Abstract
Objectives:
The aim of this prospective study was to compare the impact of using two-dimensional (2D) panoramic radiographs and three-dimensional (3D) cone beam CT for the surgical treatment planning of impacted maxillary canines.
Methods:
This study consisted of 32 subjects (19 females, 13 males) with a mean age of 25 years, referred for surgical intervention of 39 maxillary impacted canines. Initial 2D panoramic radiography was available, and 3D cone beam CT imaging was obtained upon clinical indication. Both 2D and 3D pre-operative radiographic diagnostic sets were subsequently analysed by six observers. Perioperative evaluations were conducted by the treating surgeon. McNemar tests, hierarchical logistic regression and linear mixed models were used to explore the differences in evaluations between imaging modalities.
Results:
Significantly higher confidence levels were observed for 3D image-based treatment plans than for 2D image-based plans (p < 0.001). The evaluations of canine crown position, contact relationship and lateral incisor root resorption were significantly different between the 2D and 3D images. By contrast, pre- and perioperative evaluations were not significantly different between the two image modalities.
Conclusions:
Surgical treatment planning of impacted maxillary canines was not significantly different between panoramic and cone beam CT images.
Keywords: cuspid, impacted, teeth, panoramic, cone beam CT
Introduction
The incidence of impacted maxillary canines varies from 1% to 3%.1,2 The percentage of palatally and buccally impacted canines also varies widely, according to studies in the literature. The majority of canine impactions are located palatally in Caucasians2,3 and buccally in Asian populations.4 Proper clinical and radiographical diagnosis of impacted canines before and during treatment is critically important for treatment planning and stable results with minimal complications. With delayed eruption of maxillary canines, the radiological examination serves to determine the position and spatial context. Using this evaluation, clinicians can assess the chance of a normal eruption or create an adequate therapeutic plan. Another important factor in treatment planning is the presence and extent of external root resorption in the adjacent incisors.5
A radiographic examination is an essential part of the diagnostic process when an impacted canine is involved. Several two-dimensional (2D) radiographic techniques have been used for the differential diagnosis of canine impaction, including panoramic, periapical, occlusal and cephalometric radiographs, or a combination of these approaches.1,2 The parallax technique has been used combining different 2D radiographs: two intraoral periapical radiographs with different projection angulations [same lingual opposite buccal (SLOB) rule], periapical with occlusal radiographs and panoramic with occlusal radiographs.6 A potential difference in the assessment of canine location and the risks involved can be seen in comparison with a combined set of 2D radiographs (panoramic and two periapical or occlusal) and single panoramic images. Although more accurate localization was found in some studies,7,8 other studies indicated that single panoramic images may be as clinically useful as combined image data sets themselves.9–14 In addition, the diagnostic ability of single panoramic radiographs for canine localization and in combination with occlusal radiographs showed no significant difference between the techniques.6
Patients with impacted canines present treatment challenges. In the absence of early diagnosis and prevention, the impacted canine usually requires a combination of multidisciplinary interventions to bring it into occlusion. Several methods have been used for the treatment of impacted canines, including interceptive treatment by extracting the primary canine alone,15 surgical exposure with or without attachment,16 autotransplantation17 and canine extraction. Previous studies of treatment planning were conducted based on 2D radiographic procedures. Radiographic factors and treatment methods have been correlated with the length of treatment by several authors.16,18–20 However, predicting the treatment duration associated with impacted canines is difficult.20 The angulations and position of the canines in the dental arch, the overlap between the lateral incisor and canine and the presence of root anomalies have all been discussed as having a role in the treatment decision.18,21,22
Using low-dose cone beam CT (CBCT) images to assess the impacted canine in a three-dimensional (3D) representation has shown clear benefits for both diagnosis and prognostic estimates on eruption as well as treatment planning.23–26 Most studies have compared conventional radiology and CBCT, showing a superiority of CBCT in assessing the exact position of impacted canines.24,27,28 Haney et al27 evaluated the difference between a 2D data set (including panoramic, occlusal and two periapical radiographs) and CBCT images, and showed a discrepancy between the two sets in the assessment of both the position of the impacted canine and the type of treatment chosen.27 However, previous studies have not clearly explained the influence of 2D vs 3D diagnosis on the assessment of impacted canines and subsequent surgical management. The potential influence of CBCT on pre-surgical treatment planning has not yet been evaluated. Thus, the aim of this prospective study was to compare the impact of using 2D panoramic radiographs vs 3D CBCT for surgical treatment planning of impacted maxillary canines.
Materials and methods
Thirty-two subjects (19 females, 13 males; mean age 25, standard deviation 14 years) with impacted maxillary canines participated in the study. A total of 39 impacted maxillary canines were referred for surgical intervention because they had failed to erupt normally. 17 of the impacted maxillary canines were located on the right side (Tooth 13) and 22 on the left side (Tooth 23). The study protocol was approved by the medical ethics committee board of UZ-KU Leuven university, Leuven, Belgium (approval number: B32220083749, S50910).
Two sets of radiographs were obtained within a maximum interval of 6 weeks. The first set consisted of 2D panoramic radiographs, whereas the second set consisted of 3D volumetric images obtained from CBCT scans. All panoramic radiographs were taken with Veraviewepocs 2D® (J. Morita, Kyoto, Japan). The images were viewed and analysed with the Digora® software (Soredex, Tuusula, Finland). The CBCT analyses were conducted using a 3D Accuitomo-XYZ Slice View Tomograph® (J. Morita). The CBCT images were analysed using i-Dixel One Data Viewer Version 1.27 software (J. Morita).
In this study, all patients were referred for a CBCT examination because 3D visualization of the canine relative to the adjacent teeth was clinically indicated to perform the treatment plan. CBCT images were taken whenever the canine was displaced from its normal position, or if it was very difficult to be localized, deeply impacted, horizontally impacted or associated with suspected root resorption on adjacent incisors. No patients received any additional radiographic exposure during this evaluation.
Pre-operative radiographic evaluation
A therapeutic decision for each case was made by six observers (four orthodontists and two oral surgeons), based on panoramic radiographs and CBCT radiographs. The panoramic and CBCT images were presented separately and in a random order with a 2 week interval. The observers accomplished the therapeutic plan and completed a questionnaire for the following parameters:
The observer's confidence in successful treatment planning and in performing a complete treatment without complications using the information provided. The following five-step confidence scale was used: (1) very confident, (2) confident, (3) no opinion, (4) doubtful/unsure, and (5) very doubtful/unsure.
Type of treatment, including simple surgical exposure of the canine, surgical exposure with attachment, and canine extraction.
Open or closed eruption technique.
Permanent maxillary canine crown position in the sagittal plane relative to the adjacent teeth (palatal, buccal or in line with the arch).
The position of the permanent maxillary canine in the axial plane relative to the occlusal plane (high, close to the apical third of the lateral incisor root; medium, near the middle third of the lateral incisor root; and low, near the coronal third of the lateral incisor root).
Contact relationship between the canine and the adjacent teeth. The contact relationship between the permanent maxillary canines and incisors was assigned to one of the following two categories:29 (1) contact, indicated by a distance between the crown of the permanent maxillary canine and the adjacent incisors of less than 1 mm; and (2) no contact, indicated by a distance between the crown of the permanent maxillary canine and adjacent incisors of greater than or equal to 1 mm.
Presence of root resorption in the adjacent lateral incisors.
Prediction of complications, including infection, swelling and bleeding.
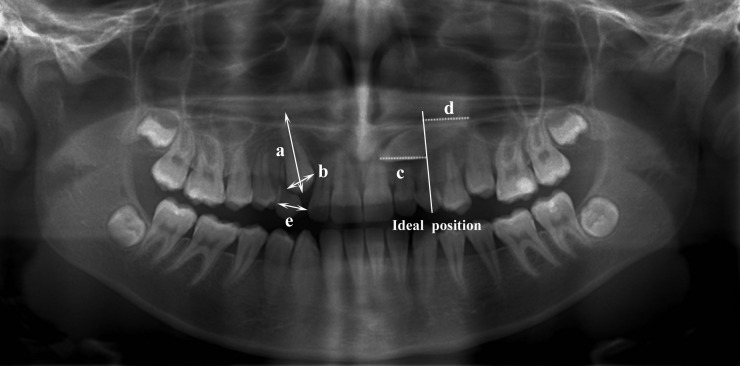
Linear measurements (in millimeters) were obtained by three observers (two orthodontists and one surgeon) for the following values: (A) the total canine length (i.e. the distance from the canine cusp tip to the apex), (B) canine crown width, (C) distance from the canine cusp tip perpendicular to the axis of the ideal position, (D) distance from the canine apex perpendicular to the axis of the ideal position and (E) mesiodistal space (i.e. from the distal surface of the lateral incisor to the mesial surface of the first premolar) (Figure 1).
Figure 1.
Panoramic image of 15 year old female patient with bilateral impacted canine illustrating the reference lines of ideal canine position as well as the linear measurements as follows: (a) the canine total length from the canine cusp tip to the apex, (b) the canine crown width, (c) the distance from the canine cusp tip perpendicular to the axis of the ideal position, (d) the distance from the canine apex perpendicular to the axis of the ideal position and (e) the mesiodistal space from the distal surface of the lateral incisor to the mesial surface of the first premolar
Perioperative evaluation
During surgery, the operating surgeon used both image modalities, recorded the type of treatment chosen as well as the eruption technique and confirmed the type of canine impaction, canine location in sagittal and axial planes and prediction of complications. Root resorption of the lateral incisor and contact relationship between the impacted canine and adjacent teeth were not included because it was not possible to assess them during surgery.
After analysing the CBCT images, the surgeon was asked to express his opinion on the use of CBCT images for diagnosis and surgery. The following information was recorded: (1) whether the CBCT added valuable diagnostic information that would not have been obtained otherwise, (2) whether the surgical plan had changed because of the diagnostic information obtained from the CBCT images and (3) whether CBCT should be used to surgically treat canine impactions.
Statistical analysis
McNemar tests were used to explore the differences in evaluations between 2D and 3D imaging. However, these tests assumed 234 scores from 39 cases evaluated by 6 observers to be independent, an inappropriate assumption that artificially inflated the amount of information. Therefore, a hierarchical logistic regression model was used for the comparisons where a significant result was obtained with the McNemar test. Only binary models were used (i.e. evaluations with more than two levels were dichotomized). To account for the correlation in the data, the model contained random effects of the observer and the subject, as well as their interactions. Linear mixed models with the same random effects structure were used to compare measurements between 2D and 3D. p < 0.05 was considered significant.
All analyses were performed using SAS software v. 9.2 of the SAS System for Windows (SAS© Institute Inc, Cary, NC). The SAS GLIMMIX procedure was used to fit the hierarchical logistic regression models.
Results
The pre-operative radiographic evaluation of the treatment plans using panoramic radiographs (2D) and CBCT radiographs (3D) are shown in Table 1. The observers had a significantly higher level of confidence in their 3D image-based surgical treatment plans than in their 2D image-based plans (p < 0.001). The treatment decision regarding canine crown position in the sagittal and axial planes, contact relationship and presence of lateral incisor root resorption was significantly different when it was based on 2D than 3D information (Table 1). Root resorption of the lateral incisors was detected more often with CBCT images than with panoramic images (18% vs 11.5%, respectively). Regarding pre-surgical treatment planning, no significant differences were found for either the type of treatment chosen or the surgical technique and prediction of complications. However, CBCT was associated with fewer canine extractions than panoramic evaluation (13% vs 18%). Moreover, no significant correlations were found between CBCT and panoramic radiographs regarding the type of treatment chosen (e.g. simple surgical exposure with or without attachment and canine extraction), regarding the eruption technique chosen (e.g. open or closed eruption) and other diagnostic factors.
Table 1.
Pre-operative radiographic evaluation of treatment planning and differences between two-dimensional panoramic imaging and three-dimensional CBCT
| Parameters | Categories | Panoramic | CBCT | p-value |
| Confidence level in treatment planning | Very convinced | 3.9 | 40.6 | <0.0001 |
| Convinced | 26.1 | 47.5 | ||
| No opinion | 5.9 | 4.7 | ||
| Doubtful | 49.6 | 5.9 | ||
| Very doubtful | 14.5 | 1.3 | ||
| Type of treatment | Simple surgical exposure | 6.5 | 8.1 | NS |
| Surgical exposure with attachment | 75.6 | 79.1 | ||
| Canine extraction | 17.9 | 12.8 | ||
| Technique | Open | 93.9 | 86.9 | NS |
| Closed | 6.1 | 13.1 | ||
| Canine crown position in sagittal plane | Buccal | 26.2 | 20.2 | 0.002 |
| Palatal | 64.4 | 61.4 | ||
| Close to the line arch | 9.4 | 18.4 | ||
| Canine crown position in axial plane | High | 30.3 | 29.0 | 0.005 |
| Medium | 51.7 | 43.6 | ||
| Low | 18.0 | 27.4 | ||
| Contact relationship | Contact | 81.6 | 89.7 | 0.008 |
| No contact | 18.4 | 10.3 | ||
| Resorption of lateral incisors | Resorption | 11.5 | 18.0 | 0.025 |
| No resorption | 88.5 | 82.0 | ||
| Prediction of complication | Complication | 17.5 | 25.6 | NS |
| No complication | 82.5 | 74.4 |
CBCT, cone beam CT; NS, not significant (p > 0.05).
Values are percentages of the 234 scores (6 observers, 39 cases).
The mean, median and standard deviation values, as well as the systematic differences for the linear measurements, are shown in Table 2. The linear measurements of the width of the canine crowns, the canine root length and the distance between the canine apex and the ideal were significantly different between the two imaging modalities.
Table 2.
Descriptive information and the differences between linear measurements (in millimeters) using two-dimensional panoramic imaging and three-dimensional CBCT
| Parameters | Values | Panoramic | CBCT | p-value |
| Canine total length | Mean | 14.6 | 14.2 | 0.04 |
| Median | 14.4 | 14.2 | ||
| SD | 2.5 | 2.3 | ||
| Canine crown width | Mean | 7.7 | 7.4 | 0.03 |
| Median | 7.3 | 7.4 | ||
| SD | 1.7 | 0.9 | ||
| Distance from cusp tip of canine to ideal axis | Mean | 6.3 | 5.8 | NS |
| Median | 5.2 | 4.6 | ||
| SD | 4.5 | 3.9 | ||
| Distance from apex of canine to ideal axis | Mean | 7.1 | 8.1 | 0.002 |
| Median | 6.3 | 6.7 | ||
| SD | 4.4 | 5.4 | ||
| Mesiodistal space | Mean | 4.9 | 4.8 | NS |
| Median | 5.8 | 5.8 | ||
| SD | 3.1 | 2.9 |
CBCT, cone beam CT; NS, not significant (p > 0.05); SD, standard deviation.
Table 3 displays the percentage of correct agreement between the pre- and perioperative evaluations and decisions related to treatment planning. This agreement was not significantly different between panoramic and CBCT images.
Table 3.
Correct agreement (expressed in percentages) between pre-operative treatment planning and perioperative treatment information when using two-dimensional panoramic imaging vs three-dimensional CBCT. None of these comparisons was significantly different (p > 0.05)
| Parameters | Categories | Panoramic | CBCT |
| Type of treatment | Simple surgical exposure | 0.4 | 0.9 |
| Surgical exposure with attachment | 51.7 | 51.7 | |
| Canine extraction | 13.3 | 8.1 | |
| Technique | Open | 78.2 | 75.2 |
| Closed | 3.0 | 6.8 | |
| Canine crown position in sagittal plane | Buccal | 5.2 | 7.3 |
| Palatal | 42.9 | 46.6 | |
| Close to the line arch | 6.4 | 7.3 | |
| Canine crown position in axial plane | High | 16.7 | 15.0 |
| Medium | 25.2 | 20.9 | |
| Low | 8.6 | 12.0 | |
| Prediction of complication | Complication | 3.9 | 6.4 |
| No complication | 58.1 | 52.6 |
CBCT, cone beam CT.
Values are percentages of the 234 scores (6 observers, 39 cases).
After evaluating the CBCT images, the treated surgeon considered the extra diagnostic information to be valuable in 92.3% (36/39) of the cases. Changes in the therapeutic plan occurred in 79.5% (31/39) of the cases when 3D information was obtained instead of panoramic information alone. CBCT was recommended in 61.5% (24/39) of canine impaction cases.
Discussion
It is important to consider the advantages of CBCT in canine localization and its impact on patient management. Therefore, the potential improvement in the surgical management of patient with the use of CBCT imaging warrants investigation. This prospective study was carried out on patients who had both 2D panoramic and 3D CBCT images and focused on surgical treatment planning based on radiographic information and factors that may affect surgical decisions.
For many years, conventional radiography was regarded as the standard technique for the diagnosis and treatment planning for impacted canines. In this study, panoramic images were chosen to represent conventional 2D radiographs because patients frequently obtain them before undergoing routine treatment for impacted canines. Several studies have compared the diagnostic information gained from panoramic vs CBCT radiography, using sectors, linear and angular measurements.13,14,30 The limitations of panoramic radiographs are well known; these include the distortion of anatomical structures, projection errors, blurred images and inaccuracies in complex 3D maxillofacial structures projected onto a 2D plane, all of which may increase the risk of misinterpretation.31,32 However, much debate exists regarding the utility of panoramic radiographs for canine localization.7–14 Reports in the literature state that when clinical information is insufficient to identify the position of the impacted canines, a 2D imaging technique such as a panoramic radiograph should be supplemented by another radiograph.2 A study by Jung et al14 correlated the diagnostic positions of panoramic with those of CBCT radiographs of impacted maxillary canines. The results showed that the panoramic radiographs were useful for predicting canine buccolingual locations based on sectors.14 Impacted canine angulation was also used to differentiate the canine positions based on panoramic radiographs.13 Differences between the present study and others, owing to the localization of canine position based on sector and angular measurements, were not evaluated.
Other studies have compared the diagnosis and treatment planning based on CBCT images with those based on 2D panoramic images in combination with a lateral cephalogram, available periapical radiographs and/or a dental cast.24,27,28 The results indicated that information from CBCT was superior to that obtained from conventional 2D radiographs, which may affect treatment planning.24,27 This study, however, did not focus on treatment opinions or treatment planning. Therefore, lateral cephalograms were not used because of insufficient information related to canine impaction caused by superimposition (i.e. mainly in the case of bilateral impaction) and because they had the same limitations as panoramic images for diagnosis of the presence or absence of root resorption of the adjacent lateral incisors. Two intraoral periapical radiographs were not used because of limitations such as the small field of view. When the canines were bilaterally impacted, four periapical radiographs were needed for each patient, which was considered to be unjustified. In addition, intraoral 2D images are subject to the same constraints as panoramic imaging and have been found to be an inaccurate diagnostic tool for the detection of root resorption of the adjacent incisor.33 Furthermore, the combination with the 2D radiographs was not used in this study because two periapical radiographs are insufficient to provide the vertical canine crown location, or the canine apex relative to the surrounding structures, and cannot be reproduced accurately with the same angulation projections for all patients referred for surgery.34 Moreover, these radiographs, according to the SLOB rule, were largely intended for canine crown localization instead of detection of root resorption on the adjacent incisors. By contrast, since CBCT was introduced at our centre (2004), it has replaced other modalities in cases requiring additional radiographs for impacted canines. As a result, unnecessary radiation has been avoided via optimization and low-dose exposures.
Linear measurements were included in comparisons between panoramic and CBCT images because they were frequently used as comparative parameters for radiological assessment.22,35,36 Several authors have suggested that linear measurements are reliable in panoramic radiographs for the assessment of correct patient position.37,38 All panoramic images in this study were acquired with patients in standardized positions and were performed by experienced technical operators. In our previous study, panoramic radiographs were found to be less reliable, resulting in lower measurement accuracy and less agreement compared with CBCT images for different diagnostic tasks related to canine impaction.30 Moreover, in agreement with our findings, CBCT had better agreement than panoramic radiography regarding canine position and the detection of external root resorption of adjacent lateral incisors.30,39
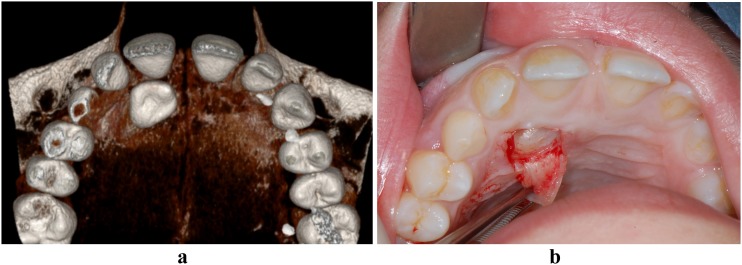
In this study, the observers had a higher level of confidence in their CBCT image-based therapy plans than in their 2D radiograph-based plans. The treatment of canine impaction was influenced by canine location, contact with adjacent teeth and the site and severity of the root lesion, all of which were significantly different between the panoramic and CBCT images. Moreover, the exact location of the impacted canines in the 3D images (i.e. sagittal, coronal and axial) and their contact with adjacent teeth allowed the clinicians to determine the direction of traction to avoid injury to adjacent teeth as well as better surgical access (Figures 2 and 3). Confidence in the therapeutic plan was also influenced by the presence and severity of root resorption, although confidence decreased when the type of treatment was chosen based on 2D radiographic images. Bjerklin and Ericson40 found a treatment approach adapted when additional 3D information was available, based on the extent of root resorption present on the maxillary lateral incisors.
Figure 2.
Two-dimensional panoramic radiograph of a 15 year old female with an impacted maxillary right canine. The root contours of the central and lateral incisors overlap with that of the canine. The canine crown is magnified indicating that it is palatally impacted with the exact location for surgical intervention is very difficult to assess
Figure 3.
(a) Three-dimensional cone beam CT image from the 3D Accuitomo-XYZ Slice View Tomograph® system (J. Morita, Kyoto, Japan) showing the exact location of the right maxillary canine. (b) Occlusal intraoral photograph showing the crown of the impacted upper right maxillary canine during surgery
In the pre-operative evaluations, no significant difference was observed between 2D and 3D information regarding the type of treatment chosen (e.g. surgical exposure with or without attachment and canine extraction) or regarding eruption technique (e.g. open vs closed eruption). One possible reason is that surgical treatment is normally based on the surgeon's personal preference and experience regarding the best surgical approach.41 Moreover, proposed treatments for impacted canines did not differ, whether based on 2D or 3D images, in agreement with our findings.28
There were no statistically significant differences in agreement between the pre- and perioperative surgical plans between the two imaging modalities. The perioperative evaluation was used as a reference standard for comparison of what was planned pre-operatively (by six observers) and the treatment that actually occurred during surgery. Surgery was performed by an independent surgeon who completed the clinical examination autonomously and had access to all available image modalities that represented normal clinical practice. The same questionnaire was completed pre- and perioperatively. Therefore, the confidence level was not assessed based on the perioperative evaluation because the operating surgeon used both panoramic and CBCT images during surgery. Moreover, root resorption of the lateral incisor and the contact relationship between the canine and adjacent teeth were difficult to assess during surgery. Consequently, the assessments of root resorption and contact relationship were not included in the perioperative evaluation.
The present study aimed to quantify the value of CBCT scans. The focus was put on surgical treatment planning and was unable to demonstrate a significant difference between the use of panoramic and CBCT radiographs for surgical treatment planning of impacted maxillary canine. A fundamental goal of this study was to understand the relative value of CBCT compared with panoramic radiographs and to aid in the justification of using CBCT for patients referred for surgical intervention.
Pre-surgical treatment planning did not differ significantly between panoramic and CBCT modalities in terms of the type of treatment chosen, surgical technique and the prediction of complications. Moreover, the agreements between pre- and perioperative evaluations and decisions related to treatment planning did not differ significantly whether panoramic or CBCT images were used. Compared with panoramic radiographs, CBCT images helped to increase the confidence level of the clinician regarding treatment planning, diagnosis of the canine location, contact with the adjacent teeth and the presence of root resorption.
Funding
The research leading to these results has received funding from the European Atomic Energy Community's Seventh Framework Program FP7/2007-2011 under grant agreement no. 212246 (SEDENTEXCT: Safety and Efficacy of a New and Emerging Dental X-ray Modality).
References
- 1.Bishara SE. Impacted maxillary canines: a review. Am J Orthod Dentofacial Orthop 1992; 101: 159–171 [DOI] [PubMed] [Google Scholar]
- 2.Ericson S, Kurol J. Radiographic examination of ectopically erupting maxillary canines. Am J Orthod Dentofacial Orthop 1987; 91: 483–492 [DOI] [PubMed] [Google Scholar]
- 3.Peck S, Peck L, Kataja M. The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod 1994; 64: 249–256 [DOI] [PubMed] [Google Scholar]
- 4.Kim Y, Hyun HK, Jang KT. The position of maxillary canine impactions and the influenced factors to adjacent root resorption in the Korean population. Eur J Orthod 2012; 34: 302–306 10.1093/ejo/cjr002 [DOI] [PubMed] [Google Scholar]
- 5.Alqerban A, Jacobs R, Lambrechts P, Loozen G, Willems G. Root resorption of the maxillary lateral incisor caused by impacted canine: a literature review. Clin Oral Investig 2009; 13: 247–255 10.1007/s00784-009-0262-8 [DOI] [PubMed] [Google Scholar]
- 6.Mason C, Papadakou P, Roberts GJ. The radiographic localization of impacted maxillary canines: a comparison of methods. Eur J Orthod 2001; 23: 25–34 [DOI] [PubMed] [Google Scholar]
- 7.Nagpal A, Pai KM, Setty S, Sharma G. Localization of impacted maxillary canines using panoramic radiography. J Oral Sci 2009; 51: 37–45 [DOI] [PubMed] [Google Scholar]
- 8.Chalakkal P, Thomas AM, Chopra S. Reliability of the magnification method for localisation of ectopic upper canines. Aust Orthod J 2009; 25: 59–62 [PubMed] [Google Scholar]
- 9.Lindauer SJ, Rubenstein LK, Hang WM, Andersen WC, Isaacson RJ. Canine impaction identified early with panoramic radiographs. J Am Dent Assoc 1992; 123: 91–97 [DOI] [PubMed] [Google Scholar]
- 10.Chaushu S, Chaushu G, Becker A. The use of panoramic radiographs to localize displaced maxillary canines. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88: 511–516 [DOI] [PubMed] [Google Scholar]
- 11.Gavel V, Dermaut L. The effect of tooth position on the image of unerupted canines on panoramic radiographs. Eur J Orthod 1999; 21: 551–560 [DOI] [PubMed] [Google Scholar]
- 12.Sudhakar S, Patil K, Mahima VG. Localization of impacted permanent maxillary canine using single panoramic radiograph. Indian J Dent Res 2009; 20: 340–345 10.4103/0970-9290.57381 [DOI] [PubMed] [Google Scholar]
- 13.Katsnelson A, Flick WG, Susarla S, Tartakovsky JV, Miloro M. Use of panoramic x-ray to determine position of impacted maxillary canines. J Oral Maxillofac Surg 2010; 68: 996–1000 10.1016/j.joms.2009.09.022 [DOI] [PubMed] [Google Scholar]
- 14.Jung YH, Liang H, Benson BW, Flint DJ, Cho BH. The assessment of impacted maxillary canine position with panoramic radiography and cone beam CT. Dentomaxillofac Radiol 2012; 41: 356–360 10.1259/dmfr/14055036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ericson S, Kurol J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod 1988; 10: 283–295 [DOI] [PubMed] [Google Scholar]
- 16.Iramaneerat S, Cunningham SJ, Horrocks EN. The effect of two alternative methods of canine exposure upon subsequent duration of orthodontic treatment. Int J Paediatr Dent 1998; 8: 123–129 [DOI] [PubMed] [Google Scholar]
- 17.Patel S, Fanshawe T, Bister D, Cobourne MT. Survival and success of maxillary canine autotransplantation: a retrospective investigation. Eur J Orthod 2011; 33: 298–304 10.1093/ejo/cjq071 [DOI] [PubMed] [Google Scholar]
- 18.Stewart JA, Heo G, Glover KE, Williamson PC, Lam EW, Major PW. Factors that relate to treatment duration for patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop 2001; 119: 216–225 10.1067/mod.2001.110989 [DOI] [PubMed] [Google Scholar]
- 19.Zuccati G, Ghobadlu J, Nieri M, Clauser C. Factors associated with the duration of forced eruption of impacted maxillary canines: a retrospective study. Am J Orthod Dentofacial Orthop 2006; 130: 349–356 10.1016/j.ajodo.2004.12.028 [DOI] [PubMed] [Google Scholar]
- 20.Fleming PS, Scott P, Heidari N, Dibiase AT. Influence of radiographic position of ectopic canines on the duration of orthodontic treatment. Angle Orthod 2009; 79: 442–446 10.2319/042708-238.1 [DOI] [PubMed] [Google Scholar]
- 21.Motamedi MH, Tabatabaie FA, Navi F, Shafeie HA, Fard BK, Hayati Z. Assessment of radiographic factors affecting surgical exposure and orthodontic alignment of impacted canines of the palate: a 15-year retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 772–775 10.1016/j.tripleo.2008.12.022 [DOI] [PubMed] [Google Scholar]
- 22.Stivaros N, Mandall NA. Radiographic factors affecting the management of impacted upper permanent canines. J Orthod 2000; 27: 169–173 [DOI] [PubMed] [Google Scholar]
- 23.Chaushu S, Chaushu G, Becker A. The role of digital volume tomography in the imaging of impacted teeth. World J Orthod 2004; 5: 120–132 [PubMed] [Google Scholar]
- 24.Botticelli S, Verna C, Cattaneo PM, Heidmann J, Melsen B. Two-versus three-dimensional imaging in subjects with unerupted maxillary canines. Eur J Orthod 2011; 33: 344–349 10.1093/ejo/cjq102 [DOI] [PubMed] [Google Scholar]
- 25.Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2005; 128: 418–423 10.1016/j.ajodo.2004.04.033 [DOI] [PubMed] [Google Scholar]
- 26.Liu DG, Zhang WL, Zhang ZY, Wu YT, Ma XC. Localization of impacted maxillary canines and observation of adjacent incisor resorption with cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105: 91–98 10.1016/j.tripleo.2007.01.030 [DOI] [PubMed] [Google Scholar]
- 27.Haney E, Gansky SA, Lee JS, Johnson E, Maki K, Miller AJ, et al. Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am J Orthod Dentofacial Orthop 2010; 137: 590–597 [DOI] [PubMed] [Google Scholar]
- 28.Wriedt S, Jaklin J, Al-Nawas B, Wehrbein H. Impacted upper canines: examination and treatment proposal based on 3D versus 2D diagnosis. J Orofac Orthop 2012; 73: 28–40 10.1007/s00056-011-0058-8 [DOI] [PubMed] [Google Scholar]
- 29.Ericson S, Bjerklin K, Falahat B. Does the canine dental follicle cause resorption of permanent incisor roots? A computed tomographic study of erupting maxillary canines. Angle Orthod 2002; 72: 95–104 [DOI] [PubMed] [Google Scholar]
- 30.Alqerban A, Jacobs R, Fieuws S, Willems G. Comparison of two cone beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. Eur J Orthod 2011; 33: 93–102 10.1093/ejo/cjq034 [DOI] [PubMed] [Google Scholar]
- 31.Ericson S, Kurol J. Incisor resorption caused by maxillary cuspids. A radiographic study. Angle Orthod 1987; 57: 332–346 [DOI] [PubMed] [Google Scholar]
- 32.Elefteriadis JN, Athanasiou AE. Evaluation of impacted canines by means of computerized tomography. Int J Adult Orthodon Orthognath Surg 1996; 11: 257–264 [PubMed] [Google Scholar]
- 33.Follin ME, Lindvall AM. Detection of lingual root resorptions in the intraoral radiographs. An experimental study. Swed Dent J 2005; 29: 35–42 [PubMed] [Google Scholar]
- 34.Becker A, Chaushu S, Casap-Caspi N. Cone-beam computed tomography and the orthosurgical management of impacted teeth. J Am Dent Assoc 2010; 141(Suppl. 3): 14S–18S [DOI] [PubMed] [Google Scholar]
- 35.Ericson S, Kurol J. Resorption of maxillary lateral incisors caused by ectopic eruption of the canines. A clinical and radiographic analysis of predisposing factors. Am J Orthod Dentofacial Orthop 1988; 94: 503–513 [DOI] [PubMed] [Google Scholar]
- 36.Power SM, Short MB. An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. Br J Orthod 1993; 20: 215–223 [DOI] [PubMed] [Google Scholar]
- 37.Volchansky A, Cleaton-Jones P, Drummond S, Bonecker M. Technique for linear measurement on panoramic and periapical radiographs: a pilot study. Quintessence Int 2006; 37: 191–197 [PubMed] [Google Scholar]
- 38.Laster WS, Ludlow JB, Bailey LJ, Hershey HG. Accuracy of measurements of mandibular anatomy and prediction of asymmetry in panoramic radiographic images. Dentomaxillofac Radiol 2005; 34: 343–349 10.1259/dmfr/28020783 [DOI] [PubMed] [Google Scholar]
- 39.Alqerban A, Jacobs R, Souza PC, Willems G. In-vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am J Orthod Dentofacial Orthop 2009; 136764 e1–11 [DOI] [PubMed] [Google Scholar]
- 40.Bjerklin K, Ericson S. How a computerized tomography examination changed the treatment plans of 80 children with retained and ectopically positioned maxillary canines. Angle Orthod 2006; 76: 43–51 10.1043/0003-3219(2006)076[0043:HACTEC]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 41.Parkin N, Benson PE, Thind B, Shah A. Open versus closed surgical exposure of canine teeth that are displaced in the roof of the mouth. Cochrane Database Syst Rev 2008; CD006966 10.1002/14651858.CD006966.pub2 [DOI] [PubMed] [Google Scholar]