Abstract
The current study examines the extent to which H1N1 was stigmatized at the height of the 2009 H1N1 pandemic in the U.S. and explores the role that H1N1 stigma played in people’s desire for physical distance from others with H1N1. H1N1 was the most stigmatized disease, with participants endorsing greater prejudice towards people with H1N1 than people with cancer or HIV/AIDS. Further, H1N1 stigma partially mediated the relationship between participants’ perceptions that H1N1 was threatening and their desire for physical distance from people with H1N1. Therefore, H1N1 stigma played a role in, but was not entirely responsible for, the relationship between perceptions that H1N1 was threatening and desire for distance from others with H1N1.
Keywords: stigma, influenza, H1N1, pandemic, HIV/AIDS
The World Health Organization first reported the discovery of H1N1, also known as the swine flu, in humans in March 2009 (“Pandemic (H1N1) 2009”, 2010). By June, the World Health Organization declared the disease to be a pandemic. Like many of its predecessors (e.g., the 1918 Spanish flu; Taubenberger & Morens, 2010), this latest influenza virus proved to be a substantial public health threat due to its contagious and disabling nature. In the United States alone, the Centers for Disease Control and Prevention estimates that approximately 61 million people were infected with, 274,000 people were hospitalized due to, and 12,470 people died from H1N1 by the end of the flu season (“Updated CDC estimates”, 2010). As a result of the threat of H1N1, the public health response to H1N1 in 2009 was swift. An important component of the public health response included implementing physical distancing measures to slow the spread of H1N1. For example, primary and secondary schools (Chan & Sulzberger, 2009; Kumar, 2009; Leland, 2009; Wong, 2009) as well as restaurants and public places (Lacey & Betancourt, 2009) were closed throughout the world, and travel restrictions were enforced (Wong, 2009). Importantly, stigma directed at people with H1N1 may have supported adherence to physical distancing measures by boosting the public’s desire to distance themselves from people with H1N1. The current work examines the extent to which H1N1 was stigmatized at the height of the 2009 H1N1 pandemic and explores the role that H1N1 stigma played in people’s desire for physical distance from others infected with H1N1.
Diseases such as H1N1 that are perceived to be contagious and disabling are often stigmatized. That is, they represent a mark of social devaluation or discrediting (Goffman, 1963). For example, HIV/AIDS and tuberculosis are among the most highly stigmatized diseases throughout the world (Aggleton & Parker, 2002; Courtwright & Turner, 2010; Van Rie et al., 2008; Westbrook, Legge, & Pennay, 1993). Evolutionary psychologists have posited that disease stigma is adaptive because it protects the self from threatening diseases (Kurzban & Leary, 2001; Park, Faulkner, & Schaller, 2003; Stevenson & Repacholi, 2005; Tybur, Lieberman, & Griskevicius, 2009). Evolved reactions to people with disease, such as feelings of disgust (Stevenson & Repacholi, 2005; Tybur et al., 2009) and prejudicial attitudes (Park et al., 2003; Park, Schaller, & Crandall, 2007), are theorized to increase desire for physical distance from others who could transmit a threatening disease to the self. Jones and colleagues (1984) labeled this dimension of stigma as “peril,” and Kurzban and Leary (2001) identified this suite of evolved adaptations as “parasite avoidance.” Therefore, stigma may increase adherence to physical distancing measures implemented by public health officials during influenza pandemics.
Despite its theorized importance, however, few studies have examined the role of stigma in people’s desire for physical distance from others with disease within the context of actual infectious disease emergencies. Understanding the relationship between stigma and people’s desire for physical distance from others with infectious disease is critical to the extent that it can inform strategies to protect public health during future influenza pandemics (e.g., H5N1; Taubenberger & Morens, 2010). If stigma fully mediates the relationship between perceptions of disease threat and desire for physical distance from others with influenza, then public health officials might encourage influenza to be stigmatized during future influenza emergencies. This stigma may ultimately protect non-infected individuals from contracting influenza. Indeed, public health practitioners during the 1918 Spanish flu pandemic may have used stigma to achieve their goal of limiting the transmission of influenza. Rosner (2010) noted that “public health practitioners were active in finding means to limit the impact of disease” employing measures such as “mandated (often public) identification and (perhaps) stigmatization” (p. 39). If, however, stigma does not fully mediate the relationship between perceptions of disease threat and desire for physical distance from others with disease, then public health officials might consider intervening to reduce stigma during future influenza emergencies. This stigma may actually undermine public health efforts aimed at curbing the spread of influenza.
Although disease stigma may be adaptive insofar as it increases non-infected individuals’ desire for distance from others with disease, it may be maladaptive to the extent that it impedes other components of public health responses to pandemic emergencies such as H1N1. Stigma associated with influenza during the 1918 Spanish flu pandemic and the 1994 Indian plague epidemic impeded effective public health responses in several ways, including undermining efforts aimed at detection and treatment of people with disease (Barrett & Brown, 2008). People diagnosed with influenza during the 1918 pandemic were subject to discriminatory statutes, panic, and even abandonment. People infected with influenza, in turn, may have evaded medical detection to avoid negative treatment. Infected individuals who went undetected may have also gone without adequate medical treatment for their symptoms and therefore suffered worse health outcomes than they may have otherwise. Thus, similar to HIV stigma, influenza stigma may ultimately undermine testing (Chesney & Smith, 1999) and treatment efforts (Chesney & Smith, 1999; Peretti-Watel, 2006; Vanable, Carey, Blair, & Littlewood, 2006), and further threaten the mental and physical health of people infected with influenza (Berger, Ferrans, & Lashley, 2001; Holzemer et al., 2007; Mak et al., 2007; Vanable et al., 2006). Furthermore, infected individuals who go undetected may be more likely to infect others with influenza. Stigma may therefore undermine the public health response to infectious disease pandemics by acting as a barrier to detection, treatment, and containment efforts.
To better understand the relationship between stigma and people’s desire for physical distance from others with infectious disease, we studied influenza stigma during the height of the 2009 H1N1 pandemic in the U.S. The objectives of the current work were to (1) examine the extent to which H1N1 was stigmatized, and (2) explore the role that influenza stigma played in people’s desire for physical distance from others with H1N1. To achieve our first objective, we measured affect towards people with H1N1 in November 2009 [i.e., the height of the U.S. H1N1 pandemic (“Pandemic (H1N1) 2009”, 2010)] and compared it to affect towards people with HIV/AIDS and cancer, two widely studied stigmatized diseases (Aggleton & Parker, 2002; Chapple, Ziebland, & McPherson, 2004; Fife & Wright, 2000; Mahajan et al., 2008; Westbrook et al., 1993). We measured affect because decreased affect is a characteristic of prejudice (Allport, 1954; Brewer, 2007), and therefore represents a way in which stigma is manifested or expressed among non-stigmatized individuals (Earnshaw & Chaudoir, 2009). To achieve our second objective, we evaluated whether affect towards people with H1N1 mediated the relationship between perceptions that H1N1 was threatening (i.e., contagious and disabling) and desire for distance from others with H1N1. We collected data to accomplish these objectives from a sample of U.S. college students because they were a segment of the U.S. population who were at an elevated risk of H1N1 infection and whose lives were particularly disrupted when infected with H1N1 (Brown, 2009).
Method
Participants and Procedure
237 students from the University of Connecticut participated in the study in exchange for partial course credit. Participants were between the ages of 17 and 24 (M = 18.81; SD = .97; 61% female). Informed consent was obtained from all participants. Participants were excluded from the data analyses if they currently or previously had H1N1 (n = 16) or cancer (n = 2). No participants reported having HIV/AIDS. The remaining sample that was included in the analyses totaled 219 participants.
The study, titled “Relating to Others,” was conducted online using psychsurveys.org. Upon accessing the website, participants were told that they would be asked what they thought about various diseases and people living with those diseases. The diseases included cancer, HIV/AIDS, and H1N1. Participants were asked to think about each disease and answer the questions that followed. The diseases were presented in random order. The study was a completely within-subjects design.
Materials
Affect
Participants’ affect towards others with cancer, HIV/AIDS, and H1N1 was measured using feeling thermometers. Participants responded to the question “How do you feel towards people who have cancer {HIV/AIDS/H1N1}?” on 100-point scales ranging from very negative (1) to very positive (100). Because prejudice is characterized in part by decreased affect (Allport, 1954; Brewer, 2007), and because explicit measures of prejudice are unlikely to be endorsed for social desirability reasons, feeling thermometers are often used to measure greater endorsement of prejudice towards others with the diseases. Lower scores reflect colder (or less positive) feelings towards the measured group.
H1N1 Threat
Participants’ assessment of the extent to which H1N1 was threatening was measured by gauging how contagious and disabling they perceived H1N1 to be. Participants’ perceptions of the extent to which H1N1 was contagious were measured with three items, including: “H1N1 is highly contagious,” “It is easy to catch H1N1 from others,” and “H1N1 is easily communicated from person to person.” Participants rated these items on a Likert scale ranging from strongly disagree (1) to strongly agree (7; α = .90). The mean score on contagiousness was 6.11 (SD = 1.05). Participants’ perceptions of the extent to which H1N1 was disabling were measured with four items, including: “People with H1N1 are very sick,” “H1N1 is a serious disease,” “People who have H1N1 have to make a lot of changes because of their health,” and “H1N1 is highly disruptive to people’s lives.” Participants rated these items on a Likert scale ranging from strongly disagree (1) to strongly agree (7; α = .82). The mean score on disabling was 4.66 (SD = 1.33). Participants’ responses to these two measures were then multiplied. The resulting H1N1 threat score therefore reflects the extent to which participants perceived H1N1 to be both contagious and disabling. Participants with high H1N1 threat scores perceived H1N1 to be very contagious and disabling, whereas participants with low H1N1 threat scores perceived H1N1 to be less contagious and disabling.
Physical Distance
Participants’ desire for physical distance from people with H1N1 was measured with five items, including: “I would not shake hands with someone who has H1N1,” “I would try to leave the room if someone who has H1N1 was in it,” “I would not hug someone who has H1N1,” “I would sit next to someone who has H1N1 at a movie” (reverse coded), and “I would sit in the same room as someone who has H1N1” (reverse coded). Participants rated these items on a Likert scale ranging from strongly disagree (1) to strongly agree (7; α = .80). Therefore, higher scores indicate greater desire for physical distance from others with H1N1. The mean score on desire for physical distance was 5.03 (SD = 1.41).
Results
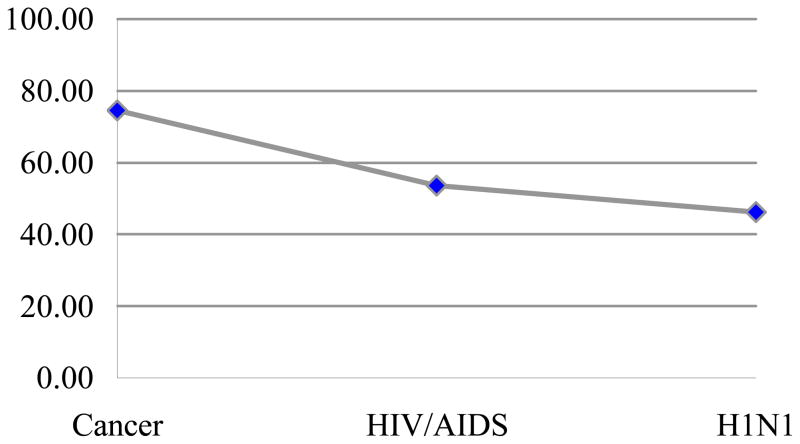
We first examined how participants felt towards people with cancer, HIV/AIDS, and H1N1 to assess how stigmatized H1N1 was in November 2009 relative to other stigmatized diseases. We analyzed responses to the feeling thermometers by conducting a repeated measures ANOVA with the 3 disease types as the repeated factor (disease type: cancer, HIV/AIDS, H1N1). Results demonstrated a multivariate effect of disease type, F (2, 214) = 135.62, p < .001, ηp2 = .56. As shown in Figure 1, participants reported the least positive affect towards people with H1N1 (M = 46.27, SD = 24.47), followed by HIV/AIDS (M = 53.60, SD = 23.14) and cancer (M = 74.66, SD = 20.95). Bonferonni adjusted post-hoc tests confirmed that the mean difference between each of the diseases was statistically significant (all ps < .001). The results of this analysis suggest that H1N1 was the most stigmatized disease in this study, with participants reporting colder affect towards people with H1N1 than people with HIV/AIDS or cancer at the height of the H1N1 pandemic.
Figure 1.
Mean ratings of affect towards others with cancer, HIV/AIDS, and H1N1 as measured by feeling thermometers.
We next examined whether perceptions of H1N1 threat were related to desire for physical distance from others with H1N1, and whether this relationship was mediated by affect. To accomplish this, we followed the steps outlined for testing mediation described by Baron and Kenny (1986). The results of this analysis, including the standardized regression weights, are shown in Figure 2. We first regressed affect on H1N1 threat. This step demonstrated that perceptions that H1N1 was threatening were related to decreased affect. Second, we regressed physical distance on H1N1 threat. This step demonstrated that perceptions of H1N1 as threatening were related to increased desire for physical distance from others with H1N1. Third, we regressed physical distance on H1N1 threat and affect. This final step demonstrated that affect was negatively related to physical distance. That is, decreased affect was related to more desire for physical distance from others with H1N1. The final step further demonstrated that when controlling for affect, the relationship between H1N1 threat and physical distance was reduced but was still statistically significant. A Sobel test demonstrated that this reduction was statistically significant. Therefore, affect partially mediated the relationship between perceptions of H1N1 as threatening and desire for physical distance from others with H1N1.
Figure 2.
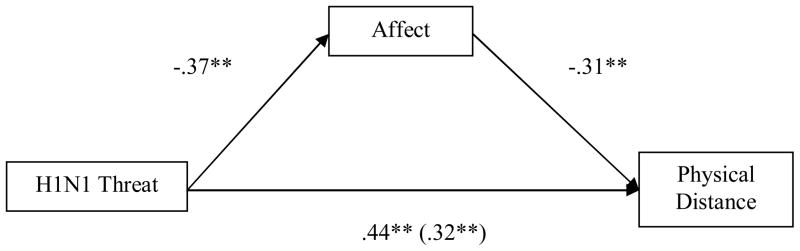
Model demonstrating the mediational role of affect in the relationship between H1N1 threat and physical distance.
Note: p < .001**; Sobel = −3.65, SE < .001, p < .001
Discussion
In the current work, we examined the extent to which H1N1 was stigmatized at the height of the 2009 H1N1 pandemic in the U.S. and explored the role that H1N1 stigma played in people’s desire for distance from others with H1N1. The results of the study demonstrate that H1N1 was stigmatized at the height of the pandemic: people held decreased affect, or increased prejudice, towards others with H1N1. Significantly, people in this sample felt more negatively towards people with H1N1 than people with HIV/AIDS. This is a striking finding given that HIV/AIDS is arguably one of the most stigmatized diseases throughout the world (Aggleton & Parker, 2002; Mahajan et al., 2008). The results of the study further demonstrate that this decreased affect was related to the extent that people perceived that H1N1 was threatening (i.e., contagious and disabling), and that it partially mediated the relationship between perceptions of H1N1 threat and desire for physical distance from others with H1N1. That is, perceptions of H1N1 threat were associated with decreased affect, which in turn were related to greater desire for physical distance from others with H1N1.
Applications to Future Pandemics
The current work can help to inform strategies to protect public health during future influenza pandemics. Influenza stigma represents a difficult paradox. On one hand, it may bolster public health efforts to protect people from influenza infection by increasing people’s desire for physical distance from others with influenza. On the other hand, it may undermine detection, treatment, and containment efforts thereby contributing to poor health outcomes of people infected with influenza and increasing the spread of influenza. According to the results of the current work, reductions in influenza stigma may not entirely undermine public health officials’ goals to increase physical distancing. Decreased affect only partially mediated the relationship between perceptions of H1N1 threat and desire for physical distance from others with H1N1. In addition to its indirect effect on physical distance through decreased affect, perceptions of H1N1 threat had a fairly robust direct effect on physical distance. This suggests that although prejudice contributes to the relationship between H1N1 threat and physical distance, the relationship between H1N1 threat and physical distance would remain without prejudice. Consequently, it may be possible to reduce people’s feelings of prejudice towards others with influenza while maintaining their desire for distance from others with influenza.
The challenge for social psychologists is to develop effective strategies to reduce influenza stigma without also reducing desire for distance from others with influenza. Effective stigma reduction strategies have been developed for other types of stigmas that could be adapted to reduce influenza stigma. However, many of these strategies rely on increasing contact with stigmatized individuals (Pettigrew & Tropp, 2008) and are therefore ill-suited to reducing influenza stigma. Facing another paradox of how to reduce influenza stigma without increasing contact with people with influenza, social psychologists might consider exploring stigma-reduction strategies recommended by Barrett and Brown (2008) involving increasing community trust of government officials and health care providers. People who trust that their government officials and health care providers will protect them from the threat of influenza may be less likely to stigmatize others with influenza. Given the possibility of an H5N1 pandemic in the coming years, social psychologists might begin developing and testing influenza stigma reduction strategies now to be better prepared to aid public health efforts to intervene in influenza stigma if and when this “pandemic-in-waiting” (p. 17; Taubenberger & Morens, 2010) hits.
Limitations
The current study is limited in the extent to which it is generalizable to populations other than U.S. college students. We chose to study this population because young adults were at an elevated risk of H1N1 and were therefore particularly hard hit by the pandemic. This was similar to the 1918 Spanish influenza in which young adults experienced the highest death rates from influenza (Taubenberger & Morens, 2010). Additionally, the lives of U.S. college students who were infected with H1N1 were often highly disrupted by isolation measures and quarantines (Brown, 2009). It is possible that these findings are not generalizable to non-college student and non-U.S. populations. However, given that the relationship between disease threat, stigma, and distancing is theorized to be an evolved psychological phenomenon (Kurzban & Leary, 2001; Park et al., 2003; Stevenson & Repacholi, 2005; Tybur et al., 2009), we are confident that these results would generalize to other populations.
An additional limitation of the current study is its use of single-item feeling thermometers to measure participants’ affect towards others with diseases. Feeling thermometers have been used in past work to measure greater endorsement of prejudice towards others, and have been demonstrated to be associated with other measures of prejudice (e.g., Miller, Smith, & Mackie, 2004). Feeling thermometers yield a blunt measure of affect; however, participants’ feelings towards others with diseases may be more nuanced. For example, they may feel compassion and/or disgust towards others with disease. These emotions are important to understand to the extent that they impact people’s interactions with others with disease and ultimately public health during disease epidemics. Therefore, future work might distinguish between other emotions when studying disease stigma.
A further limitation of the current work is that it does not capture the deleterious impact that stigma may have had on people who were infected with H1N1 during the 2009 H1N1 pandemic. This study focused on perceptions of people who were uninfected by H1N1. Therefore, we are unable to assess the extent to which H1N1 stigma undermined testing and treatment efforts, and/or contributed to decreased mental or physical health among people infected with influenza. Although we can no longer assess these outcomes for H1N1, we can learn from accumulating evidence demonstrating that stigma plays a deleterious role within other disease epidemics such as HIV/AIDS (Berger et al., 2001; Chesney & Smith, 1999; Holzemer et al., 2007; Mak et al., 2007; Peretti-Watel, 2006; Vanable et al., 2006) and tuberculosis (Courtwright & Turner, 2010). Generalizing from this robust body of disease stigma research to influenza, it is likely that influenza stigma impacted the thoughts, feelings, and behaviors of people with influenza during the H1N1 pandemic and may have a similar impact during future influenza pandemics. Future research might more fully explore the impact of influenza stigma within the context of future influenza outbreaks.
Conclusions
The current study found that H1N1 was highly stigmatized at the height of the 2009 H1N1 pandemic in the U.S. H1N1 stigma partially mediated the relationship between perceptions of H1N1 threat and desire for physical distance from others with H1N1. The current work suggests that influenza stigma can be reduced without decreasing non-infected individuals’ desire for physical distance from others infected with influenza. Therefore, social psychologists might explore strategies to reduce influenza stigma now to help public health officials be better prepared to combat its negative effects during future influenza pandemics.
Acknowledgments
Preparation of this manuscript was supported by a training fellowship (T32MH074387) awarded to the first author from the National Institute of Mental Health. We thank Amy Huntington, Kimberly McClure, Nicole Overstreet, and Eileen Pitpitan for their helpful comments on this work.
References
- Aggleton P, Parker R. A conceptual framework and basis for action: HIV/AIDS stigma and discrimination. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2002. [Google Scholar]
- Aimone F. The 1918 influenza epidemic in New York City: A review of the public health response. Public Health Reports. 2010;125(3):71–79. doi: 10.1177/00333549101250S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allport GW. The nature of prejudice. Oxford, England: Addison-Wesley; 1954. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrett R, Brown PJ. Stigma in the time of influenza: Social and institutional responses to pandemic emergencies. The Journal of Infectious Diseases. 2008;197(Suppl 1):S34–4. doi: 10.1086/524986. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Brewer MB. The social psychology of intergroup relations: Social categorization, ingroup bias, and outgroup prejudice. In: Kruglanski AW, Higgins ET, editors. Social psychology: Handbook of basic principles. New York, NY: The Guilford Press; 2007. pp. 695–715. [Google Scholar]
- Brown R. The New York Times. 2009. Sep 5, College version of quarantine is “club swine”; p. 1. [Google Scholar]
- Chan S, Sulzberger AG. The New York Times. 2009. May 26, Mayor says more school closings won’t stop swine flu’s spread; p. 14. [Google Scholar]
- Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ: British Medical Journal. 2004;328(7454):1470–1470. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesney MA, Smith AW. Critical delays in HIV testing and care: The potential role of stigma. American Behavioral Scientist. 1999;42:1158–1170. [Google Scholar]
- Courtwright A, Turner AN. Tuberculosis and stigmatization: Pathways and interventions. Public Health Reports. 2010;125(4):34–39. doi: 10.1177/00333549101250S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of Health and Social Behavior. 2000;41:50–67. [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. New York, NY: Simon & Schuster; 1963. [Google Scholar]
- Holzemer WL, Uys LR, Chirwa ML, Makoae LN, Dlamini PS, Mullan J, et al. Validation of the HIV/AIDS stigma instrument--PLWA (HASI-P) AIDS Care. 2007;19(8):1002–1012. doi: 10.1080/09540120701245999. [DOI] [PubMed] [Google Scholar]
- Kumar H. The New York Times. 2009. Aug 13, Swine flu rattles nerves as it spreads through india; p. 13. [Google Scholar]
- Kurzban R, Leary MR. Evolutionary origins of stigmatization: The functions of social exclusion. Psychological Bulletin. 2001;127(2):187–208. doi: 10.1037/0033-2909.127.2.187. [DOI] [PubMed] [Google Scholar]
- Lacey M, Betancourt A. The New York Times. 2009. Oct 8, Experience guides Mexico as swine flu cases surge; p. 14. [Google Scholar]
- Leland J. The New York Times. 2009. Oct 23, Mistrust and fear over swine flu close schools in Iraq; p. 4. [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS. 2008;22(Supplement 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak WWS, Cheung RYM, Law RW, Woo J, Li PCK, Chung RWY. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Social Science and Medicine. 2007;64(8):1549–1559. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Miller DA, Smith ER, Mackie DM. Effects of intergroup contact and political predispositions on prejudice: Role of intergroup emotions. Group Processes & Intergroup Relations. 2004;7:221–237. [Google Scholar]
- Pandemic (H1N1) 2009. 2010 Retrieved 7/23, 2010, from http://www.who.int/csr/disease/swineflu/en/index.html.
- Park JH, Faulkner J, Schaller M. Evolved disease-avoidance processes and contemporary anti-social behavior: Prejudicial attitudes and avoidance of people with physical disabilities. Journal of Nonverbal Behavior. 2003;27(2):65–87. [Google Scholar]
- Park JH, Schaller M, Crandall CS. Pathogen-avoidance mechanisms and the stigmatization of obese people. Evolution and Human Behavior. 2007;28(6):410–414. [Google Scholar]
- Peretti-Watel P. Management of HIV-related stigma and adherence to HAART: Evidence from a large representative sample of outpatients attending French hospitals (ANRS-EN12-VESPA 2003) AIDS Care. 2006;18(3):254. doi: 10.1080/09540120500456193. [DOI] [PubMed] [Google Scholar]
- Pettigrew TF, Tropp LR. How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. European Journal of Social Psychology. 2008;38(6):922–934. [Google Scholar]
- Rosner D. “Spanish flu, or whatever it is. …”: The paradox of public health in a time of crisis. Public Health Reports. 2010;125(3):38–10. [PMC free article] [PubMed] [Google Scholar]
- Stevenson RJ, Repacholi BM. Does the source of an interpersonal odour affect disgust? A disease risk model and its alternatives. European Journal of Social Psychology. 2005;35(3):375–401. [Google Scholar]
- Taubenberger JK, Morens DM. Influenza: The once and future pandemic. Public Health Reports. 2010;125(3):16–11. [PMC free article] [PubMed] [Google Scholar]
- Tomes N. “Destroyer and teacher”: Managing the masses during the 1918–1919 influenza pandemic. Public Health Reports. 2010;125(3):48–15. doi: 10.1177/00333549101250S308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tybur JM, Lieberman D, Griskevicius V. Microbes, mating, and morality: Individual differences in three functional domains of disgust. Journal of Personality and Social Psychology. 2009;97(1):103–122. doi: 10.1037/a0015474. [DOI] [PubMed] [Google Scholar]
- Updated CDC estimates of 2009 H1N1 influenza cases, hospitalizations and deaths in the United States, April 2009 – April 10, 2010. 2010 Retrieved 7/20, 2010, from http://www.cdc.gov/h1n1flu/estimates_2009_h1n1.htm.
- Van Rie A, Sengupta S, Pungrassami P, Balthip Q, Choonuan S, Kasetjaroen Y, et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: Exploratory and confirmatory factor analyses of two new scales. Tropical Medicine and International Health. 2008;13(1):21–30. doi: 10.1111/j.1365-3156.2007.01971.x. [DOI] [PubMed] [Google Scholar]
- Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS and Behavior. 2006;10:473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook MT, Legge V, Pennay M. Attitudes towards disabilities in a multicultural society. Social Science & Medicine. 1993;36(5):615–623. doi: 10.1016/0277-9536(93)90058-c. [DOI] [PubMed] [Google Scholar]
- Wong E. The New York Times. 2009. Nov 12, China’s tough policy seems to slow swine flu’s spread; p. 3. [Google Scholar]