Abstract
Objective
Epidemiologic studies have shown that a high calcium intake is related to lower body weight, fat, and serum lipids in obese individuals. However, clinical studies have shown inconclusive results. The present study was conducted to determine if dairy or calcium supplementation alters body composition or serum lipids in Puerto Rican obese adults without dietary energy restriction or exercise.
Methods
A 21-wk randomized clinical trial was conducted in 30 obese adults, aged 21–50 y, with usual calcium intakes <700 mg/d. Subjects were randomly assigned to the following: high dairy (~1300 mg/d of calcium from dairy products by substituting foods); high calcium (~1300 mg/d of calcium; ~700 mg/d from diet and 600 mg/d from a supplement); or placebo. Subjects were asked to continue their established dietary intake (except for the high dairy group) and their physical activity during the study. Body weight was measured monthly; body fat, bone, and serum lipids (total cholesterol, high-density lipoprotein, low-density lipoprotein, and triacylglycerol) were measured at baseline and at 21 wk. Pairwise differences in study endpoints among the groups were assessed using ANOVA and post-hoc analysis.
Results
Grand mean calcium intake was 1200 ± 370 (median 1187) mg/d in the high dairy group, 1171 ± 265 (median 1165) mg/d in the high calcium group, and 668 ± 273 (median 691) mg/d in the control group, which was significantly lower compared to the two treatment groups (P < 0.001). There were no significant group effects in any of the outcome variables.
Conclusion
A high dairy or calcium diet alone did not alter body composition or serum lipids profile in a sample of Puerto Rican obese adults.
Keywords: High calcium, Low calcium, Dairy products, Body fat, Cholesterol, Triacylglycerol
Introduction
Most epidemiologic studies have shown a consistent inverse relationship between dietary calcium intake and body weight and body fat [1–5], and an improvement in lipid profile [2]. However, these associations have not been fully confirmed by clinical trials.
Previous clinical trials testing the role of dietary calcium (from dairy products or from supplements) on body composition have also included energy-restricted diets and/or exercise in obese individuals, with conflicting results. Studies in obese individuals testing calcium supplementation (from supplements or dairy product) with energy restriction found a significant decrease in body weight and body fat in white adults (n = 32) [6] and black males (n = 29) [7]. Others have not found significant changes in body composition with dairy product supplementation in obese adults (mostly women) [8,9] or in premenopausal obese women (n = 58) [10] or with calcium supplementation in obese women (n = 63) [11], in pre- and postmenopausal women (n = 176) [12] or in premenopausal women (n = 58) [10] under energy-restricted diets. Still, others have also not found these effects in normal weight postmenopausal women with calcium supplementation while consuming their usual diets (n = 1471) [13]. Furthermore, a recent study in obese individuals (primarily women) did not find a significant decrease in body weight and body fat either, while consuming a calcium supplement with their usual diets for 2 y (n = 340) [14]. There is only one study published to date testing the effects of dairy product supplementation on body composition without energy-restricted diets or exercise [15]. No significant changes were seen in this study; however, it was performed in normal weight young women (n = 133).
Some trials have also shown a significant improvement in serum lipids profile with calcium supplementation on energy-restricted diets in obese women (n = 63) [11] or while consuming their usual diets in adults with hypercholesterolemia (n = 13–56) [16,17] or in normal older women (n = 223) [18] compared to placebo. However, others have not found similar results in overweight individuals (n = 72–193) [8,19] and in hypertensive (n = 43) or nonhypertensive adults (n = 27) [20].
Studies propose that a possible mechanism explaining the effects of calcium and dairy products on body composition is mediated by parathyroid hormone and 1,25(OH)2D levels. These hormones decrease fat breakdown and increase fat synthesis, possibly by increasing intracellular calcium in adipocytes [21]. Another mechanism proposed is the increase in fecal fat excretion by a diet high in calcium and dairy protein [22].
The effects of dairy or calcium supplementation are not clear without energy-restricted diets or exercise in body composition and blood lipids in obese individuals. In addition, none of these studies have been performed in Hispanics. Therefore, the objective of the present study was to determine whether dairy or calcium supplementation alters body composition or serum lipids in Puerto Rican obese adults without energy-restricted diets or without an exercise intervention.
Materials and methods
We conducted a single-center, randomized, double-blind (single-blinded for the dairy group), placebo-controlled trial for 21 wk to test the effects of calcium supplementation and dairy intake on body fat and serum lipids in obese Puerto Ricans. The study was conducted from October 2007 to April 2008 at the Clinical Research Center (CRC) of the Medical Sciences Campus of the University of Puerto Rico.
Subjects
Forty-six sedentary obese male and female adults, aged 22–50 y, were recruited for the study through flyers, local newspaper, and radio advertisements in the San Juan area in Puerto Rico. Following preliminary screening by telephone, volunteers were invited to the CRC for an orientation meeting. A detailed description of the study was provided and written consent forms were obtained from each subject. Study eligibility criteria included being 21–50 y old, obese (defined by a body mass index (BMI), of 30 kg/m2 or more [23]), absence of chronic conditions, not taking calcium supplements or taking any medication regularly (including birth control pills, weight-reducing pills, insulin, cholesterol-reducing pills, and others), and not lactose intolerant. Women were ineligible if they were pregnant (verified by a urine-based pregnancy test) or lactating. In addition, usual calcium intake from diet and multivitamin and mineral supplements could not exceed 700 mg/d, which was assessed by a 3-d food record at baseline. Of the 46 subjects recruited, 10 did not qualify due to a calcium intake above 700 mg/d and 6 subjects retired before the initial visit. Therefore, 30 subjects were enrolled in the study. They were randomly assigned to one of the three treatments: high dairy group, high calcium group, and control. Five subjects dropped out from the study before the second visit; four females and one male. The reasons for not continuing in the study were as follows: one had medical reasons and four lost interest. There were no significant differences in the subject characteristics between those who completed and those who did not complete the study (data not shown). Of the 25 subjects who completed the study, 20 were female and 5 were male. Within the five males, one was allocated to the high dairy group, two to the high calcium group, and two to the control group. All women were premenopausal. Results for female and male subjects were analyzed together as there were no gender differences in baseline characteristics.
All subjects were studied under protocols approved by the Medical Sciences Campus, University of Puerto Rico Institutional Review Board (Protocol A4540107). Each subject gave written consent for protocol participation and received monetary compensation for their travel and meal expenses.
Intervention protocol
Thirty subjects were randomly assigned to one of the following three diets for 21 wk (five visits): high dairy group, high elemental calcium group, or control group. Subjects in the high dairy group were instructed to consume four daily servings of dairy products (low-fat milk, low-fat cheese, and low-fat yogurt), with a dairy calcium intake goal of 1200–1300 mg/d. Four servings of dairy products per day were chosen because they are comparable to the US Dietary Guidelines. Subjects were advised to substitute some foods for the dairy products to maintain an isocaloric diet. This was achieved by reviewing each subject’s food record and identifying with each one the foods to substitute. In addition, subjects were instructed to distribute the consumption of the four servings of the dairy products throughout the day. These products were provided monthly by the research team. To encourage dietary adherence, the dairy products provided were tailored monthly to their taste. Subjects in the high elemental calcium group were instructed to consume their usual diet plus a calcium supplement of 600 mg/d (calcium carbonate, from Delavau LLC, Philadelphia, PA, USA), for a total calcium intake goal of 1200–1300 mg/d. This level of calcium was chosen because it is comparable to the Dietary Reference Intake (DRI) for the US [24]. Subjects in the control group were instructed to consume their usual diet plus a placebo tablet, for a total calcium intake goal of <700 mg/d. Subjects were instructed to consume one tablet daily with lunch or dinner.
To maintain a constant energy intake during the 21 wk of the study, subjects in the high elemental calcium group and subjects in the control group were instructed to maintain their usual diets. Subjects in the dairy group were advised to substitute certain foods to maintain energy intake constant throughout the study. Subjects were also instructed to maintain their usual level of physical activity throughout the study. An isocaloric diet was chosen for this study, as well as a constant level of physical activity, to rule out the effects of an energy-restricted diet or an increased physical activity on body fat and serum lipids, therefore, allowing the direct study of the effects of calcium on body composition.
Body composition measurements
Body weight was measured monthly with a calibrated scale (Detecto Inc., Northbrook, IL, USA). Height was measured at baseline using a wall-mounted tape. Measurements were taken while subjects wore light clothing, no shoes or accessories, by the CRC-trained personnel, who were blinded to the study treatments. BMI was calculated using the following formula: kg/m2. Lean body mass, total and trunk fat mass, and total and trunk percentage fat were assessed at baseline and at 21 wk by dual energy x-ray abosorptiometry (Hologic DP-W; Hologic, Bedford, MA, USA). Total bone mineral content (TBMC) and total bone mineral density (TBMD) were also assessed from dual energy x-ray abosorptiometry measurements.
Blood samples were collected at baseline and at 21 wk, between 0700 and 1100 after a 12-h fast. Then they were immediately centrifuged at 12 000 × g for 10 min, and serum was stored at −80°C. Cholesterol (total, low-density lipoprotein (LDL), and high-density lipoprotein (HDL)) and triacylglycerol levels were determined by a colorimetric assay using a commercial kit (Vitros Chemical Products, Ortho Clinical Diagnostics, Raritan, NJ, USA).
Assessment of dietary intake and compliance to the protocol
Subjects were provided individual instruction, counseling, and assessment to ensure treatment adherence. Dietary compliance was closely monitored throughout the study by the three following instruments: monthly calendar, food records, and a food frequency questionnaire (FFQ). The monthly calendar was completed daily by each subject and returned to the research team on the next monthly visit. Subjects in the high elemental calcium group or placebo group were asked to include if the tablet was consumed on each day, while subjects in the high dairy group were asked to include the number of dairy products servings consumed per day.
Food records were completed for 3 d at baseline and at 21 wk. Subjects were advised to record all foods and beverages consumed throughout the day during 2 d of the week and 1 d of the weekend. Subjects were also asked to specify time and place of each meal, type of foods, preparations, and brands as precisely as possible, and the amount of each food and beverage consumed. Detailed oral and written instructions were given to each subject to take home. In addition, each subject received a portion size picture booklet, which included food models of common foods, measuring cups and spoons, different sized bowls, glasses, plates, and mounds, to help subjects estimate portion sizes. Each record was carefully reviewed by a registered dietitian for completeness and accuracy of recording and analyzed using the Nutritionist Pro Nutrient Analysis Software (2007, Axxya System, Stafford, TX, USA). In addition, subjects completed a 24-h food recall at each monthly visit using the same instrument of the food record to monitor compliance.
Compliance was also monitored with a validated semi-quantitative FFQ of foods and beverages rich in calcium [25]. It was completed at each visit by face-to-face interviews with the investigator from the second visit (week 4). The FFQ consisted of a list of 26 items identified from the baseline food records and from other typical Puerto Rican foods rich in calcium. The FFQ was divided into the three following sections: dairy products and other calcium rich foods, prepared foods rich in calcium, and supplements. Each food item included a fixed commonly used portion size. The frequency of each food item was assessed for the previous month and included eight frequency responses, ranging from “Three or more servings per day” to “Rarely or never.” These compliance instruments were carefully revised for each subject, and if necessary, subjects were encouraged to comply with the protocol throughout the study.
Assessment of physical activity
Physical activity was also closely monitored to ensure that subjects were not changing their usual level of physical activity during the study. The Framingham Physical Activity Index questionnaire was used [26], which has been previously validated in Puerto Rican adults [27]. A person who reports sleeping all day will have an index of 24, while a very active person will have an index of 72. This questionnaire was completed at baseline and at wk 21 during 3 d at home. Detailed oral and written instructions were provided. Each questionnaire was carefully reviewed by a member of the research team for completeness and accuracy. It was also completed at each monthly visit to record the level of physical activity of the previous 24 h by face-to-face interviews with the investigator. Subjects were reminded at each monthly visit to maintain the same level of daily activity recorded at baseline throughout the study.
Statistical analysis
Sample size was calculated using the following as the main outcome variables: fat mass and body weight changes. When the sample size in each of the three groups is 7, a one-way analysis of variance (ANOVA) will have 90% power to detect a change of 5% in fat mass at the 0.05 level. We increased the sample size to 10 per group to allow for dropouts.
Means and standard error were computed for all the continuous variables. The data were checked for normality and log transformations were applied to nonnormal variables (LDL and triacylglycerol levels). A repeated measures ANOVA was performed to test for changes in energy and calcium intake and physical activity from baseline and throughout the study, with post-hoc multiple pairwise by Bonferroni. Pairwise differences in study endpoints among the three treatment groups were assessed using ANOVA and post-hoc multiple pairwise by Bonferroni. We also used analysis of covariance, with measures of body composition or serum lipids at the end of the trial as the dependent variables, treatment group as the independent variable, and baseline body composition or serum lipids measurements as the covariates.
Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at RCM-UPR [28]. REDCap is a secure, web-based application designed to support data capture for research studies. Statistical significance was set at P < 0.05. The Statistical SPSS software program (version 15.0, 2006, SPSS Inc, Chicago, IL, USA) and Microsoft Excel for Windows 2007 (Redmond, WA, USA) were used for all the statistical analyses. All data are presented as mean ± SE.
Results
A total of 25 subjects completed the 21 wk of the study, 20 females and 5 males. Initial characteristics of the subjects who completed the study are shown in Table 1. No significant differences were observed in baseline characteristics between the three treatment groups.
Table 1.
Baseline characteristic of the subjects by treatment groups (mean ± SE)
| Variable | High dairy group (n = 8) | High calcium group (n = 9) | Control group (n = 8) |
|---|---|---|---|
| Gender (%) | 88 F, 12 M | 78 F, 22 M | 75 F, 25 M |
| Age (y) | 38.3 ± 2.4 | 35.3 ± 2.2 | 39.5 ± 2.2 |
| Weight (kg) | 102.3 ± 5.7 | 115.2 ± 5.6 | 104.9 ± 4.5 |
| Height (cm) | 159.4 ± 1.2 | 164.7 ± 3.1 | 162.3 ± 1.8 |
| BMI (kg/m2) | 39.9 ± 2.2 | 38.5 ± 1.9 | 36.7 ± 1.6 |
| Ca intake (mg/d)* | 587.9 ± 30.7 | 533.8 ± 54.0 | 526.1 ± 50.4 |
| Energy intake (kcal/d)* | 2005.0 ± 69.8 | 1935.2 ± 149.5 | 1974.2 ± 186.6 |
| Physical activity index score† | 28.2 ± 0.6 | 29.3 ± 0.5 | 30.2 ± 0.8 |
There were no significant differences between the groups at baseline by ANOVA (P > 0.05).
Estimated from baseline 3-d diet records.
Estimated from baseline 3-d physical activity records.
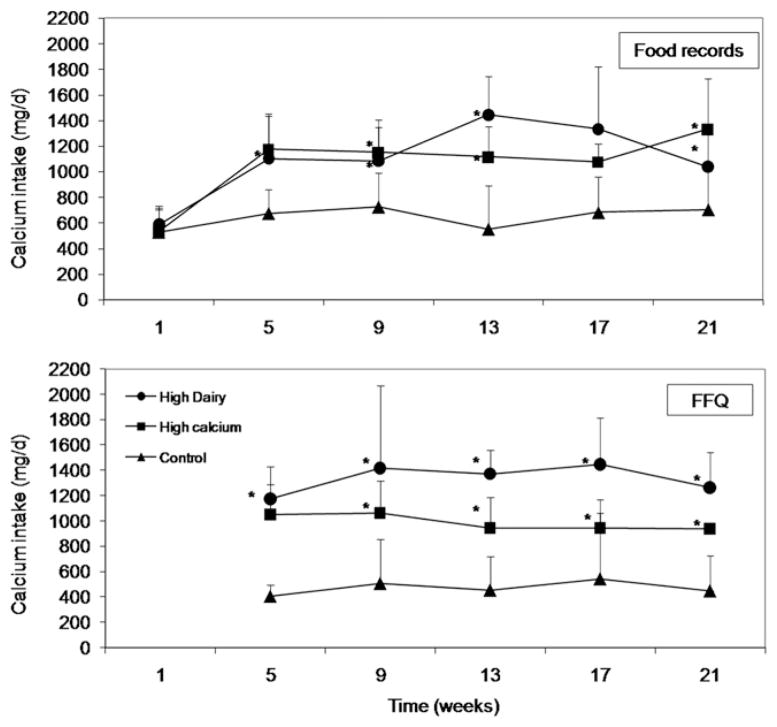
Compliance to the treatments in subjects completing the study was carefully monitored by the three following instruments: monthly calendar, calcium intake from food records, and calcium intake from FFQ, as explained in the Methods section. The compliance estimated from the monthly calendar during the trial was on average 86 ± 14% in the high dairy group, 96 ± 6% in the high calcium group, and 91 ± 10% in the control group. Calcium intake, estimated from food records, significantly increased in the treatment groups after baseline and remained significantly higher compared to the control group thereafter (P < 0.05), while it did not change in the control group throughout the study (Fig. 1). Grand mean calcium intake from food records during the trial was 1200 ± 370 mg/d (median 1187 mg/d) in the high dairy group, 1171 ± 265 mg/d (median 1165 mg/d) in the high calcium group, and 668 ± 273 mg/d (median 691 mg/d) in the control group, which was significantly lower compared to the two treatment groups (P < 0.001). Calcium intake, estimated from FFQ, was also significantly higher in the intervention groups compared to the control group throughout the study (P < 0.05) (Fig. 1). Grand mean calcium intake from FFQ during the trial was 1337 ± 380 mg/d (median 1343 mg/d) in the high dairy group, 988 ± 250 mg/d (median 958 mg/d) in the high calcium group, and 463 ± 325 mg/d (median 385 mg/d) in the control group, which was also significantly lower compared to the treatment groups (P < 0.05). There was a significant correlation between calcium intake from the monthly food records and the FFQs (r = 0.52–0.80, P < 0.01). Energy intake was similar between treatment groups throughout the study as estimated from the food records (P = 0.806; Fig. 2). Grand mean energy intake during the study was 1935 ± 529 kcal/d (median 1961 kcal/d) in the high dairy group, 2128 ± 672 kcal/d (median 2029 kcal/d) in the high calcium group, and 2003 ± 662 kcal/d (median 1900 kcal/d) in the control group. The physical activity index was also similar between treatment groups throughout the study (P = 0.764; Fig. 3). Grand mean physical activity index score during the study was 28.1 ± 2.5 (median 27.5) in the high dairy group, 27.6 ± 1.6 (median 27.2) in the high calcium group, and 27.8 ± 2.0 (median 27.2) in the control group, indicating a sedentary level.
Fig. 1.
Calcium intake estimated from food records and FFQ during the study. Repeated measures ANOVA and post-hoc multiple pairwise by Bonferroni showed a significant increased in calcium intake from baseline to month 2 and then on in the high dairy group and high elemental group (P < 0.001). There was no increase in calcium intake at any point during the study in the control group (P = 0.38). *Significantly different from the control group (P < 0.05).
Fig. 2.
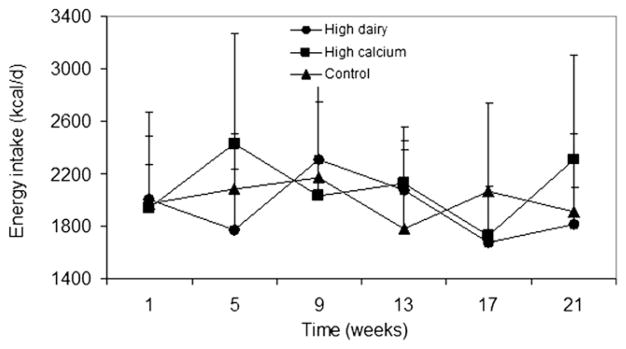
Energy intake estimated from food records during the study. No significant difference was observed between groups throughout the study by repeated measures ANOVA and post-hoc multiple pairwise by Bonferroni (P = 0.806).
Fig. 3.
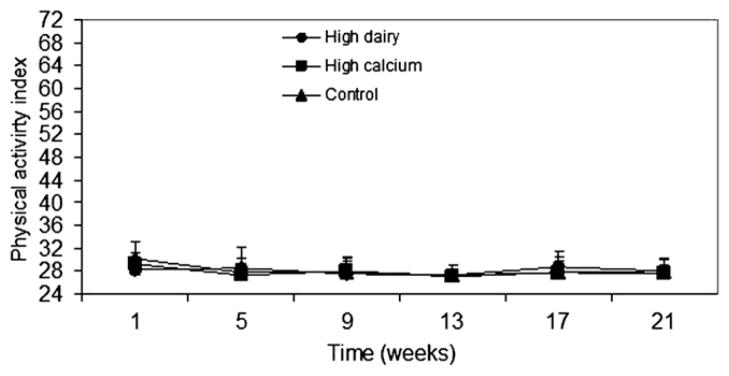
Physical activity index during the study. No significant difference was observed between groups throughout the study by repeated measures ANOVA and post-hoc multiple pairwise by Bonferroni (P = 0.764).
Measures of body composition by treatment groups at baseline and after 21 wk are shown in Table 2. No significant group effects were observed on the mean 21-wk change in weight (P = 0.77), BMI (P = 0.71), total body lean mass (P = 0.85), total body fat mass (P = 0.71), total body percentage fat (P = 0.49), trunk body fat mass (P = 0.71), trunk body percentage fat (P = 0.44), TBMC (P = 0.25), and total TBMD (P = 0.12). Subjects in the high dairy group lost more total and trunk percentage fat and fat mass compared to the other groups, but this was not statistically significant. In addition, lean mass increased in the dairy groups compared to the other groups, but this also was not statistically significant. Serum lipids profile by treatment groups at baseline and after 21 wk is also shown in Table 2. No significant group effects were observed on the mean 21-wk change in total cholesterol (P = 0.31), HDL levels (P = 0.72), LDL levels (P = 0.56), and triacylglycerol levels (P = 0.53), although there was an 18% decrease in triacylglycerol levels in the high dairy group. The results remained similar when only women were included in the analysis. Results were also similar if only subjects who were compliant with the protocol intervention were included in the analysis (high dairy group, n = 7; high calcium group, n = 9; and control group, n = 6). Compliance with the protocol included an 80% compliant rate (estimated from the monthly calendar), that subjects in the control group did not increased their mean calcium intake >200 mg/d during the study and that subjects in the intervention groups increased their daily calcium intake by >450 mg/d over the study period.
Table 2.
Changes in body composition and serum lipids by treatment groups in the study (mean ± SE)
| Variables | High dairy group (n = 8)
|
High calcium group (n = 9)
|
Control group (n = 8)
|
|||
|---|---|---|---|---|---|---|
| Baseline | 21 wk | Baseline | 21 wk | Baseline | 21 wk | |
| Weight (kg) | 102.3 ± 5.7 | 102.6 ± 6.2 | 115.2 ± 5.6 | 115.0 ± 5.7 | 104.9 ± 4.5 | 104.3 ± 4.5 |
| BMI (kg/m2) | 39.9 ± 2.2 | 40.1 ± 2.4 | 38.5 ± 1.9 | 38.4 ± 1.9 | 36.7 ± 1.6 | 36.5 ± 1.6 |
| Total body lean mass (kg) | 53.8 ± 1.8 | 53.90 ± 2.1 | 60.94 ± 3.7 | 60.64 ± 3.9 | 55.52 ± 2.5 | 55.18 ± 2.7 |
| Total body fat mass (kg) | 44.2 ± 4.3 | 43.68 ± 4.4 | 48.85 ± 2.3 | 49.09 ± 2.1 | 44.61 ± 2.9 | 44.18 ± 2.8 |
| Total body fat (%) | 42.9 ± 2.1 | 42.5 ± 2.2 | 43.7 ± 1.2 | 44.1 ± 1.1 | 43.3 ± 1.5 | 43.4 ± 1.6 |
| Trunk body fat mass (kg) | 17.5 ± 1.1 | 17.01 ± 1.1 | 21.03 ± 1.0 | 21.11 ± 1.0 | 19.37 ± 1.3 | 19.06 ± 1.3 |
| Trunk body fat (%) | 39.5 ± 1.5 | 38.7 ± 1.2 | 41.5 ± 1.0 | 41.9 ± 0.8 | 41.5 ± 1.4 | 41.6 ± 1.4 |
| TBMC (g) | 2258.8 ± 212.6 | 2254.5 ± 219.9 | 2517.5 ± 427.4 | 2519.6 ± 395.7 | 2487.3 ± 376.6 | 2447.8 ± 376.6 |
| TBMD (g/cm2) | 1.120 ± 0.054 | 1.129 ± 0.061 | 1.195 ± 0.096 | 1.181 ± 0.100 | 1.192 ± 0.093 | 1.187 ± 0.087 |
| Total cholesterol (mg/dL) | 175.8 ± 8.6 | 175.9 ± 9.4 | 171.6 ± 12.3 | 185.3 ± 11.1 | 159.9 ± 7.8 | 168.6 ± 10.6 |
| HDL cholesterol (mg/dL) | 40.0 ± 1.9 | 42.8 ± 2.0 | 37.8 ± 2.6 | 40.6 ± 2.7 | 39.0 ± 2.6 | 39.0 ± 1.7 |
| LDL cholesterol (mg/dL) | 112.3 ± 9.1 | 114.1 ± 9.3 | 111.2 ± 11.3 | 121.6 ± 9.9 | 99.5 ± 7.6 | 108.8 ± 9.5 |
| Triacylglycerol (mg/dL) | 118.0 ± 14.2 | 95.4 ± 11.8 | 112.0 ± 14.0 | 115.9 ± 17.1 | 107.4 ± 12.8 | 103.0 ± 11.5 |
TBMC, total bone mineral content, TBMD, total bone mineral density
There were no significant differences between the groups by ANOVA (P > 0.05).
The data were further analyzed by actual changes in calcium intake. Subjects were divided in two groups based on their actual calcium intake: <600 mg/d increase in calcium intake during the study (n = 15; 80% female, 20% male) or ≥ 600 mg/d increase in calcium intake during the study (n = 10; 80% female, 20% male) (Table 3). No significant group effects were observed on the mean 21-wk change in weight (P = 0.40), BMI (P = 0.41), total body lean mass (P = 0.12), total body fat mass (P = 0.67), total body percentage fat (P = 0.26), trunk body fat mass (P = 0.73), trunk body percentage fat (P = 0.38), TBMC (P = 0.48), TBMD (P = 0.59), total cholesterol (P = 0.97), HDL levels (P = 0.56), LDL levels (P = 0.96), and triacylglycerol levels (P = 0.66).
Table 3.
Changes in body composition and serum lipids by increase in calcium intake in the study (mean ± SE)
| Variables | <600 mg/d increase in calcium intake during the study (n = 15)
|
≥600 mg/d increase in calcium intake during the study (n = 10)
|
||
|---|---|---|---|---|
| Baseline | 21 wk | Baseline | 21 wk | |
| Weight (kg) | 105.9 ± 5.0 | 106.2 ± 5.1 | 110.5 ± 5.9 | 109.8 ± 6.3 |
| BMI (kg/m2) | 38.2 ± 1.8 | 38.3 ± 1.9 | 38.7 ± 2.0 | 38.4 ± 2.2 |
| Total body lean mass (kg) | 56.1 ± 2.1 | 56.3 ± 2.3 | 58.2 ± 3.8 | 57.38 ± 4.0 |
| Total body fat mass (kg) | 45.2 ± 3.6 | 44.9 ± 3.5 | 47.2 ± 2.4 | 47.19 ± 2.5 |
| Total body fat (%) | 42.9 ± 1.8 | 42.7 ± 1.9 | 44.0 ± 1.2 | 44.4 ± 1.1 |
| Trunk body fat mass (kg) | 56.1 ± 2.1 | 56.3 ± 2.3 | 58.2 ± 3.8 | 57.38 ± 4.0 |
| Trunk body fat (%) | 40.4 ± 1.5 | 40.1 ± 1.4 | 41.5 ± 0.9 | 41.9 ± 0.8 |
| TBMC (g)1 | 2425.2 ± 82.7 | 2405.5 ± 81.1 | 2424.9 ± 118.1 | 2421.2 ± 112.9 |
| TBMD (g/cm2)2 | 1.165 ± 0.022 | 1.163 ± 0.021 | 1.178 ± 0.027 | 1.171 ± 0.026 |
| Total cholesterol (mg/dL) | 163.5 ± 7.9 | 171.2 ± 10.0 | 177.6 ± 12.0 | 185.6 ± 10.6 |
| HDL cholesterol (mg/dL) | 39.8 ± 2.1 | 40.9 ± 1.7 | 37.5 ± 2.6 | 40.5 ± 2.8 |
| LDL cholesterol (mg/dL) | 103.7 ± 8.0 | 110.9 ± 9.2 | 113.9 ± 11.2 | 121.4 ± 9.6 |
| Triacylglycerol (mg/dL) | 100.2 ± 11.6 | 96.1 ± 10.2 | 130.8 ± 14.4 | 118.8 ± 17.3 |
TBMC, total bone mineral content; TBMD, total bone mineral density
There were no significant differences between the groups by ANOVA (P > 0.05).
Discussion
The present study showed that increasing calcium intake (through dairy products or calcium supplements) for 21 wk without an energy restriction or exercise intervention in Puerto Rican obese individuals did not lead to significant changes in body composition or serum lipids profile.
Most studies reported to date have tested the effects of calcium supplementation (from dairy products or calcium supplements) on body composition and blood lipids with energy-restricted diets or exercise intervention plans in obese individuals with conflicting results. With a similar study design to the present study, the study by Zemel and collaborators [6] in obese individuals (n = 32) showed that diets high in calcium from supplements (1256 ± 134 mg/d of calcium) or dairy products (1137 ± 164 mg/d of calcium) while consuming energy-restricted diets for 24 wk significantly decreased body weight and fat mass compared to placebo (430 ± 94 mg/d of calcium). However, the present study did not find similar results if subjects consumed their usual diets or isocaloric diets, without energy restriction. Nevertheless, our results are similar to those reported by Gunther et al. [15] in normal weight young women (n = 133) consuming a medium (1026 ± 311 mg/d of calcium), high dairy (1131 ±337 mg/d of calcium) diet, or placebo (742 ± 322 mg/d of calcium) for 1 y while maintaining isocaloric diets. No significant differences were observed in the mean 1-y change in fat mass or body weight between the groups in their study. However, a 6-mo follow-up study in the same population found that the high dairy group maintained a significantly higher calcium intake at 18 mo compared with the control group, and the regression analysis showed that mean calcium intake over the 18 mo predicted a negative change in fat mass (P < 0.05), after controlling for baseline BMI [29]. Another study conducted by Reid et al. [13] did not find significant changes in body weight and fat in normal weight postmenopausal women (n = 1204) with 1000 mg/d of calcium supplementation while consuming their usual diets. Furthermore, a recent study in obese individuals (n = 335) did not find significant changes in body weight or BMI with 1500 mg/d of calcium supplementation while consuming their usual diets for 2 y [14]. However, this study did not screen individuals for low habitual calcium intake.
Studies have suggested that the source of calcium intake (i.e., dairy versus supplements) may influence the effects on body weight and fat mass. Zemel et al. has shown in rodents [21] and in obese adults [6] that dairy products have greater effects on reducing body weight and fat mass than the same level of calcium intake from supplements. Dairy products are rich in bioactive compounds [30], which could explain these effects. In addition, dairy products are usually enriched with vitamin D, which could mediate the effect of calcium on body fat as shown in animal studies [31]. However, this has not been observed in human studies [32,33]. The present study did not find significant differences in body composition and serum lipids profile between the high dairy group and the high elemental calcium group. Nevertheless, subjects in the high dairy group appeared to have smaller increases in body fat and serum lipids, although it was not statistically significant. The small sample size may have been too small to detect these differences.
There are several strengths and limitations of the study. Strengths of this study include the following: design, calcium dose, and compliance measures. The design of the study, a randomized, double-blinded (single-blinded for the high dairy group), placebo-controlled trial with two calcium sources without energy-restricted diets or exercise intervention, allowed studying the effects of calcium alone on body composition and serum lipids under their usual free-living conditions. The total dose aimed in the study (four dairy products servings for the high dairy group and 1200 mg/d for the high calcium group) are similar to the US Dietary Guidelines and US DRI. In addition, these doses are comparable to those used in previous reports in obese individuals [6–9,11]. Compliance to the diet and other lifestyle variables were measured repeatedly by means of different methods (monthly calendar, food records, FFQ, monthly calls and visits to the CRC), which helped in monitoring and improving adherence to the protocol intervention. One of the limitations of the study was the small sample size. However, the sample size calculations provided a power of 90% to detect a difference of 5% in fat mass change between the control and intervention groups.
Conclusion
A high dairy or calcium diet alone did not alter body composition or serum lipids profile in this group of Puerto Rican obese adults, without energy-restricted diets or an exercise intervention plan.
Acknowledgments
This work was supported by the RCMI-RCRII Award, 1P20-RR11126, RCMI Award G12RR-03051, and RCMI-Clinical Research Center award G12RR03051. This publication was possible by Grant 5P20RR011126 from the NCRR, NIH. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
The authors thank Mariely Nieves, M.S., for her help with the statistical analysis.
References
- 1.Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB J. 2000;14:1132–8. [PubMed] [Google Scholar]
- 2.Jacqmain M, Doucet E, Despres JP, Bouchard C, Tremblay A. Calcium intake, body composition, and lipoprotein-lipid concentrations in adults. Am J Clin Nutr. 2003;77:1448–52. doi: 10.1093/ajcn/77.6.1448. [DOI] [PubMed] [Google Scholar]
- 3.Loos RJ, Rankinen T, Leon AS, Skinner JS, Wilmore JH, Rao DC, et al. Calcium intake is associated with adiposity in Black and White men and White women of the HERITAGE Family Study. J Nutr. 2004;134:1772–8. doi: 10.1093/jn/134.7.1772. [DOI] [PubMed] [Google Scholar]
- 4.Marques-Vidal P, Goncalves A, Dias CM. Milk intake is inversely related to obesity in men and in young women: data from the Portuguese Health Interview Survey 1998–1999. Int J Obes (Lond) 2006;30:88–93. doi: 10.1038/sj.ijo.0803045. [DOI] [PubMed] [Google Scholar]
- 5.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002;287:2081–9. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 6.Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res. 2004;12:582–90. doi: 10.1038/oby.2004.67. [DOI] [PubMed] [Google Scholar]
- 7.Zemel MB, Richards J, Milstead A, Campbell P. Effects of calcium and dairy on body composition and weight loss in African-American adults. Obes Res. 2005;13:1218–25. doi: 10.1038/oby.2005.144. [DOI] [PubMed] [Google Scholar]
- 8.Thompson WG, Rostad Holdman N, Janzow DJ, Slezak JM, Morris KL, Zemel MB. Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes Res. 2005;13:1344–53. doi: 10.1038/oby.2005.163. [DOI] [PubMed] [Google Scholar]
- 9.Harvey-Berino J, Gold BC, Lauber R, Starinski A. The impact of calcium and dairy product consumption on weight loss. Obes Res. 2005;13:1720–6. doi: 10.1038/oby.2005.210. [DOI] [PubMed] [Google Scholar]
- 10.Wagner G, Kindrick S, Hertzler S, DiSilvestro RA. Effects of various forms of calcium on body weight and bone turnover markers in women participating in a weight loss program. J Am Coll Nutr. 2007;26:456–61. doi: 10.1080/07315724.2007.10719636. [DOI] [PubMed] [Google Scholar]
- 11.Major GC, Alarie F, Dore J, Phouttama S, Tremblay A. Supplementation with calcium + vitamin D enhances the beneficial effect of weight loss on plasma lipid and lipoprotein concentrations. Am J Clin Nutr. 2007;85:54–9. doi: 10.1093/ajcn/85.1.54. [DOI] [PubMed] [Google Scholar]
- 12.Shapses SA, Heshka S, Heymsfield SB. Effect of calcium supplementation on weight and fat loss in women. J Clin Endocrinol Metab. 2004;89:632–7. doi: 10.1210/jc.2002-021136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reid IR, Horne A, Mason B, Ames R, Bava U, Gamble GD. Effects of calcium supplementation on body weight and blood pressure in normal older women: a randomized controlled trial. J Clin Endocrinol Metab. 2005;90:3824–9. doi: 10.1210/jc.2004-2205. [DOI] [PubMed] [Google Scholar]
- 14.Yanovski JA, Parikh SJ, Yanoff LB, Denkinger BI, Calis KA, Reynolds JC, et al. Effects of calcium supplementation on body weight and adiposity in overweight and obese adults: a randomized trial. Ann Intern Med. 2009;150:821–9. W145–6. doi: 10.7326/0003-4819-150-12-200906160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gunther CW, Legowski PA, Lyle RM, McCabe GP, Eagan MS, Peacock M, et al. Dairy products do not lead to alterations in body weight or fat mass in young women in a 1-y intervention. Am J Clin Nutr. 2005;81:751–6. doi: 10.1093/ajcn/81.4.754. [DOI] [PubMed] [Google Scholar]
- 16.Bell L, Halstenson CE, Halstenson CJ, Macres M, Keane WF. Cholesterol-lowering effects of calcium carbonate in patients with mild to moderate hypercholesterolemia. Arch Intern Med. 1992;152:2441–4. [PubMed] [Google Scholar]
- 17.Denke MA, Fox MM, Schulte MC. Short-term dietary calcium fortification increases fecal saturated fat content and reduces serum lipids in men. J Nutr. 1993;123:1047–53. doi: 10.1093/jn/123.6.1047. [DOI] [PubMed] [Google Scholar]
- 18.Reid IR, Mason B, Horne A, Ames R, Clearwater J, Bava U, et al. Effects of calcium supplementation on serum lipid concentrations in normal older women: a randomized controlled trial. Am J Med. 2002;112:343–7. doi: 10.1016/s0002-9343(01)01138-x. [DOI] [PubMed] [Google Scholar]
- 19.Bostick RM, Fosdick L, Grandits GA, Grambsch P, Gross M, Louis TA. Effect of calcium supplementation on serum cholesterol and blood pressure. A randomized, double-blind, placebo-controlled, clinical trial. Arch Fam Med. 2000;9:31–8. doi: 10.1001/archfami.9.1.31. discussion 39. [DOI] [PubMed] [Google Scholar]
- 20.Karanja N, Morris CD, Illingworth DR, McCarron DA. Plasma lipids and hypertension: response to calcium supplementation. Am J Clin Nutr. 1987;45:60–5. doi: 10.1093/ajcn/45.1.60. [DOI] [PubMed] [Google Scholar]
- 21.Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB J. 2000;14:1132–8. [PubMed] [Google Scholar]
- 22.Papakonstantinou E, Flatt WP, Huth PJ, Harris RB. High dietary calcium reduces body fat content, digestibility of fat, and serum vitamin D in rats. Obes Res. 2003;11:387–94. doi: 10.1038/oby.2003.52. [DOI] [PubMed] [Google Scholar]
- 23.WHO. Obesity: preventing and managing the global epidemic. Washington, DC: World Health Organization; 2000. [PubMed] [Google Scholar]
- 24.Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition board, Institute of Medicine. Dietary reference Intakes for calcium, phosphorus, magnesium, vitamin D, and Fluoride. Washington, DC: National Academy Press; 1997. [Google Scholar]
- 25.Rios RE, Soltero S, Bertran JJ, Matos MM, Palacios C. Validación de un cuestionario semi-cuantitativo de frecuencia de consumo de alimentos para estimar el consumo de calcio de adultos en Puerto Rico. PRHSJ. 2008;27:282. [Google Scholar]
- 26.Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29:S1–205. [PubMed] [Google Scholar]
- 27.Garcia-Palmieri MR, Costas R, Jr, Cruz-Vidal M, Sorlie PD, Havlik RJ. Increased physical activity: a protective factor against heart attacks in Puerto Rico. Am J Cardiol. 1982;50:749–55. doi: 10.1016/0002-9149(82)91229-2. [DOI] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eagan MS, Lyle RM, Gunther CW, Peacock M, Teegarden D. Effect of 1-year dairy product intervention on fat mass in young women: 6-month follow-up. Obesity (Silver Spring) 2006;14:2242–8. doi: 10.1038/oby.2006.263. [DOI] [PubMed] [Google Scholar]
- 30.Shah NP. Effects of milk-derived bioactives: an overview. Br J Nutr. 2000;84(Suppl 1):S3–10. doi: 10.1017/s000711450000218x. [DOI] [PubMed] [Google Scholar]
- 31.Shi H, Dirienzo D, Zemel MB. Effects of dietary calcium on adipocyte lipid metabolism and body weight regulation in energy-restricted aP2-agouti transgenic mice. FASEB J. 2001;15:291–3. doi: 10.1096/fj.00-0584fje. [DOI] [PubMed] [Google Scholar]
- 32.Sneve M, Figenschau Y, Jorde R. Supplementation with cholecalciferol does not result in weight reduction in overweight and obese subjects. Eur J Endocrinol. 2008;159:675–84. doi: 10.1530/EJE-08-0339. [DOI] [PubMed] [Google Scholar]
- 33.White KM, Bauer SJ, Hartz KK, Baldridge M. Changes in body composition with yogurt consumption during resistance training in women. Int J Sport Nutr Exerc Metab. 2009;19:18–33. doi: 10.1123/ijsnem.19.1.18. [DOI] [PubMed] [Google Scholar]