Abstract
Isolated fractures of the carpal hamate are rare. We describe a case of 28-year-old male patient who sustained a rare pattern of wrist injury: combined intraarticular fracture of the body and the hook of hamate in the non-dominant left hand. The patient was treated with percutaneous pinning of the fracture of hamate body.
Keywords: Hook of hamate, Body of hamate, Percutaneous pinning
Introduction
Fractures of the carpal hamate are rare injuries. These are estimated to occur in 2 % - 4 % of all carpal bone fractures [1, 2]. Milch (1934) reported a case of the fracture of body of the hamate along with a fracture of ulnar styloid [3]. He suggested that these fractures can be divided into two types: those involving the body, and others involving the hook of the hamate.
Most of these fractures occur in association with additional injuries to the wrist, especially scaphoid and distal forearm [3–7]. Isolated hamate fractures are very rare and only a few cases have been reported in English-medical literature [2, 4]. Double fractures of the body and the hook of the hamate in isolation are even rarer and only one such case has been reported till date [2]. We present a case of an adult male who sustained intraarticular fracture of the body of hamate along with ipsilateral fracture of the hook of hamate. The uniqueness of the case lies in the fact that the hook as well as the body of hamate have failed under abnormal loading and the patient was treated with percutaneous pinning of the fracture of hamate body. The hook fracture was treated by nonoperative cast immobilization.
Case Report
A 28-year-old man, right handed male fashion designer, presented to the orthopaedic emergency with a history of fall from a motorbike following a sudden jerk as it collided with a large stone on the road and the force was transmitted onto the ulnar aspect of wrist. He presented about 3 h after sustaining the trauma and complained of pain and swelling of the left wrist. Tenderness was present over medial aspect of the involved wrist around 2 cm distal to the ulnar styloid. The postero-anterior, lateral and 30° semi-pronated oblique radiographs of the involved wrist revealed a displaced intraarticular fracture of the body of hamate with a gap displacement of 2 mm along with ulnar carpometacarpal joint subluxation (Fig. 1a). The fracture line was observed to traverse the body of hamate in an oblique direction, medial to the hook of hamate. The carpal tunnel view of the involved wrist was ordered which showed a doubtful, minimally displaced fracture of the hook of hamate from its base (Fig. 1b). Fine cut multidetector noncontrast computed tomography (NCCT) was performed which confirmed the radiographic findings of combined intraarticular fracture of the hamate body and a transverse fracture of the base of the hook (Fig. 1c).
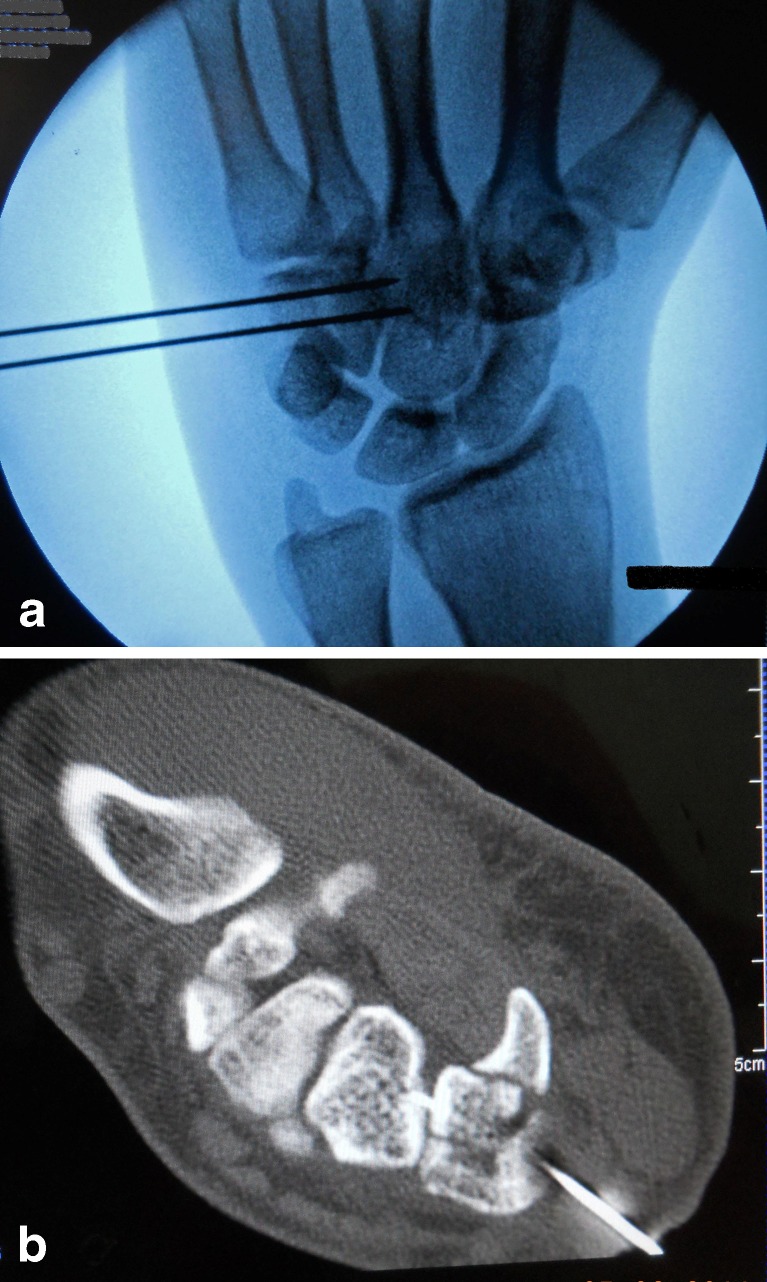
Fig. 1.
a: Postero-anterior radiograph of the left wrist showing a fracture through the body of hamate (with gap displacement 2 mm). b: Carpal tunnel view of the left wrist showing minimally displaced fracture of the hook of hamate. c: Axial section of NCCT scan through the distal carpal row showing ipsilateral fractures of the body and the hook of hamate
Fracture fixation of body of hamate, with percutaneous pinning under image intensifier guidance, was planned. A closed reduction was performed under anaesthesia with digital pressure over the ulnar aspect of hamate and two parallel 0.045-in. Kirschner wires were passed across the fracture in the body of hamate transfixing the capitate (Fig. 2a). An ulnar gutter slab in slight dorsiflexion was applied post-operatively. A fine cut NCCT was repeated, which revealed an acceptable reduction of the body of hamate and proper positioning of the wires (Fig. 2b). No further displacement of the fracture of hook of hamate was noticed. The slab was maintained for 6 weeks, after which the patient was started on grip strengthening exercises. The patient resumed his regular work at 2 weeks and the wires were removed at 8 weeks following fixation. At 12 months follow-up, the fracture of the body of hamate healed uneventfully (Fig. 3a), however, the fracture of hook of hamate resulted in nonunion (Fig. 3b). He had no pain and grip strength was 90 % of the dominant right side. He had full range of flexion, extension, radial and ulnar deviation as compared to the opposite wrist. The Mayo wrist score was 90 (excellent). The patient is being followed up on 8 weekly intervals as an outpatient.
Fig. 2.
a: Two parallel 1.2 mm Kirschner wires are being passed under C-arm image intensifier guidance through the fracture of body of hamate transfixing the capitate. b: Post-operative axial section of NCCT scan through the distal carpal row showing acceptable reduction of the fracture of the body of hamate and proper positioned wire. No further displacement of the hook of hamate was noticed
Fig. 3.
a: Follow-up postero-anterior radiograph of the left wrist showing maintained joint spaces and the evidence of fracture healing. b: Follow-up axial section of NCCT scan revealing nonunion of the fracture hook of hamate
A written, informed consent was obtained from the patient authorising the treatment, radiological and photographic documentation. He was also informed that the data concerning the case would be submitted for publication and he consented.
Discussion
The fractures of the hamate continue to pose diagnostic and therapeutic challenges for the treating orthopaedic surgeons. The bone is roughly like the shape of a triangle which is located in the medial aspect of the distal carpal row. It articulates with the triquetrum proximally, and base of 4th and 5th metacarpals distally. The fractures of the body of hamate are unstable owing to the pull of extensor carpi ulnaris, flexor carpi ulnaris, and the hypothenar muscles [4]. Therefore, it has been suggested that extensor carpi ulnaris tendon and flexor carpi ulnaris tendon are primarily responsible for the proximal and ulnar displacement of the 5th metacarpal base along with the medial fracture fragment of the hamate body. Though articular capsule, volar and dorsal carpometacarpal ligaments, intrinsic interosseous ligaments, and metacarpal interosseous ligaments limit the amount of displacement. Divergent fracture-dislocations of carpo-metacarpal joint are also rare because of these limiting factors [6, 8].
Hamate fractures are frequently missed at the time of presentation because of paucity of signs and symptoms, relative rareness of the injury pattern, and complex carpal anatomy [3, 4, 9, 10]. Ebraheim et al. reported a mean delay of 10 days for the diagnosis from the time of injury [4]. The importance of oblique views of wrist and high resolution CT for early diagnosis has been stressed in the literature [9, 11]. In an in-vitro study, Andresen et al. reported 97.2 % accuracy of high-resolution computed tomography in detecting hamate fractures in sharp contrast to 80.5 % accuracy of x-rays in different projections [11]. They concluded that hamate fractures cannot always be detected with certainty on conventional radiographs taken with different projection planes and HRCT may be considered as the imaging modality of choice for further clarification in the body or the hook of hamate fractures. Nevertheless, high index of suspicion is always required to order these investigations.
Ebraheim et al. reported 11 patients with coronal fracture of the hamate body, of which six were treated with closed reduction and percutaneous pinning and, four with open reduction and internal fixation. Closed reduction and cast immobilization was resorted to in one case [4]. All the patients did well except the one that was treated with closed reduction and casting, in which reduction was lost leading to nonunion and subluxation of hamato-metacarpal joint. Another similar case of nonunion of the body of hamate has also been reported with the casting alone [3].
Combined fractures of the body and the hook of hamate in isolation may be considered as an extremely exceptional radiological finding, and only one case of this injury pattern has been reported in the literature [2]. Kapickis et al. suggested that such combination may be caused by a combination of direct and indirect forces, and such injury pattern may be recognized as a form of ulnar axial injury of the wrist. They treated the patient with open reduction and internal fixation of both the body and the hook of hamate with two screws of 2.3 mm diameter each. However, they reported clawing of ulnar two digits post-operatively which required another 3 months to recover. We suggest that the injury pattern in our patient may be caused by a combination of direct force during the impact, as well as the shearing force applied by extrinsic flexor tendons of the ring and little finger, and traction force to the hook through the attachments of the transverse carpal ligament caused by flattening of the transverse carpal arch. We treated our patient with closed reduction and percutaneous pinning of the hamate body fracture; and the fracture of hook of hamate was treated non-operatively. Care should be taken while placing percutaneous K-wires in the body of hamate as volar misdirected wire may injure the neurovascular bundle in Guyon’s canal. The ulnar nerve injury was avoided in our case by performing the K-wires insertion under strict image intensifier control targeting the body of capitate both in anteroposterior as well as lateral projections and keeping the wires parallel to the hamate-metacarpal joint line(as seen in Fig. 2a).
The options available with us were: (a) operative fixation of both the fractures; (b) fixation of the intraarticular fracture of the body of hamate and nonoperative treatment for the hook of hamate; and (c) closed compression and plaster cast immobilization. We chose the second option since an intraarticular displaced fracture of the body of hamate is inherently unstable which requires operative fixation [4]. The fracture of the hook of hamate, being undisplaced, was treated nonoperatively. The excision of the hook of hamate may always be considered at a later stage in symptomatic cases as it is safer than the procedure of open reduction and internal fixation. The other two options were not considered because of the inherent risk of injury to deep branch of ulnar nerve while fixing the fracture of the hook of hamate and the possibility of slow progressive dislocation of the hamate-matacarpal articulation if the fracture of the body of hamate being treated with plaster cast immobilization alone. The plaster cast treatment has been known to be inadequate in preventing slow and progressive dislocation of the hamate-matacarpal joint.
We report this very unusual case of combined fractures of the body as well as the hook of hamate without other concomitant carpal or distal forearm injuries. The report intends to spread awareness about the hamate fractures and the reported injury pattern. We emphasize that high index of suspicion must be practised to evaluate the patient with ulnar sided wrist pain after trauma and multidetector computed tomography is a useful adjunct to radiographs in such cases.
Footnotes
The manuscript has been read and approved by all the authors and requirement for authorship of this document has been met. Each author certifies that the work and all investigations were conducted in conformity with ethical principles of research. Each author believes that the manuscript represents honest work. They did not receive grants from any commercial entity in support of this work. Each author certifies that he has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Dunn AW. Fractures and dislocations of the carpus. Surg Clin North Am. 1972;52:1513–1538. doi: 10.1016/s0039-6109(16)39895-4. [DOI] [PubMed] [Google Scholar]
- 2.Kapickis M, Looi K-P, Chong AK. Combined fractures of the body and hook of hamate: a form of ulnar axial injury of the wrist. Scand J Plast Reconstr Surg Hand Surg. 2005;39:116–119. doi: 10.1080/02844310410021767. [DOI] [PubMed] [Google Scholar]
- 3.Milch H. Fracture of the hamate bone. J Bone Joint Surg Am. 1934;16:459–462. [Google Scholar]
- 4.Ebraheim NA, Skie MC, Savolaine ER, Jackson WT. Coronal fracture of the body of the hamate. J Trauma. 1995;38(2):169–174. doi: 10.1097/00005373-199502000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Jones BG, Hems TEJ. Simultaneous fracture of the body of the hamate and the distal pole of the scaphoid. J Trauma. 2001;50:568–570. doi: 10.1097/00005373-200103000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Moriya K, Saito H, Takahashi Y, Ohi H. Divergent fracture-dislocation of the hamatometacarpal joint: case report. J Hand Surg. 2011;36(1):47–51. doi: 10.1016/j.jhsa.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 7.Sabat D, Dabas V, Suri T, Wangchuk T, Sural S, Dhal A. Trans-scaphoid, transcapitate, transhamate fracture of the wrist: case report. J Hand Surg. 2010;35A:1093–1096. doi: 10.1016/j.jhsa.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 8.Dillon J, Street J, Mahalingham K. Divergent dislocation of the ring and little finger carpometacarpal joints- a rare injury pattern. Acta Orthop Belgica. 2005;71:353–356. [PubMed] [Google Scholar]
- 9.Borse VH, Hahnel J, Faraj A. Lessons to be learned from a missed case of hamate fracture: a case report. J Orthop Surg Res. 2010;5:64. doi: 10.1186/1749-799X-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murray WT, Meuller PR, Rosenthal DI, Jauernek RR. Fracture of the hook of the hamate. Am J Roentgenol. 1979;133:899–903. doi: 10.2214/ajr.133.5.899. [DOI] [PubMed] [Google Scholar]
- 11.Andresen R, Radmer S, Sparmann M, Bogusch G, Banzer D. Imaging of hamate bone fractures in conventional x-rays and high-resolution computed tomography: an in vitro study. Invest Radiol. 1999;34:46–50. doi: 10.1097/00004424-199901000-00007. [DOI] [PubMed] [Google Scholar]