Abstract
Objectives:
To evaluate the effect on diagnostic yield in the detection of experimentally induced vertical root fractures on cone beam CT images using four dental software program.
Methods:
190 single-rooted extracted human teeth were divided into three groups according to the pulp canal status: unrestored (UR), filled with gutta-percha (GP) and restored with a metallic custom post (Post). One-half of the sample of each group was artificially fractured and the segments repositioned. All teeth were scanned on a cone beam CT device at 0.2 mm nominal voxel resolution (i-CAT Platinum; Imaging Sciences International, Hatfield, PA). The data were exported as digital imaging and communications in medicine files and imported into Dolphin Imaging & Management Solutions, v. 11.5 (Patterson Dental Supply Inc., St Paul, MN), InVivoDental, v. 5.0 (Anatomage Inc., San Jose, CA) and Kodak Dental Imaging Software 3D module, v. 2.1.11 (Carestream Health Inc., Rochester, NY) software. Cross-sectional images in the acquisition (using Xoran CAT™, v. 3.0.34 software; Xoran Technologies, Ann Arbor, MI) and additional software were presented to three calibrated oral radiologists who rated the presence or absence of root fracture on a five-point scale. Receiver operating characteristic analysis was performed, and treatment comparisons compared by analysis of variance and pairwise comparisons were performed using Tukey's test at an a priori value of α < 0.05%.
Results:
All dental software performed equally at detecting fractures. Fractures were significantly more difficult to detect when posts were present.
Conclusions:
The diagnosis of root fracture is software-independent. The presence of an intracanal metallic post significantly decreases the detection of artificially created root fractures.
Keywords: cone beam CT, reconstruction software, DICOM, root fracture, diagnostic tests
Introduction
Radiographical examinations are an essential component in all stages of endodontic therapy, including at diagnosis, interoperatively and in the evaluation of the final root canal filling and monitoring or healing.1 Cone beam CT (CBCT) provides practitioners with multiplanar visualization in all three dimensions through the use of dental-specific software applications that have a relatively simple interface.2
After data acquisition, images are usually displayed in the proprietary software of the CBCT equipment, initially as secondary reconstructed images in three orthogonal planes (axial, sagittal and coronal), usually at a thickness defaulted to the native resolution.3 Sometimes this software is available only on the computer directly connected to the scanner or may require a special key for activation. However, CBCT images can be exported in the third-party proprietary and also non-proprietary digital imaging and communications in medicine (DICOM) file format standard, allowing the use of public domain image processing software.
The DICOM standard provides a detailed specification for formatting and exchanging images and associated metadata information, so images from different digital imaging devices can be read on single software. Because it was developed for advanced images, such as multislice CT and MRI, the sequence of primary images need to be in one of the orthogonal directions. Considering that CBCT-basis images are similar to lateral and posterior–anterior “cephalometric” radiographical images,3 it is necessary to modify them before exporting to DICOM. For that, the proprietary software processes the images as follows: the image base is compressed in a volume, which is resegmented as primary axial reconstructions, to be compressed as a DICOM file. Currently, there are many third-party software applications able to process DICOM files and provide useful tools in different areas of dentistry, such as zoom, visual adjustments (greyscale, brightness and contrast), insertion of annotations and measurements, and three-dimensional (3D) reconstructions.1,3
The diagnostic ability of CBCT for endodontics has been described by many authors and is superior to analogue or digital intraoral radiography for the detection of dental periapical lesions and demonstrates high sensitivity and specificity in detecting dental root resorption.4–7 Much research has been performed on the use of CBCT in the detection of root fractures, which remains a diagnostic challenge.8–20 Although there is a low incidence of root fractures (approximately 0.5–10.1% in the permanent dentition), longitudinal fractures are increasingly common as a result of the greater longevity of patients, retention of more teeth and greater complexity of dental procedures.8,21,22 Previous studies related to two-dimensional conventional analogue and digital intraoral radiography might well have underestimated the incidence. Further, the materials used in dental restorative procedures, such as gutta-percha, metal posts, prosthetic crowns and restorations, can interfere with the visualization of fracture lines in CBCT images. Artefacts (e.g. streaking and beam hardening) are caused by high-density materials, affecting the quality and accuracy of the images.8,23 If the cause of the artefact is close to or associated with the tooth to be assessed, the resulting CBCT images may have decreased diagnostic values.4
Despite the variability of dental viewing software, there is a dearth of information on the relative diagnostic with regards to specific tasks.24 As third-party software uses different reconstruction algorithms, it is important to assess how each software program behaves when processing data that exhibit structures potentially causing artefacts. The aim of this study was to assess the effect of segmentation and image reconstruction of CBCT data by four software program in the diagnostic ability of observers in the detection of vertical fractures with differing root canal contents.
Methods
The study protocol was reviewed and approved by the Institutional Review Board of The Campinas University School of Dentistry at Piracicaba, São Paulo, Brazil.
190 single-rooted unrestored extracted human teeth were included in the study. The sample size was calculated using a χ2 test and assuming a fracture incidence of 5% in the adult population. The reasons for extraction and the age and sex of the individuals who donated the samples were unknown. To be included in the sample, all teeth were previously inspected by transillumination for the absence of root fracture and by conventional periapical radiographs for the absence of obliterated root canal. After disinfection with 2% glutaraldehyde, each tooth had its root canal prepared with the ProTaper rotary system (Dentsply Maillefer, Ballaigues, Switzerland) until it was size F5. The teeth were then decoronated in the cement–enamel junction to eliminate any bias of enamel fractures.9,12 Finally, the teeth were randomly coded and divided into three groups according to the pulp canal status: (1) unrestored control group with no radio-opaque root canal material present (UR), (2) root canal filled with gutta-percha (GP) and (3) restored with a metallic custom post (Post).
The GP group had a passively well-fitting non-cemented ProTaper F5 gutta-percha cone placed in the canal of the teeth. The Post group had a passively well-fitting Type III gold alloy post casted and placed in the canal of other teeth. Periapical radiographs were made to validate the gutta-percha cone and post adaptations. Finally, cones and posts were removed to produce the fracture in one-half of the sample of each group.
Vertical root fractures were induced as described by Melo et al,13 adapted from Monaghan et al25. Each tooth from the experimental sample was coated with a layer of wax approximately 2 mm thick to protect its root surface, and the teeth were fixed in a mini-table lathe. A conical wedge with a bevelled tip was driven into the tooth apically, parallel to the buccal–lingual plane, and fractures were induced by using controlled pressure applied by gentle tapping. The fractured teeth were reinspected by transillumination to confirm the presence and morphology of the root fracture (Figure 1). 10 teeth were used to learn the force that was needed to break the root into two fragments and were excluded from the final sample. The root fragments were placed together in their original position. The proper gutta-percha cones or cast posts were reinserted in the teeth of the respective groups, with care taken not to displace the fragments. Because cement might have flowed to the fracture line, the cementation procedure was avoided.13 Thereafter, further periapical radiographs were taken to check the cone/post adaptation and possible fracture displacement (Figure 2).
Figure 1.
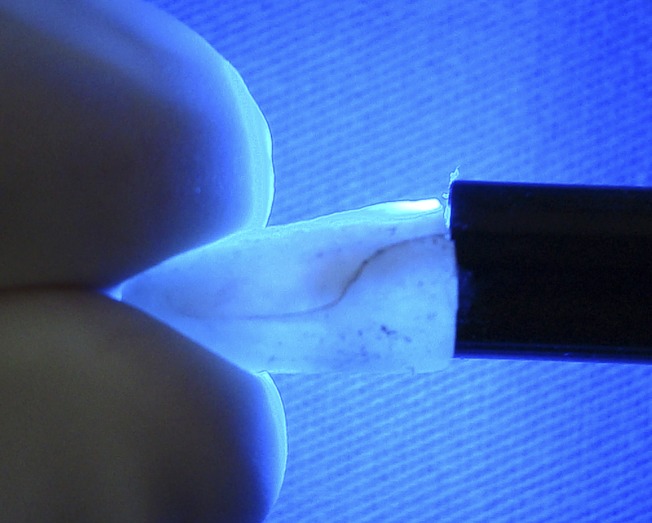
Transillumination confirming the presence of vertical root fracture (seen here as an oblique dark line running parallel to tooth longitudinal axis)
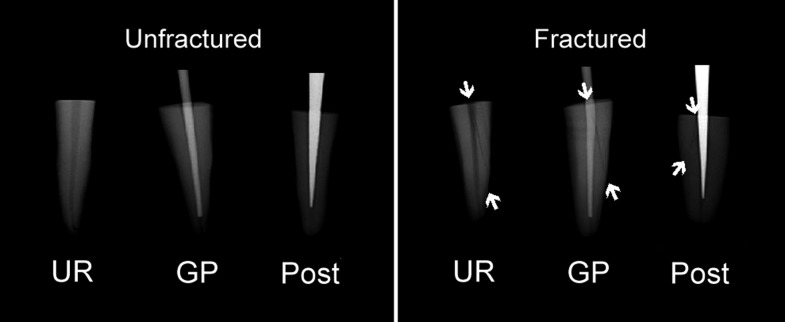
Figure 2.
Periapical radiographs taken to confirm cone/post adaptation in both unfractured and fractured teeth of all groups and to check possible fractured fragment displacement in related teeth. Arrows indicate the limits of fracture lines. gp, gutta-percha; Post, introcanal post; UR, unrestored
Before CBCT image acquisition, each tooth was uniformly coated with a 0.3 mm layer of utility wax to simulate the radiographical aspect of periodontal space7 and placed in an empty maxillary anterior socket of a dentate dry human skull (age and sex unknown). All teeth were placed with their buccal walls facing forward. The skull was coated with a 5 mm thick piece of wax to simulate the attenuation of soft tissues in the image.5 The CBCT images were obtained (i-CAT Platinum; Imaging Sciences International, Hatfield, PA) according to the protocol recommended by the manufacturer for a 0.2 mm voxel resolution (8 cm field of view, 120 kVp, 8 mA, 40 s for acquisition). Images were processed, saved originally in proprietary .xstd format and then exported in DICOM multifile format using Xoran software (Xoran CAT™, v. 3.0.34; Xoran Technologies, Ann Arbor, MI). The resultant CBCT DICOM images were imported into Dolphin (Dolphin Imaging & Management Solutions, v. 11.5; Patterson Dental Supply Inc., St. Paul, MN), KDIS3D (Kodak Dental Imaging Software 3D module, v. 2.1.11; Carestream Health Inc., Rochester, NY) and InVivo (InVivoDental, v. 5.0; Anatomage Inc., San Jose, CA) software.
The images for each tooth were reconstructed separately in all four software program (Dolphin, KDIS3D, InVivo and Xoran), and starting with the realignment of the tooth long axis parallel to the sagittal plane, the images were resliced orthogonally at 1 mm thickness in 1 mm contiguous slice increments. All resulting images were displayed on a 24-inch LCD monitor (MDRC-2124; Barco Inc., Duluth, GA) with a matrix resolution of 1920 × 1200. The images were coded and shown to the observers in a random order, and under dim-light conditions, in sets of 20 images. Each set was viewed separately by three observers, who performed a dynamic evaluation using all orthogonal slices (axial, coronal and sagittal). They could adjust brightness and contrast and use the zoom tool, but task-specific filters were not permitted. The observers were previously calibrated oral and maxillofacial radiologists with at least 10 years of experience in CT diagnosis. The calibration consisted of written and verbal instructions about CBCT image interpretation and the usage of the software, with examples of fractured roots in CBCT scans. The observer's evaluation was scored using a five-point confidence rating scale as follows: (1) fracture definitely not present, (2) fracture probably not present, (3) uncertain whether fracture is present or not, (4) fracture probably present, and (5) fracture definitely present. A total number of 2160 data points (180 teeth × 4 software × 3 observers) were collected.
Intraclass correlation coefficient was calculated to assess intraobserver and interobserver agreement and interpreted as follows: poor (0.00–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (>0.80). The diagnostic accuracy for each software program and observer was assessed by receiver operating characteristic (ROC) analysis. ROC analysis was performed by pooling observer responses for every software and condition. The Az values were compared by two-way repeated measures analysis of variance (ANOVA). Pairwise comparisons of Az values of four different software under three root-filling conditions were performed using Tukey's test. Data analyses were performed using SigmaStat® for Windows (v. 3.5; Systat Software Inc., Erkrath, Germany). The a priori level of significance was set at p < 0.05.
Results
Intraobserver coefficients ranged between fair and substantial agreement, whereas interobserver coefficients indicated moderate agreement (Table 1).
Table 1.
Intra- and interobserver intraclass correlation coefficient agreement for detection of vertical root fractures
| Group | Intraobserver | Interobserver | ||
| Observer 1 | Observer 2 | Observer 3 | ||
| UR | 0.62 | 0.73 | 0.67 | 0.54 |
| GP | 0.35 | 0.80 | 0.57 | 0.42 |
| Post | 0.40 | 0.73 | 0.37 | 0.40 |
| Overall | 0.46 | 0.76 | 0.56 | 0.47 |
GP, gutta-percha; Post, intracanal post; UR, unrestored.
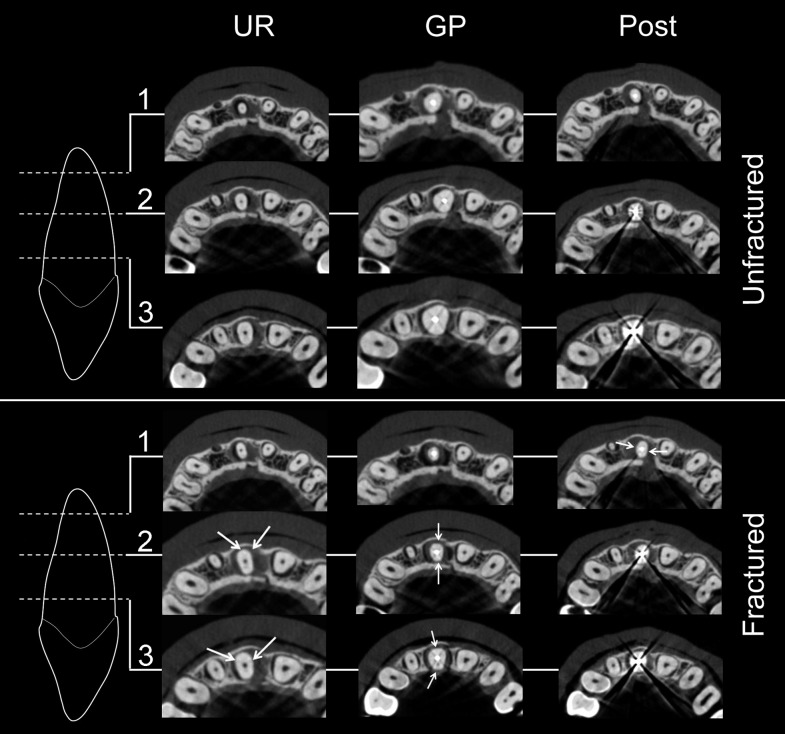
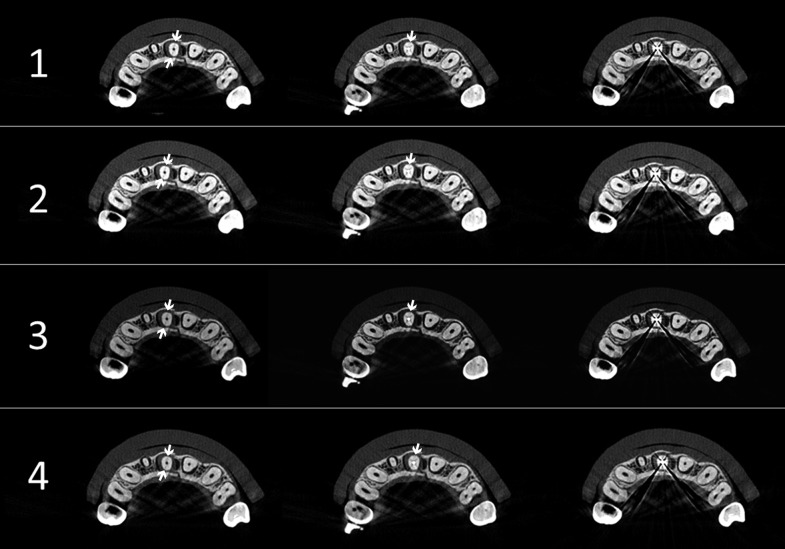
Figure 3 presents the reconstructed axial images of two different teeth in each group, seen in three different levels of the root length. Figure 4 presents the final reconstructed axial images of the same tooth in each group by all four software programs tested.
Figure 3.
Reconstructed axial images of six different teeth (one for each group and fracture status) seen in three levels of root length: (1) apical, (2) middle and (3) cervical. Arrows indicate the limits of detectable fracture lines
Figure 4.
Final reconstructed axial images of each group (columns) by all four software images tested: (1) Dolphin, (2) InVivo, (3) KDIS3D and (4) Xoran. Images of the same tooth in each group are presented on the columns: (left) UR, (centre) GP and (right) Post groups. Arrows indicate the limits of detectable fracture lines, although all teeth had a positive confirmation for fracture by transillumination. Dolphin (Dolphin Imaging & Management Solutions, v. 11.5) is manufactured by Patterson Dental Supply, Inc., St Paul, MN; InVivo (InVivoDental, v. 5.0) by Anatomage Inc., San Jose, CA; KDIS3D (Kodak Dental Imaging Software 3D module, v. 2.1.11) by Carestream Health Inc., Rochester, NY; and Xoran (Xoran CAT™, v. 3.0.34) by Xoran Technologies, Ann Arbor, MI
Data from each observation of three observers were pooled together. Table 2 summarises the results for overall sensitivity, specificity and accuracy for the diagnosis of vertical root fractures using each software program per experimental root filling group. Based on the observed means, Dolphin displayed the highest mean sensitivity for all observers combined but still close to the sensitivity recorded for the others. Specificity of InVivo images (89%) was higher than that of the Xoran images (87%) and the KDIS3D and Dolphin images (85% in both). The accuracy of all the software was very close: 73% for three (InVivo, Dolphin and Xoran) and 72% for one (KDIS3D).
Table 2.
Sensitivity, specificity and accuracy of each software program per experimental root filling group for diagnosis of vertical root fractures
| Group | Sensitivity | Specificity | Accuracy | |||||||||
| Dolphin | InVivo | KDIS3D | Xoran | Dolphin | InVivo | KDIS3D | Xoran | Dolphin | InVivo | KDIS3D | Xoran | |
| UN | 0.71 | 0.65 | 0.71 | 0.73 | 0.88 | 0.87 | 0.85 | 0.79 | 0.79 | 0.76 | 0.78 | 0.76 |
| GP | 0.68 | 0.61 | 0.63 | 0.61 | 0.81 | 0.91 | 0.78 | 0.91 | 0.74 | 0.76 | 0.70 | 0.76 |
| Post | 0.43 | 0.41 | 0.44 | 0.41 | 0.87 | 0.91 | 0.91 | 0.92 | 0.65 | 0.66 | 0.68 | 0.67 |
| Overall | 0.60 | 0.56 | 0.59 | 0.58 | 0.85 | 0.89 | 0.85 | 0.87 | 0.73 | 0.73 | 0.72 | 0.73 |
GP, gutta-percha; Post, intracanal post; UR, unrestored.
Means that are italicised are statistically different (p < 0.05).
Dolphin (Dolphin Imaging & Management Solutions, v. 11.5) is manufactured by Patterson Dental Supply, Inc., St Paul, MN; InVivo (InVivoDental, v. 5.0) by Anatomage Inc., San Jose, CA; KDIS3D (Kodak Dental Imaging Software 3D module, v. 2.1.11) by Carestream Health Inc., Rochester, NY; and Xoran (Xoran CAT™, v. 3.0.34) by Xoran Technologies, Ann Arbor, MI.
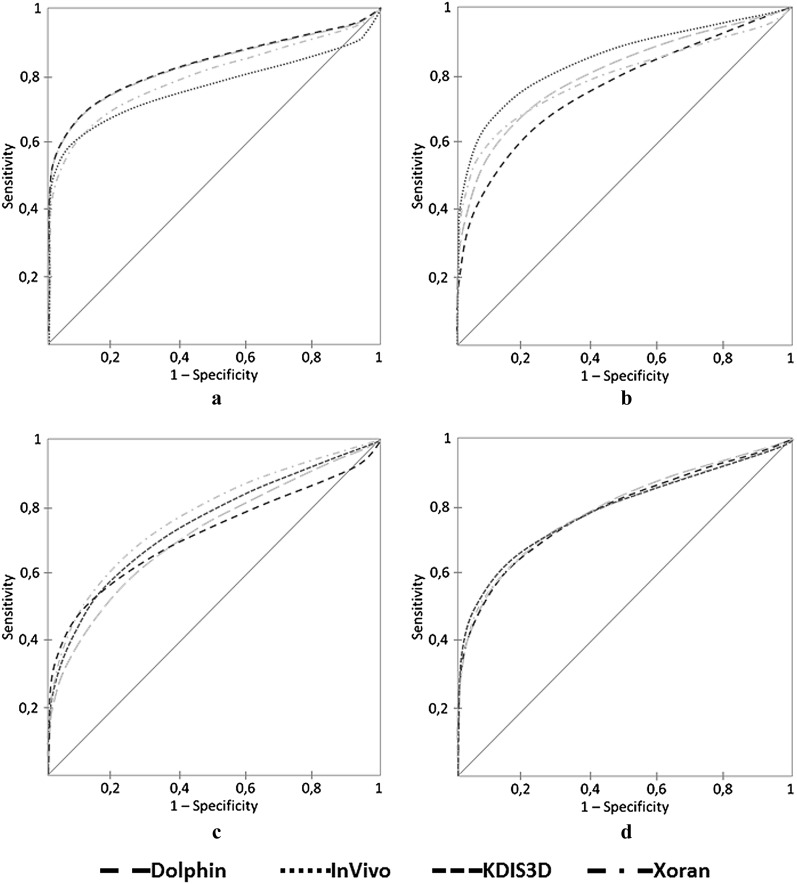
Table 3 and Figure 5 show the mean areas under ROC curves for the observers in each treatment and condition. In general, there was not a statistically significant difference between the software. The effect of different software programs did not depend on what material was present. In other words, there was not a statistically significant interaction between software and material. However, there was a statistically significant difference between materials, considering sensitivity, accuracy and area under the ROC curve. Whether compared with the UR or the GP group, the diagnostic accuracy was significantly lower in the Post group for any type of image. The Tukey test was used to discern which groups differed from the others.
Table 3.
The mean areas under receiver operating characteristic curves [Az (SD)] of three observers for diagnosis of vertical root fractures
| Group | Dolphin | InVivo | KDIS3D | Xoran |
| UN | 0.83 (0.04) | 0.77 (0.04) | 0.83 (0.04) | 0.80 (0.03) |
| GP | 0.80 (0.03) | 0.85 (0.03) | 0.76 (0.04) | 0.80 (0.04) |
| Post | 0.72 (0.04) | 0.75 (0.05) | 0.71 (0.05) | 0.77 (0.06) |
| Overall | 0.79 (0.02) | 0.79 (0.02) | 0.79 (0.02) | 0.78 (0.02) |
GP, gutta-percha; Post, intracanal post; SD, standard deviation; UR, unrestored.
Means that are italicised are statistically different (p < 0.05).
Dolphin (Dolphin Imaging & Management Solutions, v. 11.5) is manufactured by Patterson Dental Supply, Inc., St Paul, MN; InVivo (InVivoDental, v. 5.0) by Anatomage Inc., San Jose, CA; KDIS3D (Kodak Dental Imaging Software 3D module, v. 2.1.11) by Carestream Health Inc., Rochester, NY; and Xoran (Xoran CAT™, v. 3.0.34) by Xoran Technologies, Ann Arbor, MI.
Figure 5.
Receiver operating characteristic curves for all observers based on imaging software for the groups tested: (A) UR, (B) GP, (C) Post and (D) overall results for all groups together. Dolphin (Dolphin Imaging & Management Solutions, v. 11.5) is manufactured by Patterson Dental Supply, Inc., St Paul, MN; InVivo (InVivoDental, v. 5.0) by Anatomage Inc., San Jose, CA; KDIS3D (Kodak Dental Imaging Software 3D module, v. 2.1.11) by Carestream Health Inc., Rochester, NY; and Xoran (Xoran CAT™, v. 3.0.34) by Xoran Technologies, Ann Arbor, MI
Discussion
One of the most difficult problems encountered in clinical dental practice is the diagnosis of tooth root fractures owing to the limited non-specific clinical signs and symptoms and inherent limitations of projection radiography. Numerous authors have evaluated the reliability and accuracy of CBCT images, considering different parameters, such as equipment, image resolution and artefacts.8–20 None have addressed the possible influence software reconstruction may have on diagnostic accuracy. The present study evaluated the influence of software reconstruction of CBCT images in the diagnostic ability of experimentally induced vertical root fractures.
Dental software packages and applications capable of DICOM display can be categorized into proprietary and third-party commercial software. Proprietary viewers are provided by the manufacturers of CBCT equipment and act as both acquisition and viewing software. Most proprietary software is also capable of converting their proprietary data formats into an exportable DICOM file.26 Commercial third-party DICOM viewers may not be directly associated with a specific hardware. There are a number of free DICOM viewers that can be downloaded from the internet, which also have utility for viewing dental images.27 Good examples of free DICOM viewers include KDIS3D (Carestream Health Inc., Rochester, NY), Ginkgo CADx (MetaEmotion Healthcare, Valladolid, Spain), DicomWorks (DicomWorks project, Lille, France) and OsiriX (OsiriX Foundation, Los Angeles, CA).
Among the increasing number of software packages dedicated to managing and analysing DICOM images, the present study focused on three, including Dolphin, InVivo and KDIS3D. The former two must be purchased, whereas the latter is available for free. The study also investigated the proprietary manufacturer acquisition software (Xoran) used to acquire the images and display the data in the native XSTD format. Our results indicate that the choice of the software does not have any influence on CBCT accuracy for the detection of simulated vertical root fractures. The reliability and accuracy of three commercially available DICOM software programs [Dolphin, InVivo and OnDemand3D (Cybermed, Seoul, Republic of Korea)] for measuring upper airway volumes have also been reported.24 In this task, it was found that although all three were highly reliable in their airway volume calculations, they demonstrated poor accuracy, suggesting systematic errors.24
We also demonstrated that the nature of the intracanal contents directly influences diagnostic accuracy with regards to detection of vertical root fractures. Although no differences were detected between unrestored and GP-restored canals, the presence of metal posts reduced diagnostic performance significantly. Interestingly, the specificity results were the opposite: the Post group presented with the highest specificity values among all groups, but with no significant association. Many previous studies9–11,13,15–20 have found higher values for sensitivity, specificity and accuracy for root fracture diagnosis, except for specificity of fracture in teeth filled up with metal posts (Table 4).
Table 4.
Comparison of the present results with the ones found in the literature for cone beam CT diagnostic ability to assess root fractures
| Resultsa | Group | Sensitivity | Specificity | Accuracy |
| Higher | UR | 0.80–0.979,13,15,18,19 | 0.95–1.009,16–19 | 0.80–0.9816,18,19 |
| GP | 0.75–0.979,13,18–20 | 0.93 | 0.81–0.9511,19 | |
| Post | 0.55–0.9013,17,19 | — | 0.82–0.8816,17,19 | |
| Similar | UR | 0.65–0.7210,16,17 | 0.75–0.9013,16–18 | 0.75–0.8016,17 |
| GP | — | 0.879 | 0.68–0.7211,18,20 | |
| Post | 0.40–0.4516 | 0.85–0.9016,17 | 0.60–0.7016,17 | |
| Lower | UR | 0.20–0.6317 | 0.20–0.6016,17 | 0.35–0.6816,17 |
| GP | — | 0.56–0.7313,18,20 | 0.62–0.6711 | |
| Post | — | 0.35–0.8013,16,17,19 | 0.38–0.5816,17 |
GP, gutta-percha; Post, intracanal post; UR, unrestored.
In comparison with results found in the present study.
Sensitivity and specificity are fundamental measures of the accuracy of a diagnostic test. Sensitivity describes the ability of a test to correctly diagnose the presence of disease when disease is actually present (true positive), whereas specificity describes the ability of the test to correctly rule out the presence of disease when it is truly absent (true negative). Because the root fracture prognosis is poor and extraction is often required, false-positive and/or false-negative results must be avoided.13 Given that a high specificity and a low sensitivity were found in the GP and Post groups, we believe that the observers had tried to not misdiagnose the presence of fracture when artefacts were present and scored most teeth negatively for it.
An artefact is any distortion or error in the image that is unrelated to the subject being studied. The presence of hyperdense materials (i.e. gutta-percha and metal post) can lead to severe streaking artefacts. They occur because of extreme beam hardening or photon starvation owing to insufficient photons reaching the detector, resulting in horizontal streaks in the image and noisy projection reconstructions. Beam hardening happens when the mean energy of the X-ray beam increases because lower energy photons are absorbed in preference to higher energy photons. Because the CBCT X-ray beam is heterochromatic and has a lower mean kilovolt-peak energy than conventional CT, this artefact is more pronounced on CBCT images.3 Although the observers were not asked to report on image artefacts, it is possible that streaking artefacts simulate fracture lines and influenced their diagnostic ability.
The thickness of fractures also has a direct influence on CBCT accuracy.12,13 The thicker the fracture line, the higher its detectability. In the present study, all simulated fractures were “hairline” in nature to simulate the immediate post-traumatic situation in which no oedema or granulation tissue has yet displaced the fragments.10,12 To simulate this clinical situation, the sample was scanned in the smallest voxel size available (0.2 mm) for the particular CBCT device used. This setting has been reported as being optimal for diagnosis when a root canal has a filling or a metallic post.13,19 That being said, the tenuous fracture line associated with the streaking artefacts could account for the cases of false-positive and false-negative results found in the present study. This extremely difficult diagnosis association (tenuous fracture line and artefacts) can also explain the intra- and interobserver intraclass correlation coefficient variation by reducing the observer's confidence at the time of diagnosis, leading to observers' agreement at even lower levels.16,17 The level of agreement varies in research involving root fractures. It was very high to weak in samples without intracanal materials9,10,13,15–19 and high to very weak in teeth with gutta-percha or a metallic post.9–11,13,16–20 In the present study, it was found that intraobserver coefficients ranged between fair and substantial agreement, whereas interobserver coefficients indicated moderate agreement.
In real-life situations, radiographic images must be correlated with clinical parameters (probing, mobility test, sensitivity during mastication, etc.) to assist in the diagnosis of dental root fractures. The current study did not attempt to provide additional information that may have biased or improved detection. Further studies are required to elucidate the influence of history on CBCT diagnostic accuracy. In addition, this study was limited to only four commonly available software programs.
In conclusion, the diagnosis of minimally displaced vertical root fracture does not depend on the software used to reconstruct the image from CBCT DICOM data. However, diagnostic accuracy is significantly reduced for all software when root canals are restored with metallic posts.
Acknowledgments
We are grateful to the University of Louisville School of Dentistry (Louisville, KY) for the technical support to the first author while he was a visiting postgraduate fellow.
Funding
We are grateful to the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) Foundation (Brazil) for the scholarship support.
References
- 1.Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J 2007; 40: 818–830 10.1111/j.1365-2591.2007.01299.x [DOI] [PubMed] [Google Scholar]
- 2.Patel S. New dimensions in endodontic imaging: part 2. Cone beam computed tomography. Int Endod J 2009; 42: 463–475 10.1111/j.1365-2591.2008.01531.x [DOI] [PubMed] [Google Scholar]
- 3.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am 2008; 52: 707–730 10.1016/j.cden.2008.05.005 [DOI] [PubMed] [Google Scholar]
- 4.Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 114–119 10.1016/j.tripleo.2006.01.001 [DOI] [PubMed] [Google Scholar]
- 5.Liedke GS, Silveira HED, Silveira HLD, Dutra V, Figueiredo JAP. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod 2009; 35: 233–235 10.1016/j.joen.2008.11.005 [DOI] [PubMed] [Google Scholar]
- 6.Neves FS, Vasconcelos TV, Vaz SL, Freitas DQ, Haiter-Neto F. Evaluation of reconstructed images with different voxel sizes of acquisition in the diagnosis of simulated external root resorption using cone beam computed tomography. Int Endod J 2012; 45: 234–239 10.1111/j.1365-2591.2011.01966.x [DOI] [PubMed] [Google Scholar]
- 7.de Azevedo Vaz SL, Vasconcelos TV, Neves FS, de Freitas DQ, Haiter-Neto F. Influence of cone-beam computed tomography enhancement filters on diagnosis of simulated external root resorption. J Endod 2012; 38: 305–308 10.1016/j.joen.2011.10.012 [DOI] [PubMed] [Google Scholar]
- 8.Mora MA, Mol A, Tyndall DA, Rivera EM. Effect of the number of basis images on the detection of longitudinal tooth fractures using local computed tomography. Dentomaxillofac Radiol 2007; 36: 382–386 10.1259/dmfr/25073870 [DOI] [PubMed] [Google Scholar]
- 9.Hassan B, Metska ME, Ozok AR, Stelt PVD, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod 2009; 35: 719–722 [DOI] [PubMed] [Google Scholar]
- 10.Wenzel A, Haiter Neto F, Frydenberg M, Kirkevang LL. Variable-resolution cone-beam computerized tomography with enhancement filtration compared with intraoral photostimulable phosphor radiography in detection of transverse root fractures in an in vitro model. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 939–945 10.1016/j.tripleo.2009.07.041 [DOI] [PubMed] [Google Scholar]
- 11.Hassan B, Metska ME, Ozok AR, Stelt PVD, Wesselink PR. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod 2010; 36: 126–129 10.1016/j.joen.2009.09.013 [DOI] [PubMed] [Google Scholar]
- 12.Özer SY. Detection of vertical root fractures of different thicknesses in endodontically enlarged teeth by cone beam computed tomography versus digital radiography. J Endod 2010; 36: 1245–1249 10.1016/j.joen.2010.03.021 [DOI] [PubMed] [Google Scholar]
- 13.Melo SL, Bortoluzzi EA, Abreu M, Jr, Corrêa LR, Corrêa M. Diagnostic ability of a cone-beam computed tomography scan to assess longitudinal root fractures in prosthetically treated teeth. J Endod 2010; 36: 1879–1882 10.1016/j.joen.2010.08.025 [DOI] [PubMed] [Google Scholar]
- 14.Varshosaz M, Tavakoli MA, Mostafavi M, Baghban AA. Comparison of conventional radiography with cone beam computed tomography for detection of vertical root fractures: an in vitro study. J Oral Sci 2010; 52: 593–597 [DOI] [PubMed] [Google Scholar]
- 15.Özer SY. Detection of vertical root fractures by using cone beam computed tomography with variable voxel sizes in an in vitro model. J Endod 2011; 37: 75–79 10.1016/j.joen.2010.04.021 [DOI] [PubMed] [Google Scholar]
- 16.Costa FF, Gaia BF, Umetsubo OS, Cavalcanti MGP. Detection of horizontal root fracture with small-volume cone-beam computed tomography in the presence and absence of intracanal metallic post. J Endod 2011; 37: 1456–1459 [DOI] [PubMed] [Google Scholar]
- 17.Costa FF, Gaia BF, Umetsubo OS, Pinheiro LR, Tortamano IP, Cavalcanti MGP. Use of large-volume cone-beam computed tomography in identification and localization of horizontal root fracture in the presence and absence of intracanal metallic post. J Endod 2012; 38: 856–859 10.1016/j.joen.2012.03.011 [DOI] [PubMed] [Google Scholar]
- 18.Khedmat S, Rouhi N, Drage N, Shokouhinejad N, Nekoofar MH. Evaluation of three imaging techniques for the detection of vertical root fractures in the absence and presence of gutta-percha root fillings. Int Endod J 2012; 45: 1004–1009 10.1111/j.1365-2591.2012.02062.x [DOI] [PubMed] [Google Scholar]
- 19.da Silveira PF, Vizzotto MB, Liedke GS, da Silveira HLD, Montagner F, da Silveira HED. Detection of vertical root fractures by conventional radiographic examination and cone beam computed tomography—an in vitro analysis. Dent Traumatol 2013; 29: 41–46 10.1111/j.1600-9657.2012.01126.x [DOI] [PubMed] [Google Scholar]
- 20.Metska ME, Aartman IHA, Wesselink PR, Özok AR. Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod 2012; 38: 1344–1347 10.1016/j.joen.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 21.Andreasen JO. Etiology and pathogenesis of traumatic dental injuries. A clinical study of 1,298 cases. Scant J Dent Res 1970; 78: 329–342 [DOI] [PubMed] [Google Scholar]
- 22.Matsuda K, Ikebe K, Enoki K, Tada S, Fujiwara K, Maeda Y. Incidence and association of root fractures after prosthetic treatment. J Prosthodont Res 2011; 55: 137–140 10.1016/j.jpor.2010.10.003 [DOI] [PubMed] [Google Scholar]
- 23.Sogur E, Baks BG, Grondahl HG. Imaging of root canal fillings: a comparison of subjective image quality between limited cone-beam CT, storage phosphor and film radiography. Int Endod J 2007; 40: 179–185 10.1111/j.1365-2591.2007.01204.x [DOI] [PubMed] [Google Scholar]
- 24.El H, Palomo JM. Measuring the airway in 3 dimensions: a reliability and accuracy study. Am J Orthod Dentofacial Orthop 2010; 137: S50.e1–S50.e9 10.1016/j.ajodo.2010.01.014 [DOI] [PubMed] [Google Scholar]
- 25.Monaghan P, Bajalcaliev JG, Kaminski EJ, Lautenschlager EP. A method for producing experimental simple vertical root fractures in dog teeth. J Endod 1993; 19: 512–515 10.1016/S0099-2399(06)81493-7 [DOI] [PubMed] [Google Scholar]
- 26.Grauer D, Cevidanes LSH, Proffit WR. Working with DICOM craniofacial images. Am J Orthod Dentofacial Orthop 2009; 136: 460–470 10.1016/j.ajodo.2009.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham RNJ, Perriss RW, Scarsbrook AF. DICOM demystified: a review of digital file formats and their use in radiological practice. Clin Radiol 2005; 60: 1133–1140 10.1016/j.crad.2005.07.003 [DOI] [PubMed] [Google Scholar]