Abstract
Objective. Abnormal foot posture and function have been proposed as possible risk factors for low back pain, but this has not been examined in detail. The objective of this study was to explore the associations of foot posture and foot function with low back pain in 1930 members of the Framingham Study (2002–05).
Methods. Low back pain, aching or stiffness on most days was documented on a body chart. Foot posture was categorized as normal, planus or cavus using static weight-bearing measurements of the arch index. Foot function was categorized as normal, pronated or supinated using the centre of pressure excursion index derived from dynamic foot pressure measurements. Sex-specific multivariate logistic regression models were used to examine the associations of foot posture, foot function and asymmetry with low back pain, adjusting for confounding variables.
Results. Foot posture showed no association with low back pain. However, pronated foot function was associated with low back pain in women [odds ratio (OR) = 1.51, 95% CI 1.1, 2.07, P = 0.011] and this remained significant after adjusting for age, weight, smoking and depressive symptoms (OR = 1.48, 95% CI 1.07, 2.05, P = 0.018).
Conclusion. These findings suggest that pronated foot function may contribute to low back symptoms in women. Interventions that modify foot function, such as orthoses, may therefore have a role in the prevention and treatment of low back pain.
Keywords: low back pain, risk factors, flatfoot, gait
Introduction
Low back pain is a highly prevalent problem worldwide, with the point prevalence estimated at ∼18% of the general population [1]. The financial burden of low back pain in relation to health care costs and productivity loss is substantial. Direct healthcare expenditure for low back pain was reported to be $90.7 billion in the USA in 1998 [2], while total direct and indirect costs have been estimated at £11 billion in the UK in 2000 [3] and A$9.17 billion in Australia in 2001 [4]. Treatment of low back pain presents a considerable challenge, as a specific pathoanatomical diagnosis cannot be identified in ∼85% of cases [5]. A complex array of risk factors are known to contribute to the condition, such as increased age, female sex, low educational status, obesity, occupation and psychosocial factors [1].
In addition to these well-established risk factors, postural variations, such as decreased lumbar lordosis [6, 7] and leg length inequality [8] have long been suspected to play a role in predisposition to low back pain by altering the stresses placed on soft tissue structures around the spine. Abnormal foot posture and function have also been implicated, with several authors suggesting that individuals with low back pain are more likely to have planus (low-arched or pronated) feet [9]. Evidence to support this assertion, however, is inconsistent and generally of low methodological quality. A large retrospective study of 97 279 military recruits reported that those with moderate or severe pes planus (determined by clinical observation) were almost twice as likely to report a history of intermittent low back pain [10]. In contrast, two smaller clinical studies using more objective measurements of foot posture found no such association [11, 12], and a population-based study of 674 individuals reported that those with low back pain were more likely to have a cavus (highly arched or supinated) foot posture [13].
Despite this lack of evidence, an association between foot posture, function and low back pain is biomechanically and physiologically plausible. Variation in the height of the medial longitudinal arch has been shown to influence the magnitude of accelerations at the lumbar spine when running [14], and alteration of foot position can influence pelvic alignment [15–17] and the electromyographic activity of the erector spinae and gluteal muscles when walking [18]. Furthermore, indirect evidence to support this association can be derived from several small clinical trials that have reported short-term reductions in low back pain in participants prescribed a range of foot orthoses compared to no treatment or ‘placebo’ insoles [19–23].
Therefore the objective of this study was to explore the relationships between foot posture, dynamic foot function and low back pain in men and women who participated in the Framingham Foot Study, using objective biomechanical measurements. We hypothesized that (i) people with abnormal foot posture (either planus or cavus) would be more likely to report low back pain than those with neither planus nor cavus foot posture, (ii) people classified as having pronated or supinated feet when walking would be more likely to report low back pain than those with neither pronated or supinated dynamic foot function and (iii) people with asymmetry in either foot posture or dynamic foot function would be more likely to report low back pain than those with symmetrical foot posture and function.
Methods
Participants
The study sample, the Framingham Foot Study cohort, was derived from two large, population-based samples of residents of Framingham, MA, USA. The majority of the cohort was comprised of members from the Framingham Study original cohort and the Framingham offspring cohort. The Framingham Study original cohort was formed in 1948 from a two-thirds sample of the town of Framingham, MA, in order to study risk factors for heart disease [24]. This cohort has been followed biennially since that time. The Framingham offspring cohort, formed in 1972, consists of adult offspring who had a parent in the original cohort, as well as the spouses of the offspring [25]. This group has been followed every 4 years since cohort inception to study familial risk factors for heart disease. Members of the Framingham cohorts were examined for the current study either at their scheduled Framingham clinic examination or at a call-back examination.
The second population-based group used for the study was a new population sample that was derived from census-based, random-digit dialling within the Framingham community by the Center for Survey Research at the University of Massachusetts, selecting subjects who were ≥50 years old and ambulatory. This group was added to the Framingham Foot Study recruitment to increase participation by minority persons and other community members of the Framingham catchment area (using a targeted random-digit dialling schema in selected Framingham census tracts). Persons contacted via the random-digit dialling methodology who were interested in being part of a multiphase physical examination (foot, osteoarthritis, bone health and general health) received a written letter of invitation to join the study and a follow-up phone call to schedule a study appointment.
The collection of study data and information from the Framingham Foot Study participants followed strict, well-established protocols that are available upon request from the Framingham Study. All Framingham Foot Study participants gave informed consent for the data collection and this study was approved by both the Hebrew Senior Life and the Boston University Medical Center institutional review boards. The data are extensive, systematically collected, of high quality and gathered by trained personnel.
From these combined population-based cohorts, the Framingham Foot Study conducted a physical examination of the foot and collected participant history, performance measures and other data via questionnaires between 2002 and 2005. A validated foot examination was used with specific criteria to assess foot pain, foot symptoms and the presence of foot disorders. Trained clinical examiners performed all foot examinations. All participants were ambulatory and cognitively intact as indicated by Mini-Mental score screening to identify qualified study subjects who would be able to give symptom information about their feet.
For this analysis, inclusion criteria included a yes or no response to the query on low back pain, and both a static and dynamic plantar pressure assessment of each foot.
Low back pain assessment
Low back pain was documented with a structured questionnaire. Participants were provided with a body chart with 10 regions highlighted (shoulders, elbows, hips, wrists, knees, ankles on an anterior view and neck, upper back, mid-back and lower back on a posterior view) and were asked: ‘On most days, do you have pain, aching, or stiffness in any of your joints?’ Those who responded affirmatively were asked to mark an ‘X’ on the chart indicating which regions were affected. Participants who placed an ‘X’ on the lower back region (corresponding to the region between the lowest rib and the sacrum) were defined as having low back pain (see Fig. 1).
Fig. 1.

Body chart used to determine the location of low back pain.
Foot posture and function assessment
Foot posture and function were both assessed using the MatScan system (Tekscan Inc, Boston, MA, USA). The system consists of a 5-mm thick floor mat (432 × 368 mm) comprised of 2288 resistive sensors (1.4 sensors/cm2) that samples data at a frequency of 40 Hz. The reliability of the MatScan system has been described in detail previously [26]. Two types of scans were collected: standing and walking. For the standing scan, a one-frame self-selected bipedal stance image was collected for each participant. For the walking scans, participants walked across the mat at a self-selected pace using the two-step method, which involves striking the platform on the second step. One walking trial of each foot was recorded, with data from the right foot used for this analysis.
Foot posture was assessed using the arch index (AI), first described by Cavanagh and Rogers [27]. From the maximum peak pressure image of the participant’s bipedal relaxed stance, the AI was calculated as the ratio of the area of the middle third of the footprint to the entire footprint area (excluding the toes), with a higher value representing a ‘flatter’ (i.e. more planus) foot (Fig. 2). AI scores have previously been shown to be highly correlated with navicular height [28] and angular medial longitudinal arch measures [29] obtained from foot radiographs. AI scores were divided into quintiles for men and women separately, and foot posture categorized as cavus (those in the lowest 20%), the normal reference group (those in the middle 60%) or planus (those in the highest 20%). The cut-off scores to define each category were as follows: cavus (0–0.171), the reference group (0.172–0.294) and planus (0.295–0.491) for men and cavus (0–0.157), the reference group (0.158–0.286) and planus (0.287–0.486) for women.
Fig. 2.

Calculation of the AI.
The length of the static footprint excluding the toes is divided into equal thirds. The AI is then calculated as the area of the middle third of the footprint divided by the entire footprint area (AI = B/A + B + C).
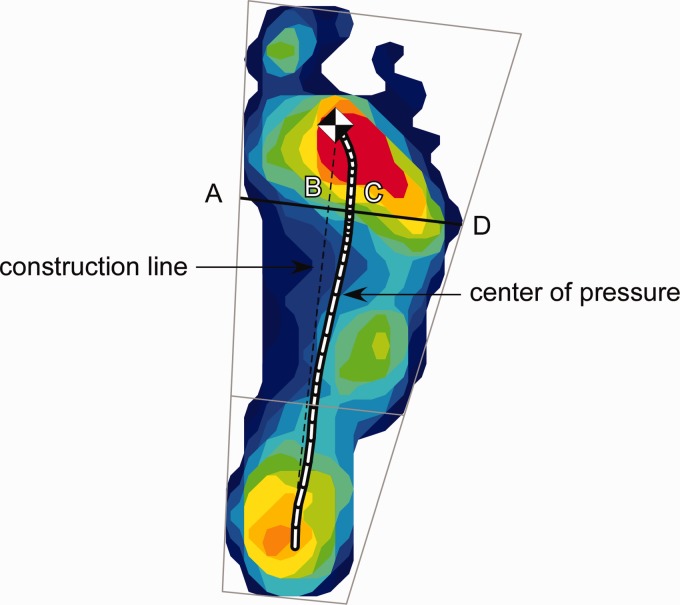
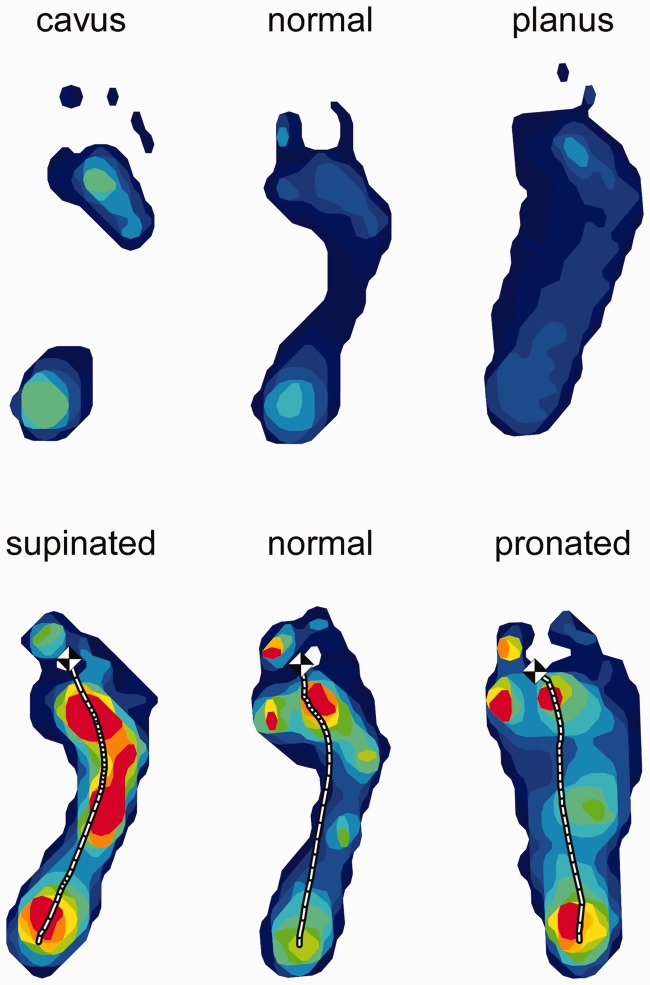
Foot function was assessed by calculating the centre of pressure excursion index (CPEI) of the walking trials. The CPEI represents the degree of lateral deviation of the centre of pressure at the anterior one-third trisection of the foot relative to a line connecting the first and last centre of pressure data points (see Fig. 3). To calculate the CPEI, the maximum peak pressure image of a dynamic footprint was divided into thirds. A construction line was drawn from the first to the last centre of pressure data point. A line (AD) was constructed at the anterior one-third trisection of the foot. The distance between the intersection of the construction line and line AD (point B) and where the centre of pressure intersects with line AD (point C) was measured. The CPEI was then calculated by normalizing the distance BC to the width of the foot (AD), so CPEI = BC/AD × 100. In a pronated foot, the concavity of the centre of pressure curve is decreased, resulting in a smaller CPEI value. In a supinated foot, the concavity of the centre of pressure curve is increased, resulting in a larger CPEI value [30]. As with AI scores, CPEI scores were then divided into sex-specific quintiles, and participants were categorized as having supinated foot function (those in the highest 20%), a reference group of foot function (those in the middle 60%) or pronated foot function (those in the lowest 20%). The cut-off scores to define each category were as follows: supinated (23.6–42.2), the normal reference group (10.3–23.4) and pronated (−25.3–10.2) for men and supinated (19.3–37.9), the reference group (6.2–19.2) and pronated (−11.2–6.1) for women. Typical examples of cavus, normal and planus foot posture and supinated, reference and pronated foot function categories using this classification system are shown in Fig. 4.
Fig. 3.
Calculation of the CPEI.
Fig. 4.
Typical examples of cavus, normal and planus foot posture categories (top) and supinated, normal and pronated foot function categories (bottom).
Asymmetry in foot posture and foot function were defined as the absolute right foot value minus the absolute left foot value, divided by the average of the right and left foot values. If both the right and left values were zero, the asymmetry score was also documented as zero. Quintiles were created and the top quintile defined as asymmetric. The cut-off scores to define asymmetry in foot posture were >0.38 for men and >0.44 for women. The cut-off scores to define asymmetry in foot function were >0.86 for men and >1.17 for women.
Covariates
Covariates in our analyses included age, sex, weight, smoking status and depressive symptoms. Age in years at the time of examination was recorded. Weight was measured using a standardized balance beam and recorded to the nearest half pound. A participant’s smoking status was assessed via questionnaire as a regular smoker in the last year. Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression (CES-D) scale. The CES-D comprises 20 questions relating to depressive feelings over the past week, documented as rarely (score = 0), some or a little of the time (score = 1), occasionally or a moderate amount of the time (score = 2) or most or all of the time (score = 3). The summed CES-D score ranges from 0 to 60, with higher scores indicating more severe depressive symptoms [31].
Statistical analysis
Because sex is a potential confounder for both low back pain and foot function, all analyses were performed as sex-specific. Descriptive statistics were generated separately for men and women as means and standard deviations or percentages, where appropriate. Sex-specific multivariable logistic models were used to calculate odds ratios (ORs) and 95% CIs for the associations of foot posture and foot function (and asymmetry in foot posture and function) to low back pain, adjusting for age, weight, smoking status and CES-D score. All analyses were conducted using the SAS statistical analysis package, version 9.1 (SAS Institute, Cary, NC, USA).
Results
Of the 3378 participants in the Framingham Foot Study, 1930 had low back pain and foot pressure data at the time of the analysis (863 men and 1067 women). The mean age of participants was 64 years (range 36–92 years) and 55% of the sample was female. The mean height and weight were 65.7 inches and 176.1 pounds, respectively. Of these participants, 661 (34%) reported the presence of low back pain, aching or stiffness on most days. Table 1 shows the characteristics of the study sample by sex.
Table 1.
Descriptive characteristics of men and women in the Framingham Foot Study who completed the biomechanical foot examinations
| Men | Women | |
|---|---|---|
| Characteristic | (n = 863) | (n = 1067) |
| Age, mean (s.d.), years | 64.5 (8.9) | 63.4 (8.9) |
| Weight, mean (s.d.), lbs | 194.7 (33.9) | 161.0 (37.4) |
| Regular smoker, n (%) | 77 (8.9) | 108 (10.1) |
| CES-D scale, mean (s.d.) | 10.3 (9.5) | 12.1 (9.9) |
| Low back pain, n (%) | 257 (29.8) | 404 (37.9) |
Table 2 reports the associations of foot posture and foot function to low back pain in men and women, adjusted for age, weight, smoking and depressive symptoms. Neither foot posture nor asymmetry in foot posture or function was significantly associated with low back pain. However, compared to the normal foot function reference group, pronated foot function was significantly associated with an increased likelihood of low back pain in women (OR = 1.51, 95% CI 1.10, 2.07, P = 0.011). This association remained significant after adjusting for age, weight, smoking and depressive symptoms (OR = 1.48, 95% CI 1.07, 2.05, P = 0.018).
Table 2.
ORs for the associations of foot posture and function with low back paina
| Men |
Women |
|||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Foot posture | ||||
| Cavus vs normal | 0.72 (0.47, 1.13) | 0.155 | 0.89 (0.61, 1.29) | 0.542 |
| Planus vs normal | 1.30 (0.87, 1.96) | 0.202 | 0.71 (0.48, 1.05) | 0.091 |
| Asymmetrical vs symmetrical | 0.65 (0.42, 1.01) | 0.056 | 0.87 (0.60, 1.24) | 0.424 |
| Foot function | ||||
| Supinated vs normal | 1.01 (0.69, 1.48) | 0.958 | 1.10 (0.79, 1.52) | 0.583 |
| Pronated vs normal | 1.11 (0.76, 1.61) | 0.597 | 1.48 (1.07, 2.05) | 0.018 |
| Asymmetrical vs symmetrical | 1.35 (0.93, 1.95) | 0.110 | 1.26 (0.91, 1.74) | 0.163 |
aAdjusted for age, weight, smoking and depressive symptoms.
Discussion
The objective of this study was to examine the associations of foot posture and foot function with low back pain using objective biomechanical measurements in people who participated in the population-based Framingham Foot Study (2002–05). Our findings indicate that pronated foot function, as indicated by centre of pressure excursion measurements obtained from dynamic footprints, is significantly associated with low back pain in women after adjusting for age, weight, smoking and depressive symptoms. Contrary to our initial hypotheses, neither foot posture (cavus or planus) nor asymmetry in foot posture or foot function showed an association with low back pain.
An association between foot posture and low back pain has been widely speculated for some time [9], with both planus [10, 32–34] and cavus [13, 35] foot types being implicated. However, contrary to our expectations, we found no relationship between static foot posture (measured using the AI) and low back pain. The mechanical basis for suspecting such an association relates to the proposed interaction between foot position and lumbo-pelvic alignment when standing. Two studies have shown that when the foot is experimentally manipulated into a pronated position using frontal plane wedges, there is a corresponding increase in anterior pelvic tilt [15, 16]. Although these observations confirm a mechanical link between foot position and pelvic alignment, it is arguable as to whether experimentally manipulating a normal foot into a pronated position is an accurate reflection of postural changes that occur in individuals with planus feet. Furthermore, it is likely that in individuals with low back pain, the potentially detrimental changes in lumbo-pelvic alignment arising from planus foot posture when standing would be compensated for by consciously altering the alignment of the lower limb.
Although we found no association between static foot posture and low back pain, our findings suggest that the dynamic function of the foot may play a role. The significant association we observed between low back pain and pronated foot function may be at least partly explained by the kinematic interaction of the lower extremity joints during walking. When the foot pronates during the early stance phase of gait, the calcaneus everts while the talus adducts and the plantar flexes [36]. The inferomedial translation of the talus induces a corresponding internal rotation of the tibia, which in turn leads to internal rotation of the femur [37]. In theory, this increase in internal rotation of the femur results in anterior pelvic tilt due to the tight fibrous connection provided by the sacroiliac joint [38]. Although these movements are considered to be normal components of gait, it is possible that in individuals with ‘excessive’ foot pronation (defined in this study as those in the lowest quintile of the CPEI), the compensatory movements of proximal joints are increased in magnitude and place greater stresses on the lumbo-pelvic region, thereby contributing to the development of low back pain.
Interestingly, the association between pronated foot function and low back pain was only evident in women, which may be partly due to sex differences in the alignment, range of motion and function of lower limb and spinal joints. Previous studies have shown that women exhibit greater static anterior pelvic tilt [39] and dorsal inclination of the spine [40], have greater internal hip rotation range of motion [39] and medial longitudinal arch flexibility [41] and walk with greater trunk extension [42] and hip internal rotation [43] compared with men. It is therefore possible that kinematic changes induced by excessive foot pronation are more readily transmitted to proximal structures in women, although more detailed kinematic studies would need to be undertaken to confirm this.
Asymmetry in foot posture or function was not associated with low back pain. The mechanical basis for suspecting this association relates to the theoretical clinical concept of ‘functional’ limb length discrepancy, where the limb with the flatter/more pronated foot functions as if it were structurally shorter, resulting in pelvic tilt to the ipsilateral side [44]. There are two possible explanations for this lack of association. First, given that moving the subtalar joint from a neutral position to a pronated position results in an average change in ankle joint height of only 3 mm [45], it could be that only very large asymmetries in foot posture or function produce clinically significant changes in lumbo-pelvic alignment and motion. Second, several authors have suggested that due to limb preference and laterality, some degree of asymmetry is a normal feature of gait, with the preferred limb providing greater propulsion and the non-preferred limb providing greater support [46]. Consistent with this concept, asymmetry in foot posture approached statistical significance in men (P = 0.056), with the direction of this association indicating that asymmetry may be protective against back pain.
In addition to providing insight into a possible ‘postural-structural-biomechanical’ mechanism [47] underlying low back pain in some individuals, the association we observed between pronated foot function and low back pain may also partly explain the apparent clinical effectiveness of foot orthoses in reducing low back symptoms. Five randomized controlled trials have reported reductions in low back pain in participants prescribed a range of foot orthoses compared to no treatment or ‘placebo’ insoles [19–23]. Although the mechanism of action was not explored in these trials, foot orthoses have been shown to reduce rearfoot eversion and tibial internal rotation [48]—kinematic variables associated with foot pronation that may be increased in magnitude in individuals with low back pain. Furthermore, controlling foot motion by applying wedges to the sole of the foot leads to earlier onset of erector spinae muscle activity when walking [18], which could potentially correct for the delayed activity of this muscle observed in individuals with low back pain [49] and assist in controlling the motion of the trunk.
The findings reported here need to be interpreted in the context of several study design limitations. First, we used a single question and a body chart to define low back pain. Recently developed consensus guidelines recommend that epidemiological case definitions of low back pain should also include questions related to the severity and duration of symptoms [50], so it is likely that our sample included individuals with relatively mild symptoms. Second, we made no attempt to delineate the underlying cause of low back pain, although previous research suggests that a specific pathoanatomical diagnosis cannot be identified in the majority of cases [5]. Third, while our measure of dynamic foot function—the CPEI—has been shown to discriminate between clinically determined planus and rectus foot types [30], it has yet to be validated against a multisegment kinematic foot model. Therefore, whether a pronated foot defined using this measure also demonstrates greater rearfoot eversion, sagittal plane midfoot motion or forefoot abduction is yet to be determined. Third, in the absence of any established criteria, we used quintiles to determine the cut-points defining the three foot posture and function categories, which assumes that 60% of participants in the reference group have ‘normal’ feet and that the distribution of ‘abnormal’ feet is symmetrical, i.e. 20% of the population has planus/pronated feet and 20% has cavus/supinated feet. While this approach is epidemiologically sound, as it examines the extremes of a large distribution, it may not reflect clinical observations suggesting that planus/pronated feet are more common than cavus/supinated feet. Finally, the key limitation of all cross-sectional studies is the inability to confidently infer causation. Although we consider reverse causation (i.e. that back pain leads to pronated foot function) to be unlikely, we acknowledge that several common causal structural or functional variables could be responsible for the observed association between foot function and low back pain.
Despite these limitations, our study has several important strengths. First, in contrast to previous investigations focusing on military [10] or clinical [11, 12] samples, our study was population-based and our findings are therefore more likely to be representative of the general population. Second, we used an objective measure of foot posture rather than relying on visual assessment by clinicians, which is known to have questionable reliability. Third, to the best of our knowledge this is first study to incorporate a measure of dynamic foot function. This is an important consideration, given that static measures of foot posture may not always provide an accurate indicator of dynamic foot function when walking.
In conclusion, pronated foot function when walking, as evidenced by centre of pressure measurements obtained with a plantar pressure system, is associated with low back pain in women. These findings provide preliminary evidence to support a possible ‘postural-structural-biomechanical’ mechanism underlying low back pain in some individuals. Interventions that modify abnormal foot function, such as foot orthoses, may therefore have a role in the prevention and treatment of low back pain and warrant further investigation.
Rheumatology key messages.
Planus or cavus foot posture is not associated with low back pain in men or women.
Pronated foot function when walking is associated with low back pain in women.
Interventions that modify abnormal foot function may facilitate prevention and treatment of low back pain.
Acknowledgements
H.B.M. is currently a National Health and Medical Research Council Senior Research Fellow (ID 1020925) and was supported by an Australian-American Fulbright Commission Senior Scholarship at the time this work was undertaken.
Funding: This work was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and National Institute on Aging (AR047853). This work was derived from the Framingham Heart Study of the National Heart Lung and Blood Institute of the National Institutes of Health and Boston University School of Medicine and was supported by the National Heart, Lung and Blood Institute’s Framingham Heart Study (Contract No. N01-HC-25195).
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Hoy D, Brooks P, Blyth F, et al. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–81. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct healthcare expenditures among individuals with back pain in the United States. Spine. 2004;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 4.Walker BF, Muller R, Grant WD. Low back pain in Australian adults: the economic burden. Asia Pac J Public Health. 2003;15:79–87. doi: 10.1177/101053950301500202. [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363–70. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 6.Barrey C, Jund J, Noseda O, et al. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study of about 85 cases. Eur Spine J. 2007;16:1459–67. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low-back pain matched for age, sex, and size. A prospective controlled clinical study. Spine. 1994;19:1611–8. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 8.Giles LG, Taylor JR. Low back pain associated with leg length inequality. Spine. 1981;6:510–21. doi: 10.1097/00007632-198109000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Bird AR, Payne CB. Foot function and low back pain. Foot. 1999;9:175–80. [Google Scholar]
- 10.Kosashvili Y, Fridman T, Backstein D, et al. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008;29:910–3. doi: 10.3113/FAI.2008.0910. [DOI] [PubMed] [Google Scholar]
- 11.Brantingham JW, Gilbert JL, Shaik J, et al. Sagittal plane blockage of the foot, ankle and hallux and foot alignment—prevalence and association with low back pain. J Chiropr Med. 2006;4:123–7. doi: 10.1016/S0899-3467(07)60144-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brantingham JW, Adams KJ, Cooley JR, et al. A single-blind pilot study to determine risk and association between navicular drop, calcaneal eversion, and low back pain. J Manipulative Physiol Ther. 2007;30:380–85. doi: 10.1016/j.jmpt.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Roncarati A, McMullen W. Correlates of low back pain in a general population sample: a multidisciplinary perspective. J Manipulative Physiol Ther. 1988;11:158–64. [PubMed] [Google Scholar]
- 14.Ogon M, Aleksiev AR, Pope MH, et al. Does arch height affect impact loading at the lower back level in running? Foot Ankle Int. 1999;20:263–6. doi: 10.1177/107110079902000410. [DOI] [PubMed] [Google Scholar]
- 15.Khamis S, Yizhar Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture. 2007;25:127–34. doi: 10.1016/j.gaitpost.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Pinto RZA, Souza TR, Trede RG, et al. Bilateral and unilateral increases in calcaneal eversion affect pelvic alignment in standing position. Man Ther. 2008;13:513–9. doi: 10.1016/j.math.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Betsch M, Schneppendahl J, Dor L, et al. Influence of foot positions on the. spine and pelvis. Arthritis Care Res. 2011;63:1758–65. doi: 10.1002/acr.20601. [DOI] [PubMed] [Google Scholar]
- 18.Bird AR, Bendrups AP, Payne CB. The effect of foot wedging on electromyographic activity in the erector spinae and gluteus medius muscles during walking. Gait Posture. 2003;18:81–91. doi: 10.1016/s0966-6362(02)00199-6. [DOI] [PubMed] [Google Scholar]
- 19.Tooms RE, Griffin JW, Green S, et al. Effect of viscoelastic insoles on pain. Orthopedics. 1987;10:1143–7. [PubMed] [Google Scholar]
- 20.Basford JR, Smith MA. Shoe insoles in the workplace. Orthopedics. 1988;11:285–8. doi: 10.3928/0147-7447-19880201-08. [DOI] [PubMed] [Google Scholar]
- 21.Shabat S, Gefen T, Nyska M, et al. The effect of insoles on the incidence and severity of low back pain among workers whose job involves long-distance walking. Eur Spine J. 2005;14:546–50. doi: 10.1007/s00586-004-0824-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cambron CA, Duarte M, Dexheimer J, et al. Shoe orthotics for the treatment of chronic low back pain: a randomized controlled pilot study. J Manipulative Physiol Ther. 2011;34:254–60. doi: 10.1016/j.jmpt.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Castro-Méndez A, Munuera PV, Albornoz-Cabello M. The short-term effect of custom-made foot orthoses in subjects with excessive foot pronation and lower back pain: a randomized, double-blinded, clinical trial. Prosthet Orthot Int. 2013 doi: 10.1177/0309364612471370. doi:10.1177/0309364612471370. [DOI] [PubMed] [Google Scholar]
- 24.Dawber T, Meadors G, Moore F. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951;41:279–81. doi: 10.2105/ajph.41.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feinleib M, Kannel W, Garrison R, et al. The Framingham Offspring Study: design and preliminary data. Prev Med. 1975;4:518–25. doi: 10.1016/0091-7435(75)90037-7. [DOI] [PubMed] [Google Scholar]
- 26.Zammit GV, Menz HB, Munteanu SE. Reliability of the TekScan MatScan system for the measurement of plantar forces and pressures during barefoot level walking in healthy adults. J Foot Ankle Res. 2010;3:11. doi: 10.1186/1757-1146-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cavanagh PR, Rodgers MM. The arch index: a useful measure from footprints. J Biomech. 1987;20:547–51. doi: 10.1016/0021-9290(87)90255-7. [DOI] [PubMed] [Google Scholar]
- 28.McCrory JL, Young MJ, Boulton AJM, et al. Arch index as a predictor of arch height. Foot. 1997;7:79–81. [Google Scholar]
- 29.Menz HB, Munteanu SE. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J Orthop Sports Phys Ther. 2005;35:479–86. doi: 10.2519/jospt.2005.35.8.479. [DOI] [PubMed] [Google Scholar]
- 30.Song J, Hillstrom HJ, Secord D, et al. Foot type biomechanics: a comparison of planus and rectus foot types. J Am Podiatr Med Assoc. 1996;86:16–23. doi: 10.7547/87507315-86-1-16. [DOI] [PubMed] [Google Scholar]
- 31.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 32.Botte RR. An interpretation of the pronation syndrome and foot types of patients with low back pain. J Am Podiatry Assoc. 1981;71:243–53. doi: 10.7547/87507315-71-5-243. [DOI] [PubMed] [Google Scholar]
- 33.Rothbart BA, Estabrook L. Excessive pronation: a major biomechanical determinant in the development of chondromalacia and pelvic lists. J Manipulative Physiol Ther. 1988;11:373–9. [PubMed] [Google Scholar]
- 34.Cibulka MT. Low back pain and its relation to the hip and foot. J Orthop Sports Phys Ther. 1999;29:595–601. doi: 10.2519/jospt.1999.29.10.595. [DOI] [PubMed] [Google Scholar]
- 35.Builder MA, Marr SJ. Case history of a patient with low back pain and cavus feet. J Am Podiatry Assoc. 1980;70:299–301. doi: 10.7547/87507315-70-6-299. [DOI] [PubMed] [Google Scholar]
- 36.Hamel AJ, Sharkey NA, Buczek FL, et al. Relative motions of the tibia, talus, and calcaneus during the stance phase of gait: a cadaver study. Gait Posture. 2004;20:147–53. doi: 10.1016/j.gaitpost.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Souza TR, Pinto RZ, Trede RG, et al. Temporal couplings between rearfoot-shank complex and hip joint during walking. Clin Biomech. 2010;25:745–8. doi: 10.1016/j.clinbiomech.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 38.Levine D, Whittle MW. The effects of pelvic movement on lumbar lordosis in the standing position. J Orthop Sports Phys Ther. 1996;24:130–5. doi: 10.2519/jospt.1996.24.3.130. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37:389–98. doi: 10.2519/jospt.2007.2487. [DOI] [PubMed] [Google Scholar]
- 40.Janssen MMA, Drevelle X, Humbert L, et al. Differences in male and female spino-pevic alignment in asymptomatic young adults. Spine. 2009;34:E826–32. doi: 10.1097/BRS.0b013e3181a9fd85. [DOI] [PubMed] [Google Scholar]
- 41.Fukano M, Fukubayashi T. Gender-based differences in the functional deformation of the foot longitudinal arch. Foot. 2011;22:6–9. doi: 10.1016/j.foot.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Chung CY, Park MS, Lee SH, et al. Kinematic aspects of trunk motion and gender effect in normal adults. J Neuroeng Rehabil. 2010;7:9. doi: 10.1186/1743-0003-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chumanov ES, Wall-Scheffler C, Heiderscheit BC. Gender differences in walking and running on level and inclined surfaces. Clin Biomech. 2008;23:1260–8. doi: 10.1016/j.clinbiomech.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 44.Baylis WJ, Rzonca EC. Functional and structural limb length discrepancies: evaluation and treatment. Clin Podiatr Med Surg. 1988;5:509–20. [PubMed] [Google Scholar]
- 45.Sanner WH, Page JC, Tolboe HR, et al. A study of ankle joint height changes with subtalar joint motion. J Am Podiatry Assoc. 1981;71:158–61. doi: 10.7547/87507315-71-3-158. [DOI] [PubMed] [Google Scholar]
- 46.Sadeghi H, Allard P, Prince F, et al. Symmetry and limb dominance in able-bodied gait: a review. Gait Posture. 2000;12:34–45. doi: 10.1016/s0966-6362(00)00070-9. [DOI] [PubMed] [Google Scholar]
- 47.Lederman E. The fall of the postural-structural-biomechanical model in manual and physical therapies: exemplified by lower back pain. J Bodyw Mov Ther. 2011;15:131–8. doi: 10.1016/j.jbmt.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 48.Mills K, Blanch P, Chapman AR, et al. Foot orthoses and gait: a systematic review and meta-analysis of literature pertaining to potential mechanisms. Br J Sports Med. 2010;44:1035–46. doi: 10.1136/bjsm.2009.066977. [DOI] [PubMed] [Google Scholar]
- 49.Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998;11:46–56. [PubMed] [Google Scholar]
- 50.Dionne CE, Dunn KM, Croft PR, et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine. 2008;33:95–103. doi: 10.1097/BRS.0b013e31815e7f94. [DOI] [PubMed] [Google Scholar]