Abstract
Reactive attachment disorder (RAD) is a psychiatric disorder developing in early or middle childhood as a consequence of significant failures in the caregiving environment. RAD results in children failing to relate socially, either by exhibiting markedly inhibited behaviour or by indiscriminate social behaviour and is associated with significant socio-behavioural problems in the longer term. This study examined RAD in South Africa, a setting with high environmental risks.
We recruited a sub-sample of 40 10-year-old children from a cohort enrolled during pregnancy for whom early attachment status was known. Children were purposefully selected to represent the four attachment categories using the data available on the strange situation procedure (SSP) at 18 months. The Manchester Child Attachment Story Task (MCAST) assessed current attachment and RAD was diagnosed using a standardised assessment package. A high proportion of the children (5/40% or 12.5%) fulfilled diagnostic criteria for RAD; all were boys and were displaying the disinhibited type. SSP classification at 18 months was not significantly associated with RAD symptoms at age of 10 years, while current MCAST classifications were. This suggests that children in this sample are at much higher risk of RAD than in high-income populations, and despite a fairly typical attachment distribution in this population at 18 months, RAD was evidenced in later childhood and associated with current attachment disorganisation.
The strengths of this research include its longitudinal nature and use of diagnostic assessments. Given increasing evidence that RAD is relatively stable over time and introduces longer term socio-behavioural risks; the high rate of RAD in this sample (12.5%) highlights potential developmental threats to children in low- and middle-income countries (LMICs). Our results should be interpreted with caution given sample size and risk of selection bias. Further research is needed to confirm these findings.
Keywords: reactive attachment disorder, LMIC, South Africa, pre-adolescent, diagnostic
Introduction
The quality of early attachment relationships are known to impact on children's later development and mental health. Attachment disorders arise from failure to form normal attachments to primary caregiving figures in early childhood, leading to problematic social relationships and disturbances of relatedness in later childhood (Fearon, Bakermans-Kranenburg, Van IJzendoorn, Lapsley, & Roisman, 2010). Risk for attachment disorders in early childhood has been shown to be linked to parental factors including abuse, neglect, insensitive care, psychological disturbances, depression and substance abuse (Breidenstine, Bailey, Zeanah, & Larrieu, 2011) and child factors including temperament, medical conditions and failure to thrive (Thompson et al., 2010). Further, environmental factors include socio-economic deprivation and poverty, violence and out of home placements (Minnis et al., 2007).
Reactive attachment disorder (RAD) describes difficulties with social relatedness in children (Zeanah & Gleason, 2010). It is considered “extremely rare” (Meltzer & Britain, 2003), with less than 1% prevalence in high-income populations (Skovgaard et al., 2007). Symptoms appear to be stable over time and cause significant morbidity in later childhood (Gleason et al., 2011; Rutter, Kreppner, & Sonuga-Barke, 2009). RAD is characterised by disinhibited (indiscriminately sociable) or inhibited (withdrawn, hyper-vigilant) behaviours (Minnis, Marwick, Arthur, & McLaughlin, 2006). A review of classification criteria for inclusion in the fifth revision of the Diagnostic and Statistical Manual (DSM-V) of the American Psychological Association (APA) (Zeanah & Gleason, 2010) found that in middle childhood, RAD (disinhibited type) manifests in over familiar behaviours, poor social boundaries and higher risk taking, while RAD (inhibited type) manifests in aggression towards self, internalising disorders and a poorly developed sense of conscience (Zeanah & Gleason, 2010).
The diagnosis, aetiology and treatment of RAD in children aged 0–6 years, while still controversial, is becoming clearer as more detailed longitudinal research emerges (Glowinski, 2011). While most research on RAD has focused on early childhood, much less is known about school-aged children (Zeanah & Gleason, 2010). More recently, research has begun to explore RAD in school-aged and older children with examples of both diagnostic (Minnis et al., 2006, 2009) and qualitative research (Bennett, Espie, Duncan, & Minnis, 2009) emerging in the literature. The diagnosis and measurement of RAD in older children is complex (Potter et al., 2009), because as children grow and develop, their psychological world and relationships to primary caregivers become more complicated and challenging to understand, with single behaviours often having multiple explanations. School-aged children exhibit different attachment behaviours and perceive threats differently to younger children as they tackle the developmental task of differentiating themselves from their parent or primary caregiver. Diagnostic specificity in older children also presents challenges as some of the primary diagnostic characteristics of RAD are common features of other disorders such as childhood depression, conduct disorder and attention-deficient disorders (Zeanah & Gleason, 2010). In recent reviews and commentary around revisions to the DSM criteria for RAD (Gleason et al., 2011; Potter et al., 2009; Zeanah & Gleason, 2010), experts caution that there is too little longitudinal evidence to guide diagnostic precision in older children, and that treatment for RAD among children who are inappropriately diagnosed with RAD may have little therapeutic impact and may in fact be harmful (Potter et al., 2009). However, analysis of a community sample of over 6000 twins examining attachment disorders, conduct disorders, hyperactivity and emotional disorders found that attachment disorders could be discriminated from other behavioural and emotional difficulties among school-aged children and were associated with harsh or negative parenting behaviours, environmental and genetic influences (Minnis et al., 2007).
The research that exists on older children has focused mainly on longer term outcomes of previously institutionalised children living in the United States or United Kingdom (Rutter, 2010). In this research, early RAD inhibited patterns has been shown not to persist once secure attachments are formed, while disinhibited patterns, such as the tendency to wander off with strangers may persist for some time after the development of a secure attachment (Potter et al., 2009). Potter and colleagues also note that in older children, disinhibited patterns can be perceived by strangers as physically intrusive and children with these difficulties tend to exhibit a reluctance to request assistance from others, they may lack stranger wariness, may be impulsive and have difficulty with transitions, delaying gratification and with problem solving. These factors could threaten the development of healthy relationships and the fulfilment of human potential. Children with RAD are more likely to have mental health problems in later childhood including conduct disorder, regardless of whether current attachment patterns are organised or disorganised (Gleason et al., 2011). RAD may thus be a useful middle childhood indicator of later risk for psychopathology particularly in high-risk populations.
It is well established that children in low- and middle-income country (LMIC) settings are exposed to multiple risks associated with poverty, HIV, trauma and conflict, which are widely associated with poor mental health and risk behaviours (Earls, Raviola, & Carlson, 2008; Kieling et al., 2011). There is increasing evidence of the loss of developmental potential common to childhood in many LMIC and its implications for later child development (Walker et al., 2011). Calls for investments to be directed to addressing these issues in LMIC have been made (Collins et al., 2011), but research is needed to inform these investments and to better understand the longer term trajectory's and needs of children exposed to early risks and those exposed to chronic risk throughout childhood (Sameroff, 2010). A recent update of the Lancet series on mental health highlights how little is known about mental disorders during the pre-adolescent and adolescent years in LMICs (Patel, Flisher, Nikapota, & Malhotra, 2008; Rohde, 2011). A review of psychopathology in childhood in sub-Saharan Africa found only 10 studies from 6 of a possible 48 countries (Cortina, Sodha, Fazel, & Ramchandani, 2012). Cortina and colleagues' meta-analysis of available data found considerable mental health problems among children and adolescents with 1 in 10 children having a specific psychiatric disorder and with children in areas of greatest deprivation at greatest risk.
While it is clear that risk exists, the specificity with which we understand psychopathology is low, with research using screening measures consistently reporting much higher prevalence's (19.8% as compared to 9.5%) than research using diagnostic assessments (Cortina et al., 2012). Since much of the available psychological research in LMIC measures psychological symptomology among children using screening questionnaires, there is little diagnostic data to inform the appropriate allocation of scarce intervention resources to those who need it. In South Africa, for example, the lack of research evidence on psychopathology among children and adolescents results in policy and implementation planning needing to rely heavily on estimates (Kleintjes et al., 2006). Furthermore, in settings where environmental risk is heightened by epidemics such as HIV, psychological symptoms (such as anxiety or depression) are also frequently attributed to single external risk factors such as parental HIV/AIDS status (Cluver, Orkin, Boyes, Gardner, & Nikelo, 2012) with little attention to relationship disorders or psychopathology which may in fact underlie child behaviour or symptom reporting.
This study aimed to use diagnostic methodology to examine RAD in a small purposely selected sample of children for whom early attachment status was known, and who had been raised in a high-risk environment. The aim of this article was to demonstrate the diagnostic validity of standardised assessments for RAD in this population, to contribute to the lack of longitudinal evidence on the longer term trajectories of children with early attachment difficulties and to establish preliminary estimates of risk for RAD in this high risk LMIC population.
Method
The study was conducted in Khayelitsha, a peri-urban settlement of approximately one million people, on the outskirts on Cape Town, South Africa. Khayelitsha, like many South African township settings, has high levels of violence, with poor infrastructure, vast areas of informal houses (shacks) and high levels of unemployment (Nleya & Thompson, 2009). Childhood in Khayelitsha is characterised by exposure to multiple childhood traumas and adversity (Cluver, Gardner, & Operario, 2009). Previously, Cooper and colleagues recruited a cohort of 147 mother–infant dyads during pregnancy and assessed them at 18 months postnatally (Cooper et al., 1999; Tomlinson, Cooper, & Murray, 2005). Surprisingly, despite known deprivation and inequality, 61.9% of the infants were found to be securely attached suggesting that early adversity is not necessarily associated with insecure attachment in this context. Our hypothesis for the current study was that relationship difficulties are associated with adversity, but that these may be expressed as a higher prevalence of RAD symptoms, rather than insecure attachment, given that RAD is known to be associated with early trauma, whereas insecure attachment can be present in typical development. Our aim was to re-enrol this cohort, to examine the prevalence of RAD and to explore associations between RAD symptoms and attachment status both now and in early childhood.
Recruitment procedure
We purposely selected 40 mother–infant dyads to participate in this research, following them up 10 years post-enrolment. The primary selection criteria for the sub-sample were attachment classification at 18 months. Figure 1 outlines attachment status of the original and current sample. To ensure that all four attachment categories in the original research were represented, we approached 40–50% of all children in each of the four infancy attachment categories. Of the 40 participants approached, none refused.
Figure 1.
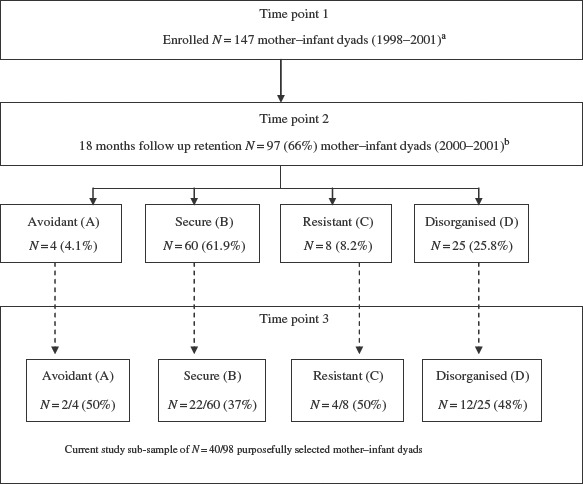
Consort diagram of sample 1999–2011.
Notes: aTomlinson et al., 2005. bTomlinson, Cooper, Stein, Swartz, & Molteno, 2006.
Measures
1. Manchester Child Attachment Story Task
The Manchester Child Attachment Story Task (MCAST) is a doll-play story stem technique measuring attachment patterns in middle childhood (Green, Stanley, Smith, & Goldwyn, 2000). It includes four stories with attachment-related themes using a dolls house, designed for use with school-aged children. The child's story is video-taped and subjected to structured coding based on the strange situation procedure (SSP) and adult attachment interview (AAI) codes to provide an attachment classification (Green et al., 2000). It has good inter-rater reliability, stability of attachment patterns over time and concurrent validity with well-validated measures of attachment (O'Connor & Gerard Byrne, 2007) and has been used in ethnically diverse samples (Futh, O'Connor, Matias, Green, & Scott, 2008).
2. RAD assessment package
The assessment package for RAD contains three elements: the Relationship Problems Questionnaire (RPQ), a 10-item questionnaire for RAD symptoms with good validity and reliability data (Minnis et al., 2007); the Waiting Room Observation (WRO), a structured observation of child behaviour with strangers in a waiting room setting (McLaughlin, Espie, & Minnis, 2010); and the CAPA-RAD, a 30-item semi-structured parent-report interview, which assesses RAD symptoms and is a module of the Child and Adolescent Psychiatric Assessment (CAPA) (Angold & Costello, 2000). The CAPA-RAD has good inter-rater reliability with good discrimination (Minnis et al., 2009).
Procedure
Children were accompanied by a primary caregiver. Following informed consent and child assent, caregivers completed the RPQ, demographic questions and the CAPA-RAD and the MCAST was administered to the child. Caregivers were given a food voucher, worth about £7, for participation. Ethical clearance was received from Stellenbosch University Health Research Ethics Committee (N06/08/149).
Results
Sample characteristics
Table 1 shows primary caregiver, household and child characteristics of all children and of the children with RAD. There were differences between the families of the 98 children at 18 months of age and the 40 currently participating children. A significantly higher proportion of caregivers was employed than in 1999 (χ2 (1, 187) = 38.174, p < 0.001), likely influenced by a high proportion of parents looking after young children in 1999. A significantly higher proportion were living in brick houses than shacks compared to 1999 (χ2 (1, 187) = 44.925, p < 0.001). Distribution of males and females was equal (50.3/49.7% in 1999; 50/50% current).
Table 1.
Sample demographics for all children (N = 40), % and children with RAD (N = 5), %.
| Characteristics | All children (N = 40), % | Children with RAD (N = 5/40), % |
|---|---|---|
| Child's age | 9.87 years | 10 years |
| Caregiver's age | 37.5 years | 36.4 years |
| Child living with biological mother | 90% | 100% |
| Living in same house as father | 50% | 40% |
| Caregiver in employment | 53% | 80% |
| Income | ZAR841 | ZAR948 |
| Living in house with water | 63% | 40% |
| Living in house with electricity | 100% | 100% |
| Living in house with inside toilet | 30% | 0% |
| Average number of people in the house | 6 | 5 |
| Owned house | 50% | 40% |
| Brick house | 53% | 20% |
Attachment patterns and RAD diagnosis
Table 2 summarises the RAD and MCAST attachment findings. Five children (12.5%), all boys, three with secure, organised current MCAST attachment, and two with insecure, disorganised MCAST attachments, fulfilled diagnostic criteria for RAD. These five children were significantly more likely to score positive (t (38) = 5.392, p ≤ 0.001) for the following seven disinhibited behaviours of the 30 behaviours rated in the CAPA-RAD: comfort seeking from adults, indiscriminate adult relationships, demanding or attention seeking, minimum checking in with caregiver in unfamiliar setting, cuddliness with strangers, personal questions and invading boundaries.
Table 2.
RAD and MCAST classification by gender.
| RAD | Present | Absent | Total |
| Male | 5 (12.5%) | 15 (37.5%) | 20 |
| Female | 0 (0%) | 20 (50%) | 20 |
| Total | 5 (12.5%) | 35 (87.5%) | 40 (100%) |
| MCAST attachment | Secure | Insecure | Total |
| Male | 13 (32.5%) | 7 (17.5%) | 20 |
| Female | 15 (37.5%) | 5 (12.5%) | 20 |
| Total | 28 (70%) | 12 (30%) | 40 (100%) |
| MCAST attachment | Organised | Disorganised | Total |
| Male | 14 (35%) | 6 (15%) | 20 |
| Female | 17 (42%) | 3 (7%) | 20 |
| Total | 31 (77%) | 9 (23%) | 40 (100%) |
Figure 2 outlines the attachment patterns of children over time from SSP attachment patterns at 18 months to MCAST attachment classifications at 10 years. There was no association between SSP classification at 18 months and RAD diagnosis (Fisher's exact test (N = 40) = 0.64). When RAD scores were examined against current attachment classification, higher RAD scores were found in children showing current insecure, disorganised attachment patterns (t (38) = −2.794, p = 0.008) on the MCAST. When adjusted in linear regression analysis, for age and gender, the results remained significant (r2 = 0.11, p = 0.014).
Figure 2.
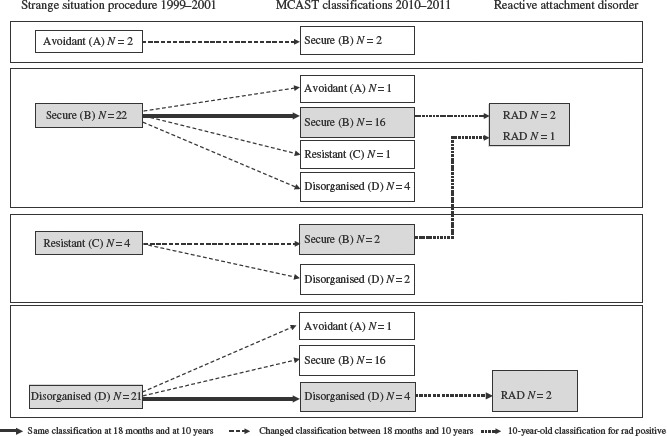
SSP classifications at 18 months and MCAST classifications at 10 years by RAD diagnosis.
Discussion
In this high-risk sample, 12.5% of children were diagnosed with RAD. This rate is higher than expected, even taking our purposive sampling into account, and concerning since RAD is associated with a significant mental health morbidity (Angold & Costello, 2000; Minnis et al., 2009), and tends to remain stable and generalise to most social contexts (Gleason et al., 2011; Rutter, 2010).
Boys appear disproportionably affected by RAD in this sample, in particular with disinhibited patterns, and they appear at slightly elevated risk of insecure and disorganised attachments. For these South African boy children, who already face significant physical, sexual and psychological risks as they enter adolescence (Bhana, 2010), a diagnosis of RAD (disinhibited type) could significantly impact on their ability to develop healthy social relationships and avoid risk behaviours. While acknowledging that this gender effect may be the result of the small sample size and possible selection bias, it is similar to findings in the attachment literature (Minnis et al., 2007) that suggest that male gender places children at elevated risk of attachment difficulties, in particular of disinhibited patterns. Some research has postulated that temperament may play an important role (Zeanah & Fox, 2004) with boys being more prone to disinhibition and girls to inhibition when exposed to similarly neglectful environments, but this remains an area of significant debate in the child development literature. This warrants further investigation in future research.
It is equally plausible that reporting bias and cultural nuances around gender and children's behaviour may have influenced parent reporting in the cultural context of this research. Disinhibition may draw greater parental attention and reporting among caregivers of boys, while inhibition in girls, given gender inequality and stereotypes about girl children in South Africa (Jewkes, Morrell, & Christofides, 2009; Jewkes, Penn-Kekana, & Rose-Junius, 2005), may have been unreported. While the strengths of the diagnostic methodology used in this research lies in triangulating parental report with observation data on children, it is possible that further research with larger and more diverse samples may provide more insight into the presence or absence of RAD amongst girl children in South Africa.
Attachment at 18 months was not significantly associated with RAD symptoms in middle childhood, while current attachments were. This is in line with current evidence from rich countries that RAD and early childhood disorganised attachment are not synonymous (Gleason et al., 2011; Minnis et al., 2009; Zeanah & Gleason, 2010). Disorganisation of current attachment at age of 10 years was significantly associated with RAD, highlighting the importance of secure and consistent relationships for children, not only in early childhood, but in the pre-adolescent years. Longitudinal research in South Africa has shown evidence of the effect of chronic poverty, loss of primary caregivers and exposure to abuse on subsequent risk of exposure to alcohol, earlier sexual debut, HIV and transactional sex in adolescents (Cluver, Orkin, Boyes, Gardner, & Meinck, 2011; Nyirenda, McGrath, & Newell, 2010; Operario, Underhill, Chuong, & Cluver, 2011). Mental disorders such as RAD may contribute to explaining the pathways to such risk exposure given that RAD can impact on a child's capacity to perceive and be wary of risk from strangers, may inhibit their approaches for assistance from others, may increase impulsivity and degrade their problem solving capacity (Potter et al., 2009). Further research on school-aged children is required to inform not only intervention but also prevention models.
Conclusions
Our findings suggest that both the MCAST and the standardised assessment package for RAD are useful measures for describing relationship functioning and social behaviour in high-risk samples in South Africa. The level of engagement of children with the MCAST story stems is systematically rated and no child was rated as being too poorly engaged with the task to continue with rating. As such this research demonstrates the feasibility of using diagnostic tools such as the MCAST and the RAD standardised assessment package to measure RAD in at risk children in South Africa. Further research is required to explore possible cultural nuances in the reporting of both inhibited and disinhibited behaviours in pre-adolescent boy and girl children in high-risk contexts, where the context of risk itself, the developmental stage of the child and established gender biases may influence or inform reporting.
This research offers preliminary support for the hypothesis that RAD may not be directly related to the presence of an early attachment disorder, but that chronic childhood adversity may be associated with relationship difficulties and that this adversity, together with other factors (not specifically examined in this research but which have been explored in the literature) such as harsh or negative parenting, genetic influences and the caregiving environment throughout childhood, may result in RAD in older children in LMIC.
The prevalence of RAD in this sample is 10 times higher than evidenced in rich countries, and further research is required to determine to what extent this is reflective of prevalence at a population level in South Africa and in other LMIC settings. The higher vulnerability of boy children in this sample (if replicated) may offer direction for the development of targeted interventions. However, this research cannot provide equivocal evidence for a lack of vulnerability among girl children given the possible risk of selection and reporting bias.
While this research is strengthened by its longitudinal nature, the availability of early attachment data and the use of diagnostic assessments, it is limited by its small sample size and risk of selection bias. Results should be interpreted with caution and confirmed by larger studies.
Acknowledgements
We thank all the mothers and children who took part in the study. This study was funded by NHS Greater Glasgow and Clyde. Mark Tomlinson is supported by the National Research Foundation (South Africa) and Tamsen Rochat receives salary support from the Wellcome Trust. We also thank Marjorie Feni for the assistance with recruitment and data collection.
References
- Angold A., Costello E. The child and adolescent psychiatric assessment (CAPA) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- Bennett J., Espie C., Duncan B., Minnis H. A qualitative exploration of children's understanding of indiscriminate friendliness. Clinical Child Psychology and Psychiatry. 2009;14:595–618. doi: 10.1177/1359104509339137. doi: 10.1177/1359104509339137. [DOI] [PubMed] [Google Scholar]
- Bhana A. Middle childhood and pre-adolescence. In: Peterson I., Bhana A., Flisher A., Swartz L., Richter L., editors. Promoting mental health in scare-resource contexts. Cape Town: HSRC Press; 2010. pp. 124–142. [Google Scholar]
- Breidenstine A. S., Bailey L. O., Zeanah C. H., Larrieu J. A. Attachment and trauma in early childhood: A review. Journal of Child & Adolescent Trauma. 2011;4:274–290. [Google Scholar]
- Cluver L., Gardner F., Operario D. Poverty and psychological health among AIDS-orphaned children in Cape Town, South Africa. AIDS Care. 2009;21:732–741. doi: 10.1080/09540120802511885. doi: 10.1080/09540120802511885. [DOI] [PubMed] [Google Scholar]
- Cluver L., Orkin M., Boyes M., Gardner F., Meinck F. Transactional sex amongst AIDS-orphaned and AIDS-affected adolescents predicted by abuse and extreme poverty. Journal of Acquired Immune Deficiency Syndrome. 2011;58:336–343. doi: 10.1097/QAI.0b013e31822f0d82. doi: 10.1097/QAI.0b013e31822f0d82. [DOI] [PubMed] [Google Scholar]
- Cluver L., Orkin M., Boyes M. E., Gardner F., Nikelo J. AIDS-orphanhood and caregiver HIV/AIDS sickness status: Effects on psychological symptoms in South African youth. Journal of Pediatric Psychology. 2012;37:857–867. doi: 10.1093/jpepsy/jss004. doi: 10.1093/jpepsy/jss004. [DOI] [PubMed] [Google Scholar]
- Collins P. Y., Patel V., Joestl S. S., March D., Insel T. R., Daar A. S., Walport M. Grand challenges in global mental health. Nature. 2011;475:27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper P. J., Tomlinson M., Swartz L., Woolgar M., Murray L., Molteno C. Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. The British Journal of Psychiatry. 1999;175:554–558. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- Cortina M. A., Sodha A., Fazel M., Ramchandani P. G. Prevalence of child mental health problems in Sub-saharan Africa: A systematic review. Archives of Pediatrics & Adolescent Medicine. 2012;166:276. doi: 10.1001/archpediatrics.2011.592. [DOI] [PubMed] [Google Scholar]
- Earls F., Raviola G. J., Carlson M. Promoting child and adolescent mental health in the context of the HIV/AIDS pandemic with a focus on sub-Saharan Africa. Journal of Child Psychology and Psychiatry. 2008;49:295–312. doi: 10.1111/j.1469-7610.2007.01864.x. [DOI] [PubMed] [Google Scholar]
- Fearon R., Bakermans-Kranenburg M. J., Van IJzendoorn M. H., Lapsley A. M., Roisman G. I. The significance of insecure attachment and disorganization in the development of children's externalizing behavior: A meta-analytic study. Child Development. 2010;81:435–456. doi: 10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- Futh A., O'Connor T. G., Matias C., Green J., Scott S. Attachment narratives and behavioral and emotional symptoms in an ethnically diverse, at-risk sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:709–718. doi: 10.1097/CHI.0b013e31816bff65. doi: 10.1097/CHI.0b013e31816bff65. [DOI] [PubMed] [Google Scholar]
- Gleason M. M., Fox N. A., Drury S., Smyke A., Egger H. L., Nelson C. A., Zeanah C. H. Validity of evidence-derived criteria for reactive attachment disorder: Indiscriminately social/disinhibited and emotionally withdrawn/inhibited types. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:216–231. doi: 10.1016/j.jaac.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowinski A. L. Reactive attachment disorder: An evolving entity. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:210–212. doi: 10.1016/j.jaac.2010.12.013. [DOI] [PubMed] [Google Scholar]
- Green J., Stanley C., Smith V., Goldwyn R. A new method of evaluating attachment representations in young school-age children: The Manchester Child Attachment Story Task. Attachment & Human Development. 2000;2:48–70. doi: 10.1080/146167300361318. [DOI] [PubMed] [Google Scholar]
- Jewkes R., Morrell R., Christofides N. Empowering teenagers to prevent pregnancy: Lessons from South Africa. Culture, Health & Sexuality. 2009;11:675–688. doi: 10.1080/13691050902846452. [DOI] [PubMed] [Google Scholar]
- Jewkes R., Penn-Kekana L., Rose-Junius H. “If they rape me, I can't blame them”: Reflections on gender in the social context of child rape in South Africa and Namibia. Social Science & Medicine. 2005;61:1809–1820. doi: 10.1016/j.socscimed.2005.03.022. [DOI] [PubMed] [Google Scholar]
- Kieling C., Baker-Henningham H., Belfer M., Conti G., Ertem I., Omigbodun O., Rahman A. Child and adolescent mental health worldwide: Evidence for action. The Lancet. 2011;374:1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- Kleintjes S., Flisher A., Fick M., Railoun A., Lund C., Molteno C., Robertson B. A. The prevalence of mental disorders among children, adolescents and adults in the Western Cape, South Africa. African Journal of Psychiatry. 2006;9:157–160. [Google Scholar]
- McLaughlin A., Espie C., Minnis H. Development of a brief waiting room observation for behaviours typical of reactive attachment disorder. Child and Adolescent Mental Health. 2010;15:73–79. doi: 10.1111/j.1475-3588.2009.00549.x. [DOI] [PubMed] [Google Scholar]
- Meltzer H., Britain G. The mental health of young people looked after by local authorities in England. London: Stationery Office; 2003. [Google Scholar]
- Minnis H., Green J., O'Connor T. G., Liew A., Glaser D., Taylor E., Polmin R. An exploratory study of the association between reactive attachment disorder and attachment narratives in early school-age children. Journal of Child Psychology and Psychiatry. 2009;50:931–942. doi: 10.1111/j.1469-7610.2009.02075.x. [DOI] [PubMed] [Google Scholar]
- Minnis H., Marwick H., Arthur J., McLaughlin A. Reactive attachment disorder – a theoretical model beyond attachment. European Child & Adolescent Psychiatry. 2006;15:336–342. doi: 10.1007/s00787-006-0539-2. [DOI] [PubMed] [Google Scholar]
- Minnis H., Reekie J., Young D., O'connor T., Ronald A., Gray A., Polmin R. Genetic, environmental and gender influences on attachment disorder behaviours. The British Journal of Psychiatry. 2007;190:490–495. doi: 10.1192/bjp.bp.105.019745. [DOI] [PubMed] [Google Scholar]
- Nleya N., Thompson L. Survey methodology in violence-prone Khayelitsha, Cape Town, South Africa. IDS Bulletin. 2009;40:50–57. doi: 10.1111/j.1759-5436.2009.00038.x. [Google Scholar]
- Nyirenda M., McGrath N., Newell M. L. Gender differentials in the impact of parental death: Adolescent's sexual behaviour and risk of HIV infection in rural South Africa. Vulnerable Children and Youth Studies. 2010;5:284–296. doi: 10.1080/17450128.2010.507804. doi: 10.1080/17450128.2010.507804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor T. G., Gerard Byrne J. Attachment measures for research and practice. Child and Adolescent Mental Health. 2007;12:187–192. doi: 10.1111/j.1475-3588.2007.00444.x. doi: 10.1111/j.1475-3588.2007.00444.x. [DOI] [PubMed] [Google Scholar]
- Operario D., Underhill K., Chuong C., Cluver L. HIV infection and sexual risk behaviour among youth who have experienced orphanhood: Systematic review and meta-analysis. Journal of the International AIDS Society. 2011;14:25. doi: 10.1186/1758-2652-14-25. doi: 10.1186/1758-2652-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Flisher A. J., Nikapota A., Malhotra S. Promoting child and adolescent mental health in low and middle income countries. Journal of Child Psychology and Psychiatry. 2008;49:313–334. doi: 10.1111/j.1469-7610.2007.01824.x. doi: 10.1111/j.1469-7610.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- Potter D., Chevy L. C., Amaya-Jackson L., O'Donnell K., Murphy R. A., Zeanah C. H., Jr Clinical Guidelines Series 2009. Reactive attachment disorder (RAD): Appropriate and inappropriate application of the reactive attachment disorder diagnosis on an age continuum from birth through age 18. 2009. Retrieved from http://www.pbhcare.org/pubdocs/upload/documents/radguidelines2009.pdf.
- Rohde L. A. The need of epidemiological data on child mental disorders from low-middle income countries. European Child & Adolescent Psychiatry. 2011;20:497–498. doi: 10.1007/s00787-011-0217-x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Child and adolescent psychiatry: Past scientific achievements and challenges for the future. European Child & Adolescent Psychiatry. 2010;19:689–703. doi: 10.1007/s00787-010-0111-y. [DOI] [PubMed] [Google Scholar]
- Rutter M., Kreppner J., Sonuga-Barke E. Emanuel miller lecture: Attachment insecurity, disinhibited attachment, and attachment disorders: Where do research findings leave the concepts? Journal of Child Psychology and Psychiatry. 2009;50:529–543. doi: 10.1111/j.1469-7610.2009.02042.x. [DOI] [PubMed] [Google Scholar]
- Sameroff A. A unified theory of development: A dialectic integration of nature and nurture. Child Development. 2010;81:6–22. doi: 10.1111/j.1467-8624.2009.01378.x. [DOI] [PubMed] [Google Scholar]
- Skovgaard A. M., Houmann T., Christiansen E., Landorph S., Jørgensen T., Team C. C. C. S., Lichtenberg A. The prevalence of mental health problems in children 1½ years of age – the Copenhagen Child Cohort 2000. Journal of Child Psychology and Psychiatry. 2007;48:62–70. doi: 10.1111/j.1469-7610.2006.01659.x. doi: 10.1111/j.1469-7610.2006.01659.x. [DOI] [PubMed] [Google Scholar]
- Thompson L., Kemp J., Wilson P., Pritchett R., Minnis H., Toms-Whittle L., Gillberg C. What have birth cohort studies asked about genetic, pre- and perinatal exposures and child and adolescent onset mental health outcomes? A systematic review. European Child & Adolescent Psychiatry. 2010;19(1):1–15. doi: 10.1007/s00787-009-0045-4. [DOI] [PubMed] [Google Scholar]
- Tomlinson M., Cooper P., Murray L. The Mother-Infant relationship and infant attachment in a South African Peri-Urban settlement. Child Development. 2005;76:1044–1054. doi: 10.1111/j.1467-8624.2005.00896.x. doi: 10.1111/j.1467-8624.2005.00896.x. [DOI] [PubMed] [Google Scholar]
- Tomlinson M., Cooper P., Stein A., Swartz L., Molteno C. Post-partum depression and infant growth in a South African peri-urban settlement. Child: Care, Health and Development. 2006;32:81–86. doi: 10.1111/j.1365-2214.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- Walker S. P., Wachs T. D., Grantham-McGregor S., Black M. M., Nelson C. A., Huffman S. L., Richter L. Inequality in early childhood: Risk and protective factors for early child development. The Lancet. 2011;378:1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- Zeanah C. H., Fox N. A. Temperament and attachment disorders. Journal of Clinical Child & Adolescent Psychology. 2004;33:32–41. doi: 10.1207/S15374424JCCP3301_4. doi: 10.1207/s15374424jccp3301_4. [DOI] [PubMed] [Google Scholar]
- Zeanah C. H., Gleason M. M. Reactive attachment disorder: A review for DSM-V. Proposed Revisions: Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence. DSM-5 Development. 2010. Retrieved from http://www.dsm5.org/Proposed%20Revision%20Attachments/APA%20DSM-5%20Reactive%20Attachment%20Disorder%20Review.pdf.


