Abstract
The Nutrition Facts panel on food labels in the United States currently displays Daily Values (DVs) that are based on outdated RDAs. The FDA has indicated that it plans to update the DVs based on the newer Dietary Reference Intakes (DRIs), but there is controversy regarding the best method for calculating new DVs from the DRIs. To better understand the implications of DV revisions, assuming that manufacturers choose to maintain current label claims for micronutrients from voluntarily fortified foods, we modeled intake of 8 micronutrients using NHANES 2007–2008 data and 2 potential methods for calculating DVs: the population-weighted Estimated Average Requirement (EAR) and the population-coverage RDA. In each scenario, levels of fortified nutrients were adjusted to maintain the current %DV. Usual nutrient intakes and percentages with usual intakes less than the EAR were estimated for the U.S. population and subpopulations aged ≥4 y (n = 7976). For most nutrients, estimates of the percentage of the U.S. population with intakes below the EAR were similar regardless of whether the DV corresponded to the population-weighted EAR or the population-coverage RDA. Potential decreases were observed in adequacy of nutrients of concern for women of childbearing age, namely iron and folate (up to 9% and 3%, respectively), adequacy of calcium among children (up to 6%), and adequacy of vitamin A intakes in the total population (5%) assuming use of the population-weighted EAR compared with the population-coverage RDA for setting the DV. Results of this modeling exercise will help to inform decisions in revising the DVs.
Introduction
The Nutrition Facts panel on food labels in the United States identifies the levels of vitamins and minerals in a food as percentages of the Daily Values (DVs)9 for those nutrients. Nutrient information presented as a percentage of the DV on food labels provides consumers with information on the relative contributions of a food in the context of their daily diet and can be used to help make nutrient comparisons between foods. The DVs also serve as the basis for health and nutrient content claims found on packaging.
The DVs used on current nutrition labels are based on the 1968 National Academy of Sciences RDAs for most vitamins and minerals. In the most recent revision of the RDAs, a process that began in the 1990s, the Institute of Medicine (IOM) of the National Academy of Sciences developed a new set of standards called Dietary Reference Intakes (DRIs) and released DRI nutrient values for use in assessing and planning diets of healthy individuals (1). The FDA has indicated that it plans to update the DVs based on the newer DRIs (2). In the notice of the FDA’s intent to revise DVs, the FDA proposed several possible approaches for calculating DVs from the DRIs (Table 1). The current method used on food labels today for calculating DVs uses a population-coverage approach, in which DVs generally correspond to the highest RDA value among those established for adults and children aged ≥4 y, excluding values for pregnant and lactating women (2). As part of the process of setting DRIs, the IOM Committee on Use of Dietary Reference Intakes in Nutrition Labeling released a report outlining principles to guide the establishment of updated reference values for nutrition labeling (3). This IOM committee recommended that new DVs for labeling be derived by weighting the life-stage (excluding pregnancy and lactation) and gender-specific EARs (or Adequate Intakes where no EAR has been set) based on census data for Americans aged ≥4 y (Table 1). The EAR-based population-weighted approach it recommended represented a substantial shift from the RDA-based population-coverage approach used to establish the current DVs.
TABLE 1.
Current and potential methods for calculating DVs for micronutrients1
| Current DVs |
Potential DVs |
||
| 1968 RDAs | 1997–2011 DRIs: EARs | 1997–2011 DRIs: RDAs | |
| Definition | Level of intake judged to be adequate to meet the known nutrient needs of practically all healthy persons in a specific age-gender group | The average daily nutrient intake level that is estimated to meet the requirements of half of the healthy individuals in a particular life-stage and gender group | The average daily dietary nutrient intake level that is sufficient to meet the nutrient requirements of nearly all (97–98%) healthy individuals in a particular life-stage and gender group |
| Derivation of a single reference value (i.e., a DV) | Population-coverage approach: | Population-coverage approach: | Population-coverage approach: |
| • Generally the highest RDA value among those established for the age-gender groups | • Highest EAR value among those established for the life-stage and gender groups | • Highest RDA value among those established for the life-stage and gender groups | |
| Or | Or | ||
| Population-weighted approach: | Population-weighted approach: | ||
| • Life-stage– and gender-specific EARs multiplied by the U.S. Census Bureau population projection for the corresponding life-stage and gender group; sum of values divided by total population projection | • Life-stage– and gender-specific RDAs multiplied by the U.S. Census Bureau population projection for the corresponding life-stage and gender group; sum of values divided by total population projection | ||
Both current and potential DVs were derived from reference values for the population of adults and children aged ≥4 y, excluding pregnant and lactating women (1, 4, 5). When insufficient evidence was available to calculate an EAR for a nutrient, an Adequate Intake (AI) corresponding to an estimated median intake was established; the AI could be used to calculate a DV following the same method. Population-weighted values were calculated as defined by the FDA (2). DV, Daily Value; EAR, Estimated Average Requirement.
There is controversy in the scientific community over whether the RDA or the EAR is the appropriate starting reference value for updated DVs and whether the DVs should be set using the current population-coverage approach or the population-weighted approach (6–9). Proponents of the population-weighted EAR approach argue that this method of calculating a DV produces the best single estimate of the nutrient requirements of any individual in the population, and in turn that this is the best point of comparison for evaluating a food’s contribution to nutrient needs without exceeding those needs (8, 9). Proponents of using the RDA to calculate a DV assert that this approach produces a value representing a 97–98% probability of nutritional adequacy for the entire population rather than just 50% of it, and values that will be more consistent with consumer expectations and other nutrition messaging (6, 7).
Potential DVs corresponding to population-weighted and population-coverage approaches using EARs and RDAs for vitamins and minerals are shown in Table 2. The potential DVs will differ on the basis of on the approach chosen because, by definition, the EAR for a nutrient for a specific population is lower than the corresponding RDA, and because a population-weighted DV will be lower than a population-coverage DV unless the RDAs/EARs are identical for all life-stage and gender groups. For the majority of the vitamins and minerals, the population-coverage RDA is equal to or lower than the current DV, and nearly all population-weighted EARs are below the current DV. For a few nutrients (e.g., calcium and vitamins D and C), ≥1 of the RDAs/EARs are higher than the current DVs.
TABLE 2.
Current DVs for select vitamins and minerals and potential DVs based on population-weighted and population-coverage RDAs and EARs1
| Nutrient | Unit | Current DV | Population-coverage RDA | Population-weighted RDA | Population-coverage EAR | Population-weighted EAR |
| Vitamin A | — | 1500 RE | 900 RAE | 754 RAE | 630 RAE | 531 RAE |
| Vitamin D | μg | 10 | 20 | 15 | 10 | 10 |
| Vitamin E | — | 30 IU | 15 mg AT | 14 mg AT | 12 mg AT | 11 mg AT |
| Vitamin C | mg | 60 | 90 | 74 | 75 | 61 |
| Thiamin | mg | 1.5 | 1.2 | 1.1 | 1.0 | 0.9 |
| Riboflavin | mg | 1.7 | 1.3 | 1.1 | 1.1 | 0.9 |
| Niacin | mg | 20 | 16 | 14 | 12 | 11 |
| Vitamin B-6 | mg | 2.0 | 1.7 | 1.3 | 1.4 | 1.1 |
| Vitamin B-12 | μg | 6.0 | 2.4 | 2.3 | 2.0 | 1.9 |
| Folate | μg | 400 | 400 | 378 | 330 | 304 |
| Calcium | mg | 1000 | 1300 | 1085 | 1100 | 885 |
| Magnesium | mg | 400 | 420 | 341 | 350 | 283 |
| Iron | mg | 18 | 18 | 11 | 8 | 6 |
| Zinc | mg | 15 | 11 | 9.1 | 9.4 | 7.7 |
| Copper | mg | 2.0 | 0.9 | 0.8 | 0.7 | 0.7 |
| Phosphorus | mg | 1000 | 1250 | 769 | 1055 | 640 |
| Selenium | μg | 70 | 55 | 52 | 45 | 43 |
With the exception of calcium and vitamin D, values are as reported by the FDA (2); the FDA’s reported population-weighted data are based on 2005 U.S. population projections (10). Values for calcium and vitamin D are based on current DRIs (5); population-weighted calcium and vitamin D values were derived by using 2005 population projection data to be consistent with FDA reported values for other nutrients (10). AT, α-tocopherol; DV, Daily Value; EAR, Estimated Average Requirement; RAE, retinol activity equivalent; RE, retinol equivalent.
Nutrients added to foods through fortification and/or enrichment make important contributions to intakes of nutrients for Americans (11–13), including many nutrients identified as “nutrients of concern” because of widespread inadequate intakes (14). Revisions to the DVs could have an impact on the levels of nutrients that manufacturers add to foods if they choose to maintain current nutrient content or health claims on labels including the %DV on the Nutrition Facts panel, nutrient content claims, and health claims such as the authorized health claim for calcium and osteoporosis (15). Currently, foods containing 10–19% of the DV or ≥20% of the DV may be labeled as a “good” or “excellent” source of a nutrient, respectively (15). Revisions to the DVs therefore could have an impact on intakes of critical nutrients if manufacturers adjust levels of fortification nutrients to align concentrations per serving (e.g., 10% or 20% of the DV) with the revised DVs. For example, if the revised DV is higher than the current DV and food manufacturers continue to voluntarily add the same percentage of the original nutrient DV to foods to maintain current label claims, the absolute amount of the nutrient added to the food through fortification would increase. Alternatively, if the revised DV is lower than the current DV, which is the case for many vitamins and minerals, the %DV on the label could increase if manufacturers continue to add current levels of fortification nutrients. In some cases, the higher %DVs could be sufficiently high to support use of a revised claim (i.e., “excellent” rather than “good” source of the nutrient). If, however, the revised DV is lower than the current DV and for consistency manufacturers choose to maintain current label claims for voluntary fortification nutrients, the absolute amount of the nutrient added to the food through fortification would decrease, and intakes of the nutrient would decrease if food consumption patterns remained the same. Thus, if current nutrient intakes are of concern or marginal, it is possible that reduced fortification due to DV changes could have adverse effects on nutrient intakes by the U.S. population.
To understand the nutritional implications of various approaches that might be used to calculate new DVs from the DRIs, we modeled nutrient intakes and adequacy of intake of several vitamins and minerals in a sample of the U.S. population aged ≥4 y under the current DV scenario and under the 2 DV scenarios representing the potential range of DV reference values calculated from the DRIs. We assumed in each scenario that manufacturers would continue to add the same %DV for nutrients from fortified foods. That is, it was assumed that manufacturers would reformulate fortification levels (either up or down) and maintain current label claims. In this article, we present results for 8 vitamins and minerals: vitamins A, D, E, C, and B-12 and folate, calcium, and iron. These nutrients have been identified as nutrients of concern or as shortfall nutrients but not currently of concern for public health for the U.S. population or subpopulations (14, 16) and are nutrients for which fortification accounts for ≥5% of total intakes (12).
Methods
Study population and data sources.
The study population included individuals aged ≥4 y (excluding pregnant or lactating women) who reported food consumption on day 1 of What We Eat in America (WWEIA) 2007–2008, the dietary interview portion of the 2007–2008 NHANES (17). NHANES and WWEIA are designed to provide nationally representative nutrition and health data and prevalence estimates for nutrition and health status measures in the United States. The study was conducted as a secondary analysis of data; the underlying NHANES study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human participants were approved under continuation of the Ethics Review Board protocol 2005–6 from the National Center for Health Statistics. Written informed consent was obtained from all participants (18). The 2007–2008 release was the most current data at the time of this analysis. The study population included data from a total of 7976 individuals.
Definition of a fortified food.
The manipulation of the micronutrient content of foods is only possible for those food items with nutrient fortification or enrichment; the inherent (i.e., intrinsic) nutrient content of the food remains the same. In this analysis, fortified foods were defined as those with ≥1 nutrients that were voluntarily added for the purposes of enhancing the naturally occurring nutrient content of a food under current U.S. regulations. Foods containing nutrients added for enrichment as defined by an FDA Standard of Identity were not considered fortified foods because it was expected that Standard of Identity levels, many of which were designed to replace nutrients lost in processing, would not be affected by regulations involving DV revisions.
Identification of fortified foods in WWEIA, NHANES 2007–2008.
The USDA Food and Nutrient Database for Dietary Studies (FNDDS) version 4.1 provides nutrient values per 100 g of foods reported by WWEIA, NHANES 2007–2008, respondents along with descriptive information (19), but there is no indicator variable for fortified foods in the FNDDS database. Therefore, a food was considered to be fortified if it had “fortified” or “added” nutrients in the FNDDS food description or in an ingredient name. A food also was considered to be fortified if the USDA nutrient file indicated that the food contained added synthetic folic acid or, for a plant-based food, if the USDA nutrient file indicated that it contained retinol (vitamin A). A ready-to-eat or cooked cereal was considered to be fortified if ≥1 nutrients were flagged as being added for that product in the USDA Standard Reference File 22, the source of nutrient data used to process WWEIA, NHANES 2007–2008 (20). Product labels were used to identify fortification nutrients when food descriptions and ingredient names did not specify which nutrients were added.
Quantification of current %DVs for fortification nutrients.
For each food (or ingredient in a mixture) identified as a fortified food, the concentration of each fortification nutrient per 100 g of the food (or ingredient in a mixture) as reported in FNDDS 4.1 was converted to a %DV by dividing the total amount of the nutrient in the food by the nutrient DV as specified in Table 2. This approach was also followed when the food was a composite of similar fortified and unfortified foods (e.g., apple juice). The %DV values for fortified foods therefore reflected nutrient contributions from both the fortification and intrinsic (naturally occurring) sources in the food, which is consistent with label nutrient declarations. We did not attempt to quantify levels of fortified versus intrinsic nutrients in each fortified food. In this analysis we assumed that the revised DV for folate will be in terms of micrograms of Dietary Folate Equivalents rather than micrograms of total folate, the current DV unit. This assumption was made to align units used in the revised DVs with units used in the underlying DRIs.
Calculation of adjusted vitamin and mineral levels in fortified foods.
Two of the 4 potential methods for calculating DVs were assessed in this study, with the DVs corresponding to the population-weighted EAR (model 1) or the population-coverage RDA (model 2). These 2 scenarios were chosen because they represent the lowest and highest values among the 4 approaches put forth for calculating DVs from DRIs. In both modeling scenarios, levels of fortified vitamins and minerals were adjusted to maintain the current %DVs in fortified foods, keeping levels of other nutrients constant. We assumed that all nutrient adjustments could be made by removing or adding fortification nutrients, with no change to levels of intrinsic nutrients in the fortified food. In the case of vitamin D, which has maximum allowable levels of addition in foods (21–23), the amount of nutrient needed to maintain the current %DV was capped at the U.S. regulatory maximum level in the scenario requiring addition of vitamin D. Maximum allowable levels of folic acid under U.S. regulations for voluntary fortification also have been specified (24), although the modeling scenarios in this analysis did not require amounts of folic acid to increase above current levels.
Analysis.
To understand the role of fortified foods in the diet corresponding to current DVs in this analysis, proportions of fortification nutrient intakes from fortified foods were estimated based on day 1 food intake data. Dietary intakes from fortification nutrients were estimated for the population aged ≥4 y; these intakes were then divided by dietary intakes from all food sources to derive population-based estimates of the proportions of nutrient intakes from fortified foods (25).
Usual dietary intakes were estimated based on the nutrient data as reported (current DV scenario) and under the 2 modeling scenarios. Usual dietary intake estimates were generated by using Software for Intake Distribution Estimation for the Windows Operating System (PC-SIDE, version 1.0, 2003; Department of Statistics, Iowa State University), which accounted for inter- and intraindividual variations in intake (26, 27). The estimates were generated with day 1 nutrient intakes from the total sample population and with day 2 responses from the subsample that completed a second dietary recall. Estimated intakes included usual dietary intakes (±SEM) and percentiles of intake (10th, 25th, 50th, 75th, 90th) for the total population aged ≥4 y, adults aged ≥19 y (males and females separately and combined), and 13 life-stage and gender subpopulations including children aged 4–8 y and for males and females separately for ages 9–13, 14–18, 19–30, 31–50, 51–70, and ≥71 y. Intakes were estimated for the life-stage and gender groups to determine if unique concerns existed within subsets of the U.S. population.
PC-SIDE software was used to estimate the percentage of each population with usual nutrient intakes below the EAR, a measure of inadequate intakes, based on the cut-point method for all nutrients except for iron. The percentage of the population with usual intakes below the EAR for iron was estimated by using the probability method (28, 29). PC-SIDE software also was used to estimate the percentage of each population with usual nutrient intakes above the Tolerable Upper Intake Level (UL) for nutrients with relevant ULs. The UL represents the highest average daily intake of a nutrient likely to pose virtually no risk of adverse health effects in a population (1). In cases in which a subpopulation included multiple age groups with different EARs or ULs for a nutrient, a combined percentage below the EAR or above the UL was calculated by weighting percentage values for specific age groups based on population sizes. A weighted SEM for each percentage below the EAR or above the UL was calculated as the unadjusted SEM for the combined population multiplied by the maximum design effect based on SEMs for the subpopulations included.
The reference weight used in all analyses was the day 1 dietary weight (WTDRD1). Jackknife weights (JK-2) were created by using Stata, version 12 (StataCorp LP).
Results
Vitamin and mineral intakes from fortified foods.
Of a total of ~4500 foods reported as consumed by the population aged ≥4 y in WWEIA, NHANES 2007–2008, 266 foods (~6%) were identified as fortified foods containing ≥1 of the 8 added nutrients of interest. The specific vitamins and minerals added to foods varied by product type (Supplemental Table 1).
Usual intakes of vitamins and minerals are shown in Table 3. The proportion of intake provided by fortified foods (based on unadjusted day 1 data) indicates that fortified foods accounted for 8–28% of dietary intakes of the individual nutrients from food on the day of recall (Table 3).
TABLE 3.
Usual dietary intake of select vitamins and minerals by the U.S. population aged ≥4 y based on current fortification of the food supply and modeled assuming constant %DVs in fortified foods under 2 potential DV scenarios1
| Usual intakes |
||||||||||
| Percentiles of intake |
||||||||||
| Nutrient and DV scenario | Intake from fortified foods2 | Usual intake3 | 10th | 25th | 50th | 75th | 90th | DV used in modeling | Below the EAR4 | Above the UL5 |
| % | % | % | ||||||||
| Vitamin A, μg RAE/d | ||||||||||
| Current | 17 | 610 ± 16.1 | 303 | 412 | 562 | 745 | 962 | 1500 RE | 44 ± 2.2 | <1 |
| Model 1 | 542 ± 14.8 | 279 | 372 | 499 | 657 | 843 | 531 RAE | 54 ± 2.3 | <1 | |
| Model 2 | 568 ± 15.2 | 290 | 389 | 524 | 690 | 888 | 900 RAE | 49 ± 3.9 | <1 | |
| Vitamin D, μg/d | ||||||||||
| Current | 12 | 4.5 ± 0.20 | 1.7 | 2.6 | 4.0 | 5.8 | 7.9 | 10 μg | 96 ± 0.9 | <1 |
| Model 1 | 4.5 ± 0.20 | 1.7 | 2.6 | 4.0 | 5.8 | 7.9 | 10 μg | 96 ± 0.8 | <1 | |
| Model 2 | 4.9 ± 0.12 | 1.8 | 2.8 | 4.4 | 6.4 | 8.6 | 20 μg | 95 ± 0.9 | <1 | |
| Vitamin E, mg AT/d | ||||||||||
| Current | 8 | 7.3 ± 0.20 | 4.0 | 5.1 | 6.7 | 8.8 | 11 | 30 IU | 90 ± 1.7 | <1 |
| Model 1 | 7.2 ± 0.20 | 4.0 | 5.1 | 6.6 | 8.6 | 11 | 11 mg AT | 91 ± 1.6 | <1 | |
| Model 2 | 7.3 ± 0.20 | 4.0 | 5.2 | 6.8 | 8.9 | 11 | 15 mg AT | 89 ± 1.7 | <1 | |
| Vitamin C, mg/d | ||||||||||
| Current | 28 | 83 ± 3.7 | 31 | 47 | 72 | 108 | 149 | 60 mg | 39 ± 2.0 | <1 |
| Model 1 | 83 ± 3.7 | 31 | 47 | 72 | 108 | 150 | 61 mg | 39 ± 2.0 | <1 | |
| Model 2 | 94 ± 4.3 | 34 | 52 | 81 | 123 | 174 | 90 mg | 34 ± 1.9 | <1 | |
| Vitamin B-12, μg/d | ||||||||||
| Current | 20 | 5.26 ± 0.289 | 2.70 | 3.60 | 4.80 | 6.30 | 8.30 | 6 μg | 2 ± 0.5 | ND |
| Model 1 | 4.61 ± 0.255 | 2.48 | 3.18 | 4.14 | 5.45 | 7.18 | 1.9 μg | 3 ± 0.6 | ND | |
| Model 2 | 4.62 ± 0.122 | 2.50 | 3.20 | 4.20 | 5.50 | 7.10 | 2.4 μg | 3 ± 0.5 | ND | |
| Folate, μg DFE/d | ||||||||||
| Current | 23 | 531 ± 10.6 | 317 | 395 | 501 | 632 | 783 | 400 μg | 9 ± 1.0 | 2 ± 0.8 |
| Model 1 | 465 ± 8.6 | 293 | 359 | 446 | 550 | 662 | 304 μg DFE | 14 ± 1.3 | <1 | |
| Model 2 | 483 ± 9.3 | 301 | 370 | 461 | 571 | 691 | 400 μg DFE | 12 ± 1.2 | <1 | |
| Calcium, mg/d | ||||||||||
| Current | 9 | 944 ± 21 | 544 | 693 | 892 | 1136 | 1408 | 1000 mg | 48 ± 1.9 | <1 |
| Model 1 | 934 ± 21 | 539 | 686 | 882 | 1123 | 1391 | 885 mg | 49 ± 1.9 | <1 | |
| Model 2 | 969 ± 21 | 552 | 706 | 913 | 1165 | 1449 | 1300 mg | 46 ± 1.9 | <1 | |
| Iron, mg/d | ||||||||||
| Current | 21 | 14.9 ± 0.27 | 9.20 | 11.3 | 14.1 | 17.6 | 21.5 | 18 mg | 5 ± — | <1 |
| Model 1 | 12.8 ± 0.18 | 8.30 | 10.0 | 12.3 | 15.0 | 17.9 | 6 mg | 7 ± — | <1 | |
| Model 2 | 14.9 ± 0.27 | 9.20 | 11.3 | 14.1 | 17.6 | 21.5 | 18 mg | 5 ± — | <1 | |
Data source: What We Eat in America, NHANES 2007–2008 (17); n = 7976. Potential DV scenarios: in model 1, the DV corresponds to the population-weighted EAR, and in model 2, the DV corresponds to the population-coverage RDA; in each scenario, levels of fortified nutrients were adjusted to maintain the current %DV. Usual mean intakes, usual percentiles of intake, and proportions below the EAR or above the UL were estimated from PC-SIDE (Department of Statistics, Iowa State University) with jackknife weights; covariates included day of recall and weekend/weekday day. AT, α-tocopherol; DFE, dietary folate equivalent; DV, Daily Value; EAR, Estimated Average Requirement; ND, not determinable; PC-SIDE, Software for Intake Distribution Estimation for the Windows Operating System; RAE, retinol activity equivalent; RE, retinol equivalent; UL, Tolerable Upper Intake Level; —, SEM not calculated.
Percentages of nutrients from fortified foods were estimated from nutrient intakes reported on day 1.
Values are means ± SEMs.
Values are percentages ± SEMs.
The UL for vitamin A was based on retinol; ULs for vitamin E and folate apply to synthetic forms; the UL for vitamin B-12 was not determinable due to a lack of data of adverse effects and concern with regard to lack of ability to handle excess amounts.
Vitamin and mineral intakes in the current vs. potential DV scenarios.
Estimates of usual dietary intakes (adjusted for intra- and interindividual intakes) were calculated from data as reported for the U.S. population aged ≥4 y in WWEIA, NHANES 2007–2008 (current DV scenario), and for intakes under the 2 potential DV scenarios (Table 3).
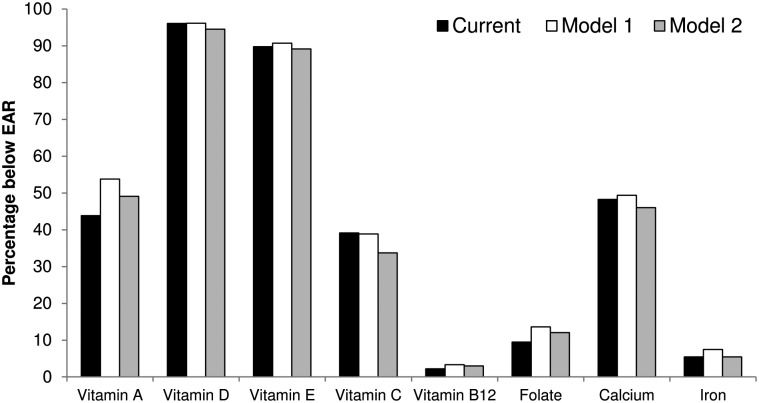
In model 1 (population-weighted EAR), reductions were observed in hypothetical intakes of vitamin A and folate. These reductions were accompanied by increases in the percentages of the population with usual intakes below the EAR for vitamin A (from 44% to 54%) and folate (from 9% to 14%) (Table 3, Fig. 1). For the remaining 6 nutrients, the difference between model 1 and the current scenario in the percentage of the population with intakes below the EAR ranged from 0% to 2%.
FIGURE 1.
Percentage of U.S. population aged ≥4 y with dietary intakes below the EAR based on current intakes and assuming constant %DVs in fortified foods under 2 potential DV scenarios (data from WWEIA, NHANES 2007–2008; n = 7976). Potential DV scenarios: in model 1, the DV corresponds to the population-weighted EAR, and in model 2, the DV corresponds to the population-coverage RDA; in each scenario, levels of fortified nutrients were adjusted to maintain the current %DV. We assumed that the revised DV for folate will be in terms of micrograms DFE. Usual proportions below the EAR were estimated from PC-SIDE (Department of Statistics, Iowa State University) with jackknife weights; covariates included day of recall and weekend/weekday day. For iron, usual proportions below the EAR were estimated by using the probability approach. DFE, Dietary Folate Equivalent; DV, Daily Value; EAR, Estimated Average Requirement; PC-SIDE, Software for Intake Distribution Estimation for the Windows Operating System; WWEIA, What We Eat in America.
In model 2 (population-coverage RDA), the hypothetical lower usual dietary intake of vitamin A was accompanied by an increase in the percentage of the population with an intake below the EAR, from the current 44% to 49% (Table 3, Fig. 1). The hypothetical increased usual dietary intake of vitamin C in model 2 corresponded to a decrease in the percentage of the population with an intake below the EAR, from 39% to 34%, whereas the percentage of the population with folate intake below the EAR increased from 9% to 12%. The modeled percentages of the population with intakes below the EAR under model 2 of iron, calcium, and vitamins D, E, and B-12 were within 2 points of values calculated by using the current DV.
Vitamin and mineral intakes in model 1 vs. model 2.
Assuming that food manufacturers continued to fortify foods at the same %DV and that food consumption patterns did not change, hypothetical nutrient intakes under model 1 (population-weighted EAR) versus model 2 (population-coverage RDA) resulted in an additional 5% of the population with usual nutrient intakes below the EAR for vitamin A (54% vs. 49%) and vitamin C (39% vs. 34%) (Table 3, Fig. 1). Under model 1, an additional 3% of the population aged ≥4 y was estimated to have usual intakes of calcium below the EAR (49% vs. 46%), and an additional 1–2% of the population had usual intakes of vitamins D and E, folate, and iron below the EAR as compared with percentages below the EAR under model 2.
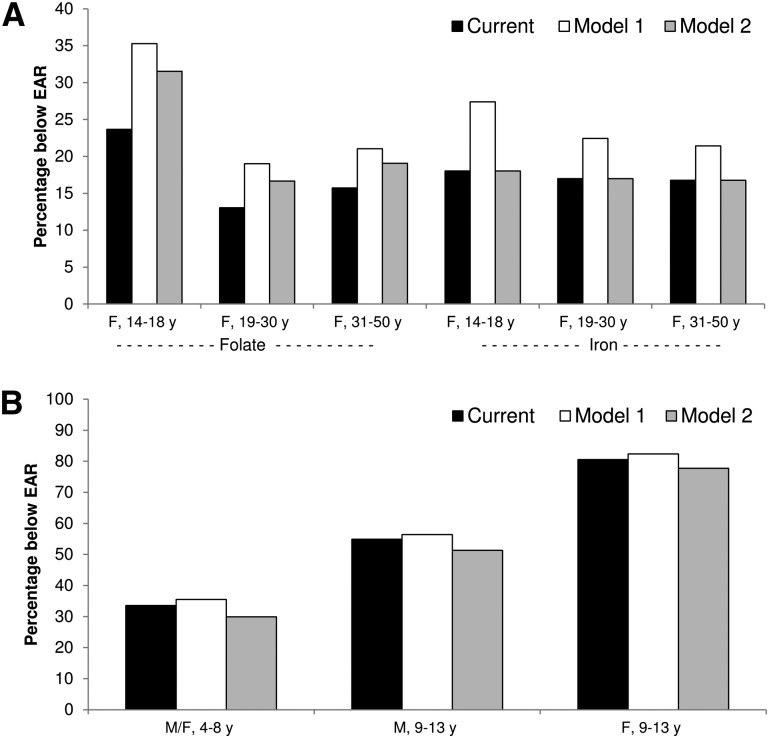
The percentage of additional individuals with usual nutrient intakes below the EAR in model 1 versus model 2 was up to 9% for iron and 3% for folate among subpopulations of women of childbearing age (Fig. 2A). Across subpopulations of children (4–13 y), the percentage of additional individuals with calcium intakes below the EAR in model 1 versus model 2 was up to 6% (Fig. 2B). Results for each nutrient and each subpopulation are shown in Supplemental Figs. 1–8.
FIGURE 2.
Percentage of females aged 14–50 y with dietary folate and iron intakes (A) and children aged 4–13 y with dietary calcium intakes (B) below the EAR based on current intakes and assuming constant %DVs in fortified foods under 2 potential DV scenarios (data from WWEIA, NHANES 2007–2008; n = 7976). Potential DV scenarios: in model 1, the DV corresponds to the population-weighted EAR, and in model 2, the DV corresponds to the population-coverage RDA; in each scenario, levels of fortified nutrients were adjusted to maintain the current %DV. We assumed that the revised DV for folate will be in terms of micrograms DFE. Usual proportions below the EAR were estimated from PC-SIDE (Department of Statistics, Iowa State University) with jackknife weights; covariates included day of recall and weekend/weekday day. For iron, usual proportions below the EAR were estimated by using the probability approach. DFE, Dietary Folate Equivalent; DV, Daily Value; EAR, Estimated Average Requirement; PC-SIDE, Software for Intake Distribution Estimation for the Windows Operating System; WWEIA, What We Eat in America.
Upper levels of nutrient intake.
Although the DVs for vitamins D and C and calcium increased above current values in 1 or both models, the proportions of the population aged ≥4 y with intakes above the UL remained very low (<1%) (Table 3).
Discussion
Fortified foods play an important role in contributing to nutrient intakes of the U.S. population (11–13). Dietary guidance in the United States encourages consumption of a nutrient-dense diet to meet nutritional needs, but it recognizes that fortified foods can help to meet nutrient gaps for some individuals (14, 30). At the same time, care must be taken to deliver sufficient levels of nutrients without exceeding the ULs (1).
Revisions to the DVs used as the basis for nutrition labeling could have an impact on the levels of nutrients that food manufacturers choose to add to foods. It is possible that manufacturers could choose to add the same absolute amounts of nutrients and revise product labels to reflect new %DVs. However, it is highly likely that food manufacturers will tailor the amount of added nutrients in foods to be consistent with the current %DV and label claims as we assumed in this modeling exercise. Changes in the amounts of fortification nutrients added to food could affect intakes of critical nutrients by the U.S. population, including vulnerable subpopulations such as women of childbearing age and children.
If manufacturers continue to fortify foods to the same %DV for each nutrient, the extent to which potential changes in DVs would affect nutrient intake adequacy depends on the proportion of nutrient intakes derived from fortified foods and the magnitude and direction of change in the DV. In this analysis, fortified foods accounted for 17–28% of total intakes of folate, iron, and vitamins A, B-12, and C and 8–12% of calcium and vitamins D and E.
It was assumed in our modeling exercise that manufacturers would choose to reformulate fortification levels (either up or down) and maintain current label claims such as the %DV, nutrient content claims (e.g., “good” or “excellent” source of a nutrient), and health claims. This assumption may or may not be valid, and the opposite response by food manufacturers to maintain current fortification practices and revise the %DV as necessary may also be possible, or they may choose to maintain only select fortification levels.
Overall, assuming that food manufacturers continue to fortify foods at the same %DV and that food consumption patterns are unchanged, under the 2 potential DVs considered in this modeling exercise, the percentage of the U.S. population aged ≥4 y with intakes below the EAR would increase ≤2 percentage points above the percentage calculated by using the current DV for 5 of the 8 nutrients examined (vitamins D, E, and B-12; calcium; iron). Additionally, results from this modeling study show that for 5 of the 8 nutrients (vitamins D, E, and B-12; folate; iron), differences in the proportion of the total population with usual intakes less than the EAR would be ≤2%, regardless of whether the basis for the revised DV is the population-weighted EARs or the population-coverage RDAs. However, it must be noted that for each percentage change in nutrient intakes below the EAR in the total population, ∼3 million individuals would be affected (10).
Potential differences in nutrient adequacy of ≥3 percentage points were observed in some subpopulations. For iron and folate, 2 nutrients of concern for women of childbearing age, the use of the population-weighted EAR rather than the population-coverage RDA or current DV could exacerbate inadequacy of intake of these nutrients. Vitamin A was identified as a shortfall nutrient (although intakes are not currently in the category “of concern”) for the U.S. population; however, the public health significance of the potential greater declines in adequacy of intake observed assuming a DV based on the population-weighted EAR warrants consideration. The use of the population-coverage RDA rather than the population-weighted EAR could result in lower rates of calcium and vitamin C inadequacy in the total population. No increased risk of excessive nutrient intakes was observed under the potential revisions to DVs considered in this study; however, the use of dietary supplements would also need to be considered when addressing the issue of high intakes.
It is important to note that DVs based on the DRIs rather than the 1968 RDAs will result in new and considerably different values for many nutrients, regardless of which approach is used to calculate the new DVs. The ramifications of using the EAR versus the RDA values for calculating DVs are many and extend beyond the objective of this assessment, namely to model the impact of revised DVs on adequacy of nutrient intake assuming that manufacturers adjust nutrient fortification levels to maintain current %DVs. For example, whatever the DV is, nutrition educators will undoubtedly recommend that individuals select foods to meet the individual’s nutrient needs for most nutrients, and not to exceed them for others, such as sodium. By definition, the use of the EAR to calculate a DV produces a value representing a 50% probability of nutritional inadequacy in the population, whereas the use of the RDA to calculate a DV produces a value representing a 2–3% probability of nutritional inadequacy. Although the DV does not define a recommended nutrient intake level for an individual, it may be interpreted as such, and if the DV for a nutrient decreases compared with the current DV, consumers may falsely assume that their dietary choices account for a greater percentage of daily needs even though the absolute amount of the nutrient in the food is unchanged. In deciding which approach to use to calculate revised DVs, it will be critical to consider many issues, including impacts on nutrition education and consumer behavior in addition to the hypothetical estimates of nutrient intakes and adequacy of intake that are the subject of this analysis.
There are several strengths to this analysis. The USDA nutrient databases used in this analysis provide the foundation for most nutrition policy research in the United States (31). The estimates are based on a nationally representative sample of the U.S. population and reflect the USDA’s assumptions about voluntary vitamin and mineral fortification of the recent food supply. Multiple strategies were used to identify fortified foods consumed by the population. Estimates of intake were developed by using statistical models to account for within-individual variation in intake; thus, the estimates are representative of usual intakes. Some limitations of the analysis also must be considered. Dietary intakes of the U.S. population were based on 24-h dietary recalls and consequently are subject to misreporting (32). This analysis did not account for potential revisions to enrichment or Standard of Identity practices that may occur in response to DV revisions. Additionally, nutrient intakes modeled in this study reflect fortification of the food supply as captured by the USDA’s food coding system for the period 2007–2008; the foods in this database do not account for every fortified food in the marketplace, the foods may not reflect current fortification practices, and the strategies used to identify fortified foods may not have identified all relevant foods. Nutrient levels in fortified foods were adjusted assuming that levels could increase or decrease with no technical or sensory limitations. Statistical significance testing was not conducted.
Results of this modeling exercise will help to inform decisions about the most appropriate %DV to be listed on the Nutrition Facts panel, although additional factors must be considered. This exercise modeled adequacy of dietary intakes, not nutritional status, and may not reflect the true public health significance of DV changes. It was assumed that food manufacturers would continue to fortify foods at the same %DV per serving and that serving sizes will remain the same, but manufacturers could instead choose to fortify foods with the same absolute nutrient amounts; in that case, if there were no changes in consumption patterns, there would be no changes in nutrient intake adequacy. Additionally, it will be critical to also consider issues of nutrition education and potential consumer behavior in light of potentially substantial changes to DV values.
In conclusion, results from this modeling exercise of potential revisions to DVs show that the impact on adequacy of nutrient intakes under the 2 potential DV models considered is within 2 percentage points of the percentage calculated by using the current DV for 5 of the 8 nutrients examined (vitamins D, E, and B-12; calcium; iron). In these models it was assumed that manufacturers continued to fortify foods at the same %DV and that food consumption patterns were unchanged. For most nutrients, estimates of the percentage of the total population with intakes below the EAR were similar regardless of whether the DV corresponds to the population-weighted EAR or the population-coverage RDA. Potential decreases were observed in adequacy of iron and folate intakes among women of childbearing age (up to 9% and 3%, respectively), adequacy of calcium among children (up to 6%), and adequacy of vitamin A intakes in the total population (5%) assuming use of the population-weighted EAR compared with the population-coverage RDA for setting the DV. It is hoped that the results of this modeling exercise will help to inform decisions in revising the DVs.
Supplementary Material
Acknowledgments
The authors thank Xiaoyu Bi for her assistance in organizing the data output. M.M.M., J.H.S., R.L.B., and J.T.D. contributed to the concept development and critically reviewed and revised the manuscript; M.M.M. and J.H.S. developed the overall research plan, analyzed data, and wrote the manuscript; and L.M.B. contributed to the statistical design. All authors read and approved the final manuscript.
Footnotes
Abbreviations used: DV, Daily Value; EAR, Estimated Average Requirement; FNDDS, Food and Nutrient Database for Dietary Studies; IOM, Institute of Medicine; PC-SIDE, Software for Intake Distribution Estimation for the Windows Operating System; WWEIA, What We Eat in America.
Literature Cited
- 1.Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes: the essential guide to nutrient requirements. Washington: The National Academies Press; 2006. [Google Scholar]
- 2.U.S. Food and Drug Administration; U.S. Department of Health and Human Services. Food labeling: revision of reference values and mandatory nutrients Fed Regist. 2007;72:62149–75. [Google Scholar]
- 3.Institute of Medicine Food and Nutrition Board. Guiding principles for nutrition labeling and fortification. Washington: The National Academies Press; 2003. [Google Scholar]
- 4.Food and Nutrition Board. Recommended Dietary Allowances. 7th. ed. Washington: National Academy Press; 1968. [Google Scholar]
- 5.Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes for calcium and vitamin D. Washington: The National Academies Press; 2011. [Google Scholar]
- 6.Murphy SP, Barr SI. Recommended Dietary Allowances should be used to set Daily Values for nutrition labeling. Am J Clin Nutr. 2006;83 Suppl:1223S–7S. [DOI] [PubMed] [Google Scholar]
- 7.Yates AA. Which dietary reference intake is best suited to serve as the basis for nutrition labeling for daily values? J Nutr. 2006;136:2457–62. [DOI] [PubMed] [Google Scholar]
- 8.Beaton GH. When is an individual an individual versus a member of a group? An issue in the application of the dietary reference intakes. Nutr Rev. 2006;64:211–25. [DOI] [PubMed] [Google Scholar]
- 9.Tarasuk V. Use of population-weighted Estimated Average Requirements as a basis for Daily Values on food labels. Am J Clin Nutr. 2006;83 Suppl:1217S–22S. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Census Bureau. 2005. Middle series data from annual projections of the resident population by age, sex, race, and Hispanic origin: lowest, middle, highest, and zero international migration series, 1999 to 2100 (NP-D1-A). Washington: Department of Commerce; 2000 [cited 2012 Jun 16]. Available from: http://www.census.gov/population/www/projections/natdet-D1A.html.
- 11.Berner LA, Clydesdale FM, Douglass JS. Fortification contributed greatly to vitamin and mineral intakes in the United States, 1989–1991. J Nutr. 2001;131:2177–83. [DOI] [PubMed] [Google Scholar]
- 12.Fulgoni VL III, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: where do Americans get their nutrients? J Nutr. 2011;141:1847–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yetley EA, Rader JI. Modeling the level of fortification and post-fortification assessments: U.S. experience. Nutr Rev. 2004;62:S50–9; discussion S60–1. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary guidelines for Americans. 7th ed. Washington: U.S. Government Printing Office; 2010. [Google Scholar]
- 15.U.S. Department of Agriculture; U.S. Department of Health and Human Services. Food labeling, 21 C.F.R. Sect. 101 (2012).
- 16.U.S. Department of Agriculture; U.S. Department of Health and Human Services. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010. Washington: U.S. Government Printing Office; 2010. [Google Scholar]
- 17.Centers for Disease Control and Prevention; National Center for Health Statistics. National Health and Nutrition Examination Survey data 2007–2008. Hyattsville (MD): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2010 [cited 2012 Jun 6]. Available from: http://wwwn.cdc.gov/nchs/nhanes/search/nhanes07_08.aspx.
- 18.Centers for Disease Control and Prevention; National Center for Health Statistics. NCHS Research Ethics Review Board (ERB) approval. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention [cited 2013 Feb 27]. Available from: http://www.cdc.gov/nchs/nhanes/irba98.htm.
- 19.U.S. Department of Agriculture. USDA Food and Nutrient Database for Dietary Studies, 4.1. Beltsville (MD): Agricultural Research Service, Food Surveys Research Group; 2010 [cited 2012 Jun 6]. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=20511.
- 20.U.S. Department of Agriculture; Agricultural Research Service. USDA National Nutrient Database for Standard Reference, release 22. Beltsville (MD): Nutrient Data Laboratory; 2009 [cited 2012 Jun 6]. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=20960.
- 21.U.S. Food and Drug Administration; U.S. Department of Health and Human Services. Food additives permitted for direct addition to food for human consumption: vitamin D2, 21 C.F.R. Sect. 172.379 (2012).
- 22.U.S. Food and Drug Administration; U.S. Department of Health and Human Services. Food additives permitted for direct addition to food for human consumption: vitamin D3, 21 C.F.R. Sect. 172.380 (2012).
- 23.U.S. Food and Drug Administration; U.S. Department of Health and Human Services. Direct food substances affirmed as Generally Recognized As Safe: vitamin D, 21 C.F.R. Sect.184.1950 (2012).
- 24.U.S. Food and Drug Administration; U.S. Department of Health and Human Services. Food additives permitted for direct addition to food for human consumption: folic acid, 21 C.F.R. Sect. 172.345 (2012).
- 25.Krebs-Smith SM, Kott PS, Guenther PM. Mean proportion and population proportion: two answers to the same question? J Am Diet Assoc. 1989;89:671–6. [PubMed] [Google Scholar]
- 26.Dodd K. A user's guide to C-SIDE: software for intake distribution estimation version 1.0. Ames (IA): Center for Agriculture and Rural Development (CARD), Iowa State University; 1996. [Google Scholar]
- 27.Guenther PM, Kott PS, Carriquiry AL. Development of an approach for estimating usual nutrient intake distributions at the population level. J Nutr. 1997;127:1106–12. [DOI] [PubMed] [Google Scholar]
- 28.Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes: applications in dietary assessment. Washington: The National Academies Press; 2000. [Google Scholar]
- 29.Moshfegh A, Goldman J, Cleveland L. What We Eat in America, NHANES 2001–2002: usual nutrient intakes from food compared to dietary reference intakes. U.S. Department of Agriculture, Agricultural Research Service; 2005 [cited 2012 Sep 10]. Available from: http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/0102/usualintaketables2001–02.pdf.
- 30.Britten P, Cleveland LE, Koegel KL, Kuczynski KJ, Nickols-Richardson SM. Updated US Department of Agriculture food patterns meet goals of the 2010 dietary guidelines. J Acad Nutr Diet. 2012;112:1648–55. [DOI] [PubMed] [Google Scholar]
- 31.Ahuja JK, Moshfegh AJ, Holden JM, Harris E. USDA food and nutrient databases provide the infrastructure for food and nutrition research, policy, and practice. J Nutr. 2013;143 Suppl:241S–9S. [DOI] [PubMed] [Google Scholar]
- 32.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, et al. The US Department of Agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.