Abstract
Low-income women may be especially vulnerable to job loss after a breast cancer diagnosis. The identification of early risk factors for not returning to work in the long term could inform interventions to help survivors avoid this outcome. A consecutive sample of low-income, employed, underinsured/uninsured women treated for stage 0–III breast cancer was surveyed 6, 18, 36, and 60 months after diagnosis. Participants were classified according to the survey in which they first reported return to work. If they were not working in every survey they were classified as not returning to work. Correlates of not returning to work were identified. Of 274 participants, 36 % returned to work by 6 months, an additional 21 % by 18, 10 % by 36, and 5 % by 60 months. 27 % never returned to work. Of those not working at 6 months, 43 % never returned. Independent predictors of never returning to work included lowest annual income (<$10,000), Latina ethnicity, high comorbidity burden, and receipt of chemotherapy. Very poor women who stop working during chemotherapy for breast cancer are at risk of not returning to work months and years following treatment. These findings may have clinical and policy implications. Conversely, radiation therapy, axillary node dissection, age, and job type do not appear to be associated with return to work. Clinicians should discuss work-related concerns with patients and facilitate early return to work when desired by the patient. Additional research is needed to develop interventions to optimize return to work.
Keywords: Breast cancer, Income, Work, Survivorship
Introduction
Return to work among cancer survivors is associated with financial security, self-esteem, and quality of life [1–4]. Studies of employment outcomes in predominantly middle-and high-income breast cancer survivors have demonstrated a rate of return to work of 70–80 % during the first year after diagnosis [5, 6]. However, low-income women appear to be more vulnerable to job loss and delayed return to work after a diagnosis of breast cancer than their higher income counterparts, with only 50 % of low-income survivors working 18 months after diagnosis and <60 % at 36 months [1, 5, 7]. This loss of work can have important adverse financial consequences. Those who lose their jobs are more likely to report having difficulty paying bills, purchasing necessities such as food and clothing, and paying for their families’ healthcare [4].
In the short term, during and shortly after treatment, receipt of chemotherapy has been associated with an increased risk of missed work and job loss [4, 8]. Conversely, most studies have shown no significant relationship between chemotherapy and return to work in the long term, at 12–18 months [5], 3 years [9], and 5–15 years after diagnosis [10]. Together, this body of literature indicates that receipt of chemotherapy may delay return to work but does not impact long-term employment outcomes. However, this longitudinal trend has not been studied prospectively or in low-income women, who may have limited sick leave, workplace accommodation, and schedule flexibility, all of which have been associated with increased return to work in middle- and high-income samples [4, 5, 8]. Low-income women are more likely to be unskilled workers and, therefore, more easily replaced. In such cases, women who intend or need to stop working temporarily during chemotherapy may be unable to return to work after treatment completion or in the long term if jobs are unavailable. Low-income women also may be less able to afford treatments for long-term complications such as neuropathy and depression.
The prospective identification of early risk factors for not returning to work in the long term could inform interventions to help patients avoid this outcome. To this end, we undertook a prospective 5-year longitudinal study of low-income, medically underserved women with a new diagnosis of breast cancer. Our goal was to identify early correlates of not returning to work for 5 years after diagnosis. Our hypothesis was that receipt of chemotherapy would be associated with increased risk of not working in the months and years after completion of therapy.
Methods
Eligibility criteria
Eligible participants were English- and/or Spanish-speaking women who were 6 months from diagnosis of localized breast cancer treated with curative intent (stage 0–III), cognitively able to participate, not undergoing treatment for another cancer, and enrolled in California’s Breast and Cervical Cancer Treatment Program (BCCTP). The program, which is administered by Medicaid, provides benefits to patients who are uninsured/underinsured, California residents, and have a family income ≤200 % of the Federal Poverty Level. Undocumented immigrants are eligible. This study was approved by the University of California, Los Angeles Human Subjects Protection Committee. Informed consent was obtained from participants before enrollment.
Recruitment and participants
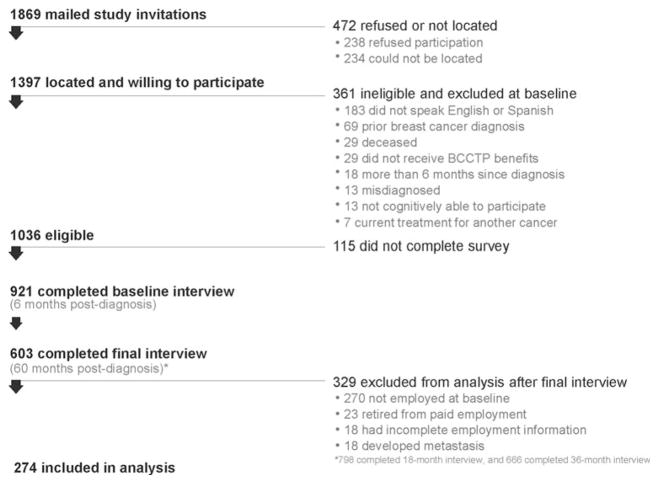
This study is part of a larger, longitudinal study described previously [11]. Of 1,869 women invited to participate, 921 completed a survey 6 months after diagnosis (Fig. 1). Since we were interested in breast cancer-related predictors of not returning to work, these analyses include only women who were employed at the time of diagnosis and who did not retire from paid employment or receive a diagnosis of metastatic breast cancer during the study period. Of 603 women who remained in the study at 60 months, 333 (55 %) were employed before diagnosis. Of these, 18 were excluded because they developed metastatic breast cancer, 23 because they retired from paid employment, and 18 because self-reported work status was missing in one or more survey. Respondents excluded due to incomplete reporting of work status were demographically similar to the study sample.
Fig. 1.
Recruitment flow
Interviews
1-h Telephone surveys were administered in English or Spanish 6, 18, 36, and 60 months post-diagnosis between March 2003 and June 2010. The study instruments were pilot tested and translated using the standard methods [12].
Variables
The primary outcome in this study was time of the first reported return to work post-diagnosis. No distinction was made between part-time and full-time employment. Participants who reported working at one or more time points were classified into 4 groups according to the survey in which they first reported that they were working (6, 18, 36, or 60 months). Those who said they were not working in every survey were classified as not returning to work. We did not analyze the characteristics of participants who stopped working after returning to work (n = 55) separately because the second survey occurred well after the time that adjuvant therapy should have been completed. In light of prior research demonstrating that health-related quality of life in long-term survivors of breast cancer is relatively stable over time [13], we can conclude that stopping work after having returned to work is more likely to be related to non-breast cancer factors, such as changes in the economy or significant family events (e.g., illness of a spouse).
All independent variables were baseline characteristics and refer to the time of the first survey (6 months post-diagnosis) except job type, which refers to the time just before diagnosis. Baseline financial status was evaluated along two measures: annual household income (<$10,000, $10,000–$20,000, or >$20,000) and perceived adequacy of financial resources to cover participant needs (adequate/inadequate). Education was classified as no high school diploma, completed high school and/or some college, and completed college and/or a post-graduate degree. Family structure was evaluated along three measures: married/partnered versus not married/partnered, children ≤17 years old living at home (0/1/2+), and seniors ≥65 years old living at home (0/1+). Social support was assessed by asking the participant if she had anyone to provide emotional support, help with daily tasks, and/or accompany her to medical appointments [14].
Participants self-identified their race/ethnicity and place of birth. Acculturation was evaluated among participants who had spoken a language other than English as children using an index based on language use and preference [15].
Job type was classified according to the U.S. Census Bureau Index of Occupations [16] and collapsed into four categories (operator/fabricator, professional/manager, service, and technical/sales/administrative) based on previously used methods [1, 5, 6, 17–19]. Examples of operators/fabricators include farm and factory workers; professionals/managers include teachers and financial workers; service jobs include housekeepers, food servers, and nannies; technical/sales/administrative jobs include clerks, administrative assistants, and skilled technical workers. Weekly hours worked before diagnosis was dichotomized as full time versus part time (≥35 vs.<35 h).
Comorbid medical conditions, evaluated using the Charlson Comorbidity Index modified for patient report, were classified as any or none [20, 21]. Clinical cancer and treatment variables were abstracted from the medical record.
Analyses
In univariate analyses, survey and clinical variables were compared by time of the first employment or no return to work using ANOVA for continuous variables and Chi-squared (or Fisher’s exact) tests for categorical variables. A multinomial logistic regression was then conducted to identify independent predictors of not returning to work using this outcome as the reference category and including variables that were statistically significant in the univariate analyses (two-sided p < 0.05). Where two variables were highly correlated (p < 0.0001) the more clinically meaningful variable was included in the model (e.g., chemotherapy was included but cancer stage was not). To separate the effects of chemotherapy and axillary lymph node dissection (ALND) and determine which to include in the model, we created an interaction term and tested its association with return to work. In another set of analyses we fit the same multivariable model after dichotomizing the primary outcome (no return to work vs. return at any time during the study period).
Results
Participant characteristics
Table 1 lists the baseline characteristics of the study sample (n = 274). More than half of the study participants reported an annual household income ≤$20,000; 98 % reported annual household income ≤$40,000 (data not shown). Just over half (53 %) described themselves as Latina. Overall educational attainment was low; 36 % had not completed high school. Service jobs were the most commonly reported occupational category (47 %). The majority of participants (73 %) reported no comorbid medical conditions. Most received chemotherapy (70 %), radiation (73 %), and endocrine therapy (69 %). In terms of surgery, 39 % underwent mastectomy, and 65 % underwent ALND.
Table 1.
Participant characteristics
| No. (%), n = 274 | |
|---|---|
| Demographics | |
| Age | |
| Median | 49 |
| Range | 26–85 |
| Birthplacea | |
| United States | 118 (43) |
| Outside of the United States | 155 (57) |
| Annual household incomea | |
| <$10,000 | 80 (30) |
| $10,000–$20,000 | 86 (32) |
| >$20,000 | 103 (38) |
| Financial resources adequate to meet needsa | |
| Adequate | 99 (37) |
| Inadequate | 171 (63) |
| Race/ethnicity | |
| Latina | 145 (53) |
| Non-Latina White | 90 (33) |
| Other | 39 (14) |
| Marital status | |
| Married/partnered | 125 (46) |
| Not married/partnered | 149 (54) |
| Children ≤17 years old at homea | |
| None | 111 (48) |
| One | 48 (21) |
| Two or more | 71 (31) |
| Seniors ≥65 years old at homea | |
| None | 194 (83) |
| One or more | 39 (17) |
| Educationa | |
| Did not complete high school | 99 (36) |
| High school ± some college | 124 (45) |
| College ± post-graduate | 50 (18) |
| Acculturation | |
| More acculturated | 20 (12) |
| Less acculturated | 148 (88) |
| Social support | |
| Support—emotionala | |
| No support | 29 (11) |
| Some support | 244 (89) |
| Support—help with daily tasksa | |
| No support | 47 (17) |
| Some support | 226 (83) |
| Support—accompanied participant to doctor’s visitsa | |
| No support | 40 (15) |
| Some support | 233 (85) |
| Work related (before diagnosis) | |
| Job type before diagnosis | |
| Operator/fabricator | 44 (16) |
| Professional/manager | 49 (18) |
| Service | 130 (47) |
| Technical/sales/administrative | 51 (19) |
| Full- vs. part-time employment before diagnosisa | |
| Full time | 189 (69) |
| Part time | 83 (31) |
| Clinical variables | |
| Comorbid conditions | |
| None | 199 (73) |
| One or more | 75 (27) |
| Cancer stage | |
| DCIS | 25 (10) |
| I | 76 (31) |
| II | 106 (44) |
| III | 35 (14) |
| Type of breast surgerya | |
| Mastectomy | 101 (39) |
| Breast-conserving surgery | 156 (61) |
| Breast reconstruction (if mastectomy) | |
| Received | 16 (16) |
| Not received | 85 (84) |
| Axillary node dissectiona | |
| Received | 168 (65) |
| Not received | 90 (35) |
| Chemotherapya | |
| Received | 180 (70) |
| Not received | 77 (30) |
| Endocrine therapya | |
| Received | 171 (69) |
| Not received | 78 (31) |
| Radiation therapya | |
| Received | 185 (73) |
| Not received | 70 (27) |
DCIS ductal carcinoma in situ
Data missing for ≥1 participant. Percentages calculated over complete data
Time of the first reported return to work
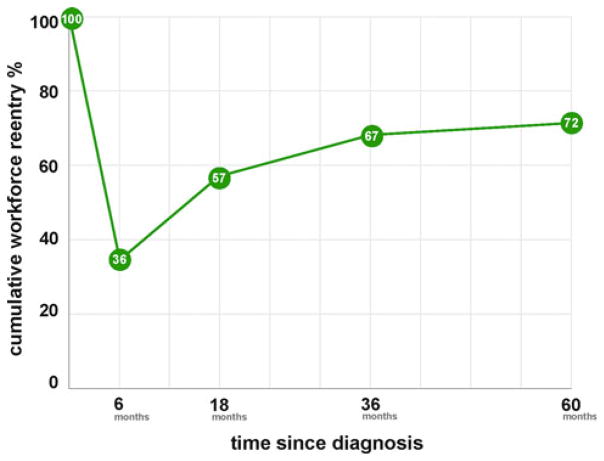
During the 5 years after a diagnosis of breast cancer, 27 % of participants reported that they had not returned to work in every survey. Just over a third of participants (36 %) reported that they were working at the time of the 6-month survey, with fewer participants reporting that they had returned to work by each subsequent survey (21, 10, and 5 % by 18, 36, and 60 months, respectively). Of 174 participants who were not working in the 6-month survey, 43 % reported not returning to work throughout the study period. Cumulative workforce reentry is shown in Fig. 2.
Fig. 2.
Cumulative workforce reentry
Predictors of not returning to work
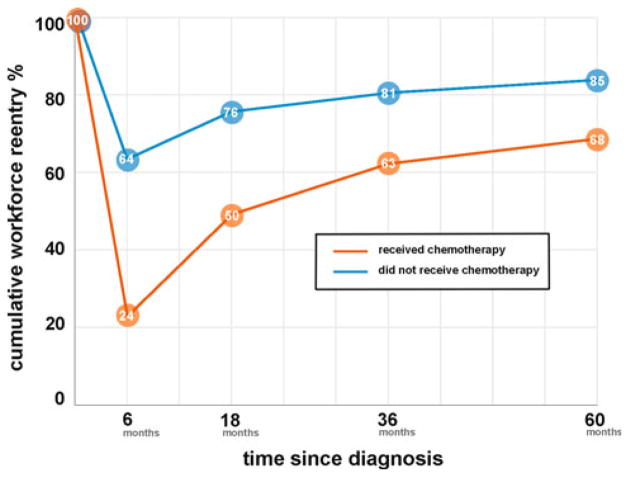
Results of univariate analyses are reported in Table 2. Since only 5 % of participants first reported return to work at 60 months and the two groups had similar baseline characteristics, participants who reported first return to work at 36 and 60 months were combined into one group to increase the power of the analyses. Variables significantly associated with return to work included age, annual household income, adequacy of financial resources, race/ethnicity, education, comorbidity burden, cancer stage, ALND, and chemotherapy. Among participants who never reported return to work, the percentage who received chemotherapy was almost twice as high as the percentage who did not receive chemotherapy. Moreover, participants who reported that they were still actively undergoing chemotherapy at the time of their 6-month survey were much more likely to report that they were not working at 6 months (81 % of those receiving chemotherapy vs. 55 % of those not in treatment, p < 0.0001, data not shown). There was no corresponding employment difference among patients still undergoing radiation therapy at the time of the 6-month survey, and overall receipt of radiation therapy was not associated with return to work. The relationship between receipt of chemotherapy and cumulative work-force reentry is shown in Fig. 3.
Table 2.
Univariate analysis of time of the first reported return to work
| Working at 6 months, No. (%), n = 100 | Working at 18 months, No. (%), n = 58 | Working at 36–60 months, No. (%), n = 41 | No reported return to work, No. (%), n = 75 | p value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | <0.05 | ||||
| Median | 49 | 48 | 45 | 50 | |
| Range | 34–85 | 26–63 | 34–65 | 31–65 | |
| Birthplacea | |||||
| United States | 49 (42) | 28 (24) | 12 (10) | 29 (25) | |
| Outside of the United States | 50 (32) | 30 (19) | 29 (19) | 46 (30) | 0.11 |
| Annual household incomea | |||||
| <$10,000 | 15 (19) | 19 (24) | 13 (16) | 33 (41) | |
| $10,000–$20,000 | 37 (43) | 20 (23) | 13 (15) | 16 (19) | |
| >$20,000 | 45 (44) | 19 (18) | 15 (15) | 24 (23) | <0.005 |
| Financial resources adequate to meet needsa | |||||
| Adequate | 52 (53) | 21 (21) | 11 (11) | 15 (15) | |
| Inadequate | 47 (27) | 36 (21) | 29 (17) | 59 (35) | <0.0005 |
| Race/ethnicity | |||||
| Latina | 39 (27) | 34 (23) | 26 (18) | 46 (32) | |
| Non-Latina White | 46 (51) | 19 (21) | 9 (10) | 16 (18) | |
| Other | 15 (38) | 5 (13) | 6 (15) | 13 (33) | <0.01 |
| Marital status | |||||
| Married/partnered | 44 (35) | 30 (24) | 20 (16) | 31 (25) | |
| Not married/partnered | 56 (38) | 28 (19) | 21 (14) | 44 (30) | 0.64 |
| Children ≤17 years old at homea | |||||
| None | 42 (38) | 24 (22) | 13 (12) | 32 (29) | |
| One | 16 (33) | 14 (29) | 10 (21) | 8 (17) | |
| Two or more | 17 (24) | 17 (24) | 12 (17) | 25 (35) | 0.18 |
| Seniors ≥65 years old at homea | |||||
| None | 64 (33) | 43 (22) | 33 (17) | 54 (28) | |
| One or more | 15 (38) | 11 (28) | 2 (5) | 11 (28) | 0.28 |
| Educationa | |||||
| Did not complete high school | 23 (23) | 19 (19) | 21 (21) | 36 (36) | |
| High school ± some college | 55 (44) | 28 (23) | 11 (9) | 30 (24) | |
| College ± post-graduate | 21 (42) | 11 (22) | 9 (18) | 9 (18) | <0.005 |
| Acculturation | |||||
| More acculturated | 9 (45) | 4 (20) | 2 (10) | 5 (25) | |
| Less acculturated | 44 (30) | 32 (22) | 28 (19) | 44 (30) | 0.52 |
| Social support | |||||
| Support—emotionala | |||||
| No support | 7 (24) | 6 (21) | 6 (21) | 10 (34) | |
| Any support | 93 (38) | 52 (21) | 35 (14) | 64 (26) | 0.43 |
| Support—help with daily tasksa | |||||
| No support | 19 (40) | 12 (26) | 3 (6) | 13 (27) | |
| Any support | 81 (36) | 46 (20) | 38 (17) | 61 (27) | 0.32 |
| Support—accompanied participant to doctor’s visitsa | |||||
| No support | 13 (33) | 7 (18) | 11 (28) | 9 (23) | |
| Any support | 87 (37) | 51 (22) | 30 (13) | 65 (28) | 0.12 |
| Work related | |||||
| Job type before diagnosis | |||||
| Operator/fabricator | 9 (20) | 8 (18) | 9 (20) | 18 (41) | |
| Professional/manager | 23 (47) | 8 (16) | 7 (14) | 11 (22) | |
| Service | 45 (35) | 30 (23) | 21 (16) | 34 (26) | |
| Technical/sales/administrative | 23 (45) | 12 (24) | 4 (8) | 12 (24) | 0.15 |
| Full- vs. part-time employment before diagnosisa | |||||
| Full time | 69 (37) | 41 (22) | 28 (15) | 51 (27) | |
| Part time | 29 (35) | 17 (20) | 13 (16) | 24 (29) | 0.98 |
| Clinical variables | |||||
| Comorbid conditions | |||||
| None | 73 (37) | 46 (23) | 34 (17) | 45 (23) | |
| One or more | 27 (36) | 12 (16) | 6 (8) | 30 (40) | <0.01 |
| Cancer stage | |||||
| DCIS | 16 (64) | 2 (8) | 2 (8) | 5 (20) | |
| I | 36 (47) | 15 (20) | 9 (12) | 16 (21) | |
| II | 30 (28) | 30 (28) | 21 (20) | 25 (24) | |
| III | 5 (14) | 6 (17) | 6 (17) | 18 (51) | <0.0005 |
| Type of breast surgerya | |||||
| Mastectomy | 27 (27) | 25 (25) | 20 (20) | 29 (29) | |
| Breast-conserving surgery | 65 (42) | 31 (20) | 20 (13) | 40 (26) | 0.08 |
| Breast reconstruction (if mastectomy) | |||||
| Received | 6 (38) | 4 (25) | 4 (25) | 2 (13) | |
| Not received | 21 (25) | 21 (25) | 16 (19) | 27 (32) | 0.42 |
| Axillary node dissectiona | |||||
| Received | 48 (29) | 38 (23) | 35 (21) | 47 (28) | |
| Not received | 45 (50) | 18 (20) | 5 (6) | 22 (24) | <0.001 |
| Chemotherapya | <0.0001 | ||||
| Received | 44 (24) | 47 (26) | 33 (18) | 56 (31) | |
| Not received | 49 (64) | 9 (12) | 7 (9) | 12 (16) | |
| Endocrine therapya | |||||
| Received | 62 (36) | 39 (23) | 22 (13) | 48 (28) | |
| Not received | 31 (40) | 16 (21) | 13 (17) | 18 (23) | 0.72 |
| Radiation therapya | |||||
| Received | 65 (35) | 40 (22) | 29 (16) | 51 (28) | |
| Not received | 28 (40) | 16 (23) | 10 (14) | 16 (23) | 0.84 |
DCIS ductal carcinoma in situ
Data missing for ≥1 participant. Percentages calculated over complete data for this variable
Fig. 3.
Chemotherapy and cumulative workforce reentry
Participants who had chemotherapy were at higher risk of not returning to work, regardless of whether or not they underwent ALND (data not shown). Those who had ALND but no chemotherapy had similar return to work than those who received neither treatment. Therefore, chemotherapy rather than ALND was included in the multinomial logistic regression model (Table 3). Controlling for all other variables in the model, women who received chemotherapy had more than six times the odds as non-recipients of not returning to work throughout the study period than of working at 6 months. A similar relationship was seen for income. In this uniformly low-income sample, those earning less than $10,000 annually had more than five times the odds as those earning at least $20,000 of never reporting return to work than of working at 6 months. Latinas had more than three times the odds as non-Latina whites of never reporting return to work than of working at 6 months. For the comparison between not returning to work and working by 6 months, no significant relationship was identified according to comorbidity burden. However, those with at least one comorbid condition had four times the odds as those without any comorbid conditions of never returning to work than of working by 36–60 months. Education and age were not significantly associated with never returning to work.
Table 3.
Multinomial logistic regression of time of the first reported working versus no reported return to work (n = 251)
| Odds ratio for 6 months versus no reported return to work (95 % CI) | Odds ratio for 18 months versus no reported return to work (95 % CI) | Odds ratio for 36–60 months versus no reported return to work (95 % CI) | ||||
|---|---|---|---|---|---|---|
| Age** | 0.98 | (0.93–1.03) | 0.96 | (0.91–1.01) | 0.95 | (0.90–1.01) |
| Annual household income | ||||||
| <$10,000† | 0.19 | (0.07–0.47) | 0.80 | (0.33–1.98) | 0.61 | (0.23–1.65) |
| $10,000–$20,000 | 1.12 | (0.45–2.74) | 1.84 | (0.70–4.85) | 1.48 | (0.52–4.25) |
| >$20,000* | 1 | 1 | 1 | |||
| Race/ethnicity | ||||||
| Latina† | 0.31 | (0.12–0.81) | 0.73 | (0.27–1.97) | 0.80 | (0.24–2.61) |
| Other | 0.41 | (0.13–1.30) | 0.36 | (0.10–1.33) | 0.98 | (0.25–3.91) |
| Non-Latina white* | 1 | 1 | 1 | |||
| Education | ||||||
| Did not complete high school | 0.64 | (0.18–2.25) | 0.43 | (0.12–1.56) | 0.64 | (0.16–2.48) |
| High school ± some college | 0.93 | (0.31–2.80) | 0.70 | (0.22–2.21) | 0.36 | (0.10–1.30) |
| College ± post-graduate* | 1 | 1 | 1 | |||
| Comorbid conditions | ||||||
| One or more† | 0.60 | (0.27–1.32) | 0.46 | (0.20–1.07) | 0.25 | (0.08–0.73) |
| None* | 1 | 1 | 1 | |||
| Chemotherapy | ||||||
| Received† | 0.15 | (0.07–0.36) | 0.87 | (0.32–2.37) | 0.69 | (0.23–2.08) |
| Not received* | 1 | 1 | 1 | |||
Statistically significant relationship based on confidence intervals, as shown, for at least one comparison between time of the first reported return to work and no reported return to work
Reference category (odds ratio = 1.00)
Odds ratio corresponds to a 1-year increase in age
Similar results were seen after dichotomizing the primary outcome (not returning to work vs. return at any time during the study). Income, the presence of at least one comorbid condition, and receipt of chemotherapy all were significantly associated with not returning to work; age and education were not associated with not returning to work. In contrast with the multinomial model, in this model race/ethnicity was not associated with not returning to work.
Discussion
In this study we found that more than a quarter of low-income, medically underserved breast cancer survivors who had been employed before their diagnosis did not return to work during the subsequent 5 years. Most women who returned to work did so early; 36 % of the study participants were working at 6 months and another 21 % had returned to work by 18 months. Among those not working 6 months after diagnosis, however, almost half never returned to work. As we had hypothesized, receipt of chemotherapy was an independent predictor of never returning to work. Since most participants who were undergoing chemotherapy at 6 months also reported that they were not working at that time, our findings indicate that the relationship between chemotherapy and not returning to work in the long term is related to the time taken off for treatment. Encouraging and facilitating early return to work or continued employment, if treatment side effects are controlled and working is feasible, could abrogate the adverse impact of chemotherapy on long-term work outcomes.
Our finding of an association between receipt of chemotherapy and not returning to work in the long term is in contrast to prior research not focused on low-income, medically underserved women. Although higher rates of job loss in the short term have been found among women treated with chemotherapy [4, 8], most studies of long-term employment outcomes have shown no relationship between chemotherapy and return to work [5, 9, 10]. Low-income women, such as those in our study, may be less likely to return to work after chemotherapy due to lack of workplace accommodation, including sick leave and schedule flexibility, all of which have been associated with increased return to work in higher income samples [4, 5, 8]. According to the Bureau of Labor Statistics, paid sick leave is available to only 21 % of workers in the lowest 10 % of wage earners nationwide compared to 87 % of those in the highest 10 % [22]. Women who lack these benefits and stop working have no guarantee that their positions will be available once they are ready to return. Our findings indicate that receipt of chemotherapy may have a more pronounced and long-term effect in such populations, such that women who stop working during treatment are at risk of never resuming work.
The increased vulnerability of low-income women to not working in the long term also is supported by the finding that, within this uniformly low-income cohort of breast cancer survivors, those in the lowest income category had the highest risk of never returning to work. Extreme poverty may be a proxy for workplace characteristics, such as working in the informal sector (working for cash in jobs such as babysitting or housekeeping). Unless an employee is a member of a union, informal employment typically has no associated sick leave or disability benefits, and an employee may quickly be replaced if she takes any time off from work.
To our knowledge, this is the first prospective, longitudinal study to report 5 years of work outcomes in low-income women treated for breast cancer. Additional strengths of this study include its high response and retention rates, which are similar to those reported in prior studies of wealthier samples [5, 6, 9]. In our analyses we investigated the best way to collapse groups by time of the first reported return to work. Although our multivariable multinomial model (no return to work vs. time of return to work) and multivariable model (no return to work vs. return at any time during the study) differed with respect to race/ethnicity, the relationship between not returning to work and receipt of chemotherapy was not sensitive to variation in how the groups were collapsed, buttressing the credibility of this finding (income and comorbidity burden also were associated with not returning to work in both models). By focusing on the more complete model, which included time of the first reported return to work, we were able to demonstrate the importance of continuing to work on long-term work outcomes even as early as 6 months after diagnosis.
A limitation of our study is that we do not have information about participants’ work status between surveys or amount of time taken off from work for those working at 6 months. After initially returning to work, most participants also reported working in all subsequent surveys, so it is likely that few women stopped and then restarted work between surveys, such that their absences are not captured in our data. However, future research should investigate whether there is a threshold number of missed work days after which women are less likely to return to work. The role of symptom management also should be investigated. A limitation of this study is that we do not have information about quality of life at baseline, but in a previous study we demonstrated that psychosocial health was associated with return to work 18 months after diagnosis among both low-income Latina and non-Latina white breast cancer survivors [1]. With respect to symptom control earlier on in the disease trajectory, previous research has indicated that depression, pain, and nausea were the three most commonly reported symptoms, occurring in 63, 56, and 42 % of low-income breast cancer patients 6 months after diagnosis [23]. However, only 26 % of physicians were aware of their patients’ depressive symptoms, compared to more than 70 % who were aware of their patients’ pain and two-thirds who were aware of their patients’ nausea, and physician recognition of depression was least common in less-acculturated Latinas and Asian/Pacific Islanders. Importantly, physician awareness of depression and of pain was associated with resolution of these symptoms. Improved symptom recognition and management by clinicians has the potential to be an important factor in facilitating early return to work and, therefore, long-term employment outcomes. Public policy should support increased clinician awareness of patient symptoms and promote understanding of the potential impact of adequate symptom management on both short-term and long-term outcomes.
Another limitation of our study is the lack of detailed information about participants’ work conditions and relationship with their employer, both of which may affect the relationship between receipt of chemotherapy and return to work [5]. The role of employee negotiation in obtaining accommodation remains poorly understood. Those least likely to obtain accommodation may be undocumented workers and those working for individual employers or small businesses, since employers of fewer than 15 workers are not obligated to provide accommodation under the Americans with Disabilities Act [24]. Brown et al. [25] recently reported on the development of an electronic education tool for cancer patients to improve communication with an employer. Additional research is needed to understand how such interventions might enhance survivors’ negotiation skills and improve employment outcomes on a large scale.
In its landmark report, From Cancer Patient to Cancer Survivor: Lost in Transition, the Institute of Medicine charged clinicians with addressing employment concerns with their patients and recommended that providers familiarize themselves with legal protections for survivors at work, provide patients with information about these protections and employment programs, and ask patients if they are experiencing health problems that affect their ability to work [26]. Future research should focus on better understanding the reasons for the relationship between job loss and receipt of chemotherapy so that appropriate interventions may be developed.
Our findings may have important policy implications. The recent passage of “Right to Work” legislation in several states [27], severely restricting the ability of unions to protect workers’ rights, may disproportionately affect workers with cancer. Those whose jobs previously were safeguarded in the event of a prolonged absence due to illness may find that these same protections are eliminated in the absence of organized labor. Such drawbacks of the new legislation should be highlighted as should its disparate impact on cancer patients and those with other life-threatening medical problems requiring long-term treatment. Similarly, the scope of the Americans with Disabilities Act should be extended to include employees of small businesses, which includes many non-unionized, low-income workers, who are less likely to have sick leave and disability benefits and are, therefore, at risk of job loss due to severe illness. For those who ultimately lose their jobs and are unable to find similar positions when they are ready to return to work, job reorientation and skill-building programs could help shorten the period of unemployment and associated financial hardship. Just as the Institute of Medicine charged clinicians with advocating for their patients by empowering them with the information needed to protect themselves at work, so should the larger oncology community, including the patient advocacy movement, promote local and national policy changes to address these concerns.
Acknowledgments
The authors gratefully acknowledge Paige Nobles for assistance with graphics.
Funding American Cancer Society (TURSG-02-081); California Breast Cancer Research Program (7PB-0070); National Cancer Institute (1R01CA119197-01A1 and 1R01CA140481-01A1); American Cancer Society (MRSGT-11-002-01-CPHPS); American Society of Clinical Oncology (CDA, Blinder).
Footnotes
Conflict of interest The authors have no conflicts of interest to disclose.
Contributor Information
Victoria Blinder, Email: blinderv@mskcc.org, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA. Center for Health Policy and Outcomes, Department of Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, 300 East 66th Street, New York, NY 10065, USA.
Sujata Patil, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA.
Carolyn Eberle, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA. Center for Health Policy and Outcomes, Department of Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, 300 East 66th Street, New York, NY 10065, USA.
Jennifer Griggs, University of Michigan Medical School, 2800 Plymouth Road, Building 16 400S, Ann Arbor, MI 48109, USA.
Rose C. Maly, David Geffen School of Medicine at UCLA, 10880 Wilshire Blvd., Suite 1800, Los Angeles, CA 90024, USA
References
- 1.Blinder V, Patil S, Thind A, Diamant A, Hudis C, Basch E, Maly R. Return to work in low-income latina non-latina white breast cancer survivors: a three-year longitudinal study. Cancer. 2012;118(6):1664–1674. doi: 10.1002/cncr.26478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Holzel D. Predictors of quality of life of breast cancer patients. Acta Oncol. 2003;42(7):710–718. doi: 10.1080/02841860310017658. [DOI] [PubMed] [Google Scholar]
- 3.Feuerstein M, Todd BL, Moskowitz MC, Bruns GL, Stoler MR, Nassif T, Yu X. Work in cancer survivors: a model for practice and research. J Cancer Surviv. 2010;4(4):415–437. doi: 10.1007/s11764-010-0154-6. [DOI] [PubMed] [Google Scholar]
- 4.Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Graff J, Katz SJ. Racial/ethnic differences in job loss for women with breast cancer. J Cancer Surviv. 2011;5(1):102–111. doi: 10.1007/s11764-010-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bouknight RR, Bradley CJ, Luo Z. Correlates of return to work for breast cancer survivors. J Clin Oncol. 2006;24(3):345–353. doi: 10.1200/JCO.2004.00.4929. [DOI] [PubMed] [Google Scholar]
- 6.Satariano WA, DeLorenze GN. The likelihood of returning to work after breast cancer. Public Health Rep. 1996;111(3):236–241. [PMC free article] [PubMed] [Google Scholar]
- 7.Bradley CJ, Neumark D, Bednarek HL, Schenk M. Short-term effects of breast cancer on labor market attachment: results from a longitudinal study. J Health Econ. 2005;24(1):137–160. doi: 10.1016/j.jhealeco.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat. 2010;119(1):213–220. doi: 10.1007/s10549-009-0389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drolet M, Maunsell E, Brisson J, Brisson C, Masse B, Deschenes L. Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol. 2005;23(33):8305–8312. doi: 10.1200/jco.2005.09.500. [DOI] [PubMed] [Google Scholar]
- 10.Peuckmann V, Ekholm O, Sjogren P, Rasmussen NK, Christiansen P, Moller S, Groenvold M. Health care utilisation and characteristics of long-term breast cancer survivors: nationwide survey in Denmark. Eur J Cancer. 2009;45(4):625–633. doi: 10.1016/j.ejca.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Diamant A, Thind A, Maly R. Determinants of breast cancer knowledge among newly diagnosed, low-income, medically underserved women with breast cancer. Cancer. 2008;112(5):1153–1161. doi: 10.1002/cncr.23262. [DOI] [PubMed] [Google Scholar]
- 12.Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28(2):212–232. doi: 10.1177/0163278705275342. [DOI] [PubMed] [Google Scholar]
- 13.Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94(1):39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 14.Seeman TE, Berkman LF. Structural characteristics of social networks and their relationship with social support in the elderly: who provides support. Soc Sci Med. 1988;26(7):737–749. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]
- 15.Marin G, Sabogal F, Marin B, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for hispanics. Hispanic J Behav Sci. 1987;9(2):183–205. [Google Scholar]
- 16. [Accessed 17 Apr 2009];United States Census Bureau Index of Occupations. 2002 http://www.census.gov/hhes/www/ioindex/ioindex02/occ02_a.html.
- 17.Health and Retirement Study. [Accessed 17 Apr 2009];Ahead core, final, version 2.0, May 2002. 1995 revised August 2007, master codes. http://hrsonline.isr.umich.edu/modules/meta/1995/core/codebook/a95_mastercode.htm.
- 18.Chirikos TN, Russell-Jacobs A, Cantor AB. Indirect economic effects of long-term breast cancer survival. Cancer Pract. 2002;10(5):248–255. doi: 10.1046/j.1523-5394.2002.105004.x. [DOI] [PubMed] [Google Scholar]
- 19.Ashing-Giwa KT, Tejero JS, Kim J, Padilla GV, Hellemann G. Examining predictive models of HRQOL in a population-based, multiethnic sample of women with breast carcinoma. Qual Life Res. 2007;16(3):413–428. doi: 10.1007/s11136-006-9138-4. [DOI] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Bureau of Labor Statistics, US Department of Labor. [Accessed 15 May 2012];Employee Benefits in the United States. 2011 Mar; USDL-11-1112. http://www.bls.gov/ncs/ebs/sp/ebnr0017.pdf.
- 23.Maly RC, Liu Y, Leake B, Thind A, Diamant AL. Treatment-related symptoms among underserved women with breast cancer: the impact of physician-patient communication. Breast Cancer Res Treat. 2010;119(3):707–716. doi: 10.1007/s10549-009-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. [Accessed 10 July 2007];The Americans with Disabilities Act of 1990, Titles I and V. 1990 http://www.eeoc.gov/laws/statutes/ada.cfm.
- 25.Brown RF, Owens M, Bradley C. Employee to employer communication skills: balancing cancer treatment and employment. Psychooncology. 2013;22(2):426–433. doi: 10.1002/pon.2107. [DOI] [PubMed] [Google Scholar]
- 26.Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: lost in transition. National Academies Press; Washington, DC: 2006. [Google Scholar]
- 27.Greenhouse S. Labor sees bright spots in membership trends. The New York Times. 2013 Jan 28; [Google Scholar]