Abstract
Bullous Systemic Lupus Erythematosus (BSLE) is a rare manifestation of Systemic Lupus Erythematosus (SLE), characterized histologically by subepidermal bullae with predominantly neutrophilic infiltrate and immunoglobulin (IgG, IgA, IgM) and C3 deposition at the basement membrane zone. Often associated is a heterogeneous profile of autoimmunity to components of type VII collagen. It needs to be differentiated from other subepidermal bullous diseases in view of potentially associated systemic manifestations of SLE. We report a 39-year-old lady who presented with an extensive vesicobullous eruption on face, neck, trunk, and mucosa. She was also found to have photosensitivity, significant anemia, and high antibody titers confirming SLE. Routine histopathology and immunoflorescence studies suggested BSLE and she responded favorably to dapsone. The importance of clinical and histopathological findings in confirming a diagnosis of BSLE along with the very encouraging response to dapsone therapy is highlighted.
Keywords: Dapsone, type VII collagen, immunobullous diseases
Introduction
What was known?
Bullous systemic lupus erythematosus (SLE) is a clinicopathologically distinctive immunobullous eruption occurring during the course of SLE. Circulating antibodies to type VII collagen (NC1 domain) are reported in most of the cases. The disease is very responsive to dapsone therapy.
Subepidermal blister formation in the course of severe systemic lupus erythematosus (SLE) can occur due to extensive interface inflammation and basal cell vacuolation, presenting as polycyclic erosions with advancing blistering border predominantly on sun-exposed areas.[1] In contrast, bullous systemic lupus erythematosus (BSLE) is a distinctive bullous eruption occurring with SLE,[1] presenting with typical clinical and pathological findings including circulating antibodies to type VII collagen (NC1 [noncollagenous domain 1] domain). Occasionally other antigens such as laminin 5, laminin 6, and BP230 (bullous pemphigoid antigen) have also been described.[2] We present a distinctive case of BSLE with an excellent response to dapsone therapy.
Case Report
A 39-year-old lady, a homemaker and mother of three, presented with largely asymptomatic vesicobullous lesions (2 months duration), involving head and neck, upper limbs, and trunk over both photo-exposed and unexposed areas. The blisters would rupture over 2-3 days; yielding clear (sometimes hemorrhagic) fluid; heal over 2-3 weeks; leaving behind pigmentation and occasional scarring. Concurrent painful oral ulcers were reported; though, other mucosae were uninvolved. A 6-month history suggestive of Raynaud's phenomenon; arthralgias involving small joints of hands and feet; photosensitivity; and intermittent episodes of mild to moderate fever was present. The patient reported three previous, spontaneous abortions, (5months gestation) the last one being 6 years back.
On examination, there were multiple, tense, clear as well as hemorrhagic, vesicles and bullae, arising over an erythematous base and predominantly involving upper body [Figure 1]. Bulla spread sign and Nikolsky sign were positive. In addition, superficial erosions, areas of postinflammatory hyperpigmentation, and small superficial scars were noted. Superficial erosions were also noted over the buccal mucosa, hard palate, and lips. Her systemic examination was essentially normal.
Figure 1.

Presence of tense vesicles (marked with an arrow) filled with cleat fluid along with superficial erosions with polycyclic margins. Lesions are present on covered as well as exposed areas
A provisional diagnosis of BSLE was considered and she was thoroughly investigated. She had a significant anemia (8.8 gm/dL) with evidence of iron deficiency on peripheral smear and iron studies. Other biochemical investigations were essentially normal, with no evidence of renal derangement. Extensive serological workup revealed antinuclear antibody positivity of 1:640 (using hep-2 cells); positive anti-dsDNA, anti-Ro, and anti-La antibodies; low levels of C3 and C4 with a normal CH50 component; negative antiphospholipid antibody, rheumatoid factor, and C-reactive protein. Russell's viper venom test revealed no lupus like anticoagulant. X-rays of chest and involved joints were normal.
A lesional biopsy revealed subepidermal split with neutrophilic infiltrate in the papillary dermis [Figure 2]. Direct immunofluorescence (both perilesional and distant-covered skin) revealed IgM and C3 deposition along the basement membrane zone (BMZ) as well as perivascular location. Due to resource constraints, indirect immunofluorescence or salt-split skin could not be performed. Based on clinical, histopathological, and serological evidence, a diagnosis of BSLE was confirmed.
Figure 2.
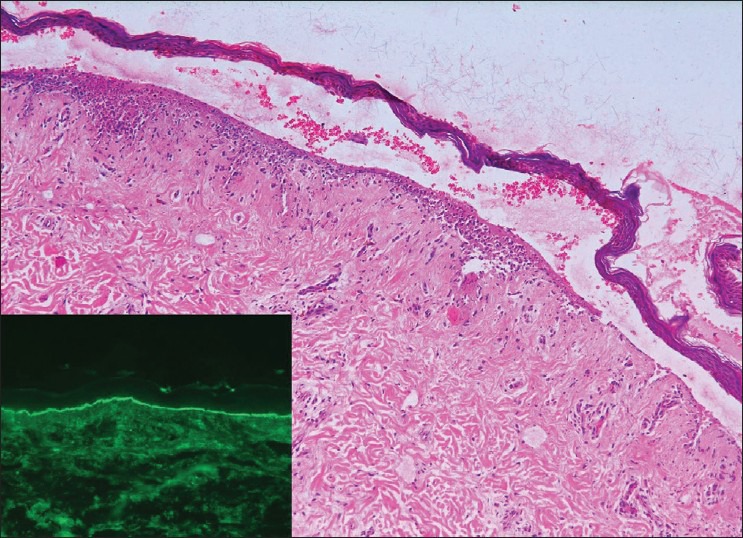
Biopsy taken from vesicular lesion revealed a subepidermal split, containing numerous red blood cells. A marked neutrophilic infiltrate is seen in the papillary dermis (H and E, ×250). Inset shows a positive lupus band (IgG) at the basement membrane zone)
With a normal glucose 6-Phosphate dehydrogenase (G6PD) activity, we planned to start her on dapsone; however, her low hemoglobin prevented this. She was started on prednisolone (1 mg/kg/day as a single morning dose); hydroxychloroquine (200 mg twice a day); along with complete sunprotection and topical care. Hematinics were also initiated. There was only partial improvement with new lesions developing even after 4 weeks; wherein, she was started on dapsone. She responded quite favorably with no new lesions and satisfactory healing of pre-existing ones [Figure 3]. Over the next 6 months, steroids were completely withdrawn, and dapsone and hydroxychloroquine continued for further 1 year. The patient has remained in remission without any systemic manifestations as well, over the last 1 year.
Figure 3.

Marked improvement seen 1 week after starting dapsone therapy
Discussion
Cutaneous lesions are reported during the course of SLE in 76% patients; however, vesicobullous lesions account for less than 1% of these.[3] One of the most distinctive clinical presentations of this is BSLE. It generally affects young adult females and involves both sun-exposed and nonexposed areas. Clinically, it is characterized by subepidermal blisters; appearing on erythematous or urticated base; with a predilection for face, upper trunk, and proximal extremities. Lesions can mimic bullous pemphigoid (BP), inflammatory variant of epidermolysis bullosa acquisita (EBA), and linear IgA disease.[4]
Our understanding of the pathology of this interesting and unique dermatologic condition has evolved with improved diagnostic criteria and clinicohistologic profiling.[4] Gammon and Briggaman suggested six diagnostic criteria: fulfillment of American Rheumatism Association (ARA) criteria for SLE; acquired vesicobullous eruption on (but not limited to) sun-exposed skin; histologic evidence of subepidermal blister with neutrophilic infiltrate; presence of IgG, IgM, IgA, and C3 at the BMZ; evidence of antibodies to type VII collagen; and codistribution of immunoglobulin deposits with anchoring fibrils/type VII collagen by immunoelectron microscopy.[5] On the basis of these, BSLE can be of two distinctive types: Type I fulfilling all six criteria, while Type II (undetermined antigen or dermal antigen other than type VII collagen) satisfies criteria 1-4 only.[5]
As seen in our case, BSLE developing with or prior to features of SLE can present a diagnostic dilemma; hence, other subepidermal vesicobullous disorders need to be ruled out. Histopathologically, a predominant neutrophilic infiltrate may suggest Dermatitis herpetiformis (DH) and dramatic response to dapsone is also common to both diseases. Clinical, histopathological, and immunopathological overlap exists with BP as well. EBA is histopathologically and immunopathologically identical, as it is also mediated by antibodies to type VII collagen; however, a dramatic response to dapsone, as in our case, helps differentiate the two as EBA is notoriously resistant to treatment.
The major antigenic epitopes for both BSLE and EBA reside within the fibronectin type III homology region (FN3) of NC1 domain of type VII collagen.[6] This region is important in mediating the interaction between anchoring fibrils and other matrix proteins.[5] Blister formation occurs as a result of antibody-induced interference with normal interactions between type VII collagen and its extracellular matrix ligands; destabilization of anchoring fibrils due to impaired antiparallel dimer formation of type VII collagen; or complement mediated tissue damage.[4,5,7,8]
Whether or not BSLE is associated with systemic activity is a hotly debated topic. Some authors argue against this; though, others have reported a clinical and/or serological flare with the eruption.[9,10] In our patient, symptoms of SLE developed shortly before the eruption, though no significant systemic activity was recorded; however, a meticulous search for systemic involvement is highly suggested.
Most reported cases have dramatically responded to dapsone, with cessation of new lesions in 1-2 days and healing within several days. The same was seen in our case with dapsone (2 mg/kg/day). Though, it may be difficult to introduce the drug initially, as in our case; every attempt should be made to use it, as relatively low doses (25-50 mg) have also been shown to be efficacious.[1] A relative resistance to steroids and immunosuppressives has been reported. Our patient showed only modest improvement on steroids and antimalarials, complete response being seen only with dapsone.
The case is presented for its typical and distinctive features which should prompt an astute physician to suspect and investigate underlying systemic manifestations of SLE. Also, the dramatic response to dapsone is highlighted which remains the drug of choice in the management of this disorder.
What is new?
Dapsone should be considered the drug of choice for bullous systemic lupus erythematosus as treatment response to other options is suboptimal. Even if one is not able to initiate dapsone due to relative contraindications, as in our case, every effort should be made to use it as early as possible. The course of the disease is benign with remission reported in most of the cases within a year, including ours.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Yung A, Oakley A. Bullous systemic lupus erythematosus. Australas J Dermatol. 2000;41:234–7. doi: 10.1046/j.1440-0960.2000.00426.x. [DOI] [PubMed] [Google Scholar]
- 2.Chan LS, Lapiere JC, Chen M, Traczyk T, Mancini AJ, Paller AS, et al. Bullous systemic lupus erythematosus with antibodies recognizing multiple basement membrane components, bullous pemphigoid antigen1, lamini-5, laminin-6, and type VII collagen. Arch Dermatol. 1999;135:569–73. doi: 10.1001/archderm.135.5.569. [DOI] [PubMed] [Google Scholar]
- 3.Gammon WR, Briggaman RA. Bullous eruption of systemic lupus erythematosus. In: Wojnarowska F, Briggaman RA, editors. Management of Blistering Diseases. London: Chapman and Hall Ltd; 1990. pp. 263–75. [Google Scholar]
- 4.Vassileve S. Bullous systemic lupus erythematosus. Clin Dermatol. 2004;22:129–38. doi: 10.1016/j.clindermatol.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 5.Gammon WR, Briggaman RA. Bullous SLE: A phenotypically distinctive but immunologically heterogeneous bullous disorder. J Invest Dermatol. 1993;100:28S–34. doi: 10.1111/1523-1747.ep12355210. [DOI] [PubMed] [Google Scholar]
- 6.Jones DA, Hunt SW, 3rd, Prisayanh PS, Briggaman RA, Gammon WR. Immunodominant auto-epitopes of type VII collagen are short, paired peptide sequences within the fibronectin type III homology region of the noncollagenous (NC1) domain. J Invest Dermatol. 1995;104:231–5. doi: 10.1111/1523-1747.ep12612780. [DOI] [PubMed] [Google Scholar]
- 7.Gammon WR. Hermann Pinkus memorial Lecture-1992. Autoimmunity to collagen VII: Autoantibody mediated pathomechanisms regulate clinical-pathological phenotypes of acquired epidermolysisbullosa and bullous SLE. J Cutan Pathol. 1993;20:109–14. doi: 10.1111/j.1600-0560.1993.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 8.Chen M, Keene DR, Costa FK, Tahk SH, Woodley DT. The carboxyl terminus of type VII collagen mediates antiparallel dimer formation and constitutes a new antigenic epitope for epidermolysisBullosaacquisita autoantibodies. J Biol Chem. 2001;276:21649–55. doi: 10.1074/jbc.M100180200. [DOI] [PubMed] [Google Scholar]
- 9.Yell JA, Allen J, Wojnarowska F, Kirtschig G, Burge SM. Bullous systemic lupus erythematosus: Revised criteria for diagnosis. Br J Dermatol. 1995;132:921–8. doi: 10.1111/j.1365-2133.1995.tb16950.x. [DOI] [PubMed] [Google Scholar]
- 10.Camisa C. Vesiculobullous systemic lupus erythematosus. A report of four cases. J Am Acad Dermatol. 1988;18:93–100. doi: 10.1016/s0190-9622(88)70014-6. [DOI] [PubMed] [Google Scholar]


