Abstract
Background
Participation is an important, yet seldom studied, outcome after total knee replacement (TKR).
Objective
The purpose of this study was to investigate the extent and predictors of participation and participation restriction among people after TKR.
Materials and Methods
This study investigated the changes in pain, function, and participation scores (measured using a subscale of the Late-Life Function and Disability Instrument) from pre-TKR to ≥1 year post-TKR among a subsample of participants from the Multicenter Osteoarthritis Study (MOST) longitudinal cohort (MOST is funded by the National Institutes of Health). The proportions of individuals with participation restriction pre-TKR and ≥1 and ≥2 years post-TKR were calculated for all participants and for important demographic subgroups. The association between demographic and clinical factors and participation was estimated using linear regression. The association between demographic and clinical factors and participation restriction was estimated using logistic regression.
Results
There were 292 individuals with outcome data ≥1 year post-TKR. Of these, 218 (75%) had data pre-TKR and ≥1 year post-TKR and 160 (55%) had data ≥2 years post-TKR. There were mean improvements in pain, function, and participation at ≥1 and 2 years. However, approximately 30% of the study sample had participation restriction pre-TKR and post-TKR, and the proportion decreased significantly only for those <65 years old. Non-whites had a higher proportion of participation restriction than any other subgroup (41% ≥1 year, 48% ≥2 years). Female sex and non-white race were associated with a worse participation score, and several demographic and modifiable factors were associated with participation restriction following TKR.
Limitations
The time between pre-TKR and post-TKR assessment varied across study participants, and data were not available on their rehabilitation utilization.
Conclusions
Although there was a mean increase in participation ≥1 year following TKR, participation restriction was common. The likelihood of low participation was increased among women, non-whites, and those with depressive symptoms, severe pain in either knee, or worse pre-TKR function.
As the number of total knee replacements (TKRs) in the United States continues to increase,1,2 it is becoming increasingly imperative to understand clinical outcomes. Although the literature focuses on pain and function,3–6 these outcomes do not address whether TKR allows people to engage more fully in their daily activities. Engagement in life situations—operationally defined as “participation” in the International Classification of Functioning, Disability and Health (ICF)7—is recognized as an important health outcome for individuals with or at risk of developing disabilities. Participation is a complex domain, which includes one's involvement with social roles and the environment and may encompass factors (eg, psychosocial needs) with unclear relation to TKR surgery. Participation has been strongly associated with health outcomes, including mortality.8
Currently, there is little research on participation-level outcomes following TKR. Most research has focused on outcomes related to pain9 and function3 (eg, getting out of a chair or climbing stairs). In general, studies show a decrease in pain and an increase in function, with approximately 75% of participants experiencing significant or clinically important improvements in these domains.3,4,10 Previous research beyond these domains has focused on component aspects of participation (eg, the ability to dress oneself, cook a meal,11 or participate in sporting activities12). One study of the trajectory of recovery of people with knee and hip TKRs13 showed improvements in participation occurring later than pain and function. To our knowledge, however, the impact of TKR on participation defined by the proportions with participation restriction has yet to be reported, nor has it been studied greater than 12 months postsurgery.
The purpose of this study was twofold. First, we sought to explore the extent of home and community participation restriction pre-TKR and post-TKR and the change after the procedure. Second, we investigated the associations between demographic and clinical factors and pain and function with participation restriction among individuals undergoing TKR. These analyses used data from a large, comprehensive multicenter cohort study in people with knee osteoarthritis. Understanding the effects of knee replacement on participation outcomes and the potential factors associated with participation will assist clinicians in designing interventions and goals to optimize the participation level activities of their patients.
Method
Participants
Participants were selected from the Multicenter Osteoarthritis Study (MOST), the National Institutes of Health–funded longitudinal cohort study of 3,026 people 50 to 79 years old with or at high risk of developing knee osteoarthritis at the time of enrollment. Included participants were overweight or obese or had a previous significant knee injury, knee surgery, or recent knee pain. Participants were recruited from the Iowa City, Iowa, and Birmingham, Alabama, communities via flyers and public service announcements. People with bilateral knee replacements, with a history of cancer other than nonmelanoma skin cancer, with certain rheumatologic conditions (eg, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and reactive arthritis), unable to walk without a walker or assistance of another person, or planning to move out of the area were excluded. Enrolled individuals were assessed via a comprehensive battery of self-report questionnaires and clinical examinations at baseline and at 30, 60, and 84 months. The sample used in this study was limited to those individuals who had at least 1 TKR following baseline but prior to the 60-month clinical visit. Given this window for TKR, participants in MOST had data on participation collected both pre-TKR and at least 12 months post-TKR, long enough after surgery to allow for adequate recovery.14
Outcome Measures
Participation.
Participation was measured at each clinic visit using the Late Life Disability Instrument-Instrumental Limitation scale (LLDI-IL), a subscale of the Late-Life Function and Disability Instrument (LLFDI).15 The LLFDI and its subscales are validated self-report measures, with the LLDI-IL questions pertaining to the amount of limitation one has with 12 instrumental home and community activities (eg, shopping or entertaining in one's home). Each item is scored from 1 to 5, with higher scores indicating better participation and totals ranging from 12 to 60. We used this measure as a continuous outcome and defined self-reported restriction with participation activities (participation restriction) using a previously established cutpoint of a scaled score of <67.6/100.16
Pain.
Pain severity was measured using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)17 pain severity subscale. This validated questionnaire consists of 5 questions regarding pain during daily activity, scored from 0 to 4, with total scores from 0 to 20. Increased scores signify increased pain.
Function.
Post-TKR function was assessed using the WOMAC17 physical function subscale, a well-validated measure consisting of 17 items related to physical functioning (eg, “stair use” and “rising from sitting”). Each item is rated on a 5-point Likert scale from 0 to 4, based on the amount of difficulty performing each functional activity. Scores are summed for a raw total score between 0 and 68, with higher scores indicating worse function.
Exposure Measures
TKR status.
Participants reported TKR at any of the MOST clinic visits. More than 95% of TKRs were confirmed by medical records or radiographs taken during study visits. Total knee replacement surgeries included total or partial joint arthroplasties; up to the 60-month visit, more than 95% of the TKRs were total.
Covariates.
In addition to using data on pre-TKR WOMAC physical function and pre-TKR severe WOMAC pain of the ipsilateral and contralateral knee (dichotomized at ≥10/20), we used the data on the following post-TKR covariates collected at the same post-TKR clinic visit as the outcomes: sex, race, age at TKR, educational attainment, depressive symptoms ≥16 (yes/no) on the Center for Epidemiologic Studies Depression Scale,18 unilateral or bilateral TKRs, body mass index ≥30 kg/m2, TKR and number of comorbidities (modified Charlson index19). Quadriceps femoris muscle strength (generated during an isokinetic concentric knee extension contraction at 60°/s and normalized to N·m/kg of body weight) was measured at the 60-month clinic visit. Values were assessed for both knees, even if both knees were replaced. The maximum value of 4 trials for the TKR knee was used when a TKR was unilateral, and the maximum value for the stronger of the 2 knees was used when the TKRs were bilateral.
Data Analysis
We computed the mean pain, function, and participation scores before and after TKR for all participants and a sensitivity analysis for those whose pre-TKR visit was within 6 months of their TKR. We compared the pre-TKR and post-TKR mean scores for each outcome using paired t tests with a 2-sided alpha set at .05. We then determined the proportion of individuals with participation restriction at least 1 year and at least 2 years after TKR. We analyzed the differences in the proportions of those with participation restriction pre-TKR and ≥1 year post-TKR using the chi-square test.
We calculated the proportions of participants who had or did not have post-TKR participation restriction based on the presence of having participation restriction or not prior to TKR using cross-tabulation methods. We then evaluated the association of participation at ≥1 year following TKR and the following independent variables: sex, race, age category at TKR, educational attainment, depressive symptoms, quadriceps muscle strength, severe pain in the ipsilateral or contralateral knee, number of knees replaced, body mass index, pre-TKR WOMAC physical function, and number of comorbidities. We assessed the association between each variable with participation as a continuous variable using linear regression and participation restriction as a dichotomous variable using logistic regression. Multivariable analyses were adjusted for the other variables in the model. We estimated standardized beta coefficients and P values for the effect of a 1-standard deviation unit increase in each independent variable on participation from the linear regression to allow a comparison of the strength of the independent variables and estimated odds ratios with 95% confidence intervals from the logistic regression.
Role of the Funding Source
The MOST Study was supported by the National Institute on Aging and by the following National Institutes of Health grants: U01-AG18820 (Dr Felson), U01-AG19069 (Dr Nevitt), U01-AG18832, U01-AG18947, and AR47785. Funding for this project also was provided by an American College of Rheumatology Rheumatology Research Foundation Rheumatology Scientist Development Award (Dr Maxwell) and by NIDRR H133B100003-11 (Dr Maxwell).
Results
There were 292 participants with outcome data ≥1 year post-TKR. Of these, 218 had pre-TKR participation data and outcome data ≥1 year post-TKR and 160 also had participation data pre-TKR and ≥2 years post-TKR available. The mean time between pre-TKR assessment and TKR was 15.4 months (SD=9.4). The mean time following TKR to outcome assessment was 25.5 months (SD=16.1) for those individuals ≥1 year post-TKR and 37.3 months (SD=14.8) for those ≥2 years post-TKR. Table 1 presents the participants' demographic and clinical data at ≥1 year after TKR for all 292 participants. There were 18 participants (12%) and 16 participants (14%) who had severe knee pain in the contralateral knee at the pre-TKR visit and ≥1 year after TKR, respectively.
Table 1.
Participant Demographics and Clinical Factors ≥1 Year Post-TKR (n=292)a
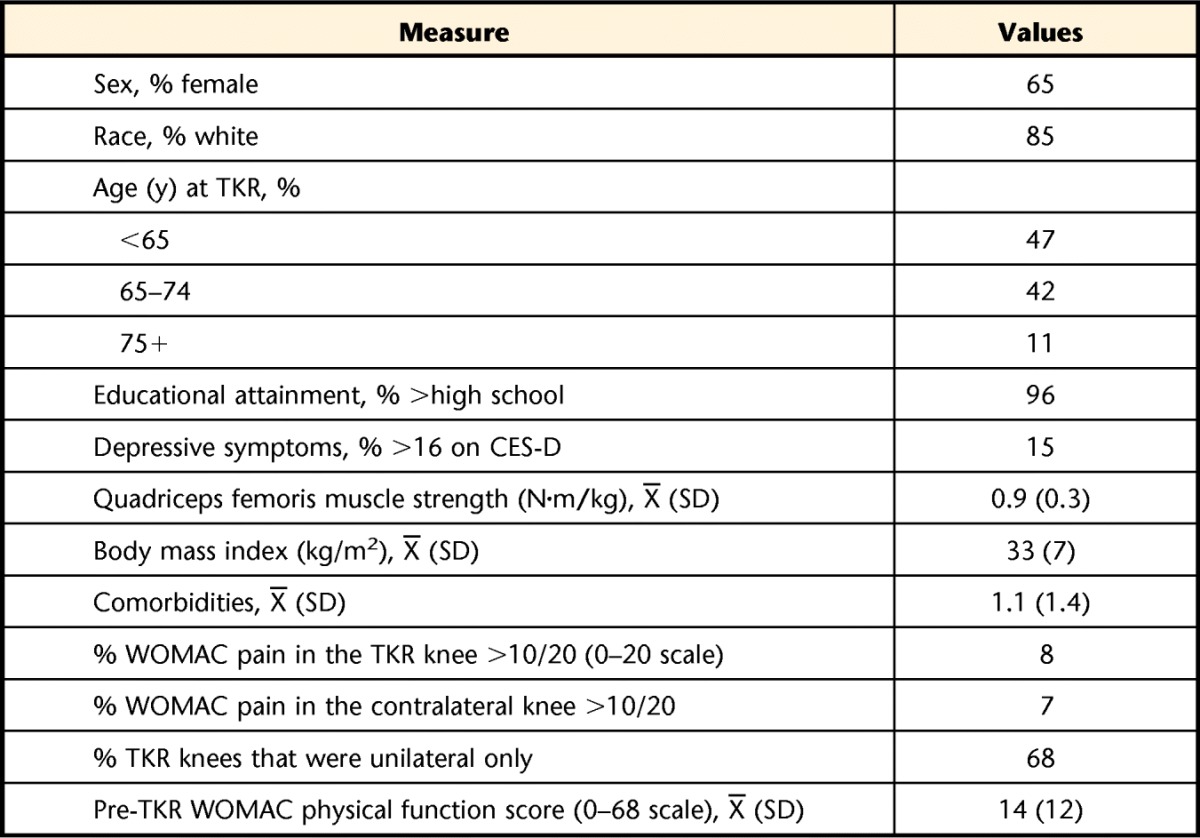
TKR=total knee replacement, CES-D=Center for Epidemiologic Studies Depression Scale, WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index.
The mean pain, function, and participation scores pre-TKR and ≥1-year post-TKR and the change between the 2 times in the 218 participants with both pre-TKR and post-TKR data are presented in Table 2. There were statistically significant improvements in mean scores for pain, function, and participation after TKR. When our sensitivity analysis was restricted to the 52 individuals who had participation assessed within 6 months prior to their TKR, the mean pre-TKR participation score decreased to 68/100 and the change increased to 7 points.
Table 2.
Pre-TKR and Post-TKR Status in Pain, Function, and Participationa

Higher scores indicate worse pain and function but also indicate better participation. TKR=total knee replacement.
b P value comparing pre-TKR and post-TKR values for the 218 participants with data ≥1 year post-TKR.
c P value comparing pre-TKR and post-TKR values for the 160 participants with data ≥2 years post-TKR.
Thirty-one percent of the study sample met our definition of participation restriction at least 1 year following TKR (Tab. 3). The proportions with participation restriction were approximately one third for all subgroups, except for men (25%) and non-whites (41%). The proportion of individuals with participation restriction decreased from pre-TKR to ≥1 year post-TKR for all groups except those aged older than 75 years; in this group, the proportion with participation restriction increased from 24% pre-TKR to 44% ≥1 year post-TKR. However, only participants less than 65 years old at the time of TKR had a statistically significant reduction in the proportion with participation restriction post-TKR (P<.01). There was no statistical difference between the proportions with participation restriction ≥1 and ≥2 years post-TKR (31% and 32%, respectively). Across all age groups, among those with participation restriction pre-TKR, approximately half continued to have participation restriction post-TKR (Tab. 4). For the 2 younger age groups, more than 80% of those without pre-TKR participation restriction had no restriction ≥1 year after TKR. However, among those 75 years old or older, 45% had participation restriction 1 year after TKR.
Table 3.
Proportions of Participants With Participation Restriction Pre-TKR and Post-TKRa

TKR=total knee replacement.
Table 4.
Proportions With Participation Status Restricted or Not Restricted Pre-TKR and ≥1 Year Post-TKR Stratified by Age Category (n=218)a
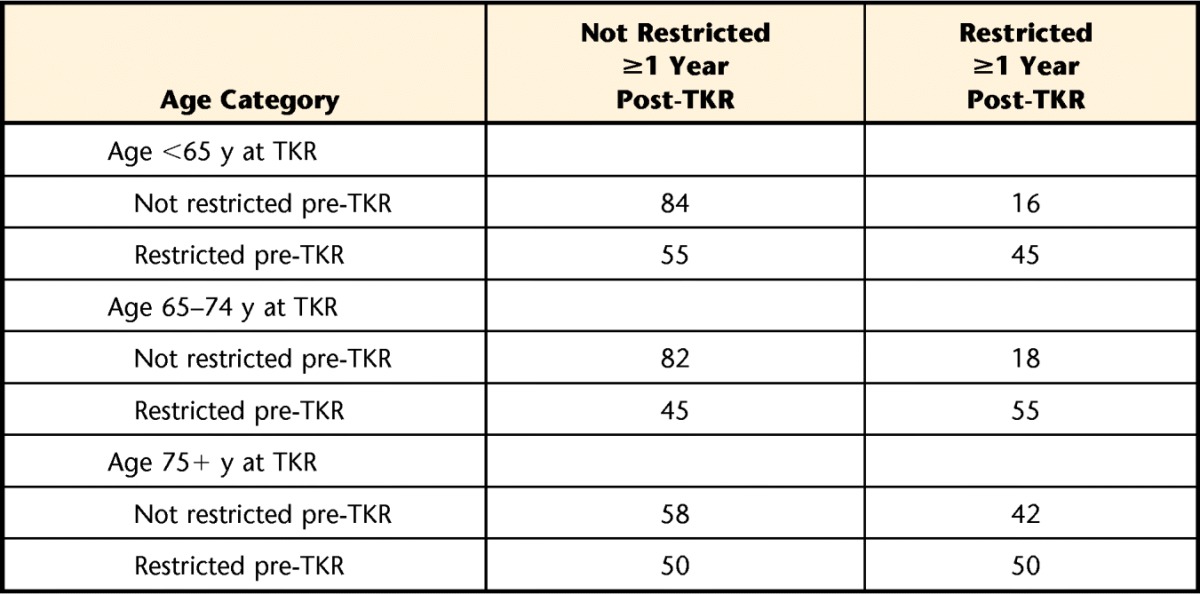
TKR=total knee replacement.
When participation restriction was defined using the cutpoint of <67.6/100 (Tab. 5), having depressive symptoms, severe pain in either knee, and lower pre-TKR physical function were statistically significantly associated with participation restriction. Being in the oldest age group, being of non-white race, and having a higher number of comorbidities had modest nonsignificant associations with participation restriction.
Table 5.
Association Between Patient Factors and Participation Restriction ≥1 Year Post-TKR (n=292)a
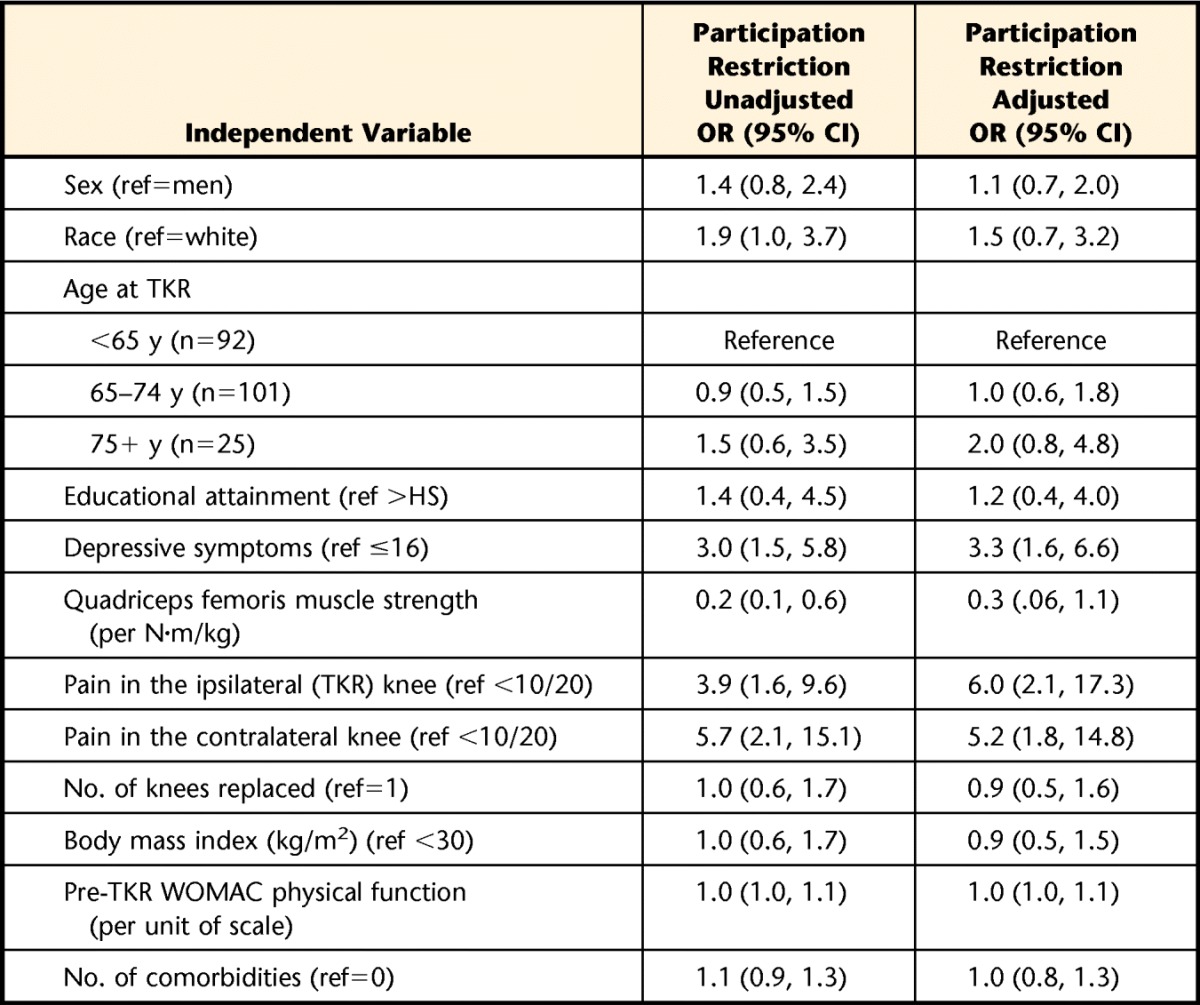
Adjusted for age, sex, race, and educational attainment. TKR=total knee replacement, WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index, OR=odds ratio, 95% CI=95% confidence interval, ref=reference, HS=high school.
During sensitivity analyses, we examined post-TKR participation as a continuous outcome measure. Female sex, non-white race, depressive symptoms, severe pain in either the replaced or contralateral knee, and lower pre-TKR physical function were all statistically associated with lower participation, with pre-TKR function (standardized β=−.32, P<.001) and depressive symptoms and severe pain in the ipsilateral knee (both standardized β=−.3, P<.001) being the factors most strongly associated with lower participation. When the participants with severe contralateral knee pain were removed from the analysis, 28% reported participation restrictions ≥1 year following TKR.
Discussion
This study showed that (1) although home and community participation improved from pre-TKR to post-TKR, approximately one third of the total study sample and subgroups reported having participation restriction ≥1 and 2 years after TKR, and (2) participation depended on age at TKR and other demographic and clinical factors. To our knowledge, this is the first quantitative study to estimate the proportions of people with self-reported participation restriction after TKR as well as to investigate the potential demographic, clinical, and psychosocial factors associated with post-TKR participation restriction. Physical therapists may want to discuss and address participation goals with patients early in the course of postoperative care to reinforce returning to life roles that may have been compromised as their osteoarthritis progressed and may consider the modifiable and nonmodifiable factors associated with participation restrictions when planning intervention and determining prognosis.
Our study confirmed previous work that demonstrated a mean improvement in participation after TKR. Davis and colleagues'13 final trajectory model of recovery over the first 12 months after TKR showed that participation on the LLDI did improve, but slower and later in the postoperative year than the other ICF domains of physical impairments and activity limitations. In our study, the improvement in pain achieved standards of minimal clinically important difference,20 and the improvement in function was just under the published minimal clinically important difference.20 As we are unaware of a validated minimal clinically important difference in participation, we are unable to characterize this amount of improvement; however, it was a small percentage change (3 points on a 100-point rating scale). Our study showed similar reductions in pain and improvements in function as the study by Davis et al,13 yet their participants had a larger increase (equivalent to 18/100 points) in participation from pre-TKR to 1 year post-TKR. Our sensitivity analysis, restricted to individuals who had participation assessed within 6 months prior to their TKR, resulted in a change from pre-TKR to post-TKR participation, which was closer to, but still lower than, the change found in the study by Davis et al. Other recent evidence suggests participation as an outcome may not change robustly from a single physical intervention,21 although this possibility should be investigated further.
Presenting statistical means to characterize improvement may be incomplete. Hence, our approach was to present the proportions of subgroups of participants with self-reported participation restriction following TKR. Doing so allows us to understand the public health impact and the experiences of the individuals most intensely affected by the intervention. Also, determining proportions with or without participation restriction pre-TKR and post-TKR allows inspection of the influence of baseline status on post-TKR outcomes. Pre-TKR functional status has been widely recognized as the strongest predictor of post-TKR functional status.22–24 Our results indicate that this finding may extend to participation status and that TKR does not produce substantial increases in participation ≥1 year for individuals with pre-TKR participation restriction. The impact of pre-TKR intervention to optimize the pre-TKR function and participation status on post-TKR participation should be studied further.
Several demographic and clinical factors were associated with post-TKR participation. Surprisingly, pre-TKR participation restriction was lowest among those in our oldest age group, although there were small numbers in this subgroup. It is possible that older people have lower expectations for their participation and, therefore, may not consider themselves “limited” in activities when answering the questions on the LLDI-IL. Conversely, this could simply describe the participation status of elderly people healthy enough to select and undergo TKR. In addition, the proportion of the oldest individuals with participation restriction at ≥1 year actually increased, and a large proportion (42%) of those without participation restriction pre-TKR reported restriction at 1 year post-TKR. This concerning finding may indicate increased recovery time for some people in this age group or simply effects of aging on participation. This proportion slightly decreased at 2 years, which would support the former hypothesis. The number of individuals in this age group at this time point, however, is small. Therefore, this is a speculative interpretation.
Our non-white participants had a higher proportion with participation restriction pre-TKR than did whites (62% versus 33%). Non-whites, particularly African Americans, have a lower utilization of TKR than whites.25 The proportion of non-white individuals with participation restriction at each time point was higher than that of the other subgroups with the exception of the oldest participants at ≥1 year and may indicate a need for increased intervention throughout the pre-TKR and post-TKR periods. The failure of variables representing non-white race and oldest age to emerge as significant predictors of participation score and participation restriction in our multivariable analyses may reflect the low numbers of subjects in these subsamples and should be explored further in a cohort with larger numbers of such individuals.
Additionally, several modifiable factors were associated with low post-TKR participation and self-reported participation restriction and, therefore, may indicate potential targets for the treatment of participation restriction in the post-TKR population. For example, severe pain in the contralateral knee was one of the strongest predictors of participation and participation restriction, suggesting that while symptoms are present in the nonreplaced knee, people may not return to their presurgical level of participation. Interestingly, however, the number of knees replaced and quadriceps muscle strength were not associated with participation restrictions in this study. Other potentially modifiable factors most strongly associated with participation restriction in our study included severe continued pain in the TKR knee and depressive symptoms. Because psychosocial factors are a significant part of the conceptual model of participation and disability in the ICF,7 it is important to consider the impact of such factors, including depressive symptoms, on participation in patient populations.26
Our study used a subscale of the LLFDI as our outcome measure, which focuses on taking care of one's daily responsibilities and social activities. A recent qualitative study explored similar constructs of participation by asking patients what activities were important to them prior to surgery and assessed their difficulty with them 1 year after TKR.26 The authors, similarly, found approximately 25% of patients were unable to perform their preferred activities of leisure 1 year after surgery. Other standardized outcome tools that measure components of participation include those focused on work or sporting activities27,28 and may be relevant as the knee replacement population continues to get younger. One such study found only a quarter of patients were participating in intense sporting activities >1 year after surgery.12 Therefore, there is growing support that patients with TKRs continue to have restrictions across participation domains following knee replacement, and more research in this area is warranted.
Among the limitations of this study was its small sample size among some demographic groups, which may have influenced the power to identify associations. The varied length of time between pre-TKR participation assessment and TKR may have influenced the proportion with participation restriction prior to TKR and the amount of change in participation, as discussed above; however, the timing between pre-TKR assessment and TKR did not affect post-TKR results. As participation is a complex construct that includes social factors and one's environment, it may be important to study changes in this population for a longer period of time after TKR. Currently, this study has examined these changes up to 2 years and did not show substantial changes from 1 to 2 years. Time frames of 5 to 10 years may be more telling. Our data also do not include information on rehabilitation services received by the participants; therefore, the impact of rehabilitation on participation outcomes post-knee replacement cannot be determined.
Conclusion
Although there were overall mean reductions in pain and improvements in function and modest improvements in participation at least 1 year following TKR, at least a third of the participants displayed post-TKR participation restriction. All groups had a reduction in the proportion of the study sample with participation restriction following TKR with the exception of those >75 years of age. Female sex, non-white race, depressive symptoms, severe pain in either knee, and lower pre-TKR functional status were associated with decreased participation ≥1 year post-TKR, and the above factors with the exception of sex and race were associated with increased odds of participation restriction. Physical therapy interventions aimed at addressing modifiable factors both presurgery and postsurgery may improve participation in the growing population of patients post-TKR, and the factors associated with participation status should be considered when designing courses of care. Physical therapists may consider the nonmodifiable factors associated with participation restriction when determining clinical prognoses.
The Bottom Line
What do we already know about this topic?
Total knee replacement produces improvement in pain and function in approximately 75% of patients, although the other 25% may have persistent pain and functional deficits. Although little studied, it appears that, overall, patients report a mean increase in participation in the first year following knee replacement.
What new information does this study offer?
This study demonstrates that a marked proportion of patients have participation restrictions at least 1 year after knee replacement, and that this proportion differs by age group. Pain in either the replaced knee or the contralateral knee and depressive symptoms were associated with participation restrictions after knee replacement.
If you're a patient, what might these findings mean for you?
Patients should understand that there is a risk of participation restrictions occurring or persisting after knee replacement, and that pain in either knee or depressive symptoms are 2 factors that could be addressed in order to improve participation following surgery.
Footnotes
Dr Maxwell, Dr Keysor, Dr Singh, Dr Wise, Dr Frey-Law, Dr Nevitt, and Dr Felson provided concept/idea/research design. Dr Maxwell, Dr Keysor, Dr Singh, Dr Frey-Law, Dr Nevitt, and Dr Felson provided writing. Dr Felson provided data collection. Dr Maxwell, Dr Niu, Dr Singh, Dr Frey-Law, and Dr Nevitt provided data analysis. Dr Nevitt provided project management and institutional liaisons. Dr Keysor, Dr Nevitt, and Dr Felson provided fund procurement. Dr Singh, Dr Wise, Dr Frey-Law, and Dr Felson provided consultation (including review of manuscript before submission). The authors thank Alan Jette, PT, PhD, FAPTA, for his unselfish time and consultation toward the improvement of this project.
A poster presentation of this research was given at the World Congress on Osteoarthritis; April 26–29, 2012; Barcelona, Spain.
The MOST Study was supported by the National Institute on Aging and by the following National Institutes of Health grants: U01-AG18820 (Dr Felson), U01-AG19069 (Dr Nevitt), U01-AG18832, U01-AG18947, and AR47785. Funding for this project also was provided by the American College of Rheumatology Rheumatology Research Foundation Rheumatology Scientist Development Award (Dr Maxwell) and by NIDRR H133B100003-11 (Dr Maxwell).
References
- 1. Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Singh JA, Vessely MB, Harmsen WS, et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85:898–904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Singh JA, O'Byrne M, Harmsen S, Lewallen D. Predictors of moderate-severe functional limitation after primary total knee arthroplasty (TKA): 4701 TKAs at 2-years and 2935 TKAs at 5-years. Osteoarthritis Cartilage. 2010;18:515–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cushnaghan J, Bennett J, Reading I, et al. Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis. 2009;68:642–647 [DOI] [PubMed] [Google Scholar]
- 5. Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1719–1724 [DOI] [PubMed] [Google Scholar]
- 6. Alzahrani K, Gandhi R, DeBeer J, et al. Prevalence of clinically significant improvement following total knee replacement. J Rheumatol. 2011;38:753–759 [DOI] [PubMed] [Google Scholar]
- 7. Jette AM. Toward a common language for functioning, disability, and health. Phys Ther. 2006;86:726–734 [PubMed] [Google Scholar]
- 8. Dale C, Prieto-Merino D, Kuper H, et al. Modelling the association of disability according to the WHO International Classification of Functioning, Disability and Health (ICF) with mortality in the British Women's Heart and Health Study. J Epidemiol Community Health. 2012;66:170–175 [DOI] [PubMed] [Google Scholar]
- 9. Wylde V, Hewlett S, Learmonth I, Dieppe P. Persistent pain after joint replacement: prevalence, sensory qualites, and postoperative determinants. Pain. 2011;152:566–572 [DOI] [PubMed] [Google Scholar]
- 10. Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466:2717–2723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. George LK, Ruiz D, Jr, Sloan FA. The effects of total knee arthroplasty on physical functioning in the older population. Arthritis Rheum. 2008;58:3166–3171 [DOI] [PubMed] [Google Scholar]
- 12. Williams DH, Greidanus NV, Masri BA, et al. Predictors of participation in sports after hip and knee arthroplasty. Clin Orthop Relat Res. 2012;470:555–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davis AM, Perruccio AV, Ibrahim S, et al. The trajectory of recovery and the inter-relationships of symptoms, activity and participation in the first year following total hip and TKR. Osteoarthritis Cartilage. 2011;19:1413–1421 [DOI] [PubMed] [Google Scholar]
- 14. Zeni JA, Jr, Snyder-Mackler L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther. 2010;90:43–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jette AM, Haley SM, Coster WJ, et al. Late Life Function and Disability Instrument, I: development and evaluation of the disability component. J Gerontol A Biol Med Sci. 2002;57:M209–M216 [DOI] [PubMed] [Google Scholar]
- 16. Keysor JJ, Jette AM, LaValley MP, et al. Community environmental factors are associated with disability in older adults with functional limitations: the MOST study. J Gerontol A Biol Sci Med Sci. 2010;65:393–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840 [PubMed] [Google Scholar]
- 18. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401 [Google Scholar]
- 19. Katz JN, Chang LC, Sangha O, et al. Can comorbidity be measured by questionnaire rather than medical record review? Med Care.1996;34:73–84 [DOI] [PubMed] [Google Scholar]
- 20. Escobar A, Quintana JM, Bilbao A, et al. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2007;15:273–280 [DOI] [PubMed] [Google Scholar]
- 21. VanSwearingen JM, Perera S, Brach JS, et al. Impact of exercise to improve gait efficiency on activity and participation in older adults with mobility limitations: a randomized controlled trial. Phys Ther. 2011;91:1740–1751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hawker G, Wright J, Coyte P, et al. Health-related quality of life after TKR. J Bone Joint Surg Am. 1998;80:163–173 [DOI] [PubMed] [Google Scholar]
- 23. Fortin PR, Penrod JR, Clarke AE, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46:3327–3330 [DOI] [PubMed] [Google Scholar]
- 24. Lingard EA, Katz JN, Wright EA, Sledge CB; Kinemax Outcomes Group Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86:2179–2186 [DOI] [PubMed] [Google Scholar]
- 25. Jha AK, Fisher ES, Li Z, et al. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691 [DOI] [PubMed] [Google Scholar]
- 26. Wylde V, Livesey C, Blom AW. Restriction in participation in leisure activities after joint replacement: an exploratory study. Age Ageing. 2012;41:246–249 [DOI] [PubMed] [Google Scholar]
- 27. Styron JF, Barsoum WK, Smyth KA, Singer ME. Preoperative predictors of returning to work following primary total knee arthroplasty. J Bone Joint Surg Am. 2011;93:2–10 [DOI] [PubMed] [Google Scholar]
- 28. Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895 [DOI] [PubMed] [Google Scholar]


