google Scholar]
- 63.Mongini PK, Vilensky MA, Highet PF, Inman JK. The affinity threshold for human B cell activation via the antigen receptor complex is reduced upon co-ligation of the antigen receptor with CD21 (CR2) J Immunol. 1997;159:3782–3791. [PubMed] [Google Scholar]
- 64.Hooks JJ, Moutsopoulos HM, Geis SA, Stahl NI, Decker JL, et al. Immune interferon in the circulation of patients with autoimmune disease. N Engl J Med. 1979;301:5–8. doi: 10.1056/NEJM197907053010102. [DOI] [PubMed] [Google Scholar]
- 65.Ytterberg SR, Schnitzer TJ. Serum interferon levels in patients with systemic lupus erythematosus. Arthritis Rheum. 1982;25:401–406. doi: 10.1002/art.1780250407. [DOI] [PubMed] [Google Scholar]
- 66.Baechler EC, Batliwalla FM, Karypis G, Gaffney PM, Ortmann WA, et al. Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc Natl Acad Sci U S A. 2003;100:2610–2615. doi: 10.1073/pnas.0337679100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bennett L, Palucka AK, Arce E, Cantrell V, Borvak J, et al. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J Exp Med. 2003;197:711–723. doi: 10.1084/jem.20021553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barrat FJ, Meeker T, Gregorio J, Chan JH, Uematsu S, et al. Nucleic acids of mammalian origin can act as endogenous ligands for Toll-like receptors and may promote systemic lupus erythematosus. J Exp Med. 2005;202:1131–1139. doi: 10.1084/jem.20050914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Means TK, Latz E, Hayashi F, Murali MR, Golenbock DT, et al. Human lupus autoantibody-DNA complexes activate DCs through cooperation of CD32 and TLR9. J Clin Invest. 2005;115:407–417. doi: 10.1172/JCI23025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vollmer J, Tluk S, Schmitz C, Hamm S, Jurk M, et al. Immune stimulation mediated by autoantigen binding sites within small nuclear RNAs involves Toll-like receptors 7 and 8. J Exp Med. 2005;202:1575–1585. doi: 10.1084/jem.20051696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hacbarth E, Kajdacsy-Balla A. Low density neutrophils in patients with systemic lupus erythematosus, rheumatoid arthritis, and acute rheumatic fever. Arthritis Rheum. 1986;29:1334–1342. doi: 10.1002/art.1780291105. [DOI] [PubMed] [Google Scholar]
- 72.Villanueva E, Yalavarthi S, Berthier CC, Hodgin JB, Khandpur R, et al. Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J Immunol. 2011;187:538–552. doi: 10.4049/jimmunol.1100450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lamkanfi M, Dixit VM. Inflammasomes and their roles in health and disease. Annu Rev Cell Dev Biol. 2012;28:137–161. doi: 10.1146/annurev-cellbio-101011-155745. [DOI] [PubMed] [Google Scholar]
- 74.Kinoshita K, Yamagata T, Nozaki Y, Sugiyama M, Ikoma S, et al. Blockade of IL-18 receptor signaling delays the onset of autoimmune disease in MRL-Faslpr mice. J Immunol. 2004;173:5312–5318. doi: 10.4049/jimmunol.173.8.5312. [DOI] [PubMed] [Google Scholar]
- 75.Hu D, Liu X, Chen S, Bao C. Expressions of IL-18 and its binding protein in peripheral blood leukocytes and kidney tissues of lupus nephritis patients. Clin Rheumatol. 2010;29:717–721. doi: 10.1007/s10067-010-1386-6. [DOI] [PubMed] [Google Scholar]
- 76.Wang D, Drenker M, Eiz-Vesper B, Werfel T, Wittmann M. Evidence for a pathogenetic role of interleukin-18 in cutaneous lupus erythematosus. Arthritis Rheum. 2008;58:3205–3215. doi: 10.1002/art.23868. [DOI] [PubMed] [Google Scholar]
- 77.Kahlenberg JM, Carmona-Rivera C, Smith CK, Kaplan MJ. Neutrophil extracellular trap-associated protein activation of the NLRP3 inflammasome is enhanced in lupus macrophages. J Immunol. 2013;190:1217–1226. doi: 10.4049/jimmunol.1202388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kahlenberg JM, Thacker SG, Berthier CC, Cohen CD, Kretzler M, et al. Inflammasome activation of IL-18 results in endothelial progenitor cell dysfunction in systemic lupus erythematosus. J Immunol. 2011;187:6143–6156. doi: 10.4049/jimmunol.1101284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Calvani N, Richards HB, Tucci M, Pannarale G, Silvestris F. Up-regulation of IL-18 and predominance of a Th1 immune response is a hallmark of lupus nephritis. Clin Exp Immunol. 2004;138:171–178. doi: 10.1111/j.1365-2249.2004.02588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Guiducci C, Tripodo C, Gong M, Sangaletti S, Colombo MP, et al. Autoimmune skin inflammation is dependent on plasmacytoid dendritic cell activation by nucleic acids via TLR7 and TLR9. J Exp Med. 2010;207:2931–2942. doi: 10.1084/jem.20101048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Knight JS, O’Dell AA, Zhao W, Khandpur R, Yalavarthi S, et al. Lupus-Prone Mice Demonstrate Enhanced Neutrophil Extracellular Trap Formation: Implications for Autoantibody Formation and Organ Damage. Arthritis Rheum. 2012;64:S619. [Google Scholar]
- 82.Campbell AM, Kashgarian M, Shlomchik MJ. NADPH oxidase inhibits the pathogenesis of systemic lupus erythematosus. Sci Transl Med. 2012;4:157ra141. doi: 10.1126/scitranslmed.3004801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brinkmann V, Zychlinsky A. Neutrophil extracellular traps: is immunity the second function of chromatin? J Cell Biol. 2012;198:773–783. doi: 10.1083/jcb.201203170. [DOI] [PMC free article] [PubMed] [Google Scholar]